Published online Oct 6, 2020. doi: 10.12998/wjcc.v8.i19.4550
Peer-review started: May 9, 2020
First decision: May 15, 2020
Revised: May 28, 2020
Accepted: August 25, 2020
Article in press: August 25, 2020
Published online: October 6, 2020
Processing time: 141 Days and 13.2 Hours
Gastro-thoracic fistula is a serious complication after radical surgery for esophageal cancer, and a conservative approach or endoscopic intervention is commonly applied to treat most cases.
Here we describe the case of a patient with a gastro-thoracic fistula which could not be closed during gastroscopy after receiving postoperative radiotherapy, together with severe multiple drug-resistant bacterial infection and chest wall fistula. The abscess was drained and local irrigation applied with ozonated water, together with oral ozonated water, which achieved a good effect and highlighted a new way to cure fistula in such patients.
Patients with gastro-thoracic fistula that cannot be closed and severe infection can be treated by drainage and flushing with ozonated water.
Core Tip: We report a patient whose gastro-thoracic fistula could not be closed surgically following radiotherapy, and who also presented with severe multiple drug-resistance bacterial infection and chest wall fistula. The patient was successfully treated by draining the abscess and applying local irrigation, as well as administering ozonated water orally. This case demonstrates that adequate local drainage and anti-infection treatment can be used to cure patients with severe infection and gastro-thoracic fistula which cannot be closed under endoscopy. As a supplement to conventional therapy, treatment using local irrigation with ozonated water to control infection can heal patients with this condition.
- Citation: Wu DD, Hao KN, Chen XJ, Li XM, He XF. Application of ozonated water for treatment of gastro-thoracic fistula after comprehensive esophageal squamous cell carcinoma therapy: A case report. World J Clin Cases 2020; 8(19): 4550-4557
- URL: https://www.wjgnet.com/2307-8960/full/v8/i19/4550.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i19.4550
The incidence and mortality of esophageal cancer are high in China. Radical surgery is often the first-line treatment option for the majority of patients[1,2]. One type of life-threatening postoperative complication is gastro-thoracic fistula with an incidence of 14.1% worldwide[3,4], which may be associated with body mass index[5]. Effective anti-infection treatment is the key to reducing mortality and improving patient quality of life.
Long-term clinical trials have proven that ozone can both effectively control infections caused by various bacteria, fungi, and viruses[6,7], and promote tissue repair[8]. Here, we report a case of gastro-thoracic fistula after comprehensive treatment for esophageal cancer, complicated by severe thoracic infection, and successfully treated using ozone.
A 50-year-old woman developed an open wound in a surgical incision scar and was readmitted to our hospital on July 31, 2019 because the wound in her left chest wall had reopened.
Following radical esophagectomy in June 2016 to treat esophageal squamous cell carcinoma, in May 2019, the patient developed an open wound in the surgical incision scar on her left chest wall (Figure 1).
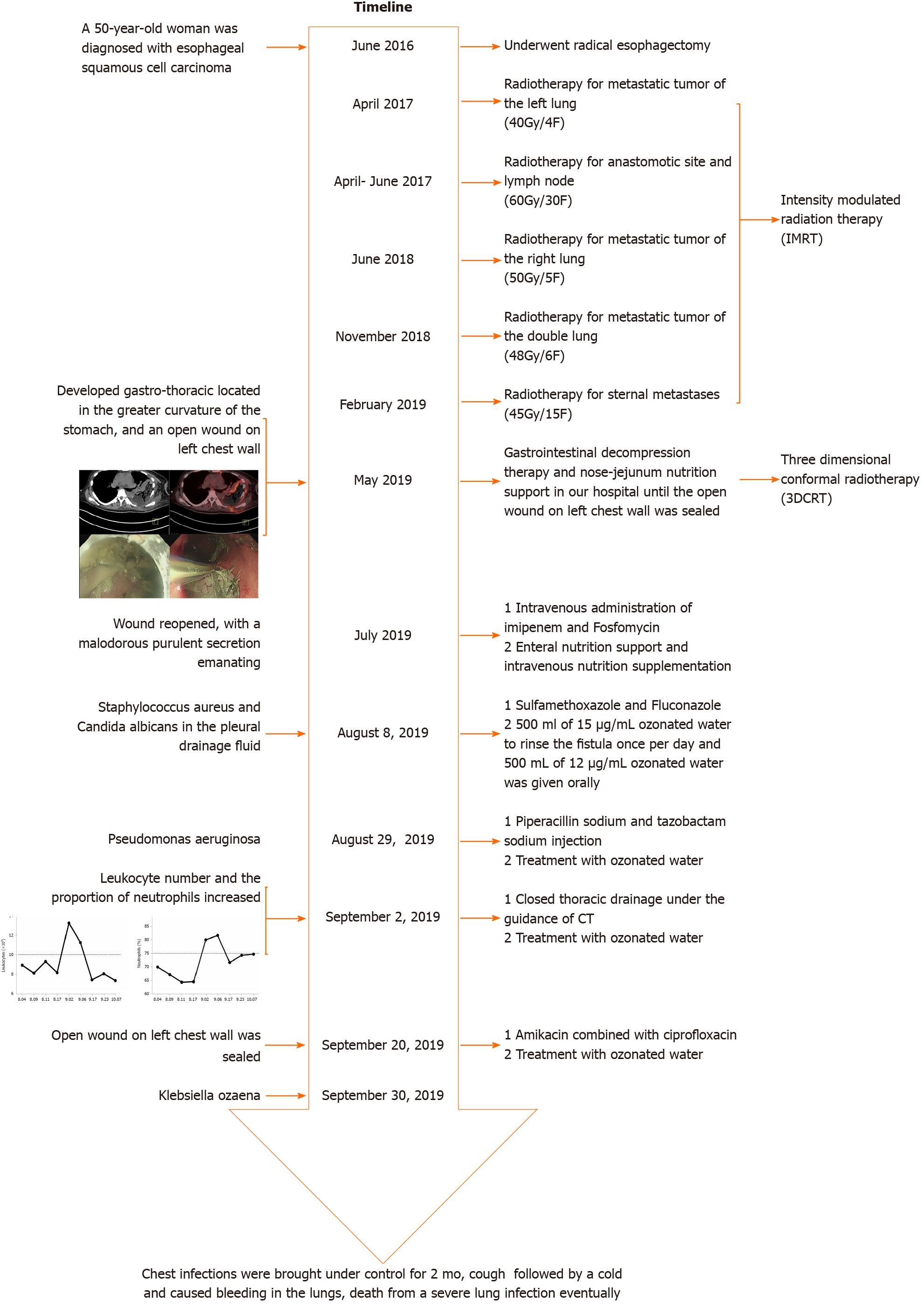
The patient was diagnosed with moderately differentiated esophageal squamous cell carcinoma in 2016. During the 3 years following surgery, the patient received repeated radiotherapy to metastatic tumor of the left lung (40 Gy/4 F), anastomotic site and lymph nodes (60 Gy/30 F), metastatic tumor of the right lung (50 Gy/5 F), metastatic tumors of both lungs (48 Gy/6 F), and sternal metastases (45 Gy/15 F) with time sequence (Figure 2).
When the patient was readmitted to our hospital on July 31, 2019, she was pale and dehydrated on physical examination, and the wound in her left chest wall had reopened, was approximately 2 cm × 3 cm, and had malodorous purulent secretion emanating from it.
Bacterial culture and drug sensitivity testing of the pleural drainage fluid on August 8, 2019 revealed positivity for methicillin-resistant Staphylococcus aureus and Candida albicans. Regular bacterial culture of the pleural abscess drainage fluid indicated that Pseudomonas aeruginosa (August 29) and Klebsiella ozaena (September 30) were present.
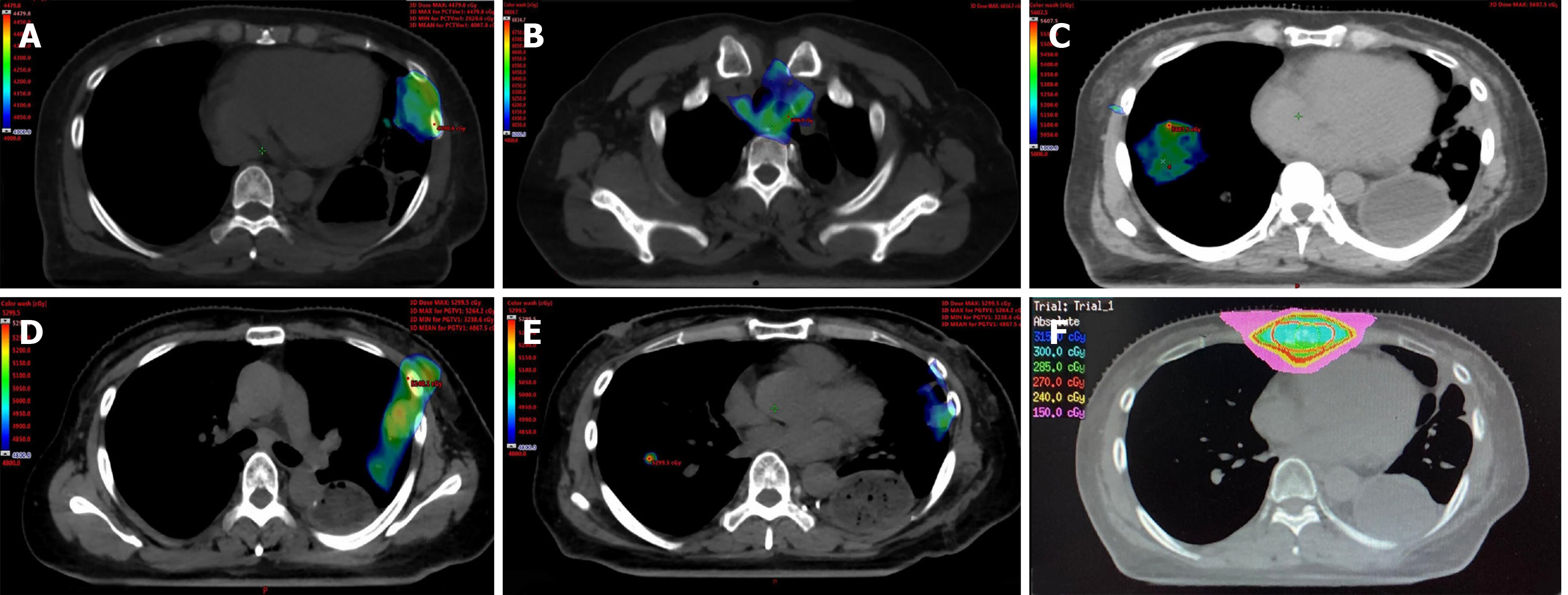
When the patient presented in May 2019, whole body positron emission tomography (PET-CT) indicated the formation of a gastro-thoracic fistula, with lesions involving the lateral chest wall (Figure 3A and B) and active malignancies in the left lung, inferior segment sternotomy, and right lobe of the liver. A gastro-thoracic fistula of approximately 5 cm, located in the greater curvature of the stomach, was confirmed on endoscopy (Figure 3C and D). Poor drainage of the abscess by the drainage tube applied was detected on computed tomography (CT) examination in September 2019.
The patient did not smoke or consume alcohol. Her mother and brother both died of esophageal cancer.
Gastro-thoracic fistula was diagnosed clearly and the fistula is too large to perform reoperation or endoscopic treatment.
The images of PET-CT showed that the gastro-thoracic fistula was complicated with severe infection that was not controlled.
The final diagnosis was gastro-thoracic fistula following comprehensive treatment for squamous cell esophageal carcinoma.
Following detection of the fistula in May 2019, her oral intake was restricted and she received gastrointestinal decompression therapy and nose-jejunum nutrition support at our hospital until the open wound was sealed.
On readmission on July 31, she received intravenous administration of imipenem and fosfomycin to treat the infection and a gastric tube was placed to irrigate the wound. She was also administered metronidazole, enteral nutrition support, and intravenous nutrition supplementation. The open wound at the site of her surgical scar was treated with local empyema and disinfection, and the dressing changed. A jejunal nutrition tube and gastric-thoracic fistula drainage tube were placed on August 7 and saline used to flush the fistula following surgery. Following detection of methicillin-resistant Staphylococcus aureus and Candida albicans on August 8, sulfamethoxazole combined with fluconazole was administered intravenously to control the infection. Next, we began application of 15 µg/mL ozonated water to rinse the fistula once per day (500 mL each time) and administered 12 µg/mL ozonated water orally (500 mL per day) from August 10. Subsequently, following detection of Pseudomonas aeruginosa (August 29) and Klebsiella ozaena (September 30), intravenous antibiotics were adjusted to piperacillin sodium and tazobactam sodium injection (September 4), in addition to amikacin combined with ciprofloxacin (September 30), according to the results of drug sensitivity testing.
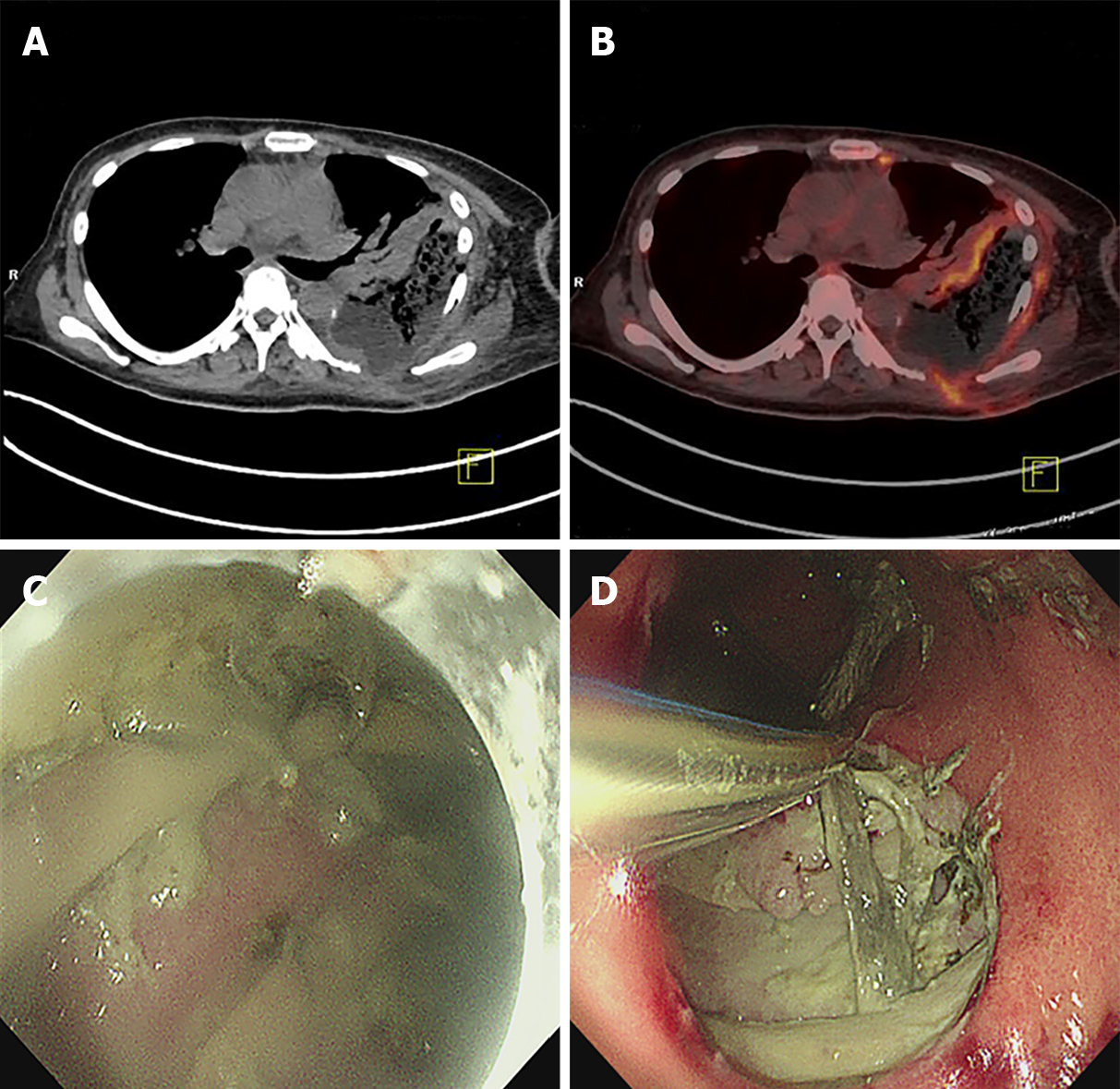
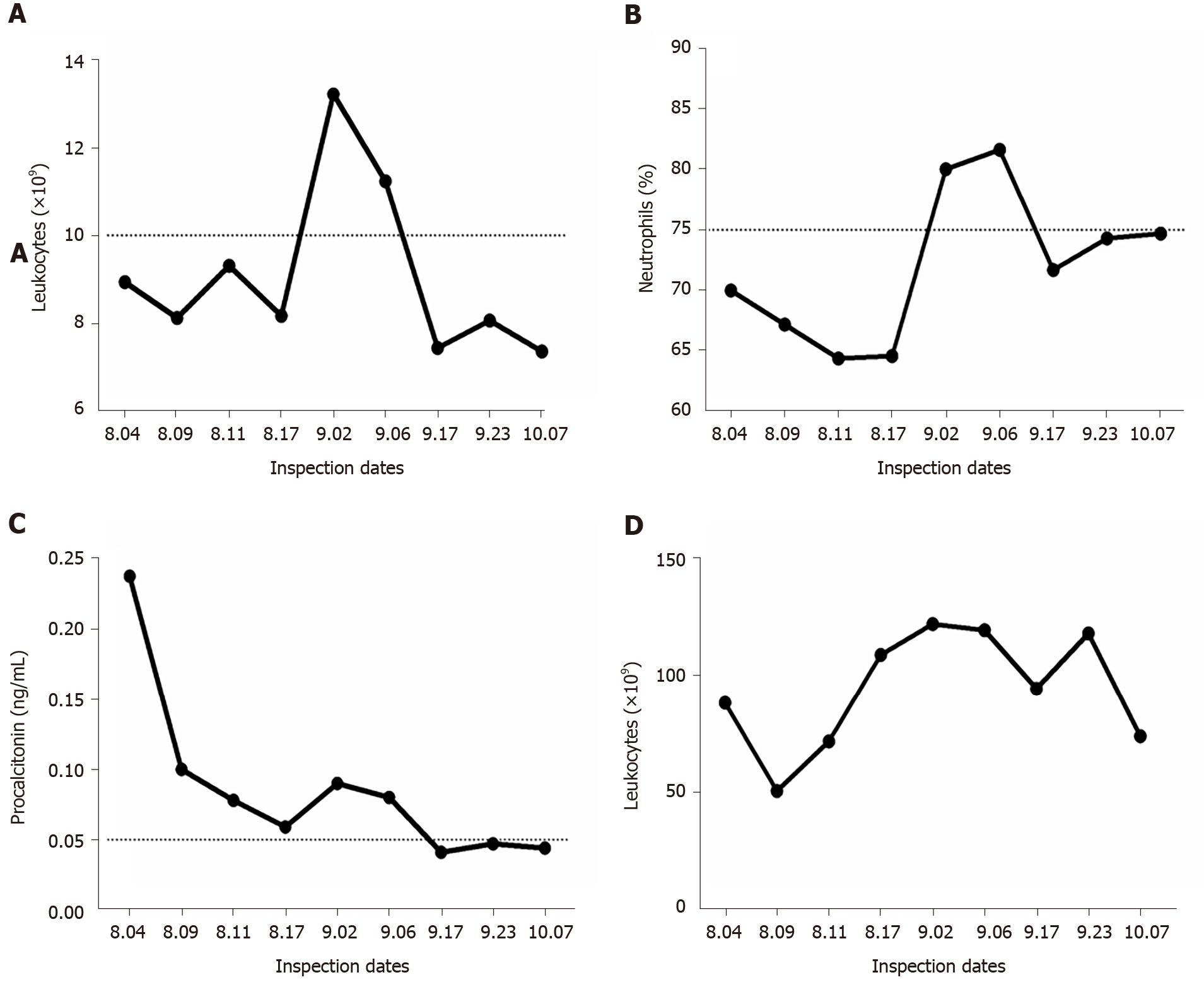
Leukocyte number and the proportion of neutrophils were found to have continued to increase on September 3 (Figure 4A and B), indicating that the infection was unsatisfactorily controlled. On detection of poor abscess drainage, we applied closed thoracic drainage under the guidance of CT on September 10, resulting in drainage of thick, dark red liquid.
The patient then received 2 mo of adequate drainage and rinsing with ozonated water.
The patient’s infection was satisfactorily controlled, leukocyte number and the proportion of neutrophils were subsequently decreased gradually after closed thoracic drainage (Figure 4A and B). Procalcitonin also declined, indicating that related symptoms, including severe bacterial infection and sepsis, were gradually improving (Figure 4C). C-reactive protein levels fluctuated, related to the changes in the underlying disease of the patient, including obstructive pneumonia (Figure 4D).
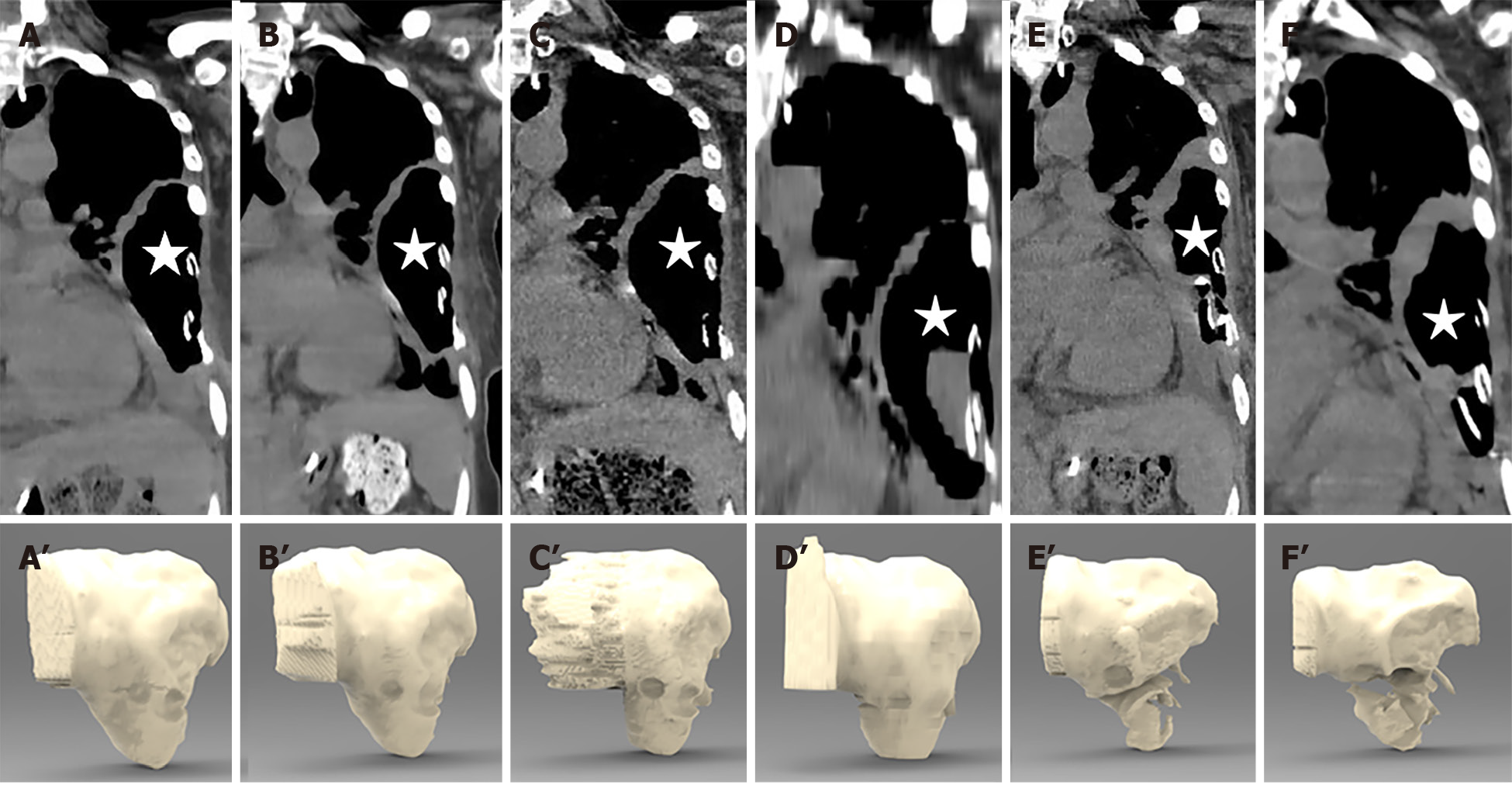
CT examinations during treatment revealed that the wall of the gastro-thoracic fistula gradually thickened (Figure 5A-F). Three-dimensional stereograms of the fistula were reconstructed from CT images using Interactive Medical Image Control System 21 software (Materialise, Belgium). Fistula volumes were measured based on the sum of the voxel volume for the fistula, using ITK-SNAP 3.8.0 (Yushkevich, University of Pennsylvania and Gerig, University of Utah), and were 131, 144, 155, 162, 98, and 96 mL on August 20, August 26, August 30, September 2, September 17, and October 8, respectively (Figure 5A’-F’).
The open wound on her left chest wall was sealed on September 20. She did not complain of chills, fever, or other types of discomfort.
First line treatments for patients with gastro-thoracic fistula generally comprise conservative approaches[9], including restriction of oral intake, infection control, thoracic drainage, and nutritional support. Patients with severe symptoms may also require endoscopic intervention, such as endoscopic clips, fibrin glue, sutures, stents, or a combination of two or more techniques[10,11]; however, due to severe infection and poor physical condition, it is challenging to conduct endoscopic clipping or re-operation for these patients[12,13]. Then, we can use the ozonated water, which has not been reported to be applied in esophageal carcinoma patients with fistula before.
In the case presented here, the gastro-thoracic fistula was located in the greater curvature of the stomach with high tension, combined with brittle local tissue, as a consequence of repeated radiotherapy; hence, endoscopic intervention would have been technically challenging. Furthermore, other conventional conservative approaches, including antibiotic administration, oral intake, and parenteral nutrition, had minimal effect, due to the poor physical condition and severe infection of the patient, which left us with more effective anti-infection therapy and adequate drainage as the crucial options. During treatment of this patient, a thoracic drainage tube was placed in the lowest position in the purulent cavity, rather than through the original higher chest wall fistula, and together with daily flushing with ozonated water, the rupture of the chest wall gradually healed and the chest infection was satisfactorily controlled.
In conclusion, adequate local drainage and anti-infection treatment are likely the best choice to aid survival of patients with gastro-thoracic fistula which cannot be closed under endoscopy and is complicated with severe infection, as in our case. Combined with conventional conservative treatments, the application of local ozonated water irrigation to control infection can promote the healing of a chest wall fistula and improve patient quality of life.
Thanks to Dr. Wang YY for her valuable comments on the logic and writing of the paper, and to Dr. Sun JY and Dr. Cao CH for their assistance in checking and verifying the radiotherapy plan and radiation dose.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: World Federation of Ozone Therapy.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chien CR S-Editor: Gong ZM L-Editor: Wang TQ E-Editor: Li X
| 1. | Uzunoglu FG, Reeh M, Kutup A, Izbicki JR. Surgery of esophageal cancer. Langenbecks Arch Surg. 2013;398:189-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Lu D, Liu X, Li M, Feng S, Dong X, Yu X, Wu H, Xiong G, Cai R, Li G, Cai K. Three-port mediastino-laparoscopic esophagectomy (TPMLE) for an 81-year-old female with early-staged esophageal cancer: a case report of combining single-port mediastinoscopic esophagectomy and reduced port laparoscopic surgery. J Thorac Dis. 2018;10:E378-E382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Turkyilmaz A, Eroglu A, Aydin Y, Tekinbas C, Muharrem Erol M, Karaoglanoglu N. The management of esophagogastric anastomotic leak after esophagectomy for esophageal carcinoma. Dis Esophagus. 2009;22:119-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 106] [Article Influence: 6.2] [Reference Citation Analysis (1)] |
| 4. | Birla R, Hoara P, Dinu D, Rosianu C, Constantinoiu S. Postoperative Esophageal Leaks in Malignant Pathology - Optimal Management: A Systematic Review. Chirurgia (Bucur). 2019;114:429-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Zhang SS, Yang H, Luo KJ, Huang QY, Chen JY, Yang F, Cai XL, Xie X, Liu QW, Bella AE, Hu RG, Wen J, Hu Y, Fu JH. The impact of body mass index on complication and survival in resected oesophageal cancer: a clinical-based cohort and meta-analysis. Br J Cancer. 2013;109:2894-2903. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 120] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 6. | Souza YM, Fontes B, Martins JO, Sannomiya P, Brito GS, Younes RN, Rasslan S. Evaluation of the effects of ozone therapy in the treatment of intra-abdominal infection in rats. Clinics (Sao Paulo). 2010;65:195-202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Song M, Zeng Q, Xiang Y, Gao L, Huang J, Huang J, Wu K, Lu J. The antibacterial effect of topical ozone on the treatment of MRSA skin infection. Mol Med Rep. 2018;17:2449-2455. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 8. | Hao K, Li Y, Feng J, Zhang W, Zhang Y, Ma N, Zeng Q, Pang H, Wang C, Xiao L, He X. Ozone promotes regeneration by regulating the inflammatory response in zebrafish. Int Immunopharmacol. 2015;28:369-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Dehn TC, Menon K. Diagnosis and conservative management of intrathoracic leakage after oesophagectomy. Br J Surg. 1999;86:427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Shen SS, Zhang XQ, Li ZL, Zou XP, Ling TS. Over-the-scope clip to close a gastrocutaneous fistula after esophagectomy. World J Gastroenterol. 2015;21:13396-13399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Kumar N, Thompson CC. Endoscopic therapy for postoperative leaks and fistulae. Gastrointest Endosc Clin N Am. 2013;23:123-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (1)] |
| 12. | Guo J, Chu X, Liu Y, Zhou N, Ma Y, Liang C. Choice of therapeutic strategies in intrathoracic anastomotic leak following esophagectomy. World J Surg Oncol. 2014;12:402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Lee DH, Kim HR, Kim SR, Kim YH, Kim DK, Park SI. Comparison of clinical outcomes after conservative and surgical treatment of isolated anastomotic leaks after esophagectomy for esophageal cancer. Dis Esophagus. 2013;26:609-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |