Published online Aug 6, 2020. doi: 10.12998/wjcc.v8.i15.3299
Peer-review started: March 21, 2020
First decision: April 24, 2020
Revised: April 30, 2020
Accepted: July 15, 2020
Article in press: July 15, 2020
Published online: August 6, 2020
Processing time: 124 Days and 8.2 Hours
Hypothyroidism is an endocrine disorder that has worldwide prevalence and can affect multiple organ systems. We report a case of hypothyroidism with elevated pancreatic amylase and trypsin without acute pancreatitis. No such case has been previously reported.
A 29-year-old woman did not pay much attention to a fever 4 d prior. During this time, she experienced anorexia and only drank a small amount of water every day. She did not present with abdominal distension, postprandial nausea, vomiting, cough or expectoration. After physical and laboratory examinations, the patient was diagnosed with hypothyroidism. During the course of the disease, hypothyroidism was generally accompanied by constantly increased pancreatic amylase and trypsin. After admission, the possible etiology of the patient was excluded and the concentrations of pancreatic lipase and amylase in serum were > 2000U/L (reference range 23-300 U/L) and 410 U/L (reference range 30-110 U/L), respectively. So we highly suspected that it may be acute pancreatitis. Interestingly, she never developed any complications associated with acute pancreatitis despite high levels of serum pancreatic amylase and trypsin, and she reported no symptoms of abdominal pain. Serum amylase and lipase decreased gradually after active thyroxine supplementation, and the patient was discharged from the hospital after active treatment.
This case suggests that clinicians should pay attention to hypothyroidism with elevated pancreatic amylase and trypsin, even if no complications of acute pancreatitis are reported.
Core tip: Hypothyroidism is an endocrine disorder that has worldwide prevalence and can affect multiple organ systems. However, even when pancreatic amylase and lipase are elevated, hypothyroidism without acute pancreatitis rarely causes clinical symptoms. Here, we report a case of hypothyroidism leading to elevated trypsin without acute pancreatitis in a patient who had no clinical symptoms. This case report can serve as a reminder to gastroenterologists, emergency physicians, and surgeons who encounter these cases in clinical practice.
- Citation: Xu YW, Li R, Xu SC. Hypothyroidism with elevated pancreatic amylase and lipase without clinical symptoms: A case report. World J Clin Cases 2020; 8(15): 3299-3304
- URL: https://www.wjgnet.com/2307-8960/full/v8/i15/3299.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i15.3299
Hypothyroidism is one of the most common endocrine disorders, affecting as much as 10% of the global population[1]. Hypothyroidism is the result of an insufficient amount of circulating thyroid hormones; thus, it can affect multiple systems[2]. In primary hypothyroidism, due to thyroid gland failure, serum thyroid hormone levels, including circulating levels of serum total thyroxine (T4) and free (FT4) thyroxine, total (T3) and free (FT3) triiodothyronine, decrease below the lower limit of the reference range, and pituitary thyrotropin (TSH) levels are elevated due to lack of feed-back inhibition the relationship of the hypothalamic-pituitary-thyroid axis. Therefore, the diagnosis of hypothyroidism is mainly based on serum parameters.
Thyroid hormones play an important role in the body and affect every organ system. The symptoms of hypothyroidism are not only nonspecific but also overlap with complaints of normal healthy people[3]. The thyroid is an important endocrine organ in the body. The secretion of thyroid hormone can regulate the metabolism of sugar, protein, and fat in the human body; affect the growth and development of the body; and to some extent affect nervous, endocrine, cardiovascular and reproductive system functioning in the body. Hypothyroidism leads to decrease in the secretion of thyroid hormones, which loses the feedback effect of thyrotropin-releasing hormone (TRH) inhibition, causing thyroid epithelial cells to proliferate, leading to thyroid enlargement. This is a common clinical phenomenon. Of course, there are some rare phenomena. Hypothyroidism can be accompanied by pericardial effusion and pleural effusion in the cardiovascular system. It also leads to anorexia, abdominal distention of the digestive system, female menorrhagia, chronic amenorrhea, male impotence, and decreased libido. Hypothyroidism can also lead to elevated serum pancreatic amylase and trypsin without acute pancreatitis; however, there have been no previous reports on this phenomenon.
A 29-year-old woman was admitted to our hospital with anorexia, nausea, vomiting, apathy, and chills.
A young woman with anorexia, nausea, vomiting, apathy, chills, and fever drank plenty of water at home and did not take her symptoms seriously. However, her temperature did not decrease. Moreover, her fatigue was aggravated, and she started experiencing chest pain. Then the patient was admitted to our hospital.
She denied hepatitis, metabolic disorders, heart disease, cerebrovascular disease, mental illness, and immunodeficiency diseases.
The patient was married and had two sons and one daughter. Her menstrual cycle was regular, the menstrual quantity was moderate, and the color was normal. No additional family history was obtained.
Physical examination after admission showed that the patient’s body temperature was 39.8 °C, her respiratory rate was 20 breaths per min, and her blood pressure was 75/72 mmHg. The results of general physical examination were not good, and she was in poor spirits and expressionless. The patient’s sclera were not stained yellow, and superficial lymph nodes were not enlarged. However, after a physical examination of the patient’s thyroid, it was not an obvious goiter, and maybe only a Grade 1 goiter. This was because the patient's condition was short and the time frame was short, so the patient's goiter did not show. An abdominal examination showed that her abdomen was flat and soft, and there was no obvious tenderness in her abdomen.
After admission to the hospital, the patient underwent a routine blood test (white blood cell count of 7.54 × 109/L, reference range 3.5 × 109/L-9.5 × 109/L; neutrophil count of 9.5 × 109/L, reference range 1.8 × 109/L-6.3 × 109/L; pancreatic amylase at 33 U/L, reference range 30-110 U/L and lipase at 363 U/L, reference range 23-300 U/L). The serum concentrations of TSH (0.09 mIU/L, reference range 0.3-5.5 mIU/L), total thyroxine (TT4 64.9 nmol/L, reference range 58.1-140.6 nmol/L, and free thyroxine FT4 10.06 pmol/L, reference range 11.5-22.7 pmol/L), and total triiodothyronine (TT3 0.63 nmol/L, reference range 0.92-2.79 nmol/L, and free FT3 1.04 pmol/L, reference range 0.92-2.79 pmol/L) were measured. The results of these tests were measured on the first day after the patient was admitted to the hospital. After treatment, the results were significantly improved (Table 1).
| Parameter | Second day ofadmission | Sixth day ofadmission | tenth day ofadmission | Reference ranges |
| Total thyroxine, TT4 | 64.9 | 62.4 | 79.4 | 58.1-140.6 nmol/L |
| Free thyroxine, FT4 | 10.06 | 10.7 | 11.4 | 11.5-22.7 pmol/L |
| Total triiodothyronine, TT3 | 0.63 | 0.59 | 0.86 | 0.92-2.79 nmol/L |
| Free triiodothyronine, FT3 | 1.04 | 2.05 | 2.21 | 0.92-2.79 pmol/L |
| Thyrotropin, thyroid stimulating hormone, TSH | 0.09 | 0.03 | 0.77 | 0.3-5.5 mIU/L |
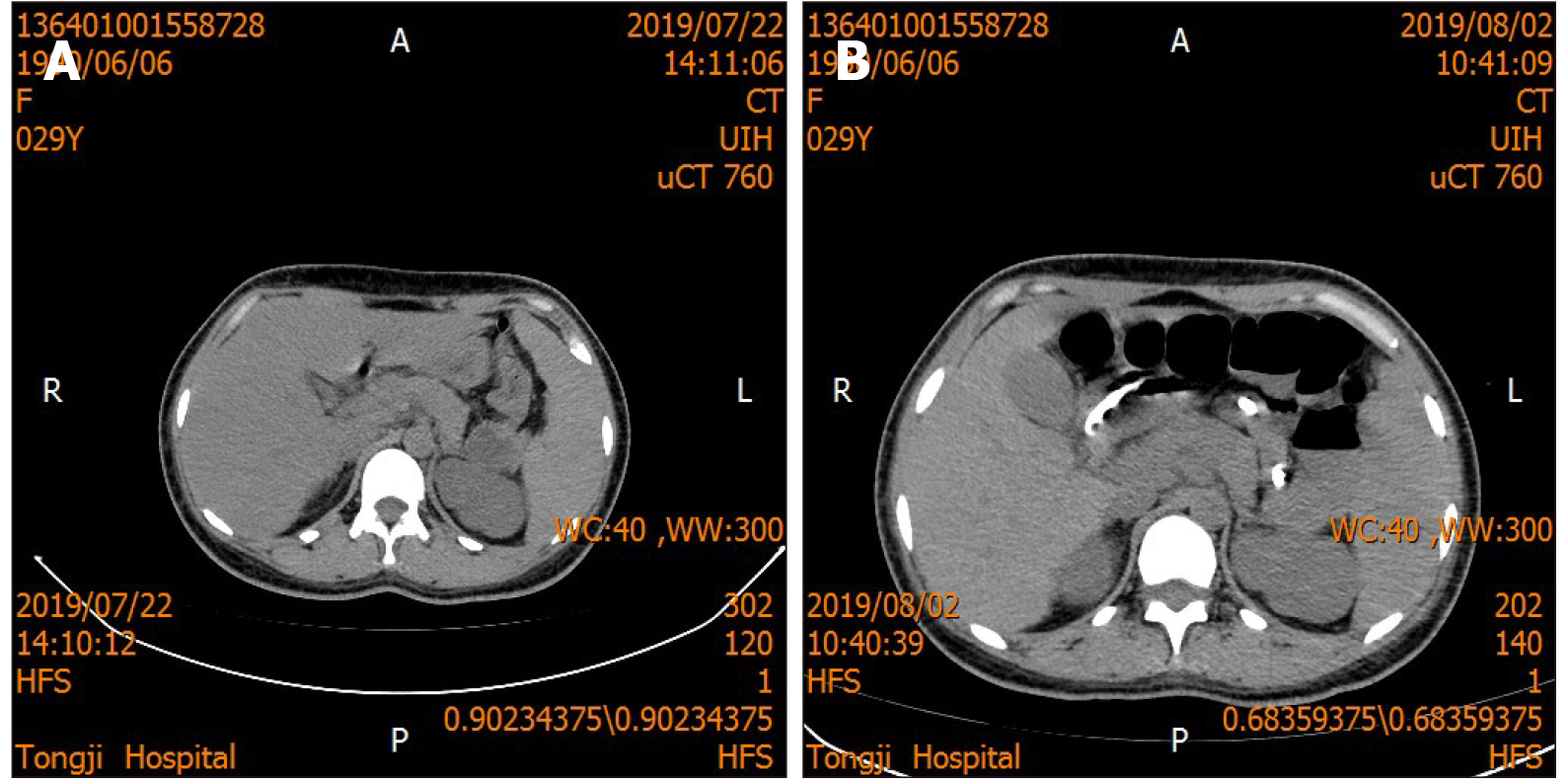
The patient was examined after admission, and a computed tomography (CT) scan of the chest showed no obvious abnormalities. The abdominal CT scan showed a small kidney stone in the left kidney, hepatic adipose infiltration and a small amount of ascites. Abdominal imaging indicated no acute pancreatitis. There was no significant difference between the results after treatment and the results before treatment (Figure 1).
The patient was diagnosed with septic shock, multiple organ dysfunction syndrome, and hypothyroidism.
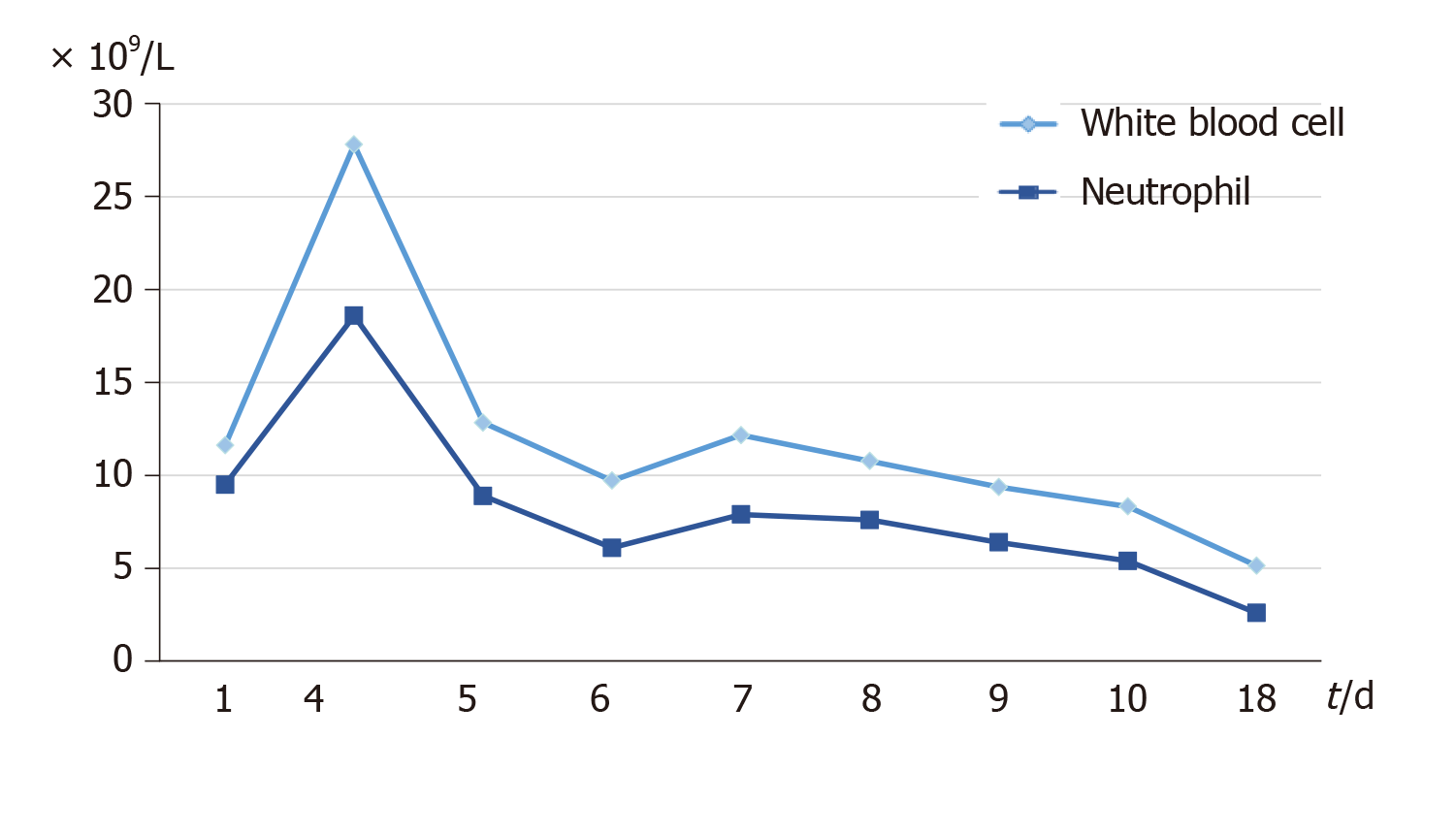
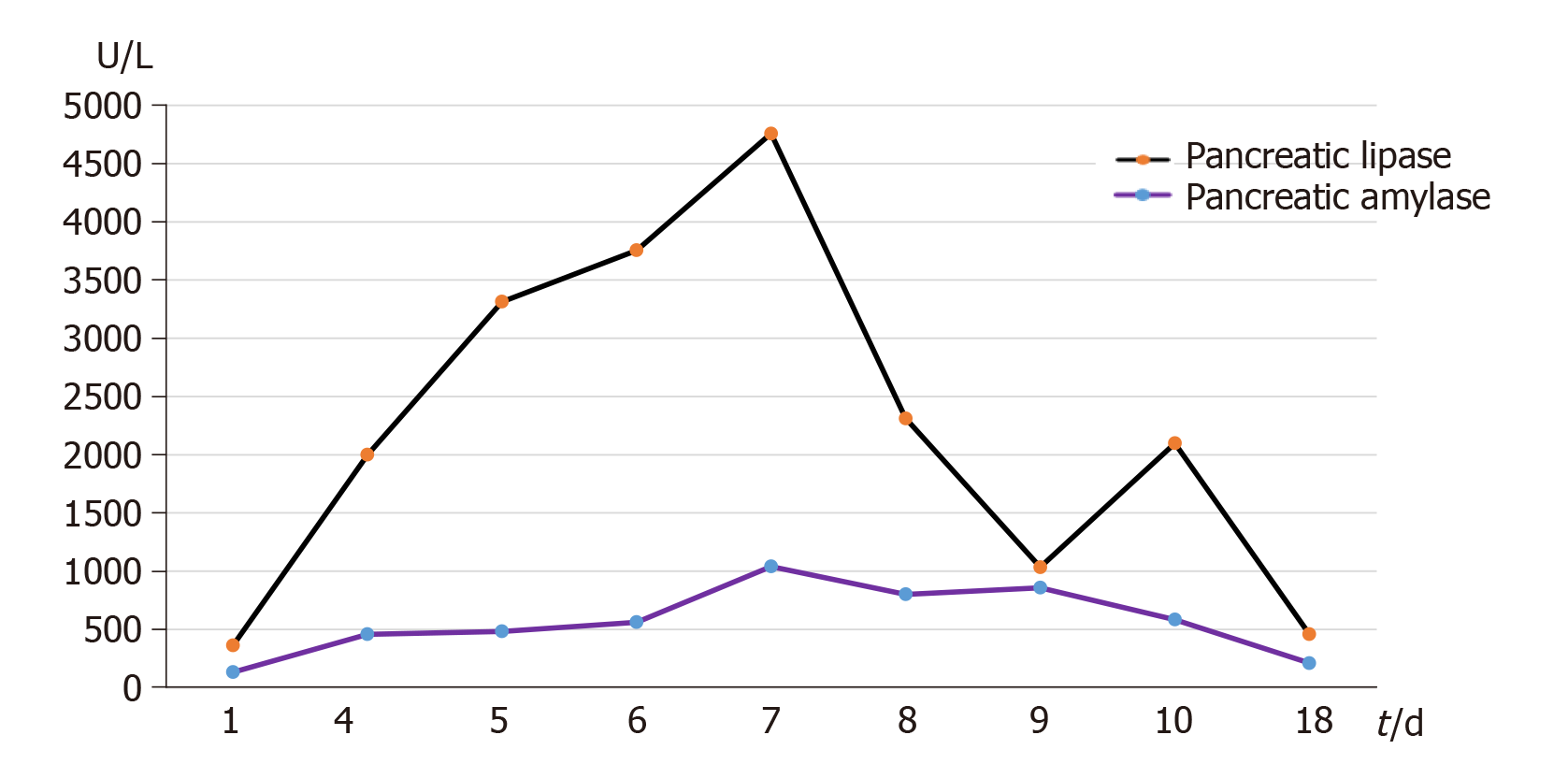
Based on the results of the examinations and after discussion with the treatment group, it was suggested that some measures be taken, including gastrointestinal decompression and rapid anti-inflammatory treatment with antibiotics. After active anti-inflammatory treatment, the inflammation indicators in the patient's blood, such as white blood cells and neutrophils, gradually decreased (Figure 2). At the same time, the patient was treated with thyroxine (75 µg) for hypothyroidism on the sixth day after admission, and the thyroid function was monitored. After supplementation with levothyroxine sodium tablets, pancreatic amylase and lipase also slowly decreased (Figure 3).
After active treatment, the patient’s symptoms gradually improved. The patient recovered and was discharged from the hospital after antibacterial treatment, supplementation with levothyroxine sodium tablets and nutritional support. The patient continued thyroxine supplementation after discharge from the hospital. After the patient was discharged, after re-examination on the eighteenth day, the serum amylase and lipase gradually became normal (Figure 3). No acute pancreatitis was observed in the patients during the course of the disease, not only lipase and amylase in the blood gradually increase,but also with it slowly decreased to normal ranges after the patient was discharged from the hospital.
Hypothyroidism is an endocrine disease with significant morbidity and worldwide prevalence, which can affect multiple organ systems. It can be asymptomatic and subclinical and has the potential to be complicated by fatal pathologies. Hypothyroidism, characterized by the absence of functional thyroid hormone, is diagnosed when decreased levels of thyroid hormones cause an increase in the secretion of TSH[4]. Hypothyroidism, which occurs in not only the thyroid itself, can cause systemic clinical symptoms because thyroid hormone is dispersed throughout the whole body.
The clinical symptoms of hypothyroidism vary and can include clinical and subclinical symptoms. Clinical manifestations can vary based on the age of the patient at the time of diagnosis and the severity of hormone deficiency. Weight gain, constipation, cold sensitivity, fatigue, and dry skin are the most commonly reported symptoms of hypothyroidism[5,6]. Hypothyroidism can also cause a variety of common diseases, including chronic nephritis, anemia, and edema in the serous cavity. Additionally, Mirwais et al[7] reported that hypothyroidism caused pericardial effusion, and Rishi Ramtahal reported that subclinical hypothyroidism caused hypertension in pregnancy[8], preeclampsia-like syndrome[9] and paralytic ileus and acute kidney injuries[10].
We began to suspect that the action of inflammatory factors caused pancreatic lipase and amylase to increase, however, after active control of inflammation, trypsin remained high and gradually increasing. Leukocytes and neutrophils were gradually reduced on the fourth day after admission, after active anti-inflammatory treatment (Figure 2). There were no clinical symptoms of acute pancreatitis, but after the control of inflammatory, amylase and lipase in the pancreas were still higher than normal. On the basis of the results of the examination, we considered that the increase in trypsin may be due to the decrease in thyroxine, maybe not due to the effect of inflammation. Therefore, we initiated thyroxine supplementation. On the fourth day after admission, the patient began to add levothyroxine on the sixth day, the thyroxine level in the patient began to gradually increase (Table 1). After with the thyroid hormone supplementation, pancreatic amylase eventually decreased (Figure 3).
Hypothyroidism has not been previously reported to lead to elevated pancreatic amylase and lipase without clinical symptoms. A previous study by Blanco-Molina A found that dissociated acini in rats with hypothyroidism showed higher bethanechol-induced amylase secretion than acini in control animals, and the experimental rates were also more sensitive to the inhibitory TRH effect than the controls[11]. The animals with hypothyroidism were more sensitive to the inhibitory effect of TRH than the control animals. It was previously shown that TRH inhibited amylase pancreatic secretion by a direct effect on acinar preparations. When TRH was decreased, the inhibition of pancreatic amylase was lost. These findings suggest that TRH could be an inhibitor of pancreatic amylase secretion, resulting in elevated, amylase and lipase levels in hypothyroidism.
This case occurred in a patient admitted to the hospital with fever. During the course of the disease, amylase and lipase were elevated, but no acute pancreatitis was observed. Hypothyroidism was finally diagnosed considering the patient's medical history and the examination results. It was finally found that the thyroid function of the patient was reduced, and serum amylase and lipase decreased gradually after thyroid hormone supplementation. The patient was finally discharged safely. According to the literature, the mechanism of this phenomenon is not clear. In the future, we will analyze additional cases to study its pathogenesis.
Hypothyroidism with elevated pancreatic amylase and lipase without clinical symptoms is a relatively rare occurrence in the clinical setting. In future clinical practice, we should pay attention to the complications of hypothyroidism. We expect that a detailed description of this case will provide valuable resources for future diagnosis. However, additional cases are needed to confirm our findings, and research is needed to further elucidate the mechanism.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Eleazu C, Inal V S-Editor: Ma YJ L-Editor: Filipodia E-Editor: Li JH
| 1. | Niazi AK, Kalra S, Irfan A, Islam A. Thyroidology over the ages. Indian J Endocrinol Metab. 2011;15:S121-S126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (3)] |
| 2. | Gomes-Lima C, Wartofsky L, Burman K. Can Reverse T3 Assay Be Employed to Guide T4 vs. T4/T3 Therapy in Hypothyroidism? Front Endocrinol (Lausanne). 2019;10:856. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Biondi B, Cooper DS. Thyroid hormone therapy for hypothyroidism. Endocrine. 2019;66:18-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (1)] |
| 4. | Udovcic M, Pena RH, Patham B, Tabatabai L, Kansara A. Hypothyroidism and the Heart. Methodist Debakey Cardiovasc J. 2017;13:55-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 143] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 5. | Carlé A, Pedersen IB, Knudsen N, Perrild H, Ovesen L, Laurberg P. Hypothyroid symptoms and the likelihood of overt thyroid failure: a population-based case-control study. Eur J Endocrinol. 2014;171:593-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (2)] |
| 6. | Diaz A, Lipman Diaz EG. Hypothyroidism. Pediatr Rev. 2014;35:336-47; quiz 348-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Mirwais S, Kazmi SH, Hussain SI, Mirwais M, Sharma A. Hypothyroidism Causing Pericardial Effusion: A Case Report. Cureus. 2019;11:e6393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Ramtahal R, Dhanoo A. Subclinical hypothyroidism causing hypertension in pregnancy. J Am Soc Hypertens. 2016;10:691-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Inversetti A, Serafini A, Manzoni MF, Dolcetta Capuzzo A, Valsecchi L, Candiani M. Severe hypothyroidism causing pre-eclampsia-like syndrome. Case Rep Endocrinol. 2012;2012:586056. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Rodrigo C, Gamakaranage CS, Epa DS, Gnanathasan A, Rajapakse S. Hypothyroidism causing paralytic ileus and acute kidney injury - case report. Thyroid Res. 2011;4:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Blanco-Molina A, Lopez Segura F, Vara E, Lopez Miranda J, Torre-Cisneros J, Perez-Jimenez F. Different secretory response of pancreatic isolated lobules and dissociated acini from hypothyroid rats to exogen TRH. Exp Clin Endocrinol. 1991;98:15-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (1)] |