Published online Jul 26, 2020. doi: 10.12998/wjcc.v8.i14.2977
Peer-review started: April 1, 2020
First decision: April 22, 2020
Revised: April 24, 2020
Accepted: July 4, 2020
Article in press: July 4, 2020
Published online: July 26, 2020
Processing time: 114 Days and 1.4 Hours
Supraspinatus tendinitis recurs easily after treatment. One of the main reasons is the lack of objective tools for the efficacy evaluation. Shear wave elastography (SWE) can quantitatively analyze the tissue elasticity of region of interest by measuring the Young’s modulus (YM) value.
To explore the role of SWE in the efficacy and prognostic evaluation of supraspinatus tendinitis.
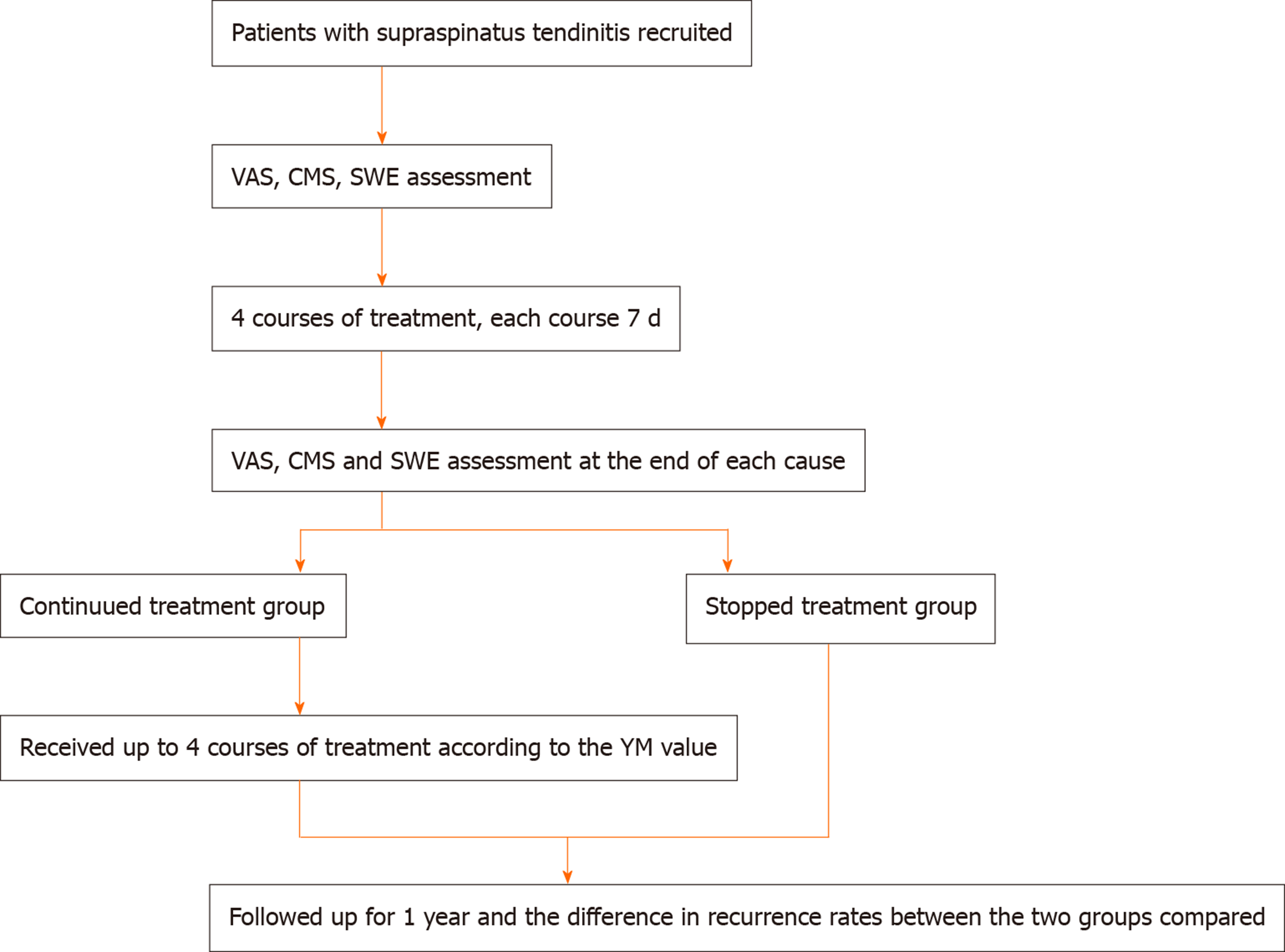
Eighty-seven patients with supraspinatus tendinitis treated in Jiading District Central Hospital Affiliated Shanghai University of Medicine and Health Sciences were recruited. Another 30 healthy volunteers were enrolled as the control group. The visual analogue scale (VAS) and Constant-Murley Score (CMS) were recorded before treatment. All participants were scanned by SWE scan, and the YM value of the region of interest were recorded. Spearman correlation analysis was performed on YM values with VAS and CMS. Univariate repeated measures analysis of variance was used to calculate the changing trend of VAS, CMS and SWE under different treatment courses. After treatment, the patients were further grouped based on who achieved significantly effective and curative treatment. The patients in the continued treatment group continued to receive treatment according to the YM value, and the remaining patients who stopped receiving treatment were included in the stopped treatment group. All patients were followed up for 1 year, and the difference in recurrence rates between the continued treatment group and the stopped treatment group were compared.
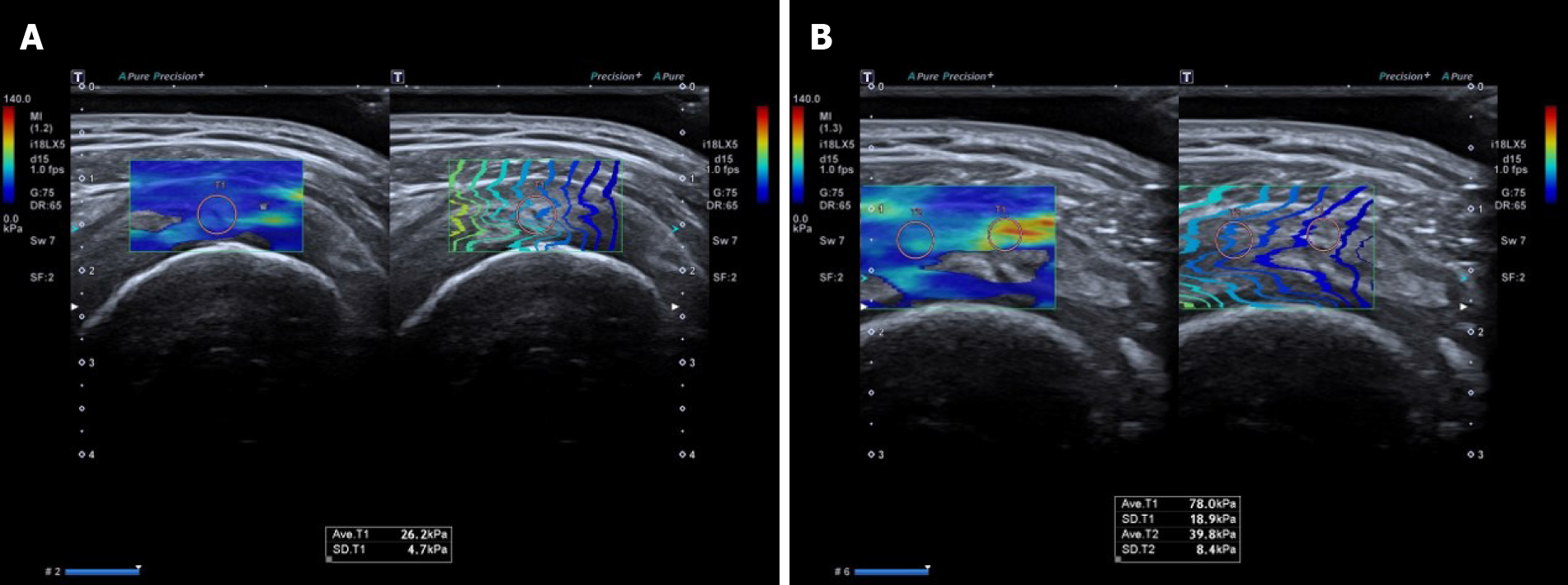
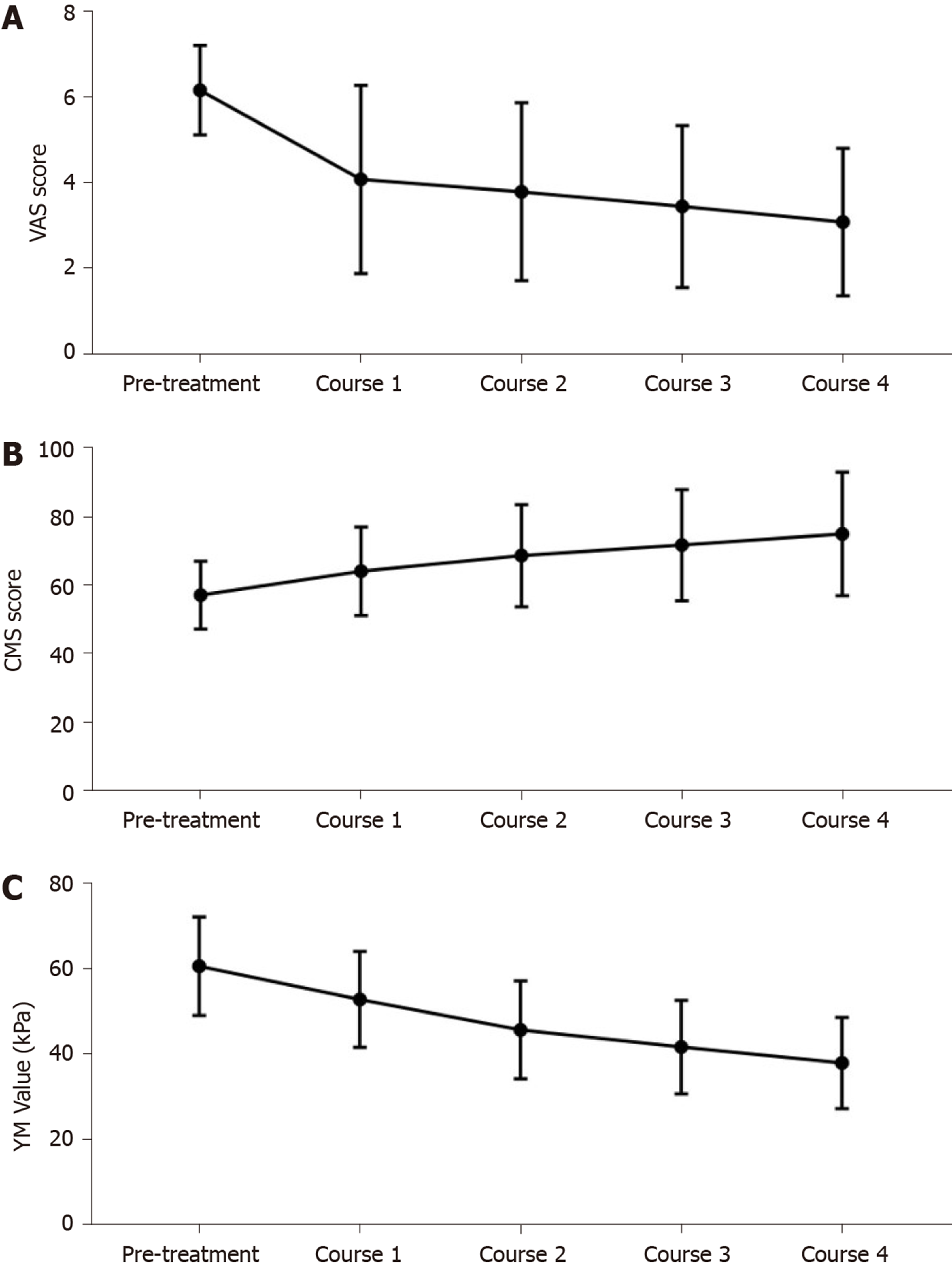
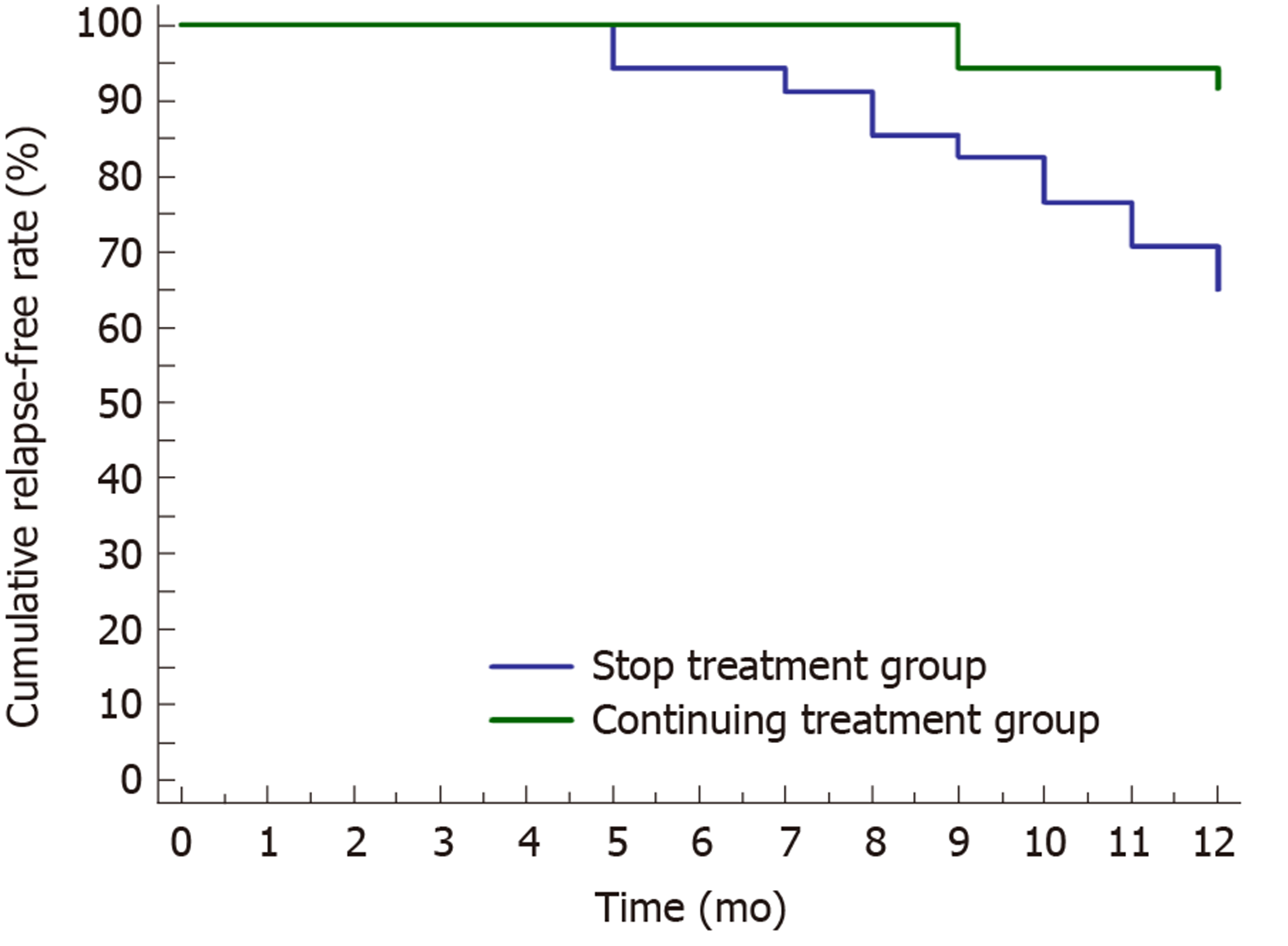
The SWE images of supraspinatus muscle in healthy volunteers were mainly blue, while those of patients with supraspinatus tendinitis showed regional red and green areas. The average YM value of the supraspinatus muscle in healthy volunteers was 26.12 ± 4.03 kPa. The average YM value of patients with supraspinatus muscle was greater than that of healthy volunteers (average YM = 60.61 ± 11.53 kPa, t = 26.344, P < 0.001). The YM value was positively correlated with VAS (r = 0.564, P < 0.001) and negatively correlated with CMS (r = -0.411, P < 0.001). The changes of VAS and CMS were the most obvious in course 1 and then decreased gradually. The degree of change in YM values was similar in different courses. After a 1-year follow-up, the cumulative relapse-free rate in the continued treatment group was 91.43%, which was significantly higher than that in the stopped treatment group (64.71%, X2 = 7.379, P = 0.007).
SWE can objectively indicate the severity of supraspinatus tendinitis. Using the YM value as a criterion for curative effect may reduce the recurrence rate.
Core tip: Supraspinatus tendinitis is a common disease. Due to the lack of objective assessment methods, it is easy to relapse after treatment. Shear wave elastography can quantitatively analyze the tissue elasticity by measuring the Young’s modulus value. This study explored the role of shear wave elastography in the efficacy and prognostic evaluation of supraspinatus tendinitis. It revealed that shear wave elastography can objectively indicate the severity of the supraspinatus tendinitis. Using the Young’s modulus value as the criterion for determining the efficacy of the treatment is more thorough, and it is expected to reduce the recurrence rate.
- Citation: Zhou J, Yang DB, Wang J, Li HZ, Wang YC. Role of shear wave elastography in the evaluation of the treatment and prognosis of supraspinatus tendinitis. World J Clin Cases 2020; 8(14): 2977-2987
- URL: https://www.wjgnet.com/2307-8960/full/v8/i14/2977.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i14.2977
Supraspinatus tendinitis is a common disease that causes shoulder pain and joint dysfunction[1,2]. Some treatments including rehabilitation training, physical therapy, nonsteroidal anti-inflammatory drugs and even local injection treatment are available according to the disease severity[3-5]. After treatment, the symptoms of supraspinatus tendinitis are usually relieved, but its recurrence is common, which affects the patient’s life quality and leads to calcium or other pathological changes[6]. One of the main reasons for the high probability of recurrence is the lack of objective curative measures[7]. At present, the visual analogue scale (VAS) and Constant-Murley score (CMS) are often utilized to evaluate the pain and function of the shoulder and to judge the effect of treatment[8,9]. The calculation of these two scores mainly depends on the patient’s feelings and physical examination. Although simple and easy to perform, they are highly subjective. Current research has indicated that VAS and CMS have difficulty in accurately assessing the real fact of treatment effects and prognosis[10,11].
Although magnetic resonance imaging is the most accurate tool in the diagnosis of supraspinatus tendinitis, it is not suitable for the evaluation of treatment efficacy because frequent assessment is unrealistic[7]. With the expansion of ultrasound applications, musculoskeletal ultrasound is increasingly popular. Baumer et al[12] demonstrated that ultrasound was feasible and repeatable in diagnosing supraspinatus tendinitis. The pathological process of supraspinatus tendinitis can be divided into three stages including edema and hemorrhage, chronic tendinitis and tendon rupture. The stiffness of muscles will change correspondingly at different pathological stages, leading to the differences in tissue elasticity[13,14].
Shear wave elastography (SWE) can quantitatively analyze the tissue elasticity in the targeted region of interest by measuring the Young’s modulus (YM) value[15]. It has been applied in the differential diagnosis of benign and malignant tumors[16]. Beason et al[17] proposed that SWE can be used to detect the difference in the YM value between the normal supraspinatus and its fatty changes. At present, it is generally believed that the tissue elasticity of the supraspinatus muscle should gradually return to a normal state after systemic treatment[18]. Therefore, SWE is hoped to be used for the evaluation of the therapeutic effect of supraspinatus tendinitis. This study observed the changes in the YM value of patients with supraspinatus tendinitis during treatment and tried to guide the treatment according to the YM value in order to explore the role of SWE in guiding the treatment of supraspinatus tendinitis.
Patients with supraspinatus tendinitis treated in Jiading District Central Hospital Affiliated Shanghai University of Medicine and Health Sciences from October 2018 to January 2020 were recruited. The inclusion criteria were as follows: (1) Patients meeting the diagnostic criteria of supraspinatus tendinitis[19]; (2) Patients did not receive other treatments during the recruitment; and (3) Patients cooperated with treatment and obeyed the arrangement voluntarily. The exclusion criteria were as follows: (1) Patients with comorbidities such as shoulder fractures, periarthritis, local infection, calcified tendinitis and other symptoms affecting treatment; (2) Patients with comorbidities such as severe cardiovascular and cerebrovascular diseases, medical diseases including liver, kidney or hematopoietic system, mental illness, etc.; and (3) Pregnant and lactating women.
In total, 87 patients with supraspinatus tendinitis were included in this study, including 46 males and 41 females, aged 51.34 ± 6.25 years. The disease duration was 2 mo-3 years. Meanwhile, 30 healthy volunteers were enrolled as the control group, including 15 males and 15 females. All patients signed an informed consent form. The study was approved by the Ethics Committee of Jiading District Central Hospital Affiliated Shanghai University of Medicine and Health Sciences.
An Aplio i800 (Cannon Medical Systems Corp, Tochigi-ken, Japan) with PLI-1205BX linear array probe (5-18MHz) was used. The participants remained seated away from the examiner and were examined using the modified Crass posture[20]. We placed the probe lightly on the shoulders of the participants and after clearly showing the supraspinatus muscle on a gray-scale ultrasonic image, we recorded the ultrasound characteristics of the supraspinatus muscle, including the echo, morphology, edge and movement of muscle fibers. Subsequently, we performed an SWE inspection. After setting the region of interest, we saved the SWE image and recorded the YM value of the region of interest.
VAS was used for the detection of the pain level: 0 for no pain, 1-3 for mild pain, 4-6 for moderate pain (sleep affected) and 7-10 for severe pain (sleep and appetite affected)[21]. CMS was used to evaluate the patient’s shoulder joint function (100 points in total): 80-100 for good function, 60-79 for moderate function and < 60 for poor function[22]. The curative effect was defined according to the changes of VAS and CMS after treatment: VAS = 0 and CMS > 80 for recovered, ΔVAS and ΔCMS ≥ 60% for significantly effective, 60% > ΔVAS and ΔCMS ≥ 30% for valid and ΔVAS and ΔCMS < 30% for invalid.
The treatment of supraspinatus tendinitis was divided into four courses with each course spanning 7 d. VAS, CMS and SWE were evaluated after each course. Patients with VAS < 3 received nonpharmacological treatment such as massage therapy, and patients were required to perform functional rehabilitation training to avoid excessive strain. Patients with VAS ≥ 3 or pain progression received additional paracetamol tablets and tizanidine hydrochloride tablets. Patients were ordered to take three paracetamol tablets (0.5 g for each tablet) a day for 5 consecutive days and pause for 2 d. The daily dose of tizanidine hydrochloride tablets was less than 12 mg in one course. If patients with VAS ≥ 7 and still invalid by the mentioned treatment, then a local injection treatment was given within one course.
After all treatments were completed, patients who achieved significant effects or recovery were grouped according to the voluntary principle. Patients continuing to receive treatment according to the YM value were included in the continued treatment group. Patients who stopped receiving treatments were included in the stopped treatment group. The SWE images in the continued treatment group were collected after each course of the treatment, and the treatment was stopped when the average YM values in the continued treatment group showed no statistical difference with that in the control group. If the average YM value increased, then the treatment was terminated after a maximum of four courses. All patients were followed up for 1 year, which included a telephone interview every 3 mo. The recurrence of the supraspinatus tendinitis during the follow-up period was defined as the endpoint event. The difference in the recurrence rates between the continued treatment group and the stopped treatment group were compared (Figure 1).
SPSS (version 22.0, SPSS Inc., Chicago, IL, United States) and Medcalc (Version 22.0.1, MedCalc Software, Ostend, Belgium) were used for statistical analysis. The numerical data were expressed as mean ± standard deviation, and independent sample t-tests were used for comparison. Univariate repeated measures analysis of variance was used to analyze the changes of VAS, CMS and YM value under different courses of treatment. Spearman was performed to analyze the correlation between YM values and VAS and CMS. Kaplan-Meier was used to calculate the PCa biochemical recurrence rate and plot a survival curve. Statistical significance was defined as 2-tailed P < 0.05 for all tests.
The SWE images of the patients with supraspinatus tendinitis and healthy volunteers are shown in Figure 2. The SWE images of supraspinatus muscles in healthy volunteers were mainly blue, while the SWE images of patients with supraspinatus tendinitis showed local red and green regions (Figure 2A and 2B). The red area indicated a harder piece of muscle tissue, suggesting that the patient was in a chronic tendinitis stage. The average YM value of the patients with supraspinatus tendinitis was 60.61 ± 11.53 kPa, which was significantly higher than that of healthy volunteers (26.12 ± 4.03 kPa) (t = 26.344, P < 0.001).
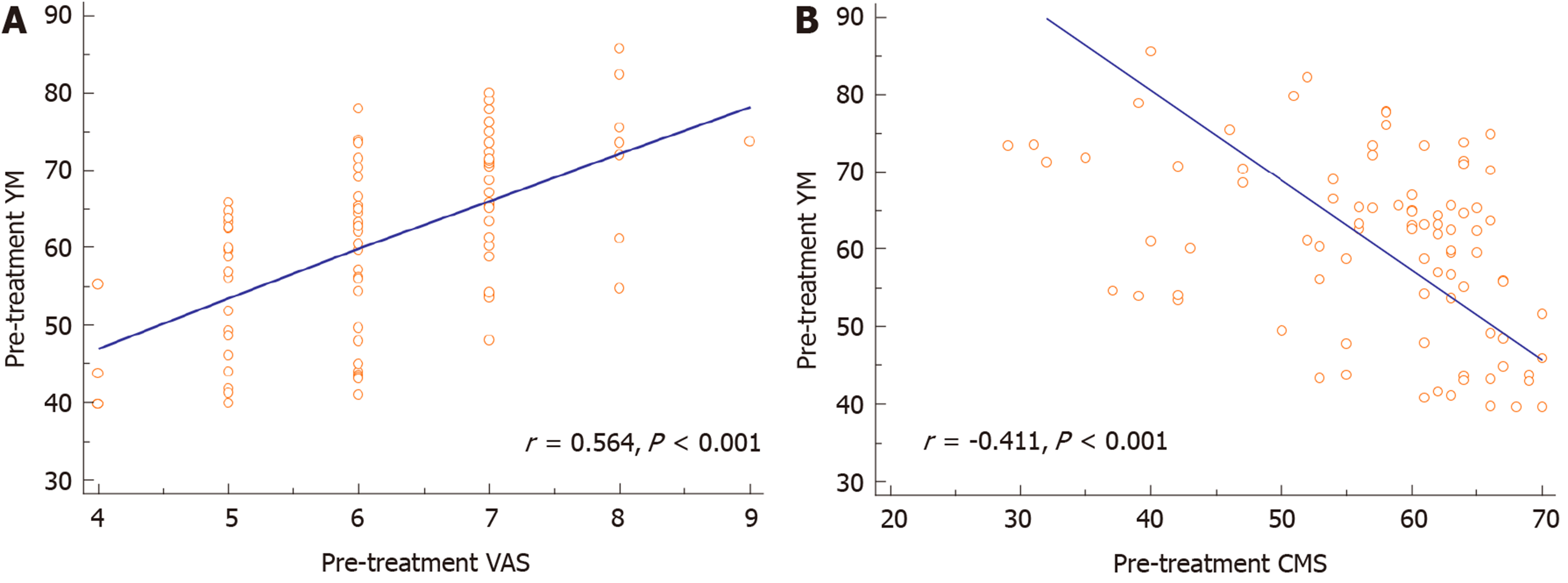
The correlation analysis between the YM value and VAS and CMS in patients with supraspinatus tendinitis is shown in Figure 3A and 3B. The YM value was positively correlated with VAS (r = 0.564, P < 0.001) and negatively correlated with CMS (r = -0.411, P < 0.001).
The treatment of supraspinatus tendinitis was divided into four courses. By comparing the VAS, CMS and YM values in different courses, it revealed that the overall trend of VAS values decreased (FVAS = 208.889, PVAS < 0.001), and the decreased degree was the greatest in course 1. The decreased degree did not change as much thereafter (Figure 4A). It showed an increasing trend in CMS during different courses (FCMS = 278.355, PCMS < 0.001). Among them, the increased degree during course 1 was relatively obvious, and the increased degree during other courses decreased gradually (Figure 4B). The overall trend of YM values decreased in different courses (FYM = 237.363, PYM < 0.001). It was worth noting that the decreased degree was similar in different courses, and it did not decrease significantly during course 1 (Figure 4C).
After the end of the treatment, the average VAS value was significantly lower than that before treatment, and the average CMS value was significantly higher (t = 14.278, P < 0.001; t = 8.074, P < 0.001). The average YM value was also lower than that before treatment (t = 13.443, P < 0.001), but still higher than the average YM value of the control group (t = 9.643, P < 0.001) (Table 1).
| Indicators | Pre-treatment | Course 1 | Course 2 | Course 3 | Course 4 | F | P value |
| VAS | 6.17 ± 1.05 | 4.08 ± 2.20 | 3.79 ± 2.09 | 3.45 ± 1.90 | 3.08 ± 1.73 | 208.889 | < 0.001 |
| CMS | 57.24 ± 9.92 | 64.21 ± 12.96 | 68.76 ± 14.95 | 71.84 ± 16.28 | 75.09 ± 18.08 | 278.355 | < 0.001 |
| YM value, kPa | 60.61 ± 11.53 | 52.86 ± 11.26 | 45.70 ± 11.46 | 41.67 ± 10.99 | 37.94 ± 10.71 | 237.363 | < 0.001 |
The clinical efficacy of supraspinatus tendinitis is shown in Table 2. Among them, 17 patients recovered, 52 patients were significantly effective, 18 were valid, and no patient was invalid. The overall treatment efficiency was 79.31%.
| Total patients | Recovered | Significantly effective | Valid | Invalid | Overall efficiency |
| 87 | 17 (19.5) | 52 (59.8) | 18 (20.7) | 0 | 79.31% |
Of the 69 patients with significant effectiveness or recovery, 35 patients continued treatment, and the remaining 34 patients stopped treatment. All patients with supraspinatus tendinitis received a 1-year follow-up (Figure 5). The follow-up results showed that only 3 patients recurred in the continued treatment group. The cumulative recurrence free rate was 91.43%. Twelve patients recurred in the stopped treatment group. The cumulative recurrence free rate was 64.71%, which was significantly lower than that of the continued treatment group (Logrank X2 = 7.379, P = 0.007).
A total of 87 patients with supraspinatus tendinitis were included in this study. SWE was performed while routinely assessing the improvement of pain and joint activity during treatment by VAS and CMS, and the YM value of the supraspinatus was recorded to explore the role of SWE in evaluating the therapeutic effect of sup-raspinatus tendinitis.
Muscle elasticity is related to its biological function, and the measurement of muscle elasticity helps evaluate its functional status[23]. SWE can quantitatively analyze the stiffness of the lesion tissue by measuring the YM value[24]. In this study, by comparing the SWE images of patients with supraspinatus tendinitis and healthy volunteers, it showed that the SWE images of the supraspinatus in healthy volunteers tended to be blue, while the SWE images of patients with supraspinatus tendinitis showed regional red and green areas. It indicated that the muscle stiffness of patients with supraspinatus tendinitis is greater than that of healthy people. SWE is feasible for observing the muscle stiffness of the supraspinatus muscle at different pathological stages[19]. In the early stage, edema and bleeding appear on the supraspinatus muscle, the tissue is not fibrotic and the image of SWE is green. In the stage of chronic tendinitis, the muscles become fibrotic, scar tissue is forming, muscle stiffness is increased and the image of SWE is red. In the stage of tendon rupture, the synovial fluid in the joint cavity enters the fissure due to the obvious fissure formed at the stump and the SWE image at the fissure is green[12]. In this study, by comparing the YM value of the patients with supraspinatus tendinitis, it showed that the average YM value of the patients is greater than that of healthy volunteers. It suggested that the stiffness of the supraspinatus tendinitis was greater than that of the healthy people, which is in line with the report by Hatta et al[25].
Clinically, the evaluation of the severity and efficacy of the supraspinatus tendinitis depends on the subjective feeling among which the VAS and the CMS are popular[26]. This study revealed that the YM value of patients with supraspinatus tendinitis was positively correlated with VAS and negatively correlated with CMS, indicating that the more painful the feeling and the more limited the joint movement, the harder the supraspinatus muscle. It suggested that the YM value of SWE can also be used for the diagnosis and efficacy evaluation of supinastomyosus tendinitis.
In order to observe in detail the changes in pain, joint mobility and muscle elasticity of patients with supraspinatus tendinitis during treatment, the VAS, CMS and YM values were recorded after each treatment course. The results showed that the overall VAS and YM value showed a downward trend, and the overall CMS showed an upward trend. However, it is worth noting that the degree of change in VAS and CMS was the most obvious in the first course, and the degree of change in the other courses decreased gradually. The degree of change of the YM value in different courses was similar. This may be due to the placebo effect during treatment, which is subjectively considered to be a significant reduction in pain (YM value showed that the hardness change was not obvious) after receiving treatment. We believe that the assessment of efficacy may be inaccurate due to the placebo effect, and treatment may be terminated prematurely.
In this study, the effective rate of the treatment of supraspinatus tendinitis was 79.31%, which was similar to the results of the study by Seil et al[27]. In order to further explore the role of SWE in guiding the treatment of supraspinatus tendinitis, 69 patients with significantly effective and recovery were divided into two groups according to the voluntary principle. Among them, 34 patients stopped treatment, and 35 patients continued treatment according to the YM value. The treatment was discontinued until the patients’ average YM value was not statistically different from that of the control group. After 1 year of follow-up, the cumulative relapse-free rate in the stopped treatment group was 64.71%, which was similar to the result of Gao[28]. The recurrence rate in the continued treatment group was significantly lower than that in the stopped treatment group, indicating that the treatment according to the YM value was more thorough and the recurrence rate was lower. Now the curative effect evaluation method adopted by the stopped treatment group is popular, and the decision basis is the patient’s pain feeling. We believe that the decision based on the subjective feelings of the patient will lead to incomplete treatment, and they are more likely to relapse.
The limitation of this study is that the YM value of supraspinatus tendinitis can also be affected by labor intensity, age, etc. Therefore, the investigation of the role of SWE in the evaluation of supraspinatus tendinitis remains to be done through further large-scale studies. The present study plans to comprehensively analyze the patient’s disease status according to the physical conditions, labor conditions and other conditions of different patients to objectively reveal the supraspinatus elasticity through the YM value in order to individualize the assessment of different patients.
In conclusion, SWE can objectively indicate the severity of supraspinatus tendinitis by detecting the YM value. The determination of the treatment according to the YM value may obtain a better treatment efficacy and a lower relapse rate of supraspinatus tendinitis.
The symptoms of supraspinatus tendinitis are usually relieved after treatment, but its recurrence is common. One of the reasons for recurrence is the lack of objective curative measures. The visual analogue scale (VAS) and Constant-Murley score (CMS) are used to evaluate the pain and function of the shoulder by the patient’s complaint and physical examination. Due to the strong subjectivity, the accurate assessment of treatment efficacy and disease prognosis is limited.
The muscle stiffness of supraspinatus tendinitis will change correspondingly at different pathological stages. Shear wave elastography (SWE) can quantitatively analyze the tissue elasticity in the targeted region of interest by measuring the Young’s modulus (YM) value. At present, it is generally believed that the tissue elasticity of the supraspinatus muscle should gradually return to a normal state after systemic treatment. Therefore, SWE is may be used for the evaluation of the therapeutic effect of the supraspinatus tendinitis.
In this study, we evaluated the improvement of pain and joint activity during treatment by VAS and CMS. We performed a SWE test and recorded the YM value of supraspinatus tendinitis. The aim of our study was to investigate the role of SWE in evaluating the diagnosis and treatment outcome of supraspinatus tendinitis.
A total of 87 patients with supraspinatus tendinitis were recruited in this study, while 30 healthy volunteers were enrolled as the control group. VAS and CMS were used for the detection of shoulder pain and function. SWE was performed, and the YM value of the supraspinatus for each patient was recorded. By comparing the differences in YM values between supraspinatus tendinitis and healthy volunteers, we explored the role of the YM value in the diagnosis of supraspinatus tendinitis. After treatment, the patients who achieved significantly effective and cured were grouped. The patients in the continued treatment group continued to receive treatment according to the YM value, and the remaining patients who stopped receiving treatment were included in the stopped treatment group. All patients were followed up for 1 year, and the difference in recurrence rate between the two groups was compared.
This study revealed that the pretreatment YM value of patients with supraspinatus tendinitis was positively correlated with VAS (r = 0.564) and negatively correlated with CMS (r = -0.411), indicating that the YM value can also be used to evaluate the severity of supraspinatus tendinitis. The degree of change of the YM value, VAS and CMS during the treatment of supraspinatus tendinitis were analyzed. It suggested that the YM value was more objective than VAS and CMS. The cumulative recurrence free rate in the continued treatment group (91.43%) was significantly higher than that of the stopped treatment group (64.71%). It indicated that the treatment according to the YM value was more thorough and the recurrence rate was lower.
Compared with VAS and CMS, the YM value of SWE can more objectively and accurately evaluate the severity and therapeutic effect of supraspinatus tendinitis. It is more valuable in the management of supinastomy tendinitis.
The YM value is contributed to reducing the recurrence rate of supraspinatus tendinitis. However, the YM value is affected by a series of factors such as physical fitness, labor strength, age, etc. In order to assess the YM value more accurately, future studies to more accurately match the general data of different groups are planned. Therefore, the specified assessment is expected to be implemented in a future study.
The authors wish to thank all the study participants, research staff and students who participated in this work.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Devonald MAJ S-Editor: Wang JL L-Editor: Filipodia E-Editor: Liu JH
| 1. | Merolla G, Singh S, Paladini P, Porcellini G. Calcific tendinitis of the rotator cuff: state of the art in diagnosis and treatment. J Orthop Traumatol. 2016;17:7-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 68] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 2. | Chianca V, Albano D, Messina C, Midiri F, Mauri G, Aliprandi A, Catapano M, Pescatori LC, Monaco CG, Gitto S, Pisani Mainini A, Corazza A, Rapisarda S, Pozzi G, Barile A, Masciocchi C, Sconfienza LM. Rotator cuff calcific tendinopathy: from diagnosis to treatment. Acta Biomed. 2018;89:186-196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 52] [Reference Citation Analysis (0)] |
| 3. | Louwerens JK, Veltman ES, van Noort A, van den Bekerom MP. The Effectiveness of High-Energy Extracorporeal Shockwave Therapy Versus Ultrasound-Guided Needling Versus Arthroscopic Surgery in the Management of Chronic Calcific Rotator Cuff Tendinopathy: A Systematic Review. Arthroscopy. 2016;32:165-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 4. | Bannuru RR, Flavin NE, Vaysbrot E, Harvey W, McAlindon T. High-energy extracorporeal shock-wave therapy for treating chronic calcific tendinitis of the shoulder: a systematic review. Ann Intern Med. 2014;160:542-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 68] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 5. | van Rijn RM, Huisstede BM, Koes BW, Burdorf A. Associations between work-related factors and specific disorders of the shoulder--a systematic review of the literature. Scand J Work Environ Health. 2010;36:189-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 321] [Cited by in RCA: 272] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 6. | Hutchinson JL, Gusberti D, Saab G. Changing appearance of intraosseous calcific tendinitis in the shoulder with time: A case report. Radiol Case Rep. 2019;14:1267-1271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Spall BF, Fransson BA, Martinez SA, Wilkinson TE. Tendon Volume Determination on Magnetic Resonance Imaging of Supraspinatus Tendinopathy. Vet Surg. 2016;45:386-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Heller GZ, Manuguerra M, Chow R. How to analyze the Visual Analogue Scale: Myths, truths and clinical relevance. Scand J Pain. 2016;13:67-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 355] [Article Influence: 39.4] [Reference Citation Analysis (0)] |
| 9. | Vrotsou K, Ávila M, Machón M, Mateo-Abad M, Pardo Y, Garin O, Zaror C, González N, Escobar A, Cuéllar R. Constant-Murley Score: systematic review and standardized evaluation in different shoulder pathologies. Qual Life Res. 2018;27:2217-2226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 119] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 10. | Cho NS, Lee BG, Rhee YG. Radiologic course of the calcific deposits in calcific tendinitis of the shoulder: does the initial radiologic aspect affect the final results? J Shoulder Elbow Surg. 2010;19:267-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 69] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 11. | Ioppolo F, Tattoli M, Di Sante L, Attanasi C, Venditto T, Servidio M, Cacchio A, Santilli V. Extracorporeal shock-wave therapy for supraspinatus calcifying tendinitis: a randomized clinical trial comparing two different energy levels. Phys Ther. 2012;92:1376-1385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | Baumer TG, Davis L, Dischler J, Siegal DS, van Holsbeeck M, Moutzouros V, Bey MJ. Shear wave elastography of the supraspinatus muscle and tendon: Repeatability and preliminary findings. J Biomech. 2017;53:201-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 13. | Vasishta A, Kelkar A, Joshi P, Hapse R. The value of sonoelastography in the diagnosis of supraspinatus tendinopathy-a comparison study. Br J Radiol. 2019;92:20180951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Crema MD, Jarraya M, Engebretsen L, Roemer FW, Hayashi D, Domingues R, Skaf AY, Guermazi A. Imaging-detected acute muscle injuries in athletes participating in the Rio de Janeiro 2016 Summer Olympic Games. Br J Sports Med. 2018;52:460-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Leong SS, Wong JHD, Md Shah MN, Vijayananthan A, Jalalonmuhali M, Ng KH. Shear wave elastography in the evaluation of renal parenchymal stiffness in patients with chronic kidney disease. Br J Radiol. 2018;91:20180235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 16. | Taljanovic MS, Gimber LH, Becker GW, Latt LD, Klauser AS, Melville DM, Gao L, Witte RS. Shear-Wave Elastography: Basic Physics and Musculoskeletal Applications. Radiographics. 2017;37:855-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 455] [Article Influence: 56.9] [Reference Citation Analysis (0)] |
| 17. | Beason DP, Hsu JE, Marshall SM, McDaniel AL, Temel RE, Abboud JA, Soslowsky LJ. Hypercholesterolemia increases supraspinatus tendon stiffness and elastic modulus across multiple species. J Shoulder Elbow Surg. 2013;22:681-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 18. | Rosskopf AB, Ehrmann C, Buck FM, Gerber C, Flück M, Pfirrmann CW. Quantitative Shear-Wave US Elastography of the Supraspinatus Muscle: Reliability of the Method and Relation to Tendon Integrity and Muscle Quality. Radiology. 2016;278:465-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 124] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 19. | de Boer RD, Marinus J, van Hilten JJ, Huygen FJ, van Eijs F, van Kleef M, Bauer MC, van Gestel M, Zuurmond WW, Perez RS. Distribution of signs and symptoms of complex regional pain syndrome type I in patients meeting the diagnostic criteria of the International Association for the Study of Pain. Eur J Pain. 2011;15:830.e1-830.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Hyvelin JM, Gaud E, Costa M, Helbert A, Bussat P, Bettinger T, Frinking P. Characteristics and Echogenicity of Clinical Ultrasound Contrast Agents: An In Vitro and In Vivo Comparison Study. J Ultrasound Med. 2017;36:941-953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 21. | Clinical pain management: a practical guide Clinical pain management: a practical guide Lynch Mary Craig Kenneth Peng Philip Wiley-Blackwell £68.99 388pp 9781444330694 1444330691 [Formula: see text]. Emerg Nurse. 2011;19:9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Oh DG, Yoo KT. The effects of therapeutic exercise using PNF on the size of calcium deposits, pain self-awareness, and shoulder joint function in a calcific tendinitis patient: a case study. J Phys Ther Sci. 2017;29:163-167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Ishii T, Narita N, Endo H. Evaluation of jaw and neck muscle activities while chewing using EMG-EMG transfer function and EMG-EMG coherence function analyses in healthy subjects. Physiol Behav. 2016;160:35-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Sande JA, Verjee S, Vinayak S, Amersi F, Ghesani M. Ultrasound shear wave elastography and liver fibrosis: A Prospective Multicenter Study. World J Hepatol. 2017;9:38-47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 25. | Hatta T, Giambini H, Uehara K, Okamoto S, Chen S, Sperling JW, Itoi E, An KN. Quantitative assessment of rotator cuff muscle elasticity: Reliability and feasibility of shear wave elastography. J Biomech. 2015;48:3853-3858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 86] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 26. | Hackett L, Millar NL, Lam P, Murrell GA. Are the Symptoms of Calcific Tendinitis Due to Neoinnervation and/or Neovascularization? J Bone Joint Surg Am. 2016;98:186-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 27. | Seil R, Litzenburger H, Kohn D, Rupp S. Arthroscopic treatment of chronically painful calcifying tendinitis of the supraspinatus tendon. Arthroscopy. 2006;22:521-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 110] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 28. | Gao Y. Observations on the efficacy of acupuncture plus tuina therapy in treating supraspinatus tendinitis. J Acupunct Tuina Sci. 2009;7:94-97. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |