Published online Jan 26, 2020. doi: 10.12998/wjcc.v8.i2.306
Peer-review started: September 26, 2019
First decision: October 24, 2019
Revised: December 17, 2019
Accepted: December 21, 2019
Article in press: December 21, 2019
Published online: January 26, 2020
Processing time: 112 Days and 8 Hours
The clinical presentation of acute lymphoblastic lymphoma is highly varied. While prognosis is good, recurrence of disease can occur. Gastrointestinal relapse, including intussusception, is well-described but the absence of abdominal pain in this setting is rare.
We report a 13-year-old male with B-cell precursor acute lymphoblastic leukemia in remission presenting with anemia and weight loss. Examination was significant for absence of abdominal pain, but a stool sample was positive for occult blood. Pan-endoscopy was performed with colonoscopy revealing a mass filling the colonic lumen. Biopsy of the mass confirmed recurrence of recurrent B-cell lymphoma. Computed tomography scan revealed ileocolic intussusception resulting from the tumor. This case is unusual in that the patient had no abdominal pain despite the presence of intussusception.
While intestinal involvement with lymphoma has been well described in the literature, presentation as painless intussusception has not been reported. This case report highlights the wide spectrum of clinical manifestations of recurrent B-cell lymphoma involving the gastrointestinal tract, in particular the near absence of symptoms despite the finding of intussusception.
Core tip: Acute lymphoblastic leukemia and recurrent B-cell lymphoma are known to present in the gastrointestinal tract, most commonly with abdominal pain, either alone or in association with other symptoms, including rectal bleeding, vomiting, and/or abdominal distention. A common presentation is that of intussusception. We report a patient who was found to have recurrent B-cell lymphoma leading to intussusception during colonoscopy being performed for evaluation of anemia. There were no other clinical features, including abdominal pain, to suggest intussusception prior to colonoscopy. This case should serve as a cautionary tale that serious complications resulting from acute lymphoblastic leukemia may occur despite minimal clinical symptoms.
- Citation: Giroux P, Collier A, Nowicki M. Recurrent lymphoma presenting as painless, chronic intussusception: A case report. World J Clin Cases 2020; 8(2): 306-312
- URL: https://www.wjgnet.com/2307-8960/full/v8/i2/306.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i2.306
Gastrointestinal (GI) involvement by hematologic cancers (leukemia and lymphoma) related to malignant infiltration of the intestinal mucosal-associated lymphoid tissue is well documented. GI complications arising from these cancers include typhlitis, intestinal perforation, hemorrhage, and intussusception. Intussusception has been described both as the initial presentation of the cancer or as a later complication, almost universally presenting with abdominal pain due to bowel obstruction as a major symptom. Various diagnostic imaging studies have been used to diagnose intussusception, however, on rare occasions unsuspected intussusception has been made colonoscopy. Surgical resection or biopsy are the principle modes of documenting lymphoma as the underlying cause of intussusception when present. We report an adolescent with a history of acute lymphoblastic leukemia (ALL) who presented with anemia and was found at colonoscopy to have intussusception due to recurrent lymphoma.
A 13-year-old white male presented with iron-deficiency anemia and weight loss.
The patient had a past medical history of B-cell precursor ALL at 2-years of age. He achieved remission in 28 mo after completing standard risk chemotherapy treatment for ALL with doxorubicin and cyclophosphamide. At 7-years of age he developed cough, shortness of breath, and tiring easily. Echocardiogram was normal. Three months later he presented to the pediatric emergency room due to worsening pulmonary symptoms; a chest-x-ray showed hilar adenopathy and right-sided pleural effusion. Echocardiogram showed a large mass in the right atrium with a pericardial effusion. Computed tomography (CT) scan of the neck, chest, abdomen and pelvis with contrast revealed a 4.5 cm right sided mediastinal mass extending into the right atrium causing obstruction of the superior vena cava, right main pulmonary artery, and distal airway compression with paratracheal and mediastinal adenopathy. Flow cytometry was non-diagnostic for malignancy and bone marrow aspirate showed no evidence of infiltrative disease. Cardiac catheterization and biopsy of the tumor was initially interpreted as inflammatory myofibroblastic tumor, and chemotherapy was initiated with ifosfamide, doxorubicin, and celecoxib which achieved a decrease in tumor size. Following three courses of scheduled chemotherapy, cardiovascular surgery performed tumor resection. Final pathology was consistent with necrotic lymphoma consistent with recurrent B-cell lymphoma. He completed chemotherapy and began maintenance therapy. Eighteen months later he presented with weight loss and anemia.
Approximately 18-mo later, at 13 years of age, he was seen in pediatric gastroenterology clinic for iron-deficiency anemia, decreased oral intake, and weight loss of 5.7 kg. He did not have fatigue, malaise, shortness of breath, palpitations, melena, hematochezia, or abdominal pain.
The patient was a student in good standing. Family history was negative for inflammatory bowel disease, polyp syndromes, and bleeding dyscrasias.
On physical examination he had no tachycardia or cardiac murmur, his lungs were clear to auscultation, his abdomen was soft, non-tender, without hepatosplenomegaly, there was no bruising, digital rectal exam revealed brown stool that was positive for fecal occult blood.
Complete blood count revealed a normal white blood cell count (9200/mm3), microcytic anemia (hemoglobin = 9.0 g/dL, hematocrit = 30.9%, mean corpuscular volume = 61 fL), and thrombocytosis (platelets = 726000/mm3). Other laboratory values were normal including a liver panel, renal panel, lactate dehydrogenase and uric acid.
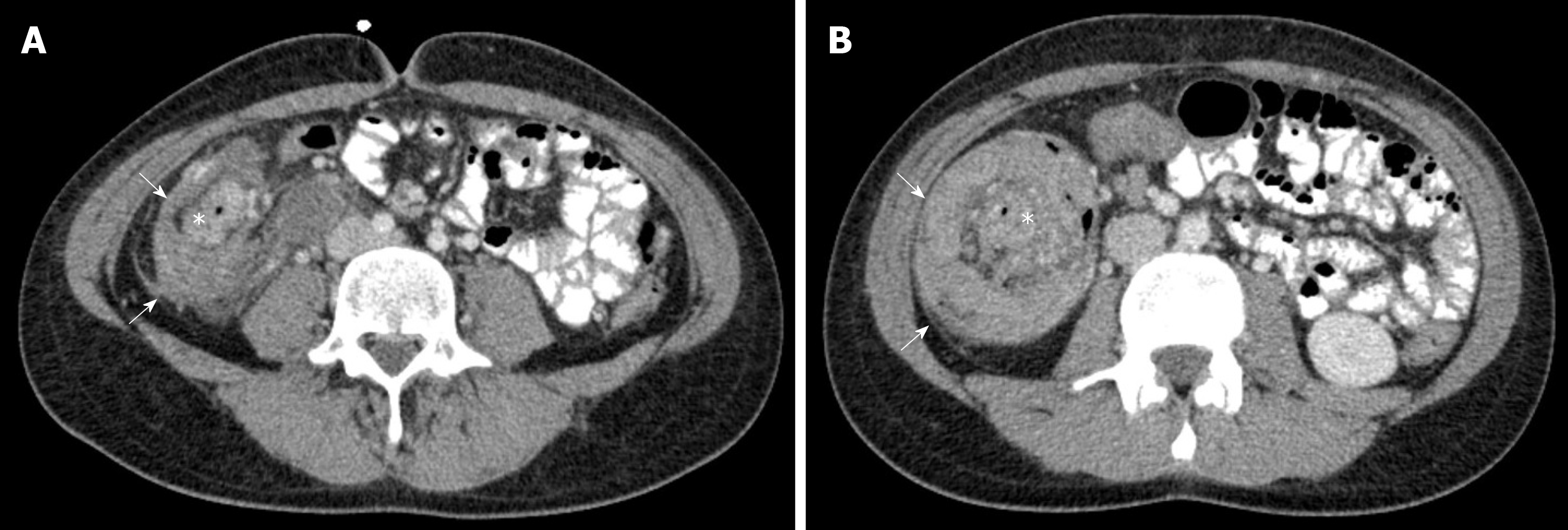
The patient underwent esophagogastroduodenoscopy (EGD) and colonoscopy. EGD results were unremarkable; however, a large, firm mass in the mid-ascending colon was discovered on colonoscopy and subsequently biopsied (Figure 1). The biopsy confirmed recurrent B-cell ALL. CT scan showed ileo-colonic intussusception (Figure 2) with the mass acting as the lead points. Pathology results showed a recurrent B-cell lymphoma in the ileum causing chronic intussusception.
The final diagnosis was ileocolic intussusception due to intestinal relapse of B-cell ALL.
The patient was admitted and started on chemotherapy including intrathecal methotrexate, cytarabine, and clofarabine.
His hospital course was complicated by febrile neutropenia, thrombocytopenia, anemia, and clostridium difficile infection. The patient was minimally responsive to chemotherapy, and palliative right hemicolectomy with primary anastomosis was performed 3 mo after diagnosis. This procedure was complicated by anastomotic leak, so the patient underwent bowel resection with ileostomy. The patient and family initially planned to proceed with bone marrow transplant. However, the patient no longer desired to pursue chemotherapy or transplant and was transferred to hospice care where he passed away 5 mo after relapse.
We report our patient to alert physicians to the subtlety to which intussusception can present, as well as to highlight the rare presentation and unusual diagnostic method utilized. Our patient was in remission and developed anemia, but was otherwise asymptomatic. He was found to have occult blood in his bowel movements. He underwent EGD and colonoscopy as part of the investigation and was found to have a luminal mass, biopsy proved to be a lymphoma. Colonoscopy as a modality for the diagnosis of intestinal lymphoma has only been reported once to date[1]. After making the diagnosis of relapsed lymphoma in the small intestine as the cause of intussusception, we performed a literature search and found three large retrospective reviews and a number of case reports/series describing intussusception related to hematologic cancers in children. We review and report on the clinical features of intussusception related to hematologic cancers.
Intussusception resulting from GI involvement in hematologic cancers (leukemia and lymphoma) is a well-described, yet occurs rarely. In a retrospective review of 378 children identified with intussusception over 31-years, only 1.6% were found to have lymphosarcoma as a lead point[2]. In two large retrospective reviews of children with Burkitt’s lymphoma, the prevalence of developing intussusception was 6.7% in one study and 17.5% in the other[3,4]. In a smaller study of children with primary abdominal non-Hodgkin’s lymphoma, 25% developed intussusception[5]. Intussusception has been reported less frequently in children with leukemia. In a study of 364 Taiwanese children with leukemia only 1 (0.3%) developed intussusception[6]. In a study from the United Kingdom no intussusception was found in 800 children[7].
Combining the data from the retrospective reviews and case reports (Table 1) there were 74 patients with intussusception and a hematologic malignancy for review[8-22]. The majority of patients were male (80.3%). The average age (8.0 ± 3.8 years) and median age (7.5 years) were higher than the typical age (< 2 years) of children with intussusception. Only two children were less than two years of age. The type of cancer was more commonly lymphoma (85.3%) than leukemia (14.3%), however, the data may be skewed as two large retrospective studies were done to assess for intussusception in children with lymphoma[3,4].
| Characteristics | Value | |
| Gender | Male | 80.3% |
| Female | 19.7% | |
| Age | Average | 8.0 ± 3.8 yr |
| Median | 7.5 yr | |
| Type of malignancy | Lymphoma | 85.3% |
| Leukemia | 14.7% | |
| Presenting symptom(s) | Anemia | 6.3% |
| Abdominal pain | 25.0% | |
| Abdominal pain, distension | 31.3% | |
| Abdominal pain, vomiting | 12.5% | |
| Abdominal pain, hematochezia | 12.5% | |
| Abdominal pain, vomiting, hematochezia | 12.5% | |
Intussusception as the initial presentation of hematologic cancer occurred in 47.6% of the patients (Table 2). Intussusception was seen as a complication of known cancer in the remaining patients; occurring more commonly during maintenance (19.0%) or at relapse of disease (19.0%), then during induction (14.3%). Where documented, most patients (89.7%) had an identifiable lead point; the most common lead point was the cancer (80.8%), followed by mucosal necrosis (7.7%), typhlitis (3.8%), hematoma (3.8%), and lymph node (3.8%). The majority of intussusceptions were ileo-colic (86.7%), followed by ileo-ileal (9.3%), ileo-ileo-colic (2.7%) and colo-colic (1.3%). Intussusception was acute in 60% of children and chronic in 40%.
| Characteristics | Percentage | |
| Timing of intussusception in relation to malignancy | At diagnosis | 47.6% |
| Induction | 14.3% | |
| Maintenance | 19.0% | |
| Relapse | 19.0% | |
| Location of intussusception | Ileo-colic | 86.7% |
| Ileo-ileal | 9.3% | |
| Ileo-ileo-colic | 2.7% | |
| Colo-colic | 1.3% | |
| Chronicity of intussusception | Acute | 40.0% |
| Chronic | 60.0% | |
| Presence of a lead point | Yes | 89.7% |
| No | 10.3% | |
| Cause of lead point | Malignancy | 80.8% |
| Necrosis | 7.7% | |
| Hematoma | 3.8% | |
| Lymph node | 3.8% | |
| Typhlitis | 3.8% | |
| Barium enema reduction | Successful | 14.3% |
| Unsuccessful | 85.7% | |
| Surgical intervention required | Yes | 95.7% |
| No | 4.3% | |
| Diagnostic mode for cancer | Surgery | 77.8% |
| Colonoscopy | 11.1% | |
| Imaging | 5.6% | |
| Autopsy | 5.6% | |
All of the reported patients presented with abdominal pain and various combinations of abdominal distension, vomiting, and hematochezia (Table 1). The patient described herein was asymptomatic regarding GI complaints. He underwent colonoscopy as part of the evaluation for anemia and was found to have a large mass filling the colon lumen; biopsy of the mass showed recurrent lymphoma.
A number of children had a contrast enema performed in an attempt to reduce intussusception, the majority (85.7%) were not successful resulting in the need for surgery (Table 2). Overall, surgical intervention occurred in the vast majority (95.7%) of the children. A tissue diagnosis was most often obtained by surgical biopsy (77.8%); diagnosis was made by colonoscopic biopsies on 2 occasions (11.1%), by PET scan (5.6%) and at autopsy (5.6%) once each.
We report a young man with ALL relapse presenting with asymptomatic intussusception with the diagnosis being made with colonoscopic biopsies. This case should serve as a cautionary tale that serious complications resulting from ALL may occur despite minimal clinical symptoms.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rolle U, Yamamoto T S-Editor: Dou Y L-Editor: A E-Editor: Xing YX
| 1. | Berkelhammer C, Caed D, Mesleh G, Bolanos J, McGinnis P, Zeiger H. Ileocecal intussusception of small-bowel lymphoma: diagnosis by colonoscopy. J Clin Gastroenterol. 1997;25:358-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Wayne ER, Campbell JB, Kosloske AM, Burrington JD. Intussusception in the older child- suspect lymphosarcoma. J Pediatr Surg. 1976;11:789-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Gupta H, Davidoff AM, Pui CH, Shochat SJ, Sandlund JT. Clinical implications and surgical management of intussusception in pediatric patients with Burkitt lymphoma. J Pediatr Surg. 2007;42:998-1001; discussion 1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 44] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | England RJ, Pillay K, Davidson A, Numanoglu A, Millar AJ. Intussusception as a presenting feature of Burkitt lymphoma: implications for management and outcome. Pediatr Surg Int. 2012;28:267-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | LaQuaglia MP, Stolar CJ, Krailo M, Exelby P, Siegel S, Meadows A, Hammond D. The role of surgery in abdominal non-Hodgkin's lymphoma: experience from the Childrens Cancer Study Group. J Pediatr Surg. 1992;27:230-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Chien CH, Lin DT, Lin KH, Chang MH, Lee CY, Lin KS. Acute abdomen in childhood leukemia. J Formos Med Assoc. 1990;89:12-16. [PubMed] |
| 7. | Micallef-Eynaud P, Eden OB. Intussusception in acute childhood lymphoblastic leukemia: an unusual complication. Pediatr Hematol Oncol. 1990;7:389-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Dudgeon DL, Hays DM. Intussusception complicating the treatment of malignancy in childhood. Arch Surg. 1972;105:52-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Sherman NJ, Williams K, Woolley MM. Surgical complications in the patient with leukemia. J Pediatr Surg. 1973;8:235-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Karakousis C, Holyoke ED, Douglass HO. Intussusception as a complication of malignant neoplasm. Arch Surg. 1974;109:515-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Goldin E, Libson E. Intussusception in intestinal lymphoma: the role of colonoscopy. Postgrad Med J. 1986;62:1139-1140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Manglani MV, Rosenthal J, Rosenthal NF, Kidd P, Ettinger LJ. Intussusception in an infant with acute lymphoblastic leukemia: a case report and review of the literature. J Pediatr Hematol Oncol. 1998;20:467-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Kumari TP, Mohan SV, Shanavas A, Kumari PK. Intussusception at the onset of acute lymphoblastic leukemia in a child. Indian Pediatr. 1998;35:470-472. [PubMed] |
| 14. | Arestis NJ, Mackinlay GA, Hendry GM. Intussusception in children with ALL receiving chemotherapy for acute lymphoblastic leukaemia. Pediatr Blood Cancer. 2005;45:838-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Schaefer EA, Dranove JE, Gupta SK. Clinical Challenges and Images in GI. Ileocolic intussusception caused by Burkitt's lymphoma. Gastroenterology. 2008;134:20, 373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Chamroonrat W, Cheng G, Servaes S, Zhuang H. Intussusception incidentally detected by FDG-PET/CT in a pediatric lymphoma patient. Ann Nucl Med. 2010;24:555-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Singal R, Gupta S, Goel M, Jain P. A rare case of chronic intussusception due to non Hodgkin lymphoma. Acta Gastroenterol Belg. 2012;75:42-44. [PubMed] |
| 18. | Kang HJ, Beylergil V, Price AP, Abramson SJ, Carrasquillo JA. FDG PET/CT detection of intussusception caused by lymphoma in a pediatric patient. Clin Nucl Med. 2014;39:97-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Sinha CK, Basson S, Patel RV, Mathur AB. Norwich paediatric triad: malrotation, intussusception and small intestinal lymphoma. BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Bassily E, Bowen A. A 12-Year-Old Girl with Persistent Abdominal Pain and Emesis. Pediatr Ann. 2015;44:270-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Choi SH, Han SA, Won KY. Chronic Intussusception Caused by Diffuse Large B-Cell Lymphoma in a 6-Year-Old Girl Presenting with Abdominal Pain and Constipation for 2 Months. J Korean Med Sci. 2016;31:321-325. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | D'Angelo G, Marseglia L, Manti M, Stroscio G, Impollonia D, Arena S, Impellizzeri P, Salpietro C, Romeo C, Gitto E. An unusual and malignant intussusception in a child. Ital J Pediatr. 2016;42:72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |