Published online Jul 26, 2020. doi: 10.12998/wjcc.v8.i14.3108
Peer-review started: March 16, 2020
First decision: April 22, 2020
Revised: June 11, 2020
Accepted: June 18, 2020
Article in press: June 18, 2020
Published online: July 26, 2020
Processing time: 128 Days and 4.5 Hours
Recurrent cystic echinococcosis (CE) with vital organ involvement is a challenge for clinicians. Herein, we report a case of aortic involvement in recurrent retroperitoneal CE lesions following primary splenic CE resection.
A 60-year-old male was admitted due to progressive abdominal pain and poor appetite. He was diagnosed with multiple recurrent CE with abdominal aortic involvement according to preoperative evaluation. During surgical resection, major aortic bleeding accidentally occurred while dissecting the cyst, which was firmly attached to the abdominal aortic wall. Hemostasis attempts were conducted to deal with this emergency situation and maintain circulation. Post-interventional recovery was uneventful, and 2-year follow-up showed no sign of recurrence or any other complications.
Radical resection of recurrent complicated CE with aortic involvement should be carefully planned and performed to prevent possible severe adverse complications, thereby improving the postoperative outcome.
Core tip: Cystic echinococcosis (CE) is a zoonotic disease caused by Echinococcus granulosis, which is globally distributed. Recurrent lesions, multiple organ involvement and vital organ involvement are considered challenging for clinicians. Herein, we report a case of aortic involvement in recurrent retroperitoneal CE lesions following primary splenic CE resection. This case highlights that primary surgery of CE should be carefully performed to prevent recurrence. Furthermore, surgical resection of recurrent complicated CE with aortic involvement should be carefully planned and performed to prevent possible severe adverse complications, thereby improving the postoperative outcome.
- Citation: Taxifulati N, Yang XA, Zhang XF, Aini A, Abulizi A, Ma X, Abulati A, Wang F, Xu K, Aji T, Shao YM, Ahan A. Multiple recurrent cystic echinococcosis with abdominal aortic involvement: A case report. World J Clin Cases 2020; 8(14): 3108-3113
- URL: https://www.wjgnet.com/2307-8960/full/v8/i14/3108.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i14.3108
Cystic echinococcosis (CE) is a zoonotic disease caused by Echinococcus granulosis, which is globally distributed[1,2]. A CE lesion often presents as an asymptomatic chronic growth within solid organs in the early stage, and thereafter gradually shows space occupying lesion-related symptoms. Radical resection in combination with postoperative albendazole therapy remains the preferred treatment option[1,3,4]. Awareness of the manifestations and treatment modalities of various CE involvements will be helpful in the individualized management of the disease and probable complications[5,6]. However, recurrent lesions, multiple organ involvement and vital organ involvement are considered challenging for clinicians. Herein, we report a case of aortic involvement in recurrent retroperitoneal CE lesions following primary splenic CE resection.
A 60-year-old male with the chief complaints of progressive abdominal pain and poor appetite was admitted to our department.
He previously underwent surgery for a splenic CE lesion. There was no other relevant personal or familial history.
Physical examination upon admission revealed a mass in the left upper quadrant of the abdomen.
Laboratory examinations (routine blood tests, routine urine tests and urinary sediment examination, routine fecal tests and occult blood test, blood biochemistry, immune indices, and infection indices) showed no apparent abnormalities.
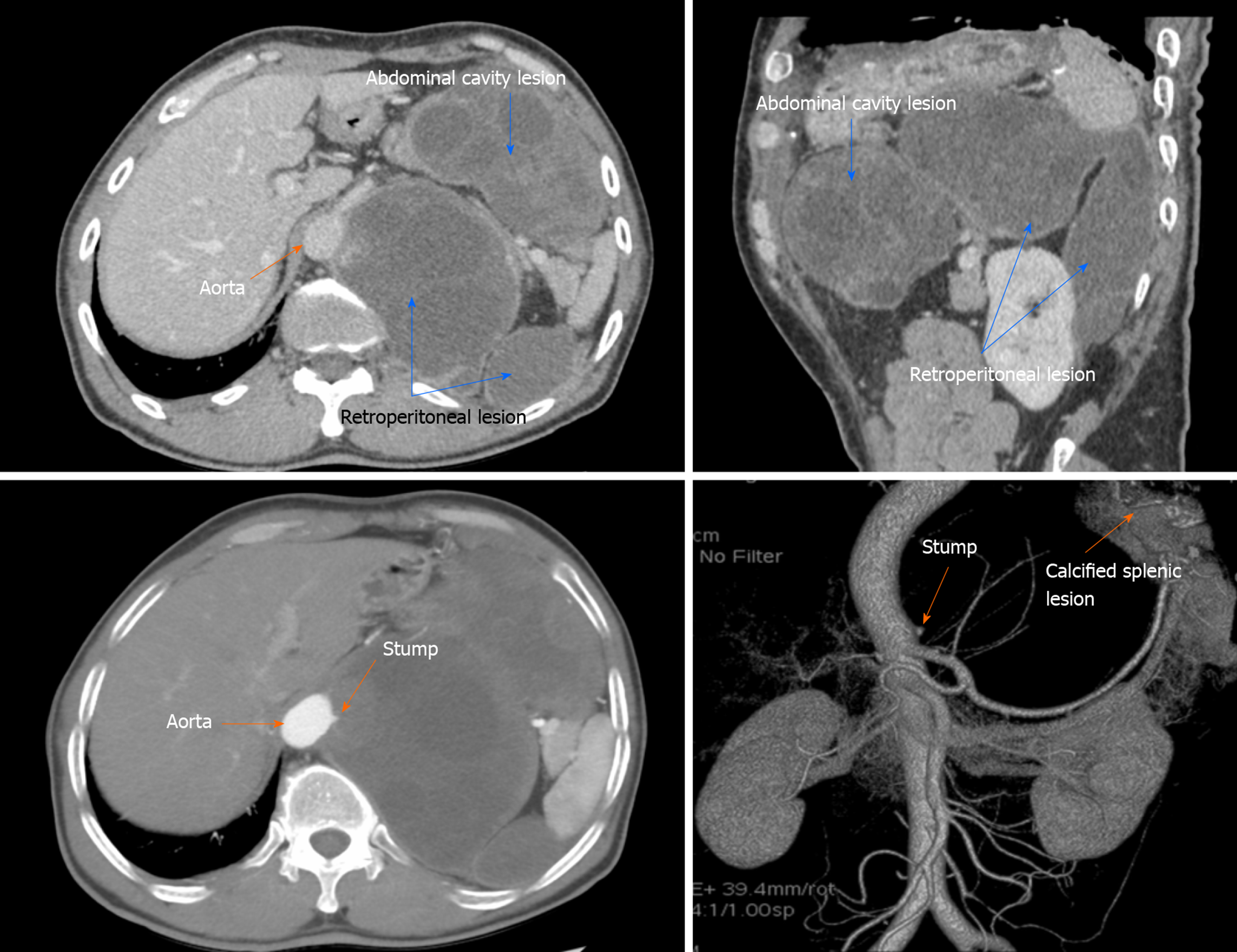
Imaging examination with computed tomography and angiography revealed two irregular CE2 lesions (approximately 10.0 cm × 14.0 cm × 13.6 cm and 12.5 cm × 11.2 cm × 5.8 cm), respectively, located in the left upper retroperitoneal cavity and the abdomen, according to World Health Organization (WHO) classification (Figure 1A and B)[1,2]. The lesions mainly invaded the liver-spleen-gastric gap, superior section of the spleen, left retro-renal cavity and the abdominal aortic wall (Figure 1C and D). There was no other abdominal organ involvement.
The patient was finally diagnosed with recurrent abdominal/retroperitoneal active CE with aortic involvement. After preoperative evaluation, abdominal hydatid excision combined with abdominal aortic stent implantation was planned and surgical treatment was performed on October 12, 2017.
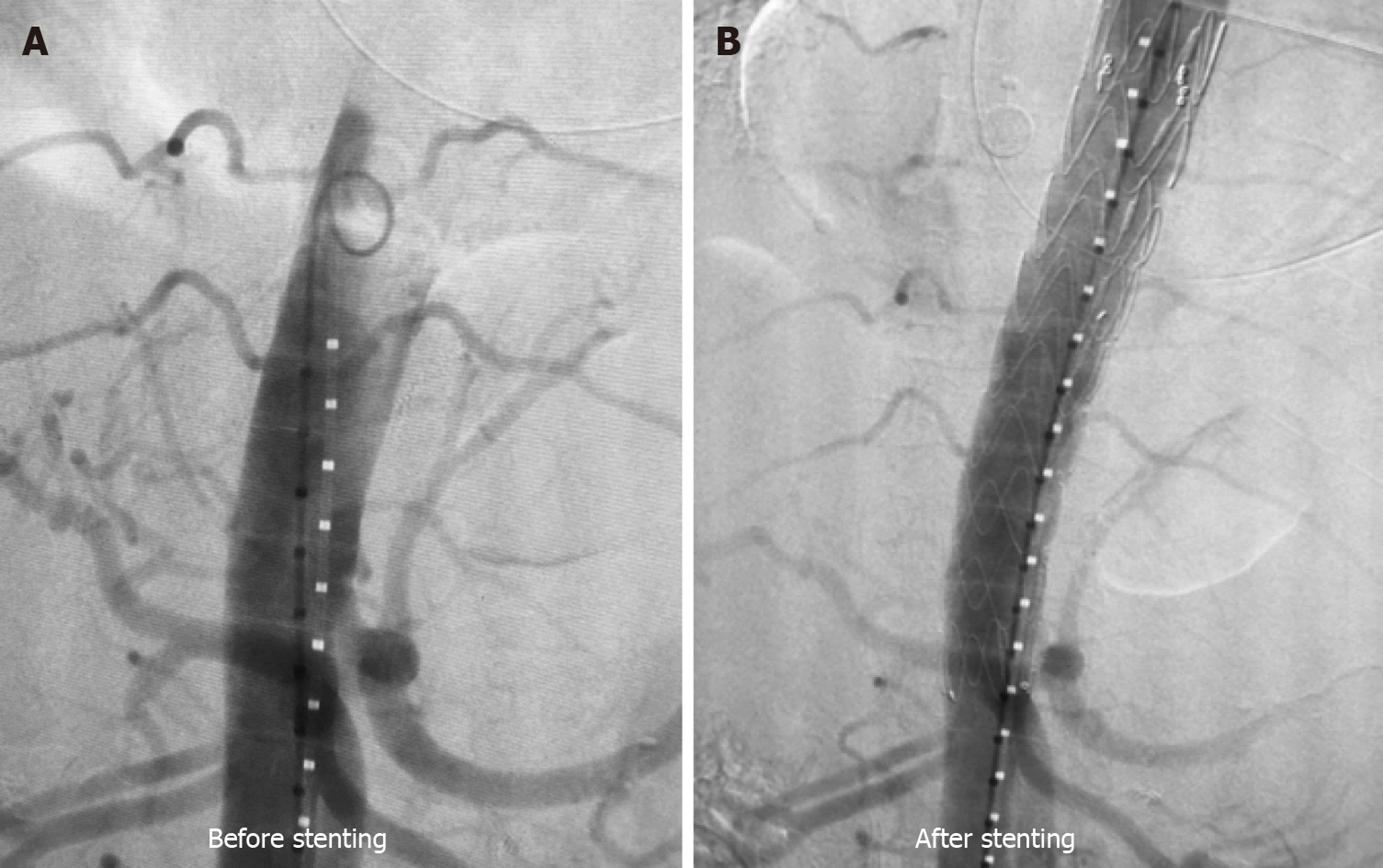
Surgery was performed under general anesthesia. Following an upper abdominal incision, two round-shaped hard lesions were found. Firstly, a lesion within the abdominal cavity was carefully removed from the gastrocolic space by total cystectomy. Another retroperitoneal lesion was then observed. Considering that the retroperitoneal lesion was huge and involved the aorta, sub-total cystectomy was performed in order to protect the aorta from possible injury. The outer capsule area was exposed as much as possible and the surrounding tissues were protected by 10% saline. The capsule of the retroperitoneal lesion was opened from the left side where it could be easily operated without affecting the aorta. The inner contents were then extracted under full vision. The residual cavity was then washed with 10% saline. Aneurysmal inflammatory granulation tissue was detected on the right capsule wall adjacent to the aortic wall. During the third saline washing of the cavity, the aortic wall suddenly ruptured. Massive bleeding suddenly occurred, accompanied by a drop in blood pressure and an increase in heart rate. The bleeding section of the abdominal aorta was immediately clamped and pressed. Blood loss was estimated to be 2500 mL. The upper end of the abdominal aorta was immediately separated and blocked intermittently for 30 min each time. Hemostasis attempts were conducted to deal with this emergency situation and maintain circulation. The rupture site was at the celiac trunk level and was sutured with 3-0 proline lines in the setting of interrupted blockage of the superior and inferior sections of the aorta. A small amount of bleeding was found in the surgical area. The patient then underwent digital subtraction angiography (DSA), which showed an ulcer on the left posterior wall of the abdominal aorta (0.5 cm above the celiac arteries) and no obvious contrast agent overflow. A covered stent (VAMF2828 C150 TE, Medtronic Inc., United States) was placed in the aortic wall after angiography of the aortic section. No active bleeding was observed. Blood flow in the aorta and main branches were confirmed to be normal (Figure 2). During surgery and DSA, a total of 11.5 units of erythrocyte suspension was transfused and vital signs and hemoglobin levels were maintained within normal levels. Thereafter, he was transferred to the intensive care unit, then to a general ward after 3 d, and discharged on day 13 following DSA. Postoperative pathological evaluation of the lesion was consistent with CE.
After surgery, the patient was administered albendazole 10 mg/kg/day according to expert consensus[3,4]. The patient was followed-up for the next two years by abdominal ultrasound examination. No abnormalities were observed during the 2-year-follow-up.
CE is a chronic zoonosis with inflating-growth characteristics compared to the infiltrating-growth pattern of alveolar echinococcosis. Liver is the most common site of CE, whereas splenic CE is very rare[1-4]. Expert consensus and WHO recommendations suggest R0 resection combined with anti-parasitic medication as the preferred treatment modality[1,3]. However, postoperative recurrence often adversely affects the outcome of patients with CE.
In this report, the patient had recurrent CE in the abdomen/retroperitoneum with aortic invasion after resection of splenic CE, which according to previous publications is even rarer[7,8]. Moreover, this patient suffered a severe intraoperative aortic rupture. We hypothesize that the lesion might have exploded due the two main facts: (1) The surgical technique when dealing with the cystic capsule; and (2) Osmotic pressure due to the high concentration of saline in the cystic cavity forced the interstitial fluid to permeate from the aneurysmal inflammatory granulation tissue, which then contracted, resulting in collapse of the aortic wall. Such an ulcerated vascular coat (connective tissue) is also an underlying situation for potential spontaneous rupture as the lesion grows. In our case, from the arterial stump to the lesion, this situation could have been predicted. From a histopathological view, the stump was the dead-end of an arterial branch, which was confirmed by preoperative imaging. After all, the coat of the stump was totally invaded. Based on the clinical and biological features of CE lesions, if the connective tissue is eroded by peri-lesion inflammation, a relevant potential gap becomes vulnerable and intermediate smooth muscle can be easily destroyed. As this phenomenon was present in previous imaging, possible invasion of the aortic main wall should have been taken into account. Then, intraoperative preventive methods (e.g., semi-blockage of the diseased aortic section in advance) would have been introduced.
Aortic or cardiovascular involvement are reported case by case[7,9,10]. There are several life-threatening complications in patients with aortic disease, such as anaphylactic shock, false aneurysm, systemic emboli and arterial occlusion[8]. Tosya et al[8] showed that an embolism of the germinative membranes was caused by ruptured cardiac hydatid cysts or by cystic lesions in the ascending aorta, and recommended using DSA, ultrasound, computed tomography and magnetic resonance imaging to accurately detect the relationship between the cyst and aorta, and excision of the capsule wall and graft implantation should be the first treatment choice. Berthet et al[5] reported a case of spontaneous or surgical rupture of a hydatid cyst into an adjacent vessel. Yörükoğlu et al[11] reported a case of thrombosis of an artery and/or vein due to compression by hydatid cysts. Moreover, Gerber et al[6] found that the cyst cavity was not related to the aortic lumen according to preoperative imaging, but aortic hemorrhage occurred after a decrease in cyst pressure, which is similar to our case. However, in this study, we observed that the abdominal aorta was invaded by CE, which presented as the development of aneurysmal granulation tissue, which may develop into a false aneurysm later. After surgery, we found an aneurysmal lesion on DSA.
In conclusion, primary surgery of CE should be carefully performed to prevent recurrence. Furthermore, the surgical resection of recurrent complicated CE with aortic or other important blood vessel involvement should be carefully planned. If the lesion is closely related to the surrounding large blood vessels, DSA should be performed to further assess the surrounding blood vessels, evaluate the possibility of complete resection, and try to avoid intraoperative hemorrhage. During the operation, if necessary, the corresponding vessels should be completely dissected and repaired using vascular surgery techniques. The blood supply of important organs should be ensured, improve complete resection of the tumor, and prevent possible severe adverse complications, thereby improving the postoperative outcome.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Larentzakis A, Vagholkar K S-Editor: Dou Y L-Editor: Webster JR E-Editor: Liu JH
| 1. | Wen H, Vuitton L, Tuxun T, Li J, Vuitton DA, Zhang W, McManus DP. Echinococcosis: Advances in the 21st Century. Clin Microbiol Rev. 2019;32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 421] [Cited by in RCA: 640] [Article Influence: 106.7] [Reference Citation Analysis (0)] |
| 2. | Deplazes P, Rinaldi L, Alvarez Rojas CA, Torgerson PR, Harandi MF, Romig T, Antolova D, Schurer JM, Lahmar S, Cringoli G, Magambo J, Thompson RC, Jenkins EJ. Global Distribution of Alveolar and Cystic Echinococcosis. Adv Parasitol. 2017;95:315-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 432] [Cited by in RCA: 640] [Article Influence: 80.0] [Reference Citation Analysis (0)] |
| 3. | Brunetti E, Kern P, Vuitton DA, Writing Panel for the WHO-IWGE. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop. 2010;114:1-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1108] [Cited by in RCA: 1336] [Article Influence: 89.1] [Reference Citation Analysis (0)] |
| 4. | Vuitton DA, Zhou H, Bresson-Hadni S, Wang Q, Piarroux M, Raoul F, Giraudoux P. Epidemiology of alveolar echinococcosis with particular reference to China and Europe. Parasitology. 2003;127 Suppl:S87-S107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 151] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 5. | Berthet B, N'Guema R, Assadourian R. An unusual complication of hydatid disease of the liver: spontaneous operative rupture of the inferior vena cava into the cyst wall. Case report. Eur J Surg. 1994;160:447-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Gerber BL, Pasquet A, El Khoury G, Verhelst R, Vanoverschelde JL, Watremez C, Vancraeynest D. Echinococcosis of the heart and ascending aorta. Circulation. 2012;125:185-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Parvizi R, Namdar H, Bilehjani E, Bayat A, Sheikhalizadeh MA. Simultaneous operation of hydatid cyst of the heart and liver: a case report. J Cardiovasc Thorac Res. 2013;5:127-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 8. | Tosya A, Uymaz B, Celebi S, Aybek T. A rare presentation of cystic echinococcosis: aortic involvement. Interact Cardiovasc Thorac Surg. 2015;21:548-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Tasdemir K, Akcali Y, Gunebakmaz O, Kaya MG, Mavili E, Sarli B, Tasdemir A, Ceyran H. Surgical approach to the management of cardiovascular echinococcosis. J Card Surg. 2009;24:281-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Kamyar MM, Ravari H. Thoracic aortic involvement in cystic echinococcosis: A case report. Electron Physician. 2017;9:5257-5260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Yörükoğlu Y, Zengin M, Dolgun A, Nazliel K, Salman E, Paşaoğlu E, Yucel E. Primary muscular hydatid cyst causing arterial insufficiency: case report and literature review. Angiology. 1993;44:399-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |