Published online Aug 6, 2020. doi: 10.12998/wjcc.v8.i15.3314
Peer-review started: April 2, 2020
First decision: April 29, 2020
Revised: May 1, 2020
Accepted: July 15, 2020
Article in press: July 15, 2020
Published online: August 6, 2020
Processing time: 125 Days and 21 Hours
Adult duodenal intussusception rarely occurs, and the majority of duodenal adenomas are located in the descending part of the duodenum. Therefore, adenomas in the horizontal part of the duodenum presenting as duodenal intussusception in adults are extremely rare.
A 36-year-old man complained of abdominal pain for 13 d. Blood analysis showed anemia. Magnetic resonance cholangiopancreatography and computed tomography revealed a tumor in the horizontal part of the duodenum as the main finding, leading to duodeno-duodenal intussusception. No obvious abnormalities were found on endoscopy or upper gastrointestinal radiography. He was diagnosed with duodenal intussusception secondary to duodenal adenoma. Laparotomy showed duodeno-duodenal intussusception and a tumor in the horizontal part of the duodenum near the ascending part. Postoperative pathology revealed tubular-villous adenoma with low-grade glandular intraepithelial neoplasia (local high-grade intraepithelial neoplasia). He was discharged without complications.
This case highlights that rational use of computed tomography, magnetic resonance cholangiopancreatography, endoscopy and upper gastrointestinal radiography for preoperative diagnosis and timely surgery is an effective strategy for the treatment of adult duodenal intussusception with duodenal masses.
Core tip: Adult duodenal intussusception is a challenging disease because of its extremely rare occurrence and nonspecific clinical manifestation, and the differential diagnosis should include digestive tract obstruction and pancreatitis. Here, we present a case of adult duodeno-duodenal intussusception with horizontal adenoma near the ascending part of the duodenum to elucidate and review the pathogenesis, presentation, diagnosis and consensus recommendations of duodenal intussusception. This case highlights the rational use of computed tomography, magnetic resonance cholangiopancreatography, endoscopy and upper gastrointestinal radiography for preoperative diagnosis. Timely surgery is an effective strategy for the treatment of adult duodenal intussusception with duodenal masses.
- Citation: Wang KP, Jiang H, Kong C, Wang LZ, Wang GY, Mo JG, Jin C. Adult duodenal intussusception with horizontal adenoma: A rare case report. World J Clin Cases 2020; 8(15): 3314-3319
- URL: https://www.wjgnet.com/2307-8960/full/v8/i15/3314.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i15.3314
Intussusception is not common in adults. Duodenal intussusception rarely occurs because the duodenum is relatively fixed in the retroperitoneum[1]. However, its occurrence is usually secondary to malrotational abnormalities[2] and to benign or malignant tumors of the duodenum, such as hamartoma, adenoma and stromal tumors[3]. It has been reported that 88% of duodenal adenomas are located in the descending part of the duodenum, and adenomas located in the horizontal part of the duodenum are rare[4]. Therefore, adenomas in the horizontal part of the duodenum presenting as duodenal intussusception in adults are extremely rare. Here, we present a case of adult duodeno-duodenal intussusception with horizontal adenoma near the ascending part of the duodenum to elucidate and review the pathogenesis, presentation, diagnosis and consensus recommendations of duodenal intussusception.
A 36-year-old man presented to the general surgery clinic of our hospital complaining of abdominal pain for 13 d.
The patient’s symptoms started 13 d ago and were characterized by persistent dull pain in the upper abdomen; the symptoms had been relieved after symptomatic treatment in a local hospital. However, abdominal pain occurred again 1 d ago, and the symptoms were the same as previously experienced.
The patient had no previous medical history.
The patient’s temperature was 36.8 °C, heart rate was 87 bpm, respiratory rate was 18 breaths per minute and blood pressure was 122/76 mmHg. Anemia signs and slight tenderness in the upper abdomen were observed, and there were no other typical pathological signs. Our first clinical considerations for the abdominal pain were as follows: Space-occupying lesions of the small intestine (possible stromal tumor), followed by possible choledocholithiasis.
Blood analysis showed a hemoglobin level of 75 g/L (normal range > 120 g/L) with a normal leukocytosis level and platelet count. The prothrombin and partial thromboplastin times, the serum C-reactive protein level and the blood biochemistry and urine analyses were normal. The electrocardiogram and chest x-ray results were also normal.
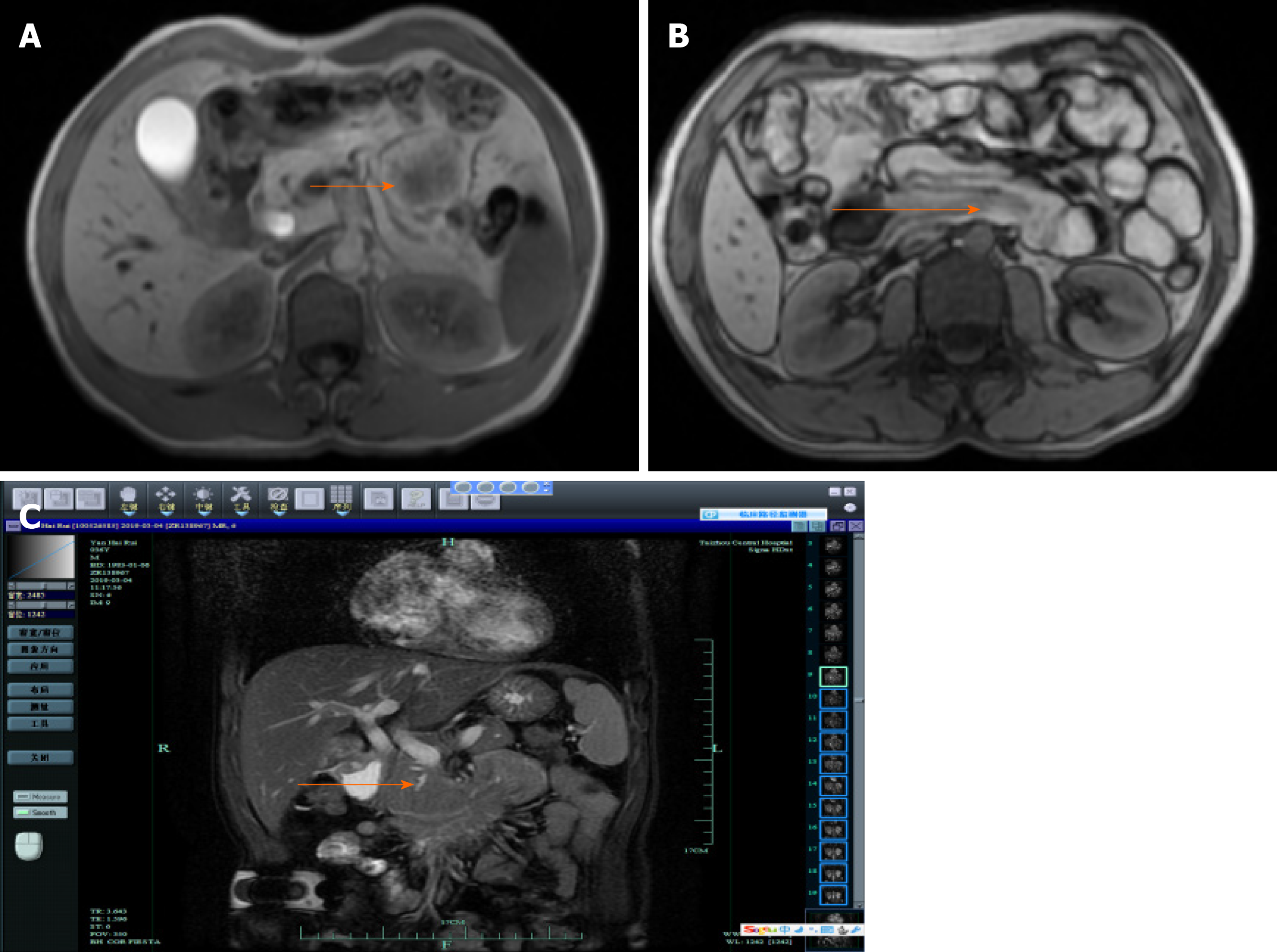
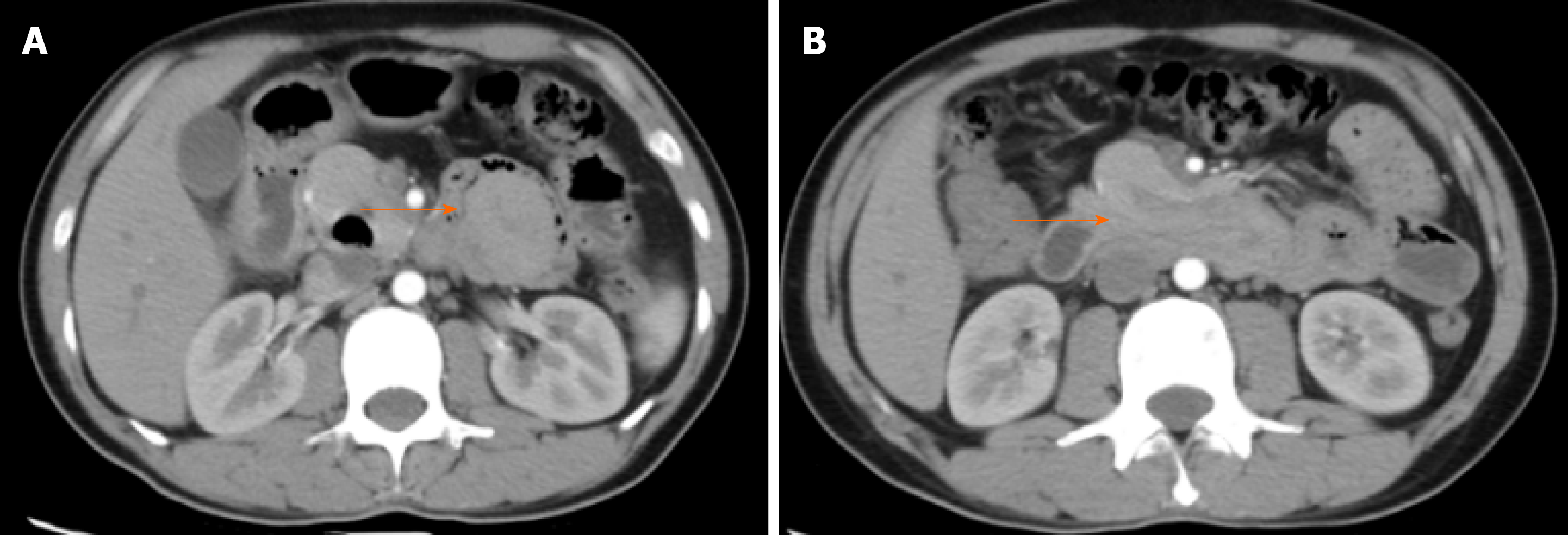
Magnetic resonance cholangiopancreatography (MRCP) revealed an abnormal mass signal in the distal duodenum with proximal intussusception (Figure 1). An abdominal enhanced computed tomography (CT) scan suggested gallstones in the lower part of the common bile duct, mild dilatation of the main pancreatic duct, a slightly disordered horizontal structure of the duodenum and a suspicious space occupying the ascending part of the duodenum with proximal duodenal intussusception (Figure 2A). A space occupying stromal tumor was considered, and the tumor boundary was clear (Figure 2B). Upper gastrointestinal radiography revealed that the duodenal bulb was adequately filled, the descending part of the duodenum was tortuous and long, the distal end was filled and passed well and there were no signs of obstruction. Gastroscopy revealed a 0.6 cm × 0.5 cm ulcer in the anterior wall of the duodenal bulb, and no abnormality was found in the descending part of the duodenum.
The final diagnosis was duodenal adenoma with duodenal intussusception.
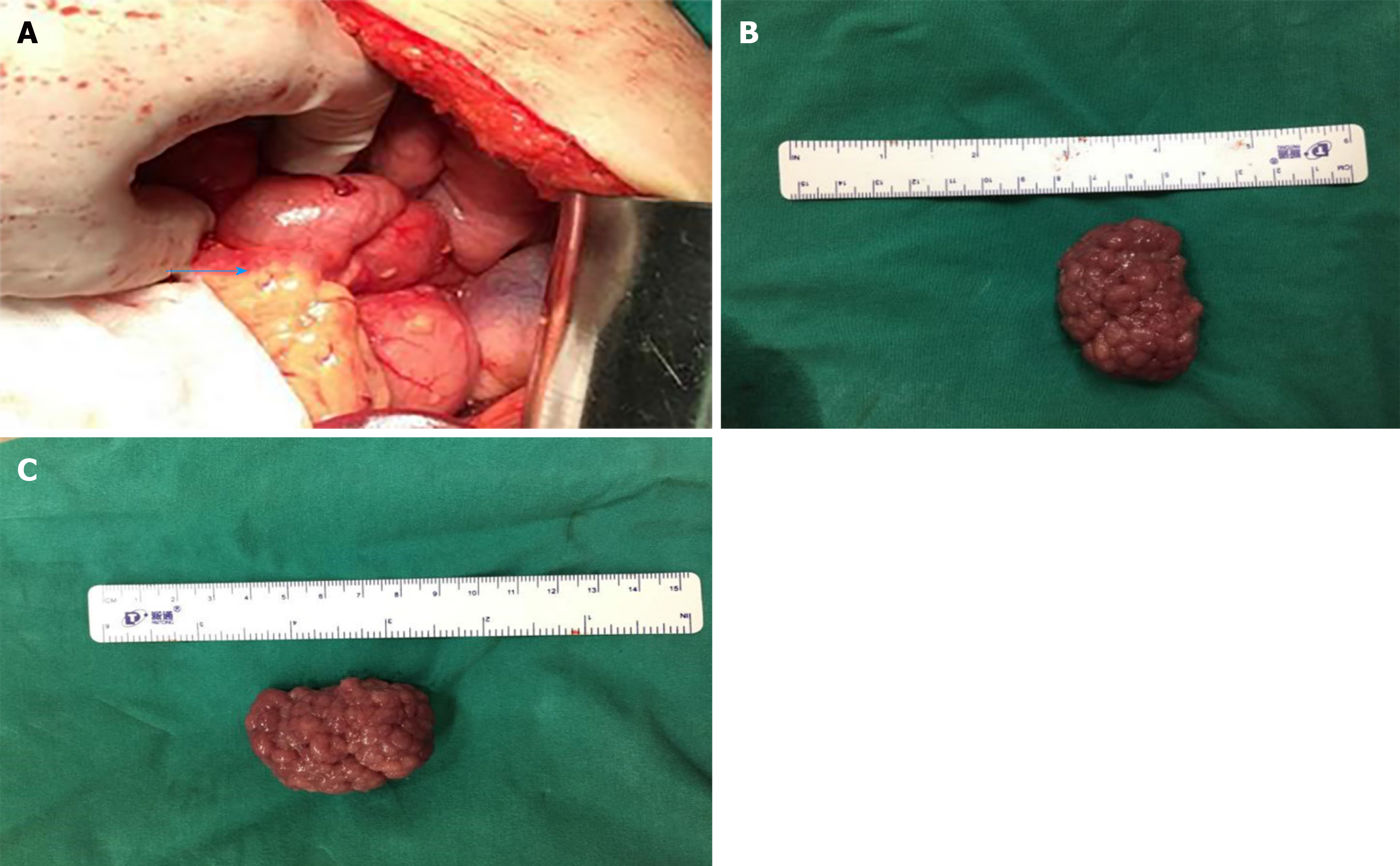
After symptomatic support treatment, such as fasting, rehydration and stomach protection, the patient's abdominal pain was relieved, and exploratory laparotomy was performed. It was found that the ascending part of the duodenum inserted into the junction of the horizontal part of the duodenum and the descending part (Figure 3A). At the intussusception, the intestinal wall was cut open and there was a pedicled tumor in the horizontal part of the duodenum near the ascending part. The tumor was approximately 5.0 cm × 3.5 cm (Figure 3B and C). Complete resection of the mass 1 cm from the edge of the tumor and rapid intraoperative frozen sections revealed tubular-villous adenoma with low-grade glandular epithelial intraepithelial neoplasia (partial moderate dysplasia). Intestinal anastomosis was performed, and a jejunal nutrition tube was placed to end the operation. After the operation, the patient was given symptomatic support treatment, such as liver protection, stomach protection and fluid replacement.
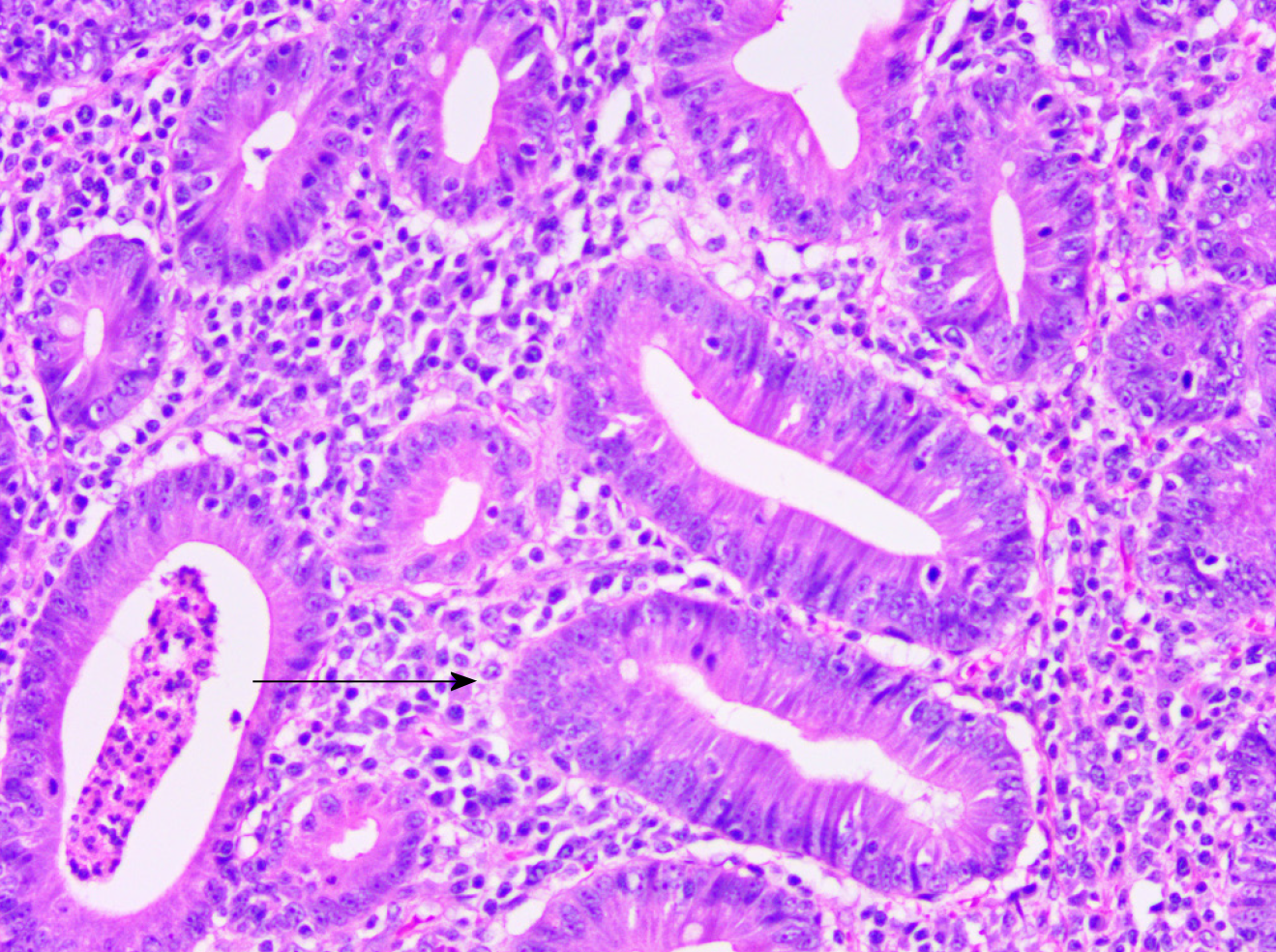
Postoperative routine pathology revealed tubular-villous adenoma with low-grade glandular intraepithelial neoplasia (local high-grade intraepithelial neoplasia) (Figure 4). On the 12th d after the operation, the patient fully recovered and was discharged from the hospital. The patient was followed for 1 year, and there was no recurrence.
Duodenal intussusception is a critical condition in which the proximal duodenum protrudes into the distal duodenum[5]. It has been reported that duodenal intussus-ception tends to occur more frequently in adult female patients[6]. However, there are no statistical data regarding its epidemiology.
An unknown topic is the elucidation of the mechanism of duodenal intussusception. It is widely recognized that malrotational abnormalities and duodenal space occupation are the main causes of duodenal intussusception in adults[1,2,7]. There are also rare cases of duodenal ulcers as the main finding, resulting in duodenal intussusception[5]. In cases of nonrotational abnormalities, tumors, polyps and ulcers are the lead point, which represents the main pathogenesis of duodenal intussusception. In this case report, a horizontal adenoma near the ascending part of the duodenum was the main finding, which led to duodeno-duodenal intussusception, and no malrotational abnormalities were found. The pathogenesis likely involves the adenoma near the ascending part of the duodenum as the lead point, whereby the enveloping mucosa is elongated, resulting in a mucosal stalk, as a tumor migrates distally by peristalsis. While the tumor migrates more distally, the wall of the descending part of the duodenum and the horizontal part of the duodenum become deformed[1].
The clinical manifestation of duodenal intussusception is nonspecific, and there are usually symptoms of acute, chronic or intermittent intestinal obstruction[8]. Some patients may also present with anemia, low fever, bloody stool, weight loss or even abdominal lumps[6]. When the intussusception affects the hepatopancreatic ampulla, patients may experience symptoms associated with the common bile duct and pancreatic duct obstruction, and patients with duodenal intussusception can present with obstructive jaundice or acute or chronic pancreatitis[3,9]. In our case, the patient had symptoms of abdominal pain, but it was relieved after conservative treatment. No obvious abnormality was found on upper gastrointestinal radiography before the operation, probably because the duodenal adenoma did not cause complete intestinal obstruction, so there was no intestinal necrosis. Moreover, imaging examination demonstrated mild dilatation of the main pancreatic duct and common bile duct, but no stones or masses were found in the lower segment of the common bile duct during the operation, which may be related to the influence of adenoma and intussusception on the opening of the duodenal papilla.
CT seems to be the most reliable method of investigation for making a preoperative diagnosis[10]. However, distal metastasis of duodenal tumors is sometimes difficult to differentiate from true duodenal intussusception with imaging. This phenomenon was introduced as mucosal prolapse[1]. Therefore, there may be misdiagnosis with CT before surgery. Endoscopy is of good value in the diagnosis of duodenal intussusception caused by lesions above the horizontal part of the duodenum. In our case, because the adenoma was located in the horizontal part of the duodenum near the ascending part of the duodenum, no abnormality was found with preoperative endoscopy. MRCP is also a necessary preoperative examination when there are abnormal manifestations of the pancreaticobiliary duct system. Upper gastrointestinal radiography is also important in the diagnosis of duodenal intussusception with intestinal obstruction. In short, the final diagnosis of duodenal adenoma with duodenal intussusception may only be made during surgery and confirmed histopathologically.
It is generally believed that adult duodenal intussusception should be treated by surgery without delay[10]. The surgical procedures used for duodenal intussusception include endoscopic resection and laparotomy or laparoscopy. Only in cases where the lesions of the duodenum are limited to the mucous layer and where the extent of the lesions is less than 2 cm can endoscopic resection be performed. When the lesion exceeds the mucous layer and the range is more than 2 cm, surgical resection is recommended[9]. In addition, in regard to idiopathic intussusception, simple reduction is recommended after excluding intestinal ischemic necrosis and intestinal perforation[9]. The choice of operation depends on the situation observed during the operation. The presence of a malignant tumor or the complete resection of the tumor will affect the function of the ampulla, and pancreaticoduodenectomy may be an appropriate choice[1]. In our case, due to the rapid intraoperative frozen sections revealing tubular-villous adenoma with low-grade glandular epithelial intraepithelial neoplasia (partial moderate dysplasia), pancreaticoduodenectomy was not performed.
Duodenal intussusception is a challenging disease because of its extremely rare occurrence and nonspecific clinical manifestation. The differential diagnosis should include digestive tract obstruction and pancreatitis. Rational use of CT, MRCP, endoscopy and upper gastrointestinal radiography for preoperative diagnosis and timely surgery is an effective strategy for the treatment of duodenal intussusception with duodenal masses.
We are very grateful to our colleagues for providing the pictures.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Member of Minimally Invasive Surgery Branch of Zhejiang Physicians Association; Youth Member of General Surgery Branch of Zhejiang Society of Integrated Traditional Chinese and Western Medicine.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mungazi SG S-Editor: Ma YJ L-Editor: Filipodia E-Editor: Xing YX
| 1. | Hirata M, Shirakata Y, Yamanaka K. Duodenal intussusception secondary to ampullary adenoma: A case report. World J Clin Cases. 2019;7:1857-1864. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Gardner-Thorpe J, Hardwick RH, Carroll NR, Gibbs P, Jamieson NV, Praseedom RK. Adult duodenal intussusception associated with congenital malrotation. World J Gastroenterol. 2007;13:3892-3894. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Watanabe F, Noda H, Okamura J, Toyama N, Konishi F. Acute pancreatitis secondary to duodenoduodenal intussusception in duodenal adenoma. Case Rep Gastroenterol. 2012;6:143-149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Chappuis CW, Divincenti FC, Cohn I. Villous tumors of the duodenum. Ann Surg. 1989;209:593-8; discussion 598-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 52] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Lingala S, Moore A, Kadire S, Shankar S, Das K, Howden CW. Unusual Presentation of Duodenal Ulcer Presenting with Duodenal Intussusception. ACG Case Rep J. 2018;5:e25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Pradhan D, Kaur N, Nagi B. Duodenoduodenal intussusception: Report of three challenging cases with literature review. J Cancer Res Ther. 2015;11:1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Desai G, Yadav K, Pande P, Sali P, Tampi C, Wagle P. Brunner gland adenoma masquerading as duodenal gastrointestinal stromal tumor with intussusception: case report. Arq Bras Cir Dig. 2017;30:71-72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Singhal M, Kang M, Narayanan S, Gupta R, Wig JD, Bal A. Duodenoduodenal intussusception. J Gastrointest Surg. 2009;13:386-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Limi L, Liew NC, Badrul RH, Faisal MJ, Daniel YP. Duodenal intussusception of Brunner's gland adenoma mimicking a pancreatic tumour. Med J Malaysia. 2010;65:311-312. [PubMed] |
| 10. | Loo GH, Mohamad Abu Zeid WM, Lim SL, Ismail AM. Rare presentation of idiopathic duodenoduodenal intussusception. Ann R Coll Surg Engl. 2017;99:e188-e190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |