Published online Jul 26, 2020. doi: 10.12998/wjcc.v8.i14.2893
Peer-review started: May 19, 2020
First decision: June 4, 2020
Revised: June 15, 2020
Accepted: June 29, 2020
Article in press: June 29, 2020
Published online: July 26, 2020
Processing time: 66 Days and 7.6 Hours
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 has spread rapidly around the world and is a significant threat to global health. Patients in the Neonatal Surgery Department have rapidly progressing diseases and immature immunity, which makes them vulnerable to pulmonary infection and a relatively higher mortality. This means that these patients require multidisciplinary treatment including early diagnosis, timely transport, emergency surgery and intensive critical care. The COVID-19 pandemic poses a threat to carrying out these treatments. To provide support for the health protection requirements of the medical services in the Neonatal Surgery Department, we developed recommendations focusing on patient transport, surgery selection and protection requirements with the aim of improving treatment strategies for patients and preventing infection in medical staff during the current COVID-19 pandemic.
Core tip: We have developed recommendations focused on practices such as patient transport, surgery selection and protection requirements in the Neonatal Surgery Department, with the aim of improving treatment strategies for patients and preventing infection in medical staff during the current coronavirus disease 2019 pandemic.
- Citation: Ma LS, Zhao YL, Wei YD, Liu C. Recommendations for perinatal and neonatal surgical management during the COVID-19 pandemic. World J Clin Cases 2020; 8(14): 2893-2901
- URL: https://www.wjgnet.com/2307-8960/full/v8/i14/2893.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i14.2893
Since December 2019, the novel coronavirus infection has spread rapidly, posing a significant threat to global health. As a tertiary referral hospital and one of the National Clinical Research Centers for Child Health and the National Children’s Medical Centers, our center provides care for a large proportion of prenatal and neonatal cases in north China and has accumulated plentiful practical experience in patient transport and treatment. Following the latest national recommendations for diagnosis and treatment of coronavirus disease 2019 (COVID-19), we have developed recommendations focusing on practices such as patient transport, surgery selection and protection requirements in the neonatal surgery department, aiming to improve treatment strategies for patients and prevent infection in medical staff during the current COVID-19 pandemic.
This recommendation is in accordance with the latest “Guideline for the Diagnosis and Treatment of COVID-19 Infections” (version 7) (National Health Committee of China)[1], “The Coronavirus Disease 2019 (COVID-19) Treatment Guidelines” published by the National Institutes of Health (United States) (Updated: May 12, 2020)[2] and other literature and experts’ consensus related to COVID-19 published recently, combined with the procedures performed in the institution and our previous clinical treatment experience[3-8].
COVID-19 is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which has been identified as the seventh type of coronavirus to infect humans[9]. These coronaviruses are classified into four genera, based on their genome characteristics: α-CoV, β-CoV, γ-CoV and δ-CoV[10]. According to deep sequencing, SARS-CoV-2 belongs to β-CoV[9].
It is thought that SARS-CoV-2 is spread mainly through respiratory droplets or close contact[11]. In the later stage of infection, the virus has also been detected in anal swabs from patients, which suggests the possibility of transmission via the oral-fecal route[11]. However, there is currently no evidence of vertical transmission of SARS-CoV-2 via intrauterine infection in women who develop COVID-19 pneumonia. In addition, there are no reports of patients’ breast milk testing positive for the virus. However, after birth a newborn is susceptible to the virus due to person-to-person spread[12-14].
The epidemiology of COVID-19 in neonates may have its own pattern. Droplet transmission and close contact with infected individuals are the main causes of SARS-CoV-2 infection in neonates, and most neonatal cases have been found in infected family clusters[15]. A study on 9 infected infants reported by Wei et al[16] found that all these infants belonged to a family cluster. The first infected neonate in China, a 17-day-old male infant, was reported to contract the infection via contact with his parents[17].
According to current epidemiological data, COVID-19 has an incubation period ranging from 1 to 14 d, but mainly from 3 to 7 d[18]. Clinical symptoms in pediatric patients are relatively milder compared with those in adult patients. Most infected children have mild clinical manifestations. They may be asymptomatic or have fever, dry cough and fatigue. Some infected children experience gastrointestinal symptoms such as nausea, vomiting and diarrhea. Most pediatric patients recover within 1–2 wk after disease onset. Few may progress to lower respiratory tract infections[6,16,17,19].
Real-time reverse transcriptase polymerase chain reaction of nasal and pharyngeal swabs, sputum, blood, feces and urine specimens can be used for the diagnosis of COVID-19[20]. A chest computed tomography (CT) scan can help physicians monitor disease changes and evaluate therapeutic effects[21].
Neonates can develop a range of complex and diverse diseases mainly involving hereditary factors and other abnormalities. As a result of their anatomical and physiological characteristics (especially their immature immunity), neonate diseases progress quickly. Without timely treatment these patients can deteriorate within a short time with high mortality. Due to the advances in prenatal diagnostic techniques, more and more patients who require surgical treatment, such as those with congenital diaphragmatic hernia, congenital intestinal atresia and omphalocele, can be detected by antenatal ultrasonography. Patients admitted to the hospital are mainly transferred from outpatient services, emergency departments and other hospitals.
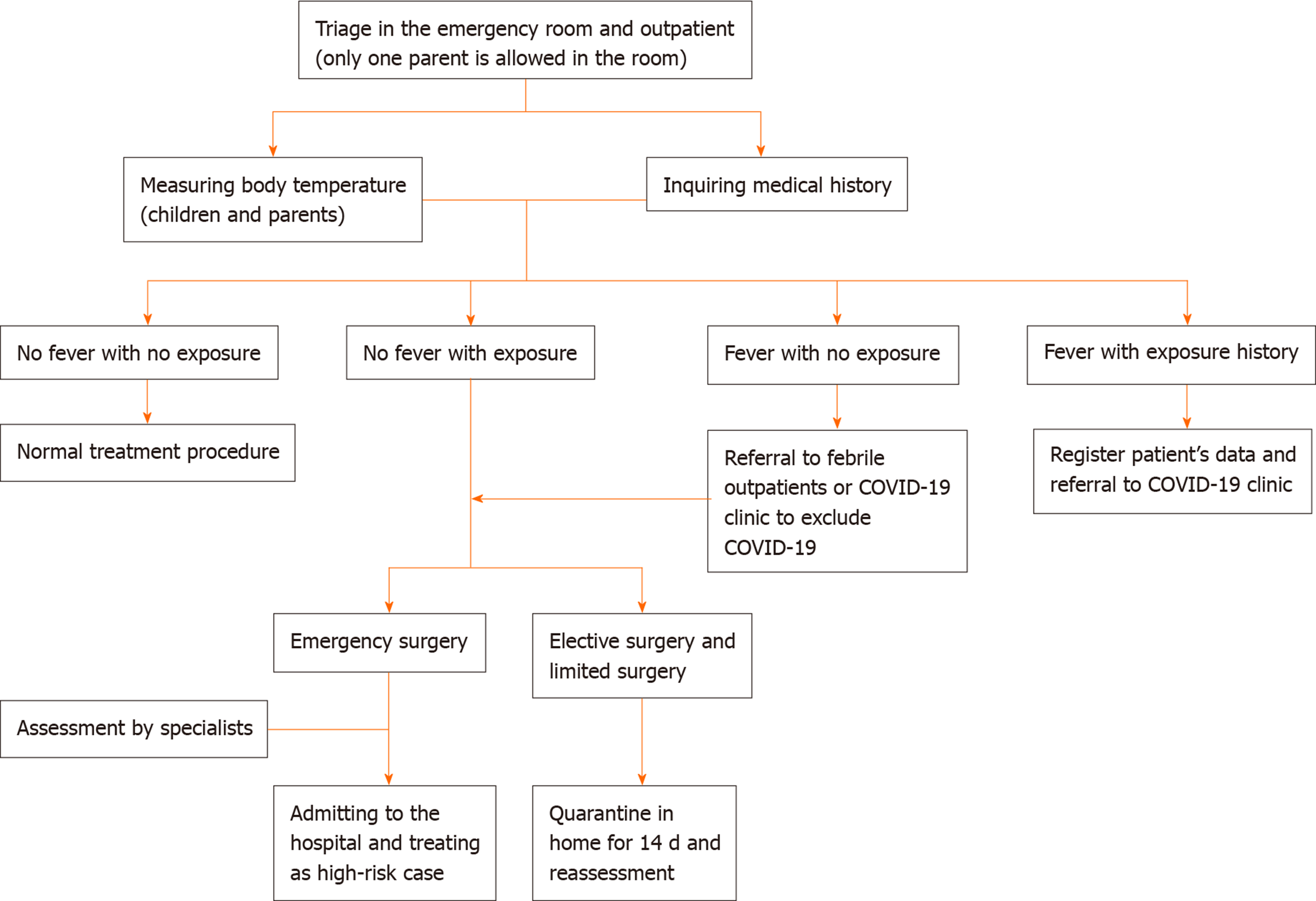
The evaluation and management process of patients in the emergency and outpatient departments is as follows.
Only one parent is allowed to accompany a child into the consulting room; body temperature and medical history are taken at the entrance.
All patients with suspected COVID-19 should attend the febrile outpatient or COVID-19 clinic before visiting the neonatal surgery clinic. Patients with symptoms such as nausea, vomiting and diarrhea due to diseases such as congenital hypertrophic pyloric stenosis, Hirschsprung disease and congenital intestinal malrotation should be differentiated from COVID-19 patients. We recommend real-time reverse transcriptase polymerase chain reaction and a chest CT scan for patients with suspected COVID-19 in addition to routine examinations. COVID-19 pneumonia manifests with chest CT imaging abnormalities early and in asymptomatic patients. Multiple patchy ground glass opacities in bilateral multiple lobular with periphery distribution are typical chest CT imaging features of the COVID-19 pneumonia[22]. Combining assessment of imaging features with clinical and laboratory findings could facilitate early diagnosis of COVID-19 pneumonia[21]. Patients definitively diagnosed with emergency surgical conditions should be admitted as soon as possible for further treatment. Patients who test positive for SARS-CoV-2 or those highly suspected of having COVID-19 should be transferred to a designated medical institution immediately and should be reported to the local Center for Disease Control and Prevention (Figure 1).
Patients diagnosed prenatally with abnormalities that require surgery, such as congenital diaphragmatic hernia, congenital intestinal atresia, meconium peritonitis and omphalocele, who were born in nonepidemic areas and had no contact with COVID-19 patients, can be transferred under general protection and treated with routine procedures. If patients are in an unstable condition and require emergency surgery, such as for severe congenital diaphragmatic hernia and omphalocele, neonatal surgeons should wait in the delivery room/operating room and perform the operation immediately or transfer the patients to appropriate medical institutions for further treatment after delivery under intensive care and monitoring. For children in a stable condition who require elective surgical treatment, we suggest a remote consultation with neonatal specialists and give conservative treatment and support until the appropriate operation can be performed.
Patients who had a history of epidemiological exposure to COVID-19 or were born in epidemic areas should be transferred to and treated in designated medical institutions for COVID-19. Although there is no evidence of intrapartum transmission, special attention is required to prevent infection in babies born to mothers with COVID-19 pneumonia. Admitting pregnant women with laboratory-confirmed COVID-19 pneumonia to designated medical institutions for COVID-19 and advance notification to the neonatal surgical team before delivery are suggested if the neonates were prenatally diagnosed with conditions that require surgery after birth. According to the proposed management of COVID-19 during pregnancy and puerperium in China, mothers with COVID-19 pneumonia should deliver in a negative pressure ward/operating room. It is recommended that ligation of the umbilical cord is performed early, and the cord is not squeezed. All medical staff should perform these procedures under protection including the use of personal protective equipment (e.g., N95 respirators, face shields, gloves, goggles and gowns)[2] (Figure 2).
Most of the neonatal surgical wards are nonescort wards, and it is better to temporarily cancel parent visiting during the COVID-19 outbreak. In escort wards, only one nucleic acid test-negative patient is allowed in the room. Neonatal care that requires family support such as feeding by the mother and kangaroo care should be suspended. In areas with severe outbreaks, it is suggested that receiving breast milk from outside the hospital should be canceled.
A quarantine chamber is necessary for suspected COVID-19 patients who are identified during the hospitalization period. Quarantine in negative pressure infectious disease wards or airborne infection isolation rooms is approved in principle. A ward with an independent air circulation system is acceptable when negative pressure rooms or airborne infection isolation rooms are unavailable. The babies are placed in warm boxes and cared for by designated medical staff. Infants who test positive for SARS-CoV-2 are immediately transferred to a designated medical institution and other babies in the same ward are isolated and undergo nucleic acid testing. The body temperature of all infants and medical staff in the ward is measured, and anyone who develops fever, dry cough and fatigue is isolated. The living zone in the ward should be independent of the working zone. All clinical procedures should be performed by medical personnel wearing protective equipment such as medical masks and protective hats. It is worth mentioning that hand hygiene is extremely important for the prevention of nosocomial infection.
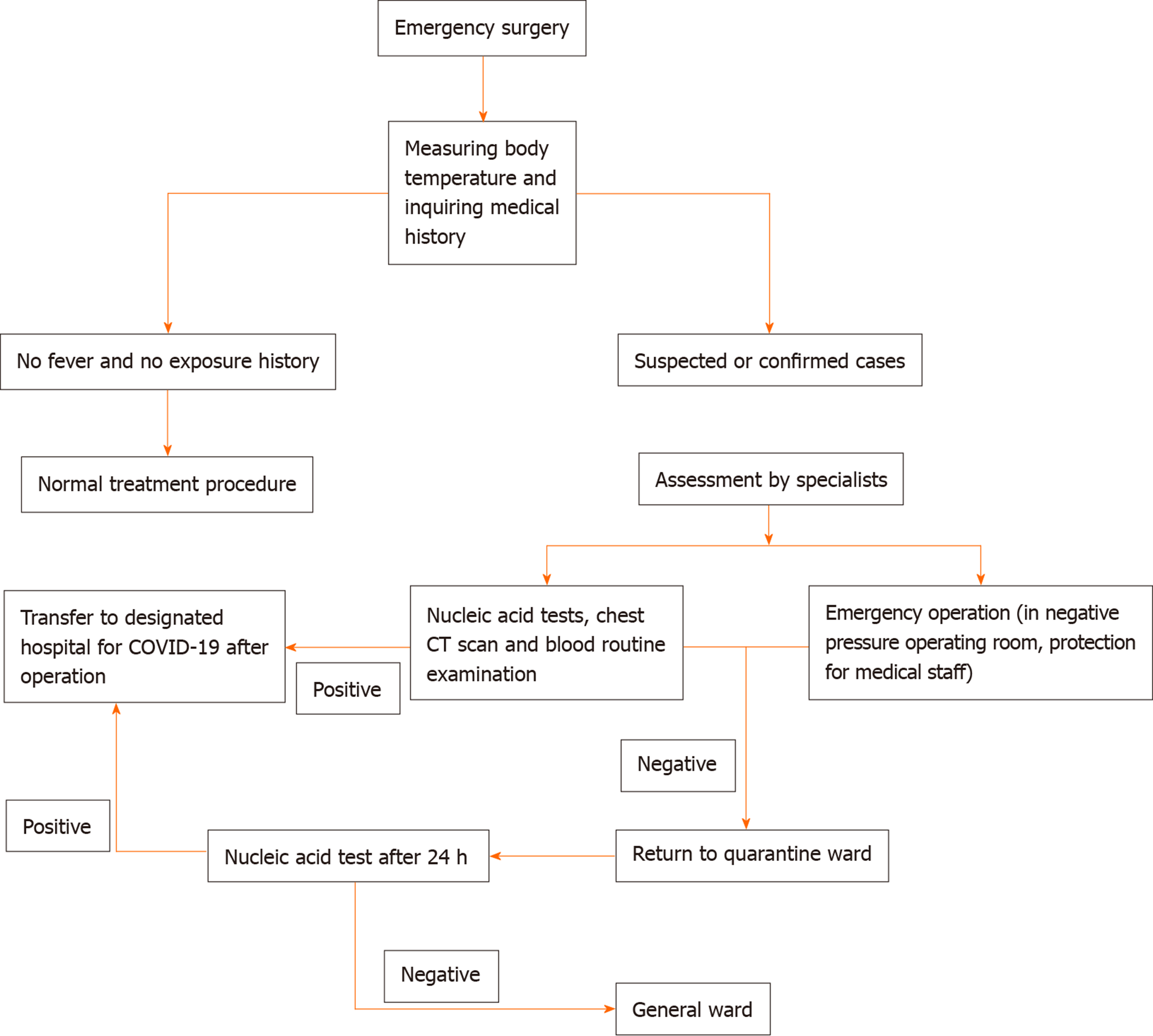
As the majority of operations in the Neonatal Surgery Department are emergency procedures and limited surgery, suspending operations completely is unrealistic. Children with emergency conditions and low risk (no exposure history or symptoms) can be treated using routine procedures. High-risk children (suspected cases) and those with confirmed COVID-19 pneumonia should be transferred to and treated in a designated hospital as suggested above. If there is not enough time for transport or the transfer service is unavailable, surgeons can perform the surgery in a negative pressure operating room in cooperation with the Department of Anesthetics (Figure 3).
We recommend for children who require selective/limited operations that the appropriate time for the operation is decided by the surgeons in coordination with the child’s guardians based on the surgeons’ opinion and local COVID-19 severity.
Strategies for transport of patients with suspected or diagnosed SARS-CoV-2 infection should be formulated in advance. The strategies should be reviewed by an expert committee consisting of specialists in pediatric surgery, anesthesiology, pneumology, infectious disease, radiology and the operating room. Preoperative consultation needs to consider details including transport and hand over of care, surgical program, anesthesia process, organization of the operating suite, transport routes, medical staff protection and environmental disinfection.
Anesthesiologists support most neonatal patients with endotracheal intubation following general anesthesia. Anesthesiologists performing these procedures in patients with SARS-CoV-2 infection require level 3 protection. We suggest placing a disposable filter between the anesthesia breathing circuit and the endotracheal tube in order to reduce pollution[23]. It would be better to achieve intubation by video laryngoscopy if it is available. Moderate sedation and appropriate muscle relaxation before induction are critical for minimizing virus spread through respiratory droplets from coughs. Adaptation of high frequency, small tidal volume ventilation with limited pressure models or high frequency oscillatory ventilation is necessary to avoid pulmonary barotrauma and reduce virus spread. It is highly recommended that a closed endotracheal suction system is used to clear secretions within the endotracheal tube during and after surgery. It is necessary to ensure that patients meet the criteria for returning to the quarantine ward or pediatric intensive care unit before leaving the operating room. Patients should wear masks with nasal catheter oxygen, or they can be escorted by ventilators. All drugs and devices used should be marked and stored in designated areas after disinfection.
If there are any exposure incidents during surgery, a 14 d medical monitor is recommended. Nucleic acid testing is necessary for those who develop symptoms.
Children with no exposure history or symptoms can return to the pediatric intensive care unit for further treatment, and it is suggested that parent visiting is canceled. In escort wards, only one nucleic acid test-negative patient is allowed in each room. Body temperature is measured in all infants and parents in the ward twice a day[7]. Those who develop fever, dry cough and fatigue should be isolated and undergo nucleic acid testing for SARS-CoV-2 and a chest CT scan.
As suggested above, children with confirmed COVID-19 pneumonia should be transferred to and treated in designated medical institutions. All daily clinical procedures should be performed by medical personnel wearing appropriate personal protective equipment.
Oxygen therapy and nebulizer therapy are recommended for patients with mild to moderate hypoxemia. For severe and critical patients with respiratory distress, high-flow nasal cannula oxygen therapy, noninvasive or invasive mechanical ventilation and even extracorporeal membrane oxygenation should be considered[2].
Special attention should be paid to organ protection and supportive treatments as there are reports that SARS-CoV-2 may damage the liver, kidneys and myocardium to some extent. The signs to look for are elevated levels of aminotransferases, increased serum creatinine, blood urea nitrogen, creatine kinase and myoglobin as well as troponin in critical patients[20,24,25].
Early enteral feeding is generally preferred in ill children. Adequate protein delivery is also associated with fewer ventilator days and reduced mortality after adjusting for illness severity[26]. Enteral microbial agents can be used in selected patients.
Children, especially those receiving corticosteroids, are susceptible to secondary infections due to their incomplete immunity. In addition, those who receive mechanical ventilation are susceptible to ventilator-associated pneumonia. According to the Guideline for the diagnosis and treatment of COVID-19 infections (version 7) issued by the National Health Commission of China[1], inappropriate and unnecessary use of antimicrobial therapy, especially an irrational combination use of broad spectrum antibiotics is not advised. The administration of empiric antimicrobial agents should be considered when bacterial pneumonia or sepsis is suspected (e.g., the procalcitonin levels increase) or sputum or blood specimens show clear evidence of etiology. It is, of course, advisable to timely adjust the drug according to antimicrobial drug susceptibility test results and de-escalate or stop antibiotics if there is no evidence of bacterial infection.
According to The Coronavirus Disease 2019 (COVID-19) Treatment Guidelines published by National Institutes of Health, except in the context of a clinical trial, the COVID-19 Treatment Guidelines Panel recommends against the use of non-SARS-CoV-2-specific intravenous immunoglobulin for the treatment of COVID-19[2].
According to the Guideline for the Diagnosis and Treatment of COVID-19 Infections (version 7) issued by the National Health Commission of China, the criteria for deregulating quarantine procedures are normal body temperature for more than 3 d; significant improvement in respiratory symptoms; marked absorption of acute exudative lesions on radiological images; and two consecutive negative nucleic acid test results of samples such as nasal and pharyngeal swabs and sputum with a sampling interval at least 24 h. Patients who meet all the above criteria can discharge from quarantine and then leave the hospital when they meet the discharge criteria for their own surgical conditions.
These caveats include remaining in contact with the local primary medical institutions in the patient’s place of residence and tracking the patient’s condition. Also monitoring the health of the child for 14 d and ensuring family care is provided by one healthy person is recommended.
Mask wearing is encouraged. Hand hygiene, personal protection and disinfection of the baby’s equipment after use are required. Upon discharge, we encourage the patients to revisit the hospital every 2 wk for the 1st mo for follow-up.
Considering the good prognosis of neonates during the COVID-19 pandemic, the involvement of a multidisciplinary team consisting of specialists in obstetrics, maternal-fetal medicine and pediatrics in adjusting the prevention and control strategies for antenatal, intrapartum and postpartum diagnosis, care and treatment, is highly recommended.
We thank all members of the Chinese Society of Obstetrics and Gynecology, the Chinese Society of Pediatrics and the Chinese Neonatologist Association, Chinese Medical Association. The experts who contributed to this manuscript (in order by their contribution to this manuscript) include: Yang-Yu Zhao, Jun-Tao Liu, Xin Wang, Xue-Feng Zhang, Zhi-Chun Feng, Wei Ji and Ying Wang.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Machairas N, Mastoraki A, Pavone V S-Editor: Ma YJ L-Editor: Filipodia E-Editor: Liu JH
| 1. | National Health Commission of the People’s Republic of China. Guideline for the diagnosis and treatment of COVID-19 infections (version 7). 2020. Available from: http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989/files/ce3e6945832a438eaae415350a8ce964.pdf. |
| 2. | COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health. 2020. Available from: https://www.covid19treatmentguidelines.nih.gov/. |
| 3. | Chen ZM, Fu JF, Shu Q, Chen YH, Hua CZ, Li FB, Lin R, Tang LF, Wang TL, Wang W, Wang YS, Xu WZ, Yang ZH, Ye S, Yuan TM, Zhang CM, Zhang YY. Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World J Pediatr. 2020;1-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 331] [Cited by in RCA: 329] [Article Influence: 65.8] [Reference Citation Analysis (0)] |
| 4. | Jin YH, Cai L, Cheng ZS, Cheng H, Deng T, Fan YP, Fang C, Huang D, Huang LQ, Huang Q, Han Y, Hu B, Hu F, Li BH, Li YR, Liang K, Lin LK, Luo LS, Ma J, Ma LL, Peng ZY, Pan YB, Pan ZY, Ren XQ, Sun HM, Wang Y, Wang YY, Weng H, Wei CJ, Wu DF, Xia J, Xiong Y, Xu HB, Yao XM, Yuan YF, Ye TS, Zhang XC, Zhang YW, Zhang YG, Zhang HM, Zhao Y, Zhao MJ, Zi H, Zeng XT, Wang YY, Wang XH; for the Zhongnan Hospital of Wuhan University Novel Coronavirus Management and Research Team, Evidence-Based Medicine Chapter of China International Exchange and Promotive Association for Medical and Health Care (CPAM). A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil Med Res. 2020;7:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 881] [Cited by in RCA: 1136] [Article Influence: 227.2] [Reference Citation Analysis (0)] |
| 5. | Nicola M, O'Neill N, Sohrabi C, Khan M, Agha M, Agha R. Evidence based management guideline for the COVID-19 pandemic - Review article. Int J Surg. 2020;77:206-216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 218] [Cited by in RCA: 211] [Article Influence: 42.2] [Reference Citation Analysis (0)] |
| 6. | Shen K, Yang Y, Wang T, Zhao D, Jiang Y, Jin R, Zheng Y, Xu B, Xie Z, Lin L, Shang Y, Lu X, Shu S, Bai Y, Deng J, Lu M, Ye L, Wang X, Wang Y, Gao L; China National Clinical Research Center for Respiratory Diseases; National Center for Children’s Health, Beijing, China; Group of Respirology, Chinese Pediatric Society, Chinese Medical Association; Chinese Medical Doctor Association Committee on Respirology Pediatrics; China Medicine Education Association Committee on Pediatrics; Chinese Research Hospital Association Committee on Pediatrics; Chinese Non-government Medical Institutions Association Committee on Pediatrics; China Association of Traditional Chinese Medicine, Committee on Children’s Health and Medicine Research; China News of Drug Information Association, Committee on Children’s Safety Medication; Global Pediatric Pulmonology Alliance. Diagnosis, treatment, and prevention of 2019 novel coronavirus infection in children: experts' consensus statement. World J Pediatr. 2020;1-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 362] [Cited by in RCA: 383] [Article Influence: 76.6] [Reference Citation Analysis (0)] |
| 7. | National Children's Medical Center; Children's Hospital of Fudan University. Recommendations for control and prevention of infections for outpatient and emergency clinics and inpatient operations of pediatric orthopedic during the epidemic period of SARS-CoV-2. Linchuang Xiaoer Waike Zazhi. 2020;19:98-103. [DOI] [Full Text] |
| 8. | Wang L, Shi Y, Xiao T, Fu J, Feng X, Mu D, Feng Q, Hei M, Hu X, Li Z, Lu G, Tang Z, Wang Y, Wang C, Xia S, Xu J, Yang Y, Yang J, Zeng M, Zheng J, Zhou W, Zhou X, Zhou X, Du L, Lee SK, Zhou W; Working Committee on Perinatal and Neonatal Management for the Prevention and Control of the 2019 Novel Coronavirus Infection. Chinese expert consensus on the perinatal and neonatal management for the prevention and control of the 2019 novel coronavirus infection (First edition). Ann Transl Med. 2020;8:47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 208] [Article Influence: 41.6] [Reference Citation Analysis (0)] |
| 9. | Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W; China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727-733. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18987] [Cited by in RCA: 17632] [Article Influence: 3526.4] [Reference Citation Analysis (0)] |
| 10. | Su S, Wong G, Shi W, Liu J, Lai ACK, Zhou J, Liu W, Bi Y, Gao GF. Epidemiology, Genetic Recombination, and Pathogenesis of Coronaviruses. Trends Microbiol. 2016;24:490-502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1725] [Cited by in RCA: 1876] [Article Influence: 208.4] [Reference Citation Analysis (0)] |
| 11. | Zhang W, Du RH, Li B, Zheng XS, Yang XL, Hu B, Wang YY, Xiao GF, Yan B, Shi ZL, Zhou P. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect. 2020;9:386-389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1192] [Cited by in RCA: 1219] [Article Influence: 243.8] [Reference Citation Analysis (0)] |
| 12. | Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, Li J, Zhao D, Xu D, Gong Q, Liao J, Yang H, Hou W, Zhang Y. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395:809-815. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2400] [Cited by in RCA: 2272] [Article Influence: 454.4] [Reference Citation Analysis (0)] |
| 13. | Karimi-Zarchi M, Neamatzadeh H, Dastgheib SA, Abbasi H, Mirjalili SR, Behforouz A, Ferdosian F, Bahrami R. Vertical Transmission of Coronavirus Disease 19 (COVID-19) from Infected Pregnant Mothers to Neonates: A Review. Fetal Pediatr Pathol. 2020;39:246-250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 211] [Cited by in RCA: 243] [Article Influence: 48.6] [Reference Citation Analysis (0)] |
| 14. | Schwartz DA. An Analysis of 38 Pregnant Women with COVID-19, Their Newborn Infants, and Maternal-Fetal Transmission of SARS-CoV-2: Maternal Coronavirus Infections and Pregnancy Outcomes. Arch Pathol Lab Med. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 506] [Cited by in RCA: 567] [Article Influence: 141.8] [Reference Citation Analysis (0)] |
| 15. | Zimmermann P, Curtis N. Coronavirus Infections in Children Including COVID-19: An Overview of the Epidemiology, Clinical Features, Diagnosis, Treatment and Prevention Options in Children. Pediatr Infect Dis J. 2020;39:355-368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 714] [Cited by in RCA: 695] [Article Influence: 139.0] [Reference Citation Analysis (0)] |
| 16. | Wei M, Yuan J, Liu Y, Fu T, Yu X, Zhang ZJ. Novel Coronavirus Infection in Hospitalized Infants Under 1 Year of Age in China. JAMA. 2020;323:1313-1314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 469] [Cited by in RCA: 431] [Article Influence: 86.2] [Reference Citation Analysis (1)] |
| 17. | Zeng LK, Tao XW, Yuan WH, Wang J, Liu X, Liu ZS. [First case of neonate infected with novel coronavirus pneumonia in China]. Zhonghua Er Ke Za Zhi. 2020;58:E009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 72] [Reference Citation Analysis (0)] |
| 18. | Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708-1720. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19202] [Cited by in RCA: 18867] [Article Influence: 3773.4] [Reference Citation Analysis (7)] |
| 19. | Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, Tong S. Epidemiology of COVID-19 Among Children in China. Pediatrics. 2020;145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2328] [Cited by in RCA: 2411] [Article Influence: 482.2] [Reference Citation Analysis (0)] |
| 20. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35178] [Cited by in RCA: 30098] [Article Influence: 6019.6] [Reference Citation Analysis (3)] |
| 21. | Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, Fan Y, Zheng C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425-434. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2493] [Cited by in RCA: 2310] [Article Influence: 462.0] [Reference Citation Analysis (0)] |
| 22. | Xu X, Yu C, Qu J, Zhang L, Jiang S, Huang D, Chen B, Zhang Z, Guan W, Ling Z, Jiang R, Hu T, Ding Y, Lin L, Gan Q, Luo L, Tang X, Liu J. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging. 2020;47:1275-1280. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 457] [Cited by in RCA: 491] [Article Influence: 98.2] [Reference Citation Analysis (0)] |
| 23. | Hu YQ, Huang JJ, Wang JH, Tang DX, Dou JF, Cheng QJ, Wang W, Chen ZM, Fu JF, Fang XM, Shu Q. Anesthesia management in pediatric populations suspected of or diagnosed with SARS-CoV-2 infection. Linchuang Xiaoer Waike Zazhi. 2020;19:111-4. [DOI] [Full Text] |
| 24. | Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14869] [Cited by in RCA: 12970] [Article Influence: 2594.0] [Reference Citation Analysis (1)] |
| 25. | Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475-481. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6231] [Cited by in RCA: 6656] [Article Influence: 1331.2] [Reference Citation Analysis (0)] |
| 26. | Wong JJ, Han WM, Sultana R, Loh TF, Lee JH. Nutrition Delivery Affects Outcomes in Pediatric Acute Respiratory Distress Syndrome. JPEN J Parenter Enteral Nutr. 2017;41:1007-1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 56] [Article Influence: 6.2] [Reference Citation Analysis (0)] |