Published online Jan 26, 2020. doi: 10.12998/wjcc.v8.i2.284
Peer-review started: September 23, 2019
First decision: December 4, 2019
Revised: December 17, 2019
Accepted: December 21, 2019
Article in press: December 21, 2019
Published online: January 26, 2020
Processing time: 115 Days and 21.5 Hours
Relapse following orthodontic treatment has been a common problem that can occur due to several factors. It was suggested that surgical circumferential supracrestal fiberotomy (CSF) is an effective measure to reduce this relapse. However, very few studies have reported the amount of relapse that occurs afterward.
To assess the frequency of rotational relapse on anterior teeth 1 year following CSF.
Eleven adults (six male and five female) with a mean age of 23 years (standard deviation = 5.2), who had a total of 90 rotated anterior teeth, were included in this study. CSF was performed after comprehensive orthodontic treatment involving the use of full-fixed preadjusted edgewise appliances (Victory Series APC, 3M, United States) with a 0.022-inch slot and Roth prescription brackets (Ovation; DENTSPLY GAC, Bohemia, New York, United States) and placement of a fixed lingual retainer from canine to canine in both arches using a 0.016 Australian wire (AJ Wilcock, Australia). Degrees of rotational correction and relapse were measured on three sets of casts [pretreatment, post-treatment (at the debond visit), and 1-year post-treatment]. Rotational relapse was categorized as follows: Unnoticeable relapse (0°), barely noticeable relapse (1°-3°), noticeable relapse (4°-9°), and clearly noticeable relapse (≥ 10°). The percent relapse that had occurred 1 year after teeth were aligned to their ideal position was calculated. Data were analyzed by dental arch type and tooth types.
Mean rotational correction was 14.05° during posttreatment. Mean relapse at 1-year follow-up was 1.1° (10.8%). More than half (n = 52, 57.8%) of teeth were categorized as having unnoticeable relapse (0°). Of the remaining teeth, 31 (34.5%) had barely noticeable relapse (1°-3°), 6 (6.6%) had noticeable relapse (4°-9°), and only one (1.1%) had clearly noticeable relapse (> 10°). When analyzed by arch, 54.5% (n = 6) of the relapsed maxillary teeth had barely noticeable relapse (1°-3°). While most of the mandibular teeth (3, 37.5%) fell into noticeable relapse category (4°-9°), only 1 (12.5%) tooth had clearly noticeable relapse (≥ 10°).
When relapse was measured following CSF, it was found to be more pronounced in maxillary than in mandibular arch. Most frequent relapse was found in maxillary lateral incisors and mandibular canines.
Core tip: Postorthodontic rotational relapse was more frequent in the maxillary arch than in the mandibular arch. Approximately 42% of teeth showed some degree of rotational relapse. Only one tooth had clearly noticeable relapse (> 10°). Relapse was most frequent in the maxillary lateral incisors and mandibular canines. Conventional circumferential supracrestal fiberotomy was effective in minimizing rotational relapse when assessed 1 year after the procedure. Future controlled studies with larger sample sizes are warranted to evaluate the present findings.
- Citation: Al-Jasser R, Al-Jewair T, Al-Rasheed A. One-year rotational relapse frequency following conventional circumferential supracrestal fiberotomy. World J Clin Cases 2020; 8(2): 284-293
- URL: https://www.wjgnet.com/2307-8960/full/v8/i2/284.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i2.284
Rotational tooth movement, according to Smith et al[1], is the process of rotating a tooth around its longitudinal axis or its center of resistance. The prevalence of tooth rotation in the general population ranges between 2.2%-5.1%[2]. Rotations are most prevalent in the mandibular premolars and maxillary central incisors[3,4]. In terms of severity, the majority of rotations are between 45° and 90° from the normal position[5].
The etiology of tooth rotation is not fully understood. However, multiple genetic and environmental factors may contribute to its development. These include the presence of supernumerary teeth, severe tooth-size arch length discrepancy, ectopic eruption of permanent teeth, tooth bud position abnormalities, dental crowding, cleft palate, over-retained primary teeth, and genetic factors[6-9].
Orthodontic treatment has been successful at correcting tooth rotations[10,11]. However, relapse following orthodontic treatment has been a long-standing problem that can occur due to poor compliance with wearing retainers, iatrogenic factors[12], limited ability of supra-alveolar fibers to reorganize and adapt to the corrected tooth position even with a long period of mechanical retention[13], or a combination of the above factors. When the supra-alveolar fibers, attachment to related teeth remains unchanged after correction of rotations, the elasticity of these fibers will act to pull teeth back to their pretreatment positions, and relapse will likely occur. It was suggested that rotational relapse postorthodontic treatment could be predicted from the amount of rotation present pretreatment[14].
Multiple methods have been proposed to prevent or minimize rotational relapse. These techniques include overcorrection of rotated teeth, interproximal reduction to widen proximal contacts, long-term use of retainers, and surgical circumferential supracrestal fiberotomy (CSF)[4,15]. CSF is a surgical periodontal procedure that is performed to separate the free gingiva and transseptal fibers around orthodontically derotated teeth. This separation reduces tension occurring from these fibers that pulls teeth into their original positions, hence preventing relapse[15].
CSF is more effective at alleviating pure rotational relapse than labiolingual relapse. Furthermore, CSF is also more effective at reducing relapse in the maxillary anterior segment than in the mandibular anterior segment[15,16]. Regarding the periodontal status of treated teeth, no clinically significant increase in periodontal sulcus depth or decrease in labially attached gingiva of CSF-treated teeth was observed at 1 mo and 6 mo following the surgical procedure[13].
Long-term stability after CFS has been documented in a few studies[15,17,18]. Edwards[15] evaluated the effects of CSF in preventing orthodontic relapse over a 15-year period. The author compared two groups of orthodontic patients: One received CSF while the other did not. CSF was performed on both the maxillary and mandibular teeth. A statistically significant difference between the mean relapse of the controls and the CSF cases was reported, with approximately 29% less mean relapse in the CSF cases.
New advances in CSF, such as laser-aided CSF, have been proposed and evaluated in recent studies. Jahanbin et al[19] reported that an Er:YAG laser and low-level laser at high density are both as effective as conventional CSF at 1 mo after performing the procedures. These new procedures are associated with fewer side effects. Future studies are needed to investigate laser-aided CSF.
Very few studies have examined the frequency of rotational relapse in relation to CSF. Additionally, evidence on relapse by tooth type and location is scarce[15,17,18]. Therefore, the aims of the present study were to assess the frequency of rotational relapse in the maxilla and mandible 1 year after performing a CSF procedure and orthodontic therapy.
This case series was conducted from January 2016 to June 2017 at one private practice in the city of Riyadh, Saudi Arabia. The Institutional Committee of Research Ethics at the University approved the protocol of this study (NF 2254).
The sample consisted of adult subjects who underwent corrective anterior tooth derotation during orthodontic treatment followed by surgical CSF. Subjects were assessed at three time points: T1 = pretreatment (initial records visit); T2 = postorthodontic treatment, day of appliance debonding, insertion of fixed lingual retainers, and surgical CSF procedure; and T3 = 12-mo retention follow-up.
The inclusion criteria were healthy adults (18 years or older) who presented with anterior tooth rotations in either of the two arches and received nonsurgical full-fixed orthodontic treatment to correct the rotated teeth and the malocclusion. Patients with anterior tooth extraction, buccolingual tooth displacement, or a significant medical history including diabetes, pregnancy, autoimmune disease, history of periodontal disease, or previous orthodontic treatment were all excluded. Subjects were also excluded if their orthodontic treatment involved teeth extraction or treatment modalities that might affect the buccolingual tooth inclination, such as growth modification and arch expansion.
Orthodontic treatment: After obtaining consent from all participants, all names were deidentified, and only numerical codes were assigned to ensure confidentiality. The orthodontic treatment involved the use of full-fixed preadjusted edgewise appliances (Victory Series APC, 3M, United States) with a 0.022-inch slot and Roth prescription brackets (Ovation; DENTSPLY GAC, Bohemia, NY, United States). All patients were corrected for normal Class I dental occlusion. Overcorrection of rotation was not attempted in any of the cases. Following appliance debonding, a lingual bonded fixed retainer was placed from canine to canine in both arches using a 0.016 Australian wire (AJ Wilcock, Australia). All patients were treated by the same orthodontist (N.J.).
CSF was performed after the anteriorly rotated teeth were appropriately aligned to their ideal positions, and the lingual bonded retainer was placed. All patients had well-controlled oral hygiene and no signs of gingival inflammation or pockets around the target teeth at the time of surgery. Lidocaine 5% ointment was applied to the gingiva for topical anesthesia, followed by local infiltration with lidocaine (1:100000 epinephrine). Using a No. 15 or No. 12 blade, a crevicular (sulcular) incision was made through the gingival crevice of the aligned tooth down to the level of the alveolar crest. Keeping the blade close to the cementum and parallel to the root, the incision was extended down to the crestal bone, passing circumferentially from the labial surface to the lingual surface, including the proximal surface, and severing all the supracrestal fibers around each derotated tooth. Following the CSF, the teeth were smeared with saline, after which pressure was applied to the labial and lingual surfaces for 5 min using cotton gauze. No periodontal packs were used, and the healing was uneventful. All postsurgical follow-up evaluations were performed by one periodontist (A.R.). None of the patients reported postoperative discomfort or any noticeable changes in the surgical sites at the 1-wk follow-up appointment.
Three sets of study models were obtained from each patient at each of the three time points (T1, T2, and T3). The derotated teeth were marked with a black pen marker on all serial models prior to data measurements. Then, a high-resolution photocopy of the occlusal surface of each cast was made. All casts were photocopied by the same operator (R.J.).
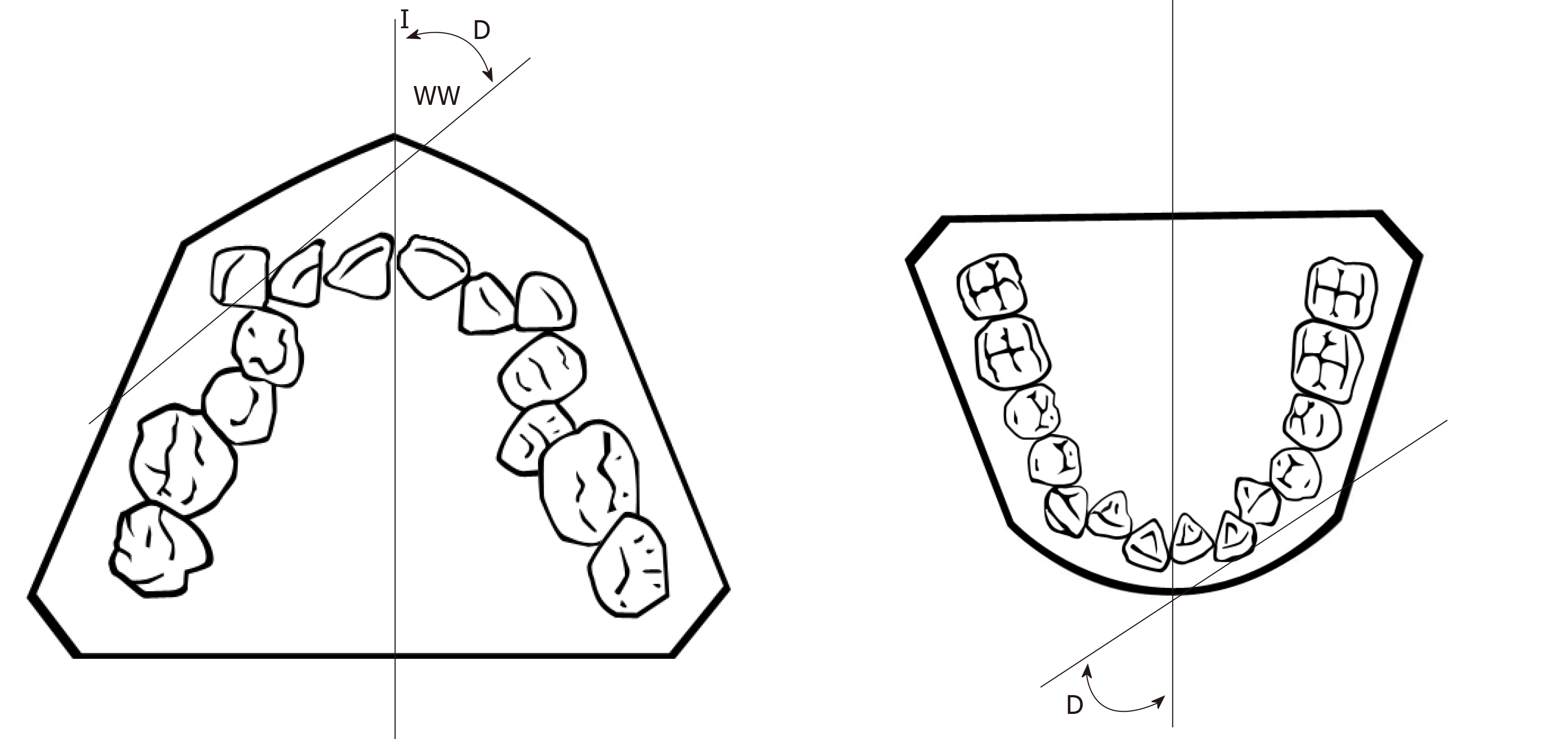
Several parameters were assessed on the cast photocopies at each time point utilizing the method of Ahrens et al[20]. In the maxillary arch, the angle formed by the incisal plane that passed through the incisal edge of the tooth and the median palatal plane was used to measure the degree of rotation (D) of each anterior tooth. In the mandibular arch, due to the lack of a stable and reproducible landmark, a modification was made as follows: A line was drawn connecting the middle fossa of the lower first molar on each side to represent the intermolar plane, which was confirmed by the treating orthodontist to be stable in all cases throughout treatment and to be the most stable landmark in the mandibular arch after orthodontic treatment. A line perpendicular to the intermolar plane line was drawn and chosen as the reference line for measurement of the mandibular anterior teeth[21]. The incisal plane of each mandibular tooth was then drawn as described above, and the angle formed by the incisal plane and the lower reference line determined the degree of rotation of that tooth (Figure 1).
The angle of rotation of each target tooth in the sample was measured in degrees on the T1 cast (D1), T2 cast (D2), and T3 cast (D3). The degree of rotational correction required (C), defined as the amount of correction needed to derotate a tooth from its pretreatment position (T1) to its aligned position (zero degree rotation) relative to the adjacent teeth, was measured as the difference between the angle measured for a rotated tooth on the T1 cast (D1) and the angle measured for the same tooth on the T2 cast (D2), i.e., C = D1 – D2. The amount of rotational relapse (R) that occurred in each aligned tooth was determined by calculating the difference between D3 and D2 angles, i.e., R = D3 – D2. The percent relapse (R%) relative to the degree of rotational correction was calculated as follows: R% = (R / C) × 100[22].
All measurements were made by one orthodontist (N.J.), who was blinded to the type of cast. The amount of relapse was assessed using the following categories: Unnoticeable relapse (0°), barely noticeable relapse (1°-3°), noticeable relapse (4°-9°), and clearly noticeable relapse (≥ 10°).
Four randomly selected casts representing 36 rotated teeth were measured on two occasions, separated by an interval of 1 wk. The intra-examiner reliability of the measurements was assessed using Cohen’s Kappa score.
Data were analyzed using IBM SPSS version 16.0 for Windows. Data on the extent of relapse constituted the variable of interest. A descriptive analysis was performed to determine the percent relapse that had occurred 1 year after teeth were aligned to their ideal position. Data were analyzed by dental arch and by type of tooth. For arch level analysis, the highest relapse category present was selected to categorize the arches. The Wilcoxon test for dependent variables was used to assess whether there was any significant difference in the change in rotational angle for all teeth between pretreatment cast 1 and postalignment cast 2. The same test was used to compare the change in rotational angle for all teeth between cast 2 and cast 3. The paired t-test was used to estimate the correlation between the first and second readings to confirm intra-examiner reliability. All analyses were performed at a significance level of α = 0.05.
In terms of reliability, there was no statistically significant difference in the two sets of cast measurements taken by the same examiner, indicating excellent intra-examiner reliability.
Eleven subjects (six males and five females) with a mean age of 23 years [standard deviation = 5.2) were included in this study. The mean comprehensive orthodontic treatment length (T2-T1) was 24 mo (standard deviation = 3). The mean retention duration following comprehensive orthodontic treatment (T3-T2) was 12 mo (standard deviation = 1.5).
The malocclusions in all subjects were corrected to Class I molar and canine relationships with preservation of the midlines. A total of 90 rotated teeth in 11 maxillary and 8 mandibular arches were assessed. The mean initial rotation at T1 was 14.05° (2.10°). This value was similar to the mean rotational correction (derotation) (C°) from T1 to T2 and reflected a 100% rotational correction.
The mean rotational relapse and the percent relapse from T2 to T3 were 1.1° (2.4°) and 10.8%, respectively. There was a statistically significant difference in the change in rotational angles for all teeth between T1 and T2 (P = 0.020, Wilcoxon test) but not between T2 and T3 (P = 0.190).
When assessed by arch, 8% (n = 6) of the 52 rotated maxillary teeth had rotational relapse. The mean relapse for these teeth was 0.81° (0.20°). The mean relapse for the mandibular teeth was 1.44° (0.60°), and the relapse percentage was 14%, which was higher than that of the maxillary teeth. However, no significant difference in the amount of relapse was noted between the two arches (P = 0.070) (Table 1).
| Arch, n = 19 | Tooth, n = 90 | C° | R° | R% |
| Maxillary, n = 11 | Total, n = 52 | 14.6 (2.7) | 0.8 (0.2) | 8.0 |
| Canine, n = 17 | 9.4 (1.5) | 0.4 (0.3) | 6.1 | |
| Lateral incisor, n = 19 | 14.9 (2.4) | 1.0 (0.2) | 10.8 | |
| Central incisor, n = 16 | 19.8 (1.5) | 10.6 (0.5) | 7.6 | |
| Mandibular, n = 8 | Total, n = 38 | 13.5 (4.2) | 1.4 (0.6) | 14.0 |
| Canine, n = 11 | 12.2 (2.6) | 2.9 (0.3) | 17.8 | |
| Lateral incisor, n = 13 | 14.5 (3.2) | 0.8 (0.1) | 13.9 | |
| Central incisor, n = 14 | 13.1 (2.4) | 1 (0.2) | 12.3 |
The overall rotational relapse frequency is presented in Table 2. When assessed at T3 more than half (n = 52, 57.8%) of the teeth were categorized as having unnoticeable relapse (0°). Of the remaining teeth, 34.5% (n = 31) had barely noticeable relapse (1°-3°), 6.6% (n = 6) had noticeable relapse (4°-9°), and 1.1% (n = 1) had a clearly noticeable relapse (≥ 10°).
| Relapse category | Teeth, n = 90 | Percent |
| Unnoticeable relapse, 0° | 52 | 57.8 |
| Barely noticeable relapse, 1°-3° | 31 | 34.5 |
| Noticeable relapse, 4°-9° | 6 | 6.6 |
| Clearly noticeable relapse, ≥ 10° | 1 | 1.1 |
The frequency of rotational relapse in the maxillary and mandibular arches is depicted in Table 3. Overall, 42% (n = 8) of the teeth had barely noticeable relapse (1°-3°). When analyzed by arch, 54.5% (n = 6) of the relapsed maxillary teeth had barely noticeable relapse (1°-3°), 37.5% (n = 3) of the mandibular teeth exhibited noticeable relapse (4°-9°), and 12.5% (n = 1) was categorized as having a clearly noticeable relapse (≥ 10°).
| Category | Total | Maxillary | Mandibular |
| Unnoticeable relapse, 0° | 4 (21.0) | 2 (18.2) | 2 (25.0) |
| Barely noticeable relapse, 1°-3° | 8 (42.1) | 6 (54.5) | 2 (25.0) |
| Noticeable relapse, 4°-9° | 6 (31.6) | 3 (27.3) | 3 (37.5) |
| Clearly noticeable relapse, ≥ 10° | 1 (5.3) | 0 (0.0) | 1 (12.5) |
| Total | 19 (100.0) | 11 (100.0) | 8 (100.0) |
When data were further analyzed by tooth type, all anterior teeth had unnoticeable relapse (0°) as the highest category, indicating stability of results except for the maxillary central incisors, which showed barely noticeable relapse (1°-3°) as their highest category (n = 9, 56.2%). Finally, mandibular canines were shown to include a clearly noticeable relapse (≥ 10°) category (n = 1, 9.1%) (Table 4).
| Category | Tooth type | |||||
| Maxillary | Mandibular | |||||
| Canine | Lateral incisor | Central incisor | Canine | Lateral incisor | Central incisor | |
| Unnoticeable relapse, 0° | 12 (70.5) | 10 (52.6) | 6 (37.5) | 6 (54.5) | 11 (84.6) | 7 (50.0) |
| Barely noticeable relapse, 1°-3° | 5 (29.5 ) | 7 (36.8) | 9 (56.3) | 2 (18.2) | 1 (7.7) | 4 (28.6) |
| Noticeable relapse, 4°-9° | 0 (0.0) | 2 (10.5) | 1 (6.2) | 2 (18.2) | 1 (7.7) | 3 (21.4) |
| Clearly noticeable relapse, ≥ 10° | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (9.1) | 0 (0.0) | 0 (0.0) |
| Total | 17 (100.0) | 19 (100.0) | 16 (100.0) | 11 (100.0) | 13 (100.0) | 14 (100.0) |
| P value | 0.132 | 0.194 | ||||
This case series determined the frequency of rotational relapse following CSF and retainer placement performed on 90 derotated anterior maxillary and mandibular teeth. At the 12-mo follow-up assessment, 57.8% of the teeth maintained their corrected position, and no statistically significant relapse had occurred, which confirms the effectiveness of CSF, as reported in multiple previous studies[12,15,20,23].
The percent relapse among the 90 teeth was 8% in the maxillary arch and 14% in the mandibular arch. The percentage in the maxillary arch was similar to the findings of Jahanbin et al[19], who found a 9.7 ± 2.3% relapse in the maxillary arch with conventional CSF surgery at the 1-mo assessment. Edwards[15], in his classic study, reported that the mean relapse of subjects who underwent CSF was 29% lower than that of control subjects when assessed long-term (retention period ranging from 24-40 mo). These findings demonstrate that despite permanent retention and CSF surgery, relapse can still occur. Other methods to prevent relapse may need to be investigated.
When assessed by tooth type, the highest relapse frequency occurred in the lateral incisors of the maxilla (10.8%) and in the canines of the mandible (17.8%). However, these differences were not statistically significant in relation to the other tooth types observed. These findings contradict those of other researchers, who have stated that CSF is more effective in reducing relapse in maxillary anterior teeth vs mandibular teeth[15,16]. Swanson et al[21] evaluated the incidence and stability of rotated teeth in 116 subjects over a 10-year postretention period. The authors found that the incidence of rotation ranged from highest to lowest in cuspids, premolars, lateral incisors, central incisors, and finally first molars in both arches. Our results were consistent with their findings for the mandibular arch but different for the maxillary arch. The differences between the two studies could partly be explained by the different follow-up durations and the methodology used to measure rotational relapse. We assessed relapse categorically, while they reported mean changes in their samples. Our results were also partially consistent with those of Edwards[15], who determined that mandibular cuspids relapse the most followed by maxillary cuspids[15]. Notably, Edwards evaluated relapse using Little’s irregularity index with a dial caliper on stone models[16]. However, this index has multiple limitations. It mainly measures horizontal malalignment and does not specifically measure rotational relapse or changes in torque or tip. Additionally, its scores have low repeatability and precision, and it can only be applied on anterior teeth[24]. The present study used a modification of the method of Ahrens et al[20] but analyzed rotation relapse categorically to fully explain the severity of relapse in comparison to the amount of rotation at the pretreatment stage.
While there is no absolute theory to explain how and why relapse occurs, multiple hypotheses have been proposed, such as late mandibular growth, lack of reorganization of the gingival and periodontal fibers after being stretched at the rotation treatment stage, and unstable tooth position after teeth alignment, among other factors[25-27]. Thus, the reason why maxillary lateral incisors and mandibular canines showed the greatest amount of relapse compared to other teeth can only be hypothesized.
In this study, only fixed bonded lingual retainers were utilized from canine to canine, and no additional vacuum-formed retainers were prescribed. This approach might explain the relapse in the mandibular canines because they are at the end of the sectional wire and their distal contacts may slip out of contact more easily than those of other teeth.
The tendency of certain teeth to relapse more than others is likely influenced by the amount of rotational correction from the initial dental position that is required. Boese [28] and Swanson et al[21] separately reported a direct relationship between relapse and initial rotation,. Ultimately, teeth that require a greater amount of rotational correction are more likely to relapse and should be considered for surgical intervention. In this study, although the tooth rotations were greater than 10 degrees for multiple anterior teeth at preorthodontic treatment, the relapse fell into the barely noticeable and noticeable categories, and only one tooth had a clearly noticeable relapse. In fact, the majority of teeth in the maxilla and mandible had “barely noticeable” relapse (1°-3°). This finding can be explained by the tendency of the intercanine width to return to its pretreatment value or by the anterior component of force[19,29], in addition to the fact that CSF is reported to be less effective in the mandibular anterior segment than in the maxillary segment[30].
Multiple authors have attempted to objectively quantify post-treatment and postretention dental relapse, including rotational relapse. One very popular index is Little’s irregularity index[16]. The limitations of this index were previously acknowledged in this section[24]. Edwards[15], on the other hand, argued that this index provides an easy measure of relapse, especially for labiolingual displacement. Another index by Swanson et al[21] measures the angles of teeth relative to the midpalatal raphe on standardized stone models. A third method to measure rotational relapse is by assessing the direction of relapse after the teeth are derotated to an ideal alignment. The directions are relapsed in the same direction of movement vs relapse in the opposite direction[31]. A gold standard method to determine relapse does not exist, and valid and reliable methods to quantify rotational relapse are severely needed. This study proposed a new classification for relapse by degree of rotation from unnoticeable to clearly noticeable relapse (≥ 10°). A 10-degree cut-off was chosen because at this amount, the tooth was clinically clear to be shifted from its normal position, which was unaesthetic and indicated for an additional orthodontic intervention, as reported by the orthodontist in this study This method of categorization when used clinically was found to be simple and clear and made it easy to determine the post-treatment results and tooth prognosis.
This study has several limitations. The small sample size, the absence of a separate control group for proper comparison, and the lack of a short-term assessment of relapse prior to the 1-year mark limit the generalizability of the results. Future longitudinal studies with control groups and different evaluation durations can validate our results.
Additionally, in this study, conventional surgical CSF was performed by one periodontist. This procedure, while effective in minimizing rotational relapse, is technique sensitive and may result in side effects, including pain and periodontal recession[32].
The conventional surgical approach to CSF remains an acceptable method[33]. However, the use of a scalpel blade during the procedure can lead to some deleterious effects, including pain, bleeding, and poor patient acceptance[34]. Therefore, minimally invasive approaches have been proposed to overcome these effects. These methods include low-level laser therapy[35], electrosurgery[34], and laser-aided fiberotomy[36,37]. A clinical trial was performed to compare the effect of Er, Cr:YSGG laser-aided CSF to a conventional approach and revealed comparative results in reducing the rotational relapse tendency[37]. This finding was further supported by a study that compared the effects of (Ga-Al-As) diode laser CSF and low-level laser therapy on orthodontically rotated teeth in beagles. The study found that laser CSF was an effective procedure to decrease relapse after tooth rotation, while low-level laser therapy was not[36].
Finally, Edwards[15] reported that elastic oxytalan fibers, which are prevalent in the free gingival margin and the transseptal areas, increase during orthodontic rotation treatment. However, it is not clear if their numbers remain the same during the relapse phase. Future studies are warranted to investigate this area.
In conclusion, rotational relapse was more frequent in the maxillary arch than in the mandibular arch. Approximately 42% of teeth showed some degree of rotational relapse. Only one tooth had clearly noticeable relapse (≥ 10°). Relapse was most frequent in the maxillary lateral incisors and mandibular canines. Conventional CSF was effective in minimizing rotational relapse when assessed 1 year after the procedure. Proposing a categorical system to evaluate rotational relapse can aid in proper prognosis and decision-making or further orthodontic correction when needed. Future controlled studies with larger sample sizes are warranted to evaluate the present findings.
Prevention of relapse of the dentition to their respective pretreatment positions plays an essential role in the success of orthodontic treatment. Rotated teeth are more susceptible to revert back toward their original positions after removal of the orthodontic appliances compared to teeth displaced in other directions. This might be due to the lack of reorganization and subsequent reorientation of the supra-crestal periodontal fibers and gingival fibers after tooth rotation and retention appear to be torn, ripped, disorganized, laterally spaced, and of increased diameter. Various procedures have been proposed in order to overcome this problem and to reduce this relapse, which include the circumferential supracrestal fiberotomy (CSF) procedure. Very few studies have examined the frequency of rotational relapse in relation to CSF.
There are only a few articles that have addressed the association between CSF and tooth rotation following orthodontic treatment. Few have measured the prevalence of rotational relapse following this approach. This information is essential for patients to understand outcome of treatment as well as to guide orthodontists in the proper management of cases requiring teeth rotation.
The purpose of this study was to assess the amount of relapse following the CSF of the orthodontically derotated anterior teeth and to find out if there is any potential effect of CSF in reducing rotational relapse by measuring the prevalence of relapse in post-CSF orthodontically derotated teeth.
Subjects were recruited who underwent derotational alignment of maxillary and mandibular anterior teeth during orthodontic treatment. The CSF surgery was performed after completion of orthodontic treatment and placement of a fixed retainer. Angles of the rotation correction and relapse were measured on three different set of casts obtained from the patients (pretreatment, post-treatment with retainer, and post-treatment with no retainer). Relapse percentage of each derotated tooth, which results as a post-treatment adverse outcome was calculated and determined from the post-treatment casts. Rotational relapse was categorized as follows: Unnoticeable relapse (0°), barely noticeable relapse (1°-3°), noticeable relapse (4°-9°), and clearly noticeable relapse (≥ 10°). The percent relapse that had occurred 1 year after teeth were aligned to their ideal position was calculated. Data were analyzed by dental arch type and tooth type. Wilcoxon test was used to determine if there were any significant differences between rotational degree angles.
Eleven subjects with a mean age of 23 years old and a total of 90 teeth were included. In regard to frequency of rotational relapse following CSF and retainer placement at the 12 mo follow-up assessment, 57.8% of the teeth maintained their corrected position, and no statistically significant relapse had occurred, which confirms the effectiveness of CSF. When relapse was evaluated and categorized among subjects, overall mean relapse was 1.1° (10.8%). More than half (n = 52, 57.8%) of teeth were categorized as having unnoticeable relapse (0°). Of the remaining teeth, 34.5% (n = 31) had barely noticeable relapse (1°-3°), 6.6% (n = 6) had noticeable relapse (4°-9°), and 1.1% (n = 1) had clearly noticeable relapse (≥ 10°). When analyzed by arch, 54.5% (n = 6) of the relapsed maxillary teeth had barely noticeable relapse (1°-3°), 37.5% (n = 3) of the mandibular teeth had noticeable relapse (4°-9°), and 12.5% (n = 1) had clearly noticeable relapse (≥ 10°).
Minimal amount of rotational relapse was shown after CSF surgery if used in conjunction with an adequate period of post-treatment retention. Thus, CSF surgery is a possible adjunctive treatment modality for minimizing the rotational relapse of the anterior teeth. Furthermore, rotational relapse was more frequent in the maxillary arch than in the mandibular arch. Approximately 42% of teeth showed some degree of rotational relapse. Only one tooth had clearly noticeable relapse (≥ 10°). Relapse was most frequent in the maxillary lateral incisors and mandibular canines. This can be essential when planning for orthodontic rotation of maxillary teeth as it might need an increased amount of rotation compared to mandibular. However, further studies with larger sample sizes and longer follow-up periods are needed to confirm this conclusion.
Identifying post orthodontic rotational relapseâs frequency following fibrotomy can aid in proper prognosis and decision-making or further orthodontic correction when needed. Future controlled studies with larger sample sizes and long follow-ups are warranted to evaluate the present findings.
Authors would like to thank the College of Dentistry Research Center and the Deanship of Scientific Research at King Saud University, Riyadh, Saudi Arabia (CDRC) for all the support provided during this study.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: Saudi Arabia
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Galiatsatos A, Paredes-Vieyra JP S-Editor: Zhang L L-Editor: Filipodia E-Editor: Liu MY
| 1. | Smith RJ, Burstone CJ. Mechanics of tooth movement. Am J Orthod. 1984;85:294-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 180] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 2. | Shpack N, Geron S, Floris I, Davidovitch M, Brosh T, Vardimon AD. Bracket placement in lingual vs labial systems and direct vs indirect bonding. Angle Orthod. 2007;77:509-517. [DOI] [Full Text] |
| 3. | Gupta SK, Saxena P, Jain S, Jain D. Prevalence and distribution of selected developmental dental anomalies in an Indian population. J Oral Sci. 2011;53:231-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 80] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 4. | Naraghi S, Andrén A, Kjellberg H, Mohlin BO. Relapse tendency after orthodontic correction of upper front teeth retained with a bonded retainer. Angle Orthod. 2006;76:570-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 5. | Baccetti T. A controlled study of associated dental anomalies. Angle Orthod. 1998;68:267-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Frank CA. Treatment options for impacted teeth. J Am Dent Assoc. 2000;131:623-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 53] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Isaacson KG, Muir J, Reed RT. Removable orthodontic appliances. Costa Mesa, CA: Wright Publishing Co Inc.; 2003. |
| 8. | Abuabara A, Yoshida AH, Lago JCF. Correction of canine rotation with Box loop. Archives of Oral Research. 2008;4. |
| 9. | Tay WM. Rotated maxillary second premolars two cases with 180 degrees rotation. Br Dent J. 1968;124:326. [PubMed] |
| 10. | Dutta B, Krishnapriya V, Sriram CH, Reddy MK. Surgical Derotation Technique: A Novel Approach in the Management of Rotated Immature Permanent Incisor. Int J Clin Pediatr Dent. 2015;8:220-223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Virk P, Shama U. Management of torsiversion of a tooth secondary to a mesiodens. Ind J Dent Educ. 2011;. |
| 12. | Littlewood SJ, Millett DT, Doubleday B, Bearn DR, Worthington HV. Orthodontic retention: A systematic review. J Orthod. 2006;33:205-212. [RCA] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 77] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 13. | Retain K. Tissue rearrangement during retention of orthodontically rotated teeth. Angle Orthod. 1959;29:105-113. [DOI] [Full Text] |
| 14. | Harris EF. Commentary: Rotated premolars. Dent Anthropol. 2006;19:74-78. |
| 15. | Edwards JG. A long-term prospective evaluation of the circumferential supracrestal fiberotomy in alleviating orthodontic relapse. Am J Orthod Dentofacial Orthop. 1988;93:380-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 101] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Little RM. The irregularity index: a quantitative score of mandibular anterior alignment. Am J Orthod. 1975;68:554-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 522] [Cited by in RCA: 565] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 17. | McNamara JA, Brudon WL, Kokich VG. Orthodontics and dentofacial orthopedics. Needham: Needham Press; 2001. |
| 18. | Gokhale SA, Byakod G, Gupta G, Muglikar S, Gupta S. Effects of laser-aided circumferential supracrestal fiberotomy on relapse of orthodontically treated teeth: A pilot study. J Dent Lasers. 2015;9:16-22. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Jahanbin A, Ramazanzadeh B, Ahrari F, Forouzanfar A, Beidokhti M. Effectiveness of Er: YAG laser-aided fiberotomy and low-level laser therapy in alleviating relapse of rotated incisors. Am J Orthod Dentofacial Orthop. 2014;146:565-572. [RCA] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 20. | Ahrens DG, Shapira Y, Kuftinec MM. An approach to rotational relapse. Am J Orthod. 1981;80:83-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 18] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Swanson WD, Riedel RA, D'Anna JA. Postretention study: incidence and stability of rotated teeth in humans. Angle Orthod. 1975;45:198-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Al-Jasser R, Al-Subaie M, Al-Jasser N, Al-Rasheed A. Rotational relapse of anterior teeth following orthodontic treatment and circumferential supracrestal fiberotomy. The Saudi Dental Journal 2019: In Press. . [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Taner TU, Haydar B, Kavuklu I, Korkmaz A. Short-term effects of fiberotomy on relapse of anterior crowding. Am J Orthod Dentofacial Orthop. 2000;118:617-623. [RCA] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Macauley D, Garvey TM, Dowling AH, Fleming GJP. Using Little’s Irregularity Index in orthodontics: outdated and inaccurate? J Dent. 2012;40:1127-1133. [RCA] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Berg R. Post-retention analysis of treatment problems and failures in 264 consecutively treated cases. Eur J Orthod. 1979;1:55-68. [RCA] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Vaden JL, Harris EF, Gardner RL. Relapse revisited. Am J Orthod Dentofacial Orthop. 1997;111:543-553. [RCA] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 78] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Jones ML. The Barry Project--a further assessment of occlusal treatment change in a consecutive sample: crowding and arch dimensions. Br J Orthod. 1990;17:269-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 28. | Boese LR. Increased stability of orthodontically rotated teeth following gingivectomy in Macaca nemestrina. Am J Orthod. 1969;56:273-290. [RCA] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 48] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 29. | Kalra A, Jaggi N, Bansal M, Goel S, Medsinge SV, Abraham R, Jasoria G. Comparison of rate of canine retraction into recent extraction site with and without gingival fiberotomy: a clinical study. J Contemp Dent Pract. 2013;14:419-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Crum RE, Andreasen GF. The effect of gingival fiber surgery on the retention of rotated teeth. Am J Orthod. 1974;65:626-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Wong K. Orthodontic Rotational Relapse: Prevalence and Prevention. University of Southern California: ProQuest LLC; 2018. |
| 32. | Pinson RR, Strahan JD. The effect on the relapse of orthodontically rotated teeth of surgical division of the gingival fibres--pericision. Br J Orthod. 1974;1:87-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | Proffit W, Fields H. Contemporary Orthodontics. 5th ed. Mosby: Elsevier; 2012; 768. |
| 34. | Fricke LL, Rankine CA. Comparison of electrosurgery with conventional fiberotomies on rotational relapse and gingival tissue in the dog. Am J Orthod Dentofacial Orthop. 1990;97:405-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 35. | Youssef M, Ashkar S, Hamade E, Gutknecht N, Lampert F, Mir M. The effect of low-level laser therapy during orthodontic movement: a preliminary study. Lasers Med Sci. 2008;23:27-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 170] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 36. | Kim SJ, Paek JH, Park KH, Kang SG, Park YG. Laser-aided circumferential supracrestal fiberotomy and low-level laser therapy effects on relapse of rotated teeth in beagles. Angle Orthod. 2010;80:385-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 37. | Miresmæili AF, Mollabashi V, Gholami L, Farhadian M, Rezaei-Soufi L, Javanshir B, Malekshoar M. Comparison of conventional and laser-aided fiberotomy in relapse tendency of rotated tooth: A randomized controlled clinical trial. Int Orthod. 2019;17:103-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |