Published online Jul 26, 2020. doi: 10.12998/wjcc.v8.i14.3114
Peer-review started: January 11, 2020
First decision: June 8, 2020
Revised: June 10, 2020
Accepted: July 4, 2020
Article in press: July 4, 2020
Published online: July 26, 2020
Processing time: 194 Days and 19.9 Hours
Dental focal infection-induced ventricular and spinal canal empyema is an extremely rare, severe, acute disease that is clinically associated with extremely high morbidity and mortality. Traditional cerebrospinal fluid (CSF) bacterial culture is time-consuming, with a low positive rate, which frequently results in severe irreversible consequences. The next-generation sequencing technique is an emerging pathogenic microorganism detection method that can obtain results in a short time with high accuracy, thus providing great assistance in the clinical diagnosis and treatment of this disease.
This paper reports a rare case of dental focal infection-induced ventricular and spinal canal empyema. During the course of treatment at a local hospital, the patient had negative results from repeated CSF bacterial cultures and was empirically given vancomycin treatment. After transfer to our hospital, the next-generation sequencing technique was adopted to determine that the pathogenic microorganisms were multiple anaerobic infectious bacteria derived from the oral cavity. The antibiotic therapeutic scheme was adjusted in a timely manner, and the ventricular and spinal canal inflammation was also controlled. However, the antibiotics that had been applied at the local hospital were not able to cover all pathogenic microorganisms, which resulted in irreversible injury to the brain stem, finally leading to patient death.
Dental focal infection-induced ventricular and spinal canal empyema is an extremely rare, severe, acute disease with high morbidity and mortality. Any delay in diagnosis and treatment will result in irreversible consequences. The early application of the next-generation sequencing technique can obtain results in a short time and clarify a diagnosis. Appropriate antibiotic treatment combined with suitable surgical intervention is the key to managing this disease.
Core tip: Dental focal infection-induced ventricular and spinal canal empyema is an extremely rare severe acute disease with high morbidity and mortality. Any delay in diagnosis and treatment will result in irreversible consequences. The early application of the next-generation sequencing technique can obtain results in a short time and clarify a diagnosis. Appropriate antibiotic treatment combined with suitable surgical intervention is the key to managing this disease.
- Citation: Xue H, Wang XH, Shi L, Wei Q, Zhang YM, Yang HF. Dental focal infection-induced ventricular and spinal canal empyema: A case report. World J Clin Cases 2020; 8(14): 3114-3121
- URL: https://www.wjgnet.com/2307-8960/full/v8/i14/3114.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i14.3114
Dental focal infection-induced ventricular and spinal canal empyema is an extremely rare, severe, acute disease with high morbidity and mortality. Fewer than 5% of brain abscesses that develop from a dental focal infection manifest as pyocephalus, which is extremely rare[1,2]. Analysis by computed tomography (CT) is the preferred imaging examination, while magnetic resonance imaging (MRI) is an examination modality with higher identification ability than CT, and it is the essential imaging analysis, if feasible based on the patient condition[2]. Traditional laboratory bacterial culture is time-consuming, with a low positive rate[2,3]. The next-generation sequencing technique is an emerging pathogenic microorganism detection method that can obtain results in a short time with high accuracy and provide great assistance in the clinical diagnosis and treatment of this disease[4].
A 53-year-old female patient was admitted to the Neurotrauma Surgery Department of Jilin University First Hospital on September 13, 2019, due to intermittent fever for 6 d and unconsciousness for 4 d.
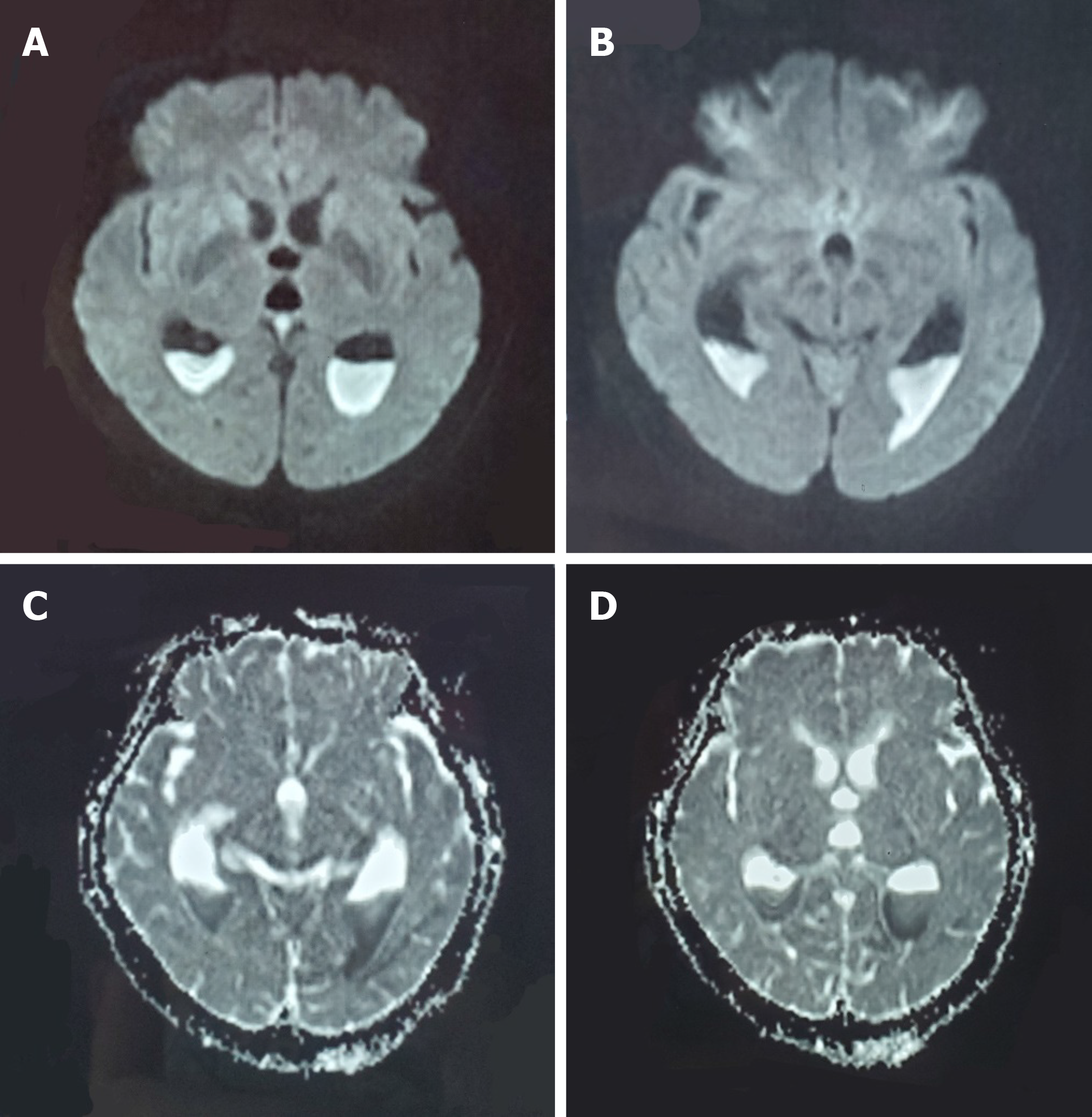
Initially, the patient was admitted to a local hospital as a result of hypertensive disease; 1 day after admission, she had fever, with the highest body temperature of 38.8 °C; 2 d later, the patient had sudden unconsciousness. Emergency head MRI revealed the fester-traditional cerebrospinal fluid (CSF) level inside the posterior horns of bilateral lateral ventricles, the fester diffuse weighted imaging (DWI) showed a high signal, and the apparent diffusion coefficient map showed a low signal (Figure 1). Thereafter, the patient was transferred to the Neurosurgery Department to receive emergency extraventricular drainage. Multiple CSF bacterial cultures after surgery revealed negative results, and the local physician empirically administered vancomycin treatment to the patient. After surgery, the patient was in continuous narcosis, and her family visited our hospital to seek further diagnosis and treatment.
The patient had a past history of hypertension for 10 years and received oral antihypertensive drug therapy, but no ideal control effect was achieved. In addition, the patient had had dental caries for 3 years, and she did not receive systemic treatment after the medulla oblongata treatment 1 month prior.
The patient had a free personal and family history.
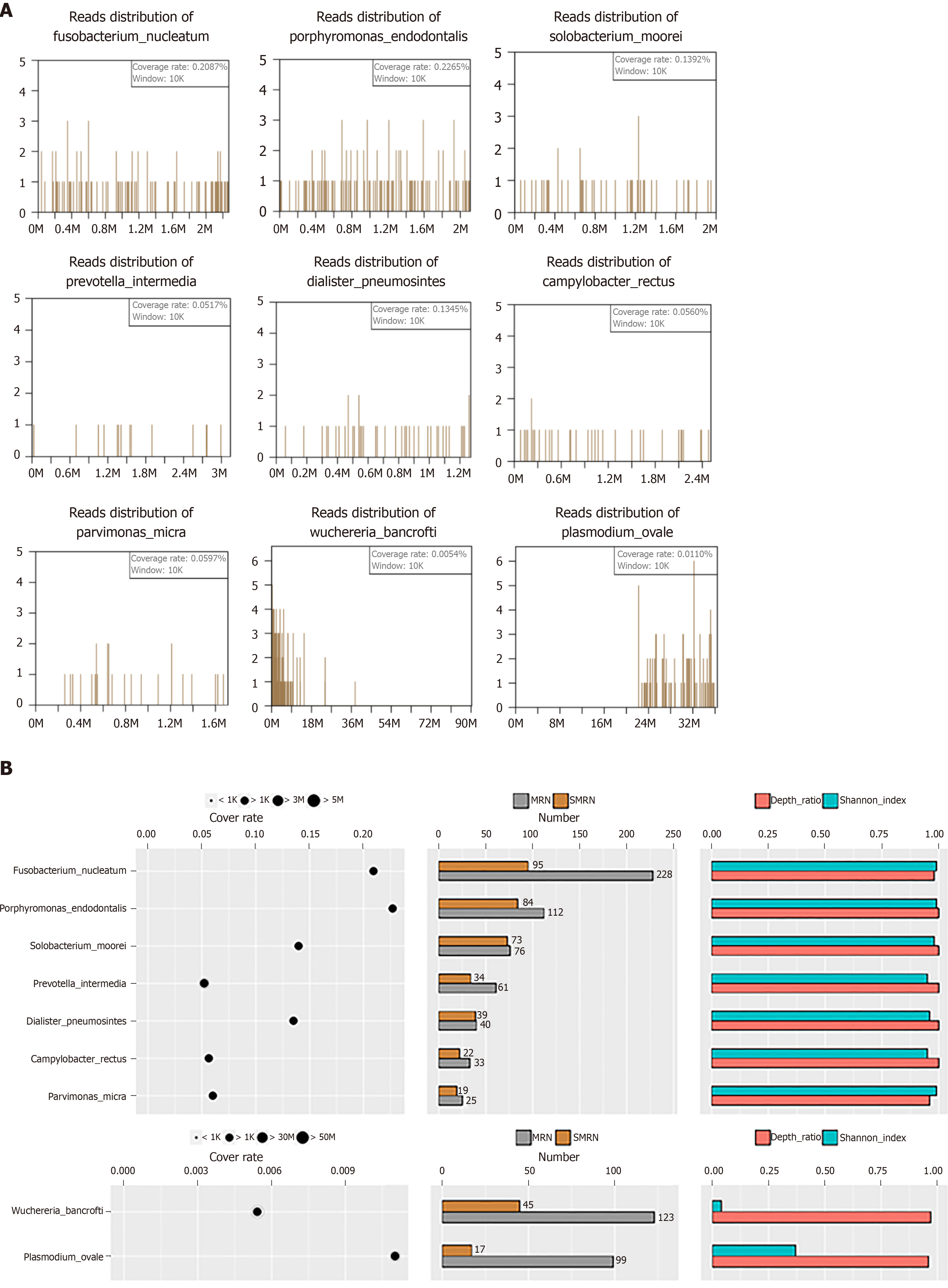
Physical examination upon admission showed that the patient was in narcosis with no autonomous respiration. The Glasgow Coma Scale score was E3V1M4. Extensive lesions and loosening of the second molars in the bilateral mandibles were found. CSF culture and next-generation sequencing of pathogenic microorganisms were carried out after admission. The intraventricular CSF culture results were negative, while pathogenic microorganism next-generation sequencing suggested Fusobacterium, Porphyromonas, Solobacterium, Prevotella, Dialister, Fusobacterium nucleatum, Fusobacterium hwasookii, Porphyromonas endodontalis, Solobacterium moorei, Prevotella intermedia, and Dialister pneumosintes (Figure 2A and B).
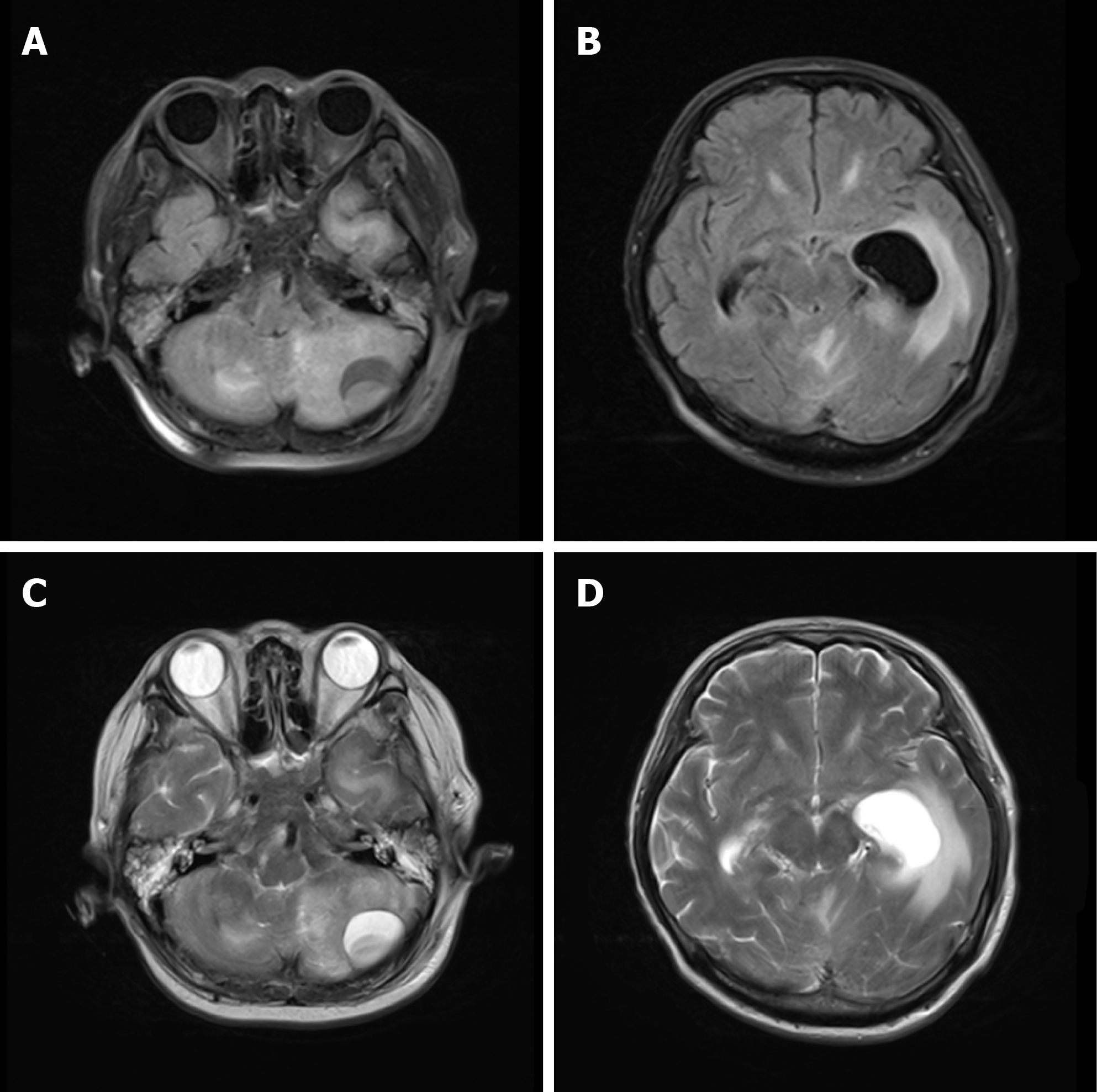
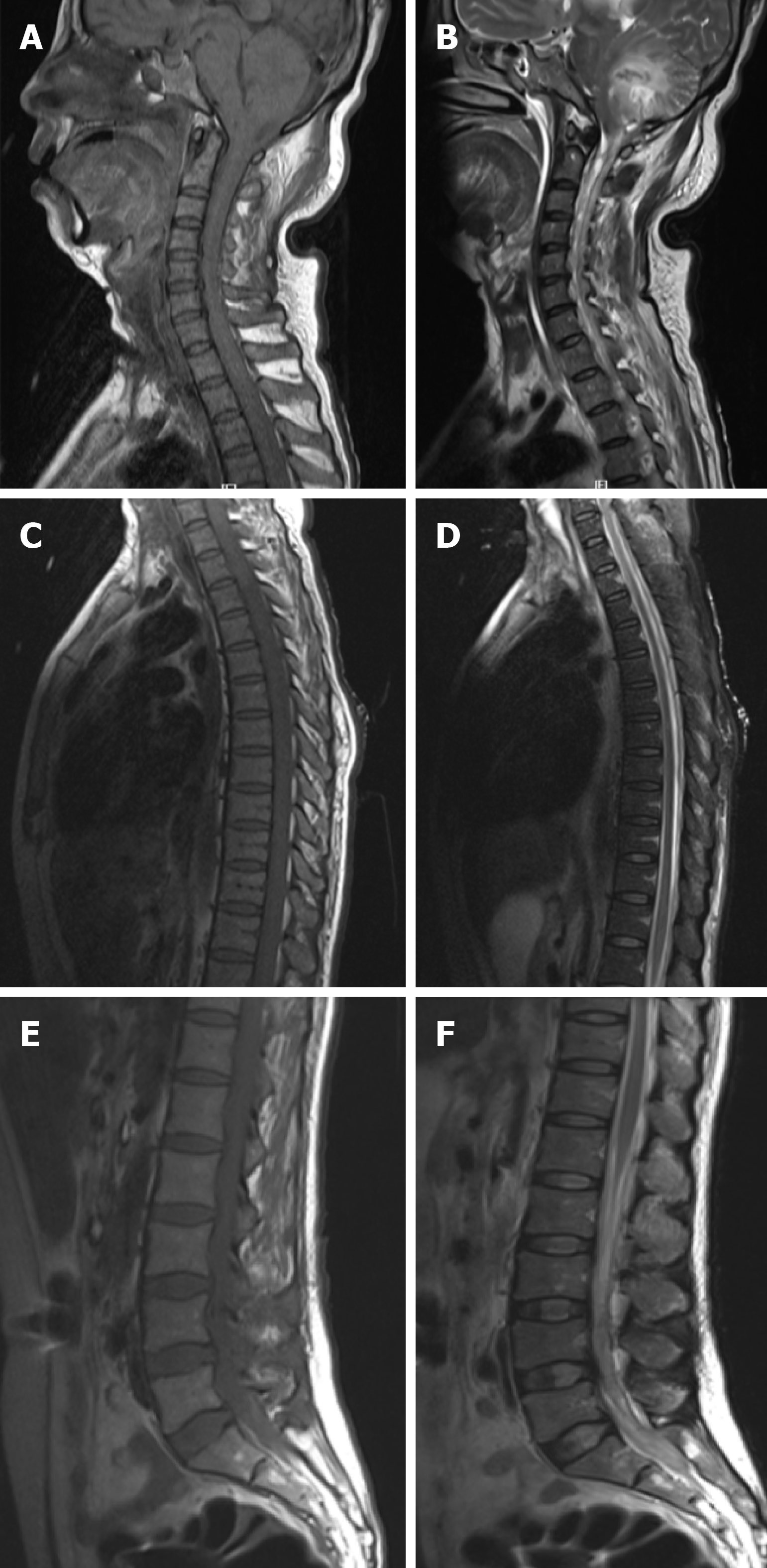
Head MRI revealed a quasicircular liquid signal opacity in the left cerebellum. The adjacent brain stem was compressed, the fourth ventricle became narrower, and ventricular hydrops accompanied by paraventricular edema was observed (Figure 3). Spinal MRI revealed stripe-like long T1 and long T2 signals in C7-T2 spinal canals (Figure 4).
The final diagnosis of the presented case was ventricular and spinal canal empyema.
After admission, the patient underwent several extracentricular drainages and lumbar punctures. The antibiotic therapeutic scheme was adjusted immediately to vancomycin, meropenem, gentamicin, and S-ornidazole combined with anti-infective treatment.
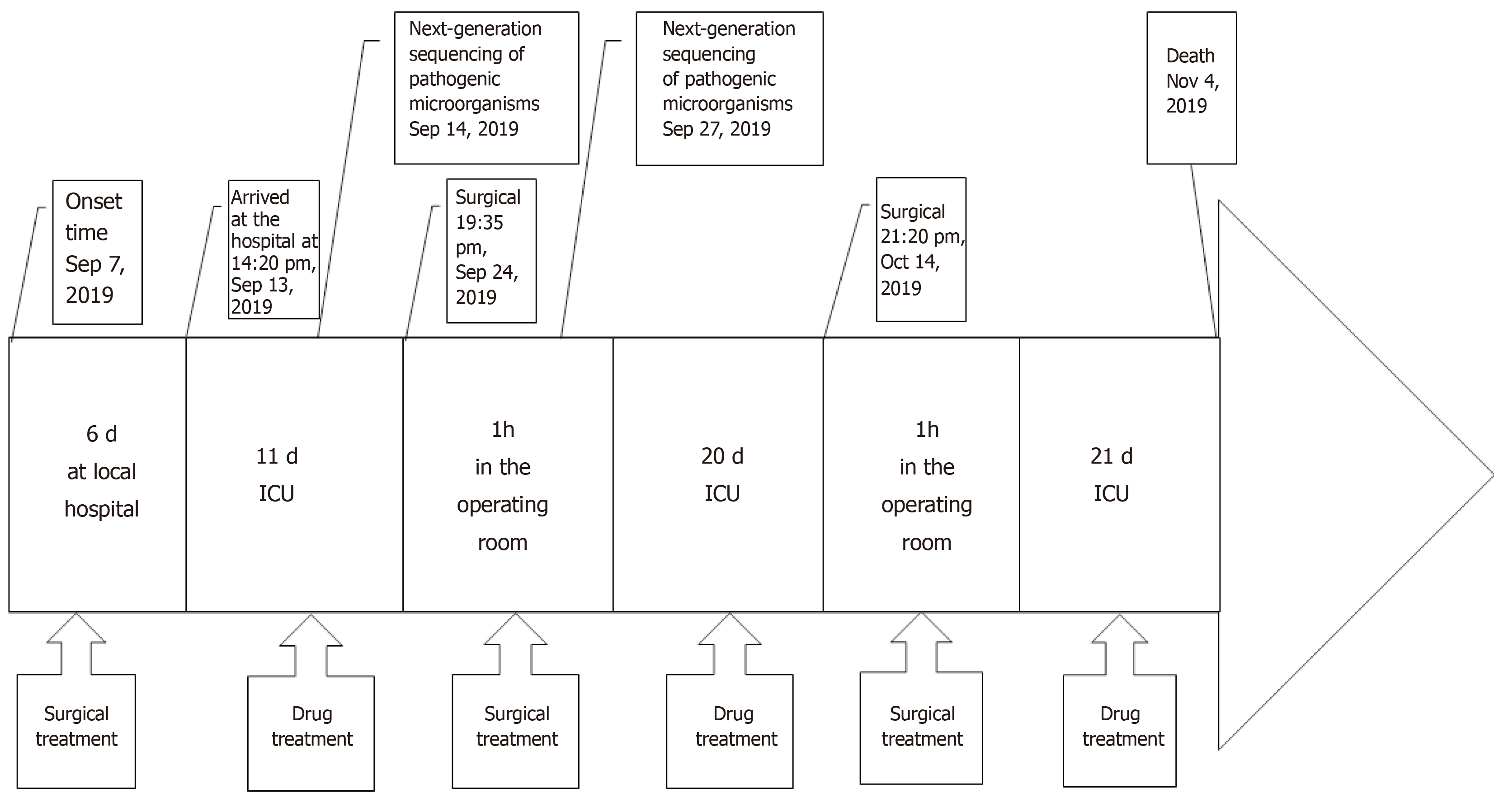
The patient died of brain stem injury-induced respiratory circulatory failure at 2 mo after admission. The timeline of the case is shown in Figure 5.
Brain abscess is an extremely rare, life-threatening disease in neurosurgery, and its morbidity is reported to be 1/100000 in the Unites States[1]. In the early 1970s, the mortality of brain abscess was 30%-60% but was reduced to 0-24% in recent years due to the rapid development of neuroimaging techniques (such as CT and MRI), the development of more effective antibiotics, and the improvement of surgical techniques[5]. Among all causes of brain abscess, otogenic causes account for 65.75%, hematogenous causes account for 13%, and odontogenic causes account for a low fraction. In addition, only < 5% of dental focal infection-induced brain abscesses manifest as pyocephalus, which is extremely rare[1,2].
As part of the Human Microbiome Project, the molecular identification method has been used to identify over 1200 kinds of microorganisms in the human oral cavity[6]. Over 350 distinct microorganisms were isolated from marginal periodontitis[6], and 150 different bacterial strains were isolated from endodontic infections[7]. The commonly seen pathogenic microorganisms include Streptococcus viridans (especially the anginosus group), Actinomyces, Peptostreptococcus, Prevotella, Fusobacterium, Aggregatibacter actinomycetemcomitans, and Eikenella corrodens[2]. The next-generation sequencing results suggested that the 11 infectious bacteria in our patient were mostly colonizers of the oral cavity.
Research shows that the pathogenic microorganisms result in dental focal infection-induced brain abscess through the following four pathways: (1) Systemic bacteremia; (2) Direct drainage to the cavernous sinus through facial and pterygoid vein systems; (3) Infection through continuous diffusion; and (4) Lymphatic drainage[8]. The most likely infection pathway of our patient was systemic hematogenous infection. The patient had a past dental operation history, and she did not receive systemic treatment. Dental operations cause periodontal vascular endothelial damage, and as a result, a large number of oral bacteria enter the blood. According to the research by Roberts et al[9], periodontal small blood vessel injury results in bacteremia, and 38.5% of people have transient bacteremia even in daily tooth brushing. Our patient had a history of hypertension, and her blood brain barrier (BBB) integrity was destroyed. The BBB is an important defense barrier in the human body that provides physical protection for the central nervous system (CNS). However, in hypertensive patients, the BBB is broken, which may result in leakage of small arterioles, thus promoting the occurrence of bacteremia[10].
CT examination is the preferred imaging modality, and a plain MRI scan combined with DWI should be performed subsequently[2]. MRI-DWI can distinguish benign abscesses from primary or metastatic tumors[2]. Its typical MRI manifestation includes the liquid level formed by fester, necrotic debris, and CSF in the cerebral ventricle. Fester and debris are located at the weight-bearing sites in the occipital horn and trigonum of the cerebral ventricle; compared with the CSF signal, fester tissue debris shows a slightly low T2WI signal and a slightly high T1WI signal[11-13].
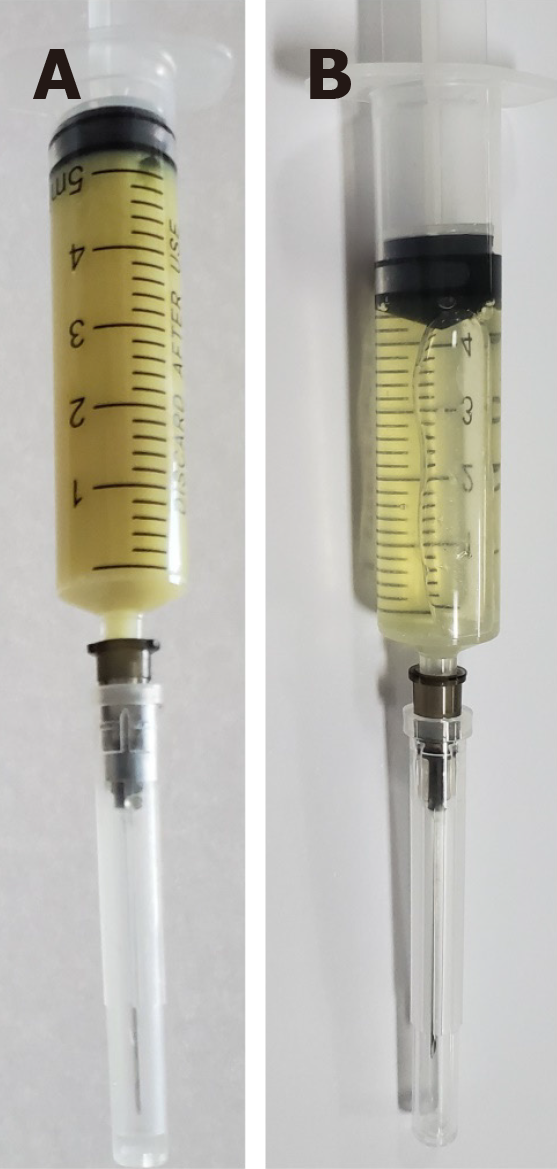
Additionally, CSF bacterial culture is an essential laboratory examination. However, under certain circumstances, standard bacterial culture may not serve as an effective pathogen identification method, particularly when the source of infection is suspected to be derived from the oral cavity. This is because numerous oral bacteria are fastidious pathogenic bacteria, which may not necessarily grow in culture sufficiently to allow easy identification. Some bacteria induce infection only in the presence of other pathogenic bacteria, and they are called concomitant pathogens[2]. In addition, traditional bacterial culture is time-consuming. Therefore, we adopted a new pathogen detection method, namely, next-generation sequencing. Its principle is to employ the second-generation high-throughput sequencing technique to sequence the nucleic acid in the sample, carry out a comparative analysis through the microorganism database according to the metagenomics principle, and obtain the species information of the suspected pathogenic microorganism by means of an intelligent algorithm[4]. Using this microorganism detection method, results are obtained in 1 d, and it can achieve high accuracy[4]. After the patient was admitted, we conducted traditional bacterial culture and pathogenic microorganism next-generation sequencing at the same time. The results of multiple bacterial cultures were negative, while pathogenic microorganism next-generation sequencing identified multiple oral microorganism infections. The antibiotic usage scheme was adjusted immediately based on the pathogenic microorganism next-generation sequencing results, and the CSF white blood cell count in the patient decreased from 551723 × 106 mmol/L to 33 × 106 mmol/L. The appearance of the CSF also changed from the original resemblance to rice water to that of a faint-yellow, clear liquid (Figure 6).
In terms of treatment, enough importance should first be attached to the progression of CNS disease, which should be regarded as a life-threatening, severe, acute disease[14]. Once a diagnosis is confirmed, treatments from three aspects should be applied immediately: (1) Aggressive surgery for abscess debridement or drainage; (2) Suitable combined antibiotic treatment selected according to the pathogenic microorganisms; and (3) Treatment specific to the primary infection lesion[14]. In our patient, the antibiotics combined with anti-infective treatment were adjusted in a timely manner, and local oral treatment was also applied, but the antibiotics that had been applied at the local hospital did not cover all pathogenic bacteria, and the brain stem function was subjected to irreversible damage, finally leading to patient death.
Dental focal infection-induced ventricular and spinal canal empyema is an extremely rare, severe, acute disease with high morbidity and mortality. Any delay in diagnosis and treatment will result in irreversible consequences. The early application of the next-generation sequencing technique can obtain results in a short time and clarify a diagnosis. Appropriate antibiotic treatment combined with suitable surgical intervention is the key to managing this disease.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Alimehmeti RH S-Editor: Wang JL L-Editor: Wang TQ E-Editor: Xing YX
| 1. | Li X, Tronstad L, Olsen I. Brain abscesses caused by oral infection. Endod Dent Traumatol. 1999;15:95-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 52] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Moazzam AA, Rajagopal SM, Sedghizadeh PP, Zada G, Habibian M. Intracranial bacterial infections of oral origin. J Clin Neurosci. 2015;22:800-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 85] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 3. | Van der Cruyssen F, Grisar K, Maes H, Politis C. Case of a cerebral abscess caused by Porphyromonas gingivalis in a subject with periodontitis. BMJ Case Rep. 2017;2017:bcr2016218845. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Salzberg SL, Breitwieser FP, Kumar A, Hao H, Burger P, Rodriguez FJ, Lim M, Quiñones-Hinojosa A, Gallia GL, Tornheim JA, Melia MT, Sears CL, Pardo CA. Next-generation sequencing in neuropathologic diagnosis of infections of the nervous system. Neurol Neuroimmunol Neuroinflamm. 2016;3:e251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 124] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 5. | Xiao F, Tseng MY, Teng LJ, Tseng HM, Tsai JC. Brain abscess: clinical experience and analysis of prognostic factors. Surg Neurol. 2005;63:442-9; discussion 449-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 103] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 6. | Dewhirst FE, Chen T, Izard J, Paster BJ, Tanner AC, Yu WH, Lakshmanan A, Wade WG. The human oral microbiome. J Bacteriol. 2010;192:5002-5017. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2580] [Cited by in RCA: 2250] [Article Influence: 150.0] [Reference Citation Analysis (0)] |
| 7. | Corson MA, Postlethwaite KP, Seymour RA. Are dental infections a cause of brain abscess? Case report and review of the literature. Oral Dis. 2001;7:61-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 48] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Antunes AA, de Santana Santos T, de Carvalho RW, Avelar RL, Pereira CU, Pereira JC. Brain abscess of odontogenic origin. J Craniofac Surg. 2011;22:2363-2365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Roberts GJ, Holzel HS, Sury MR, Simmons NA, Gardner P, Longhurst P. Dental bacteremia in children. Pediatr Cardiol. 1997;18:24-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 119] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Setiadi A, Korim WS, Elsaafien K, Yao ST. The role of the blood-brain barrier in hypertension. Exp Physiol. 2018;103:337-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 83] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 11. | Fujikawa A, Tsuchiya K, Honya K, Nitatori T. Comparison of MRI sequences to detect ventriculitis. AJR Am J Roentgenol. 2006;187:1048-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Fukui MB, Williams RL, Mudigonda S. CT and MR imaging features of pyogenic ventriculitis. AJNR Am J Neuroradiol. 2001;22:1510-1516. [PubMed] |
| 13. | Pezzullo JA, Tung GA, Mudigonda S, Rogg JM. Diffusion-weighted MR imaging of pyogenic ventriculitis. AJR Am J Roentgenol. 2003;180:71-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 39] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Ewald C, Kuhn S, Kalff R. Pyogenic infections of the central nervous system secondary to dental affections--a report of six cases. Neurosurg Rev. 2006;29:163-6; discussion 166-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 54] [Article Influence: 2.8] [Reference Citation Analysis (0)] |