Published online Jul 6, 2020. doi: 10.12998/wjcc.v8.i13.2849
Peer-review started: March 15, 2020
First decision: April 22, 2020
Revised: May 4, 2020
Accepted: May 29, 2020
Article in press: May 29, 2020
Published online: July 6, 2020
Processing time: 113 Days and 22.4 Hours
Pheochromocytomas with inferior vena cava (IVC) or renal vein tumor thrombus are rare. Surgical management is the first choice.
We presented a 42-year-old man with adrenal pheochromocytoma and delayed tumor thrombus detection in the renal vein at the entrance of the IVC three months after adrenalectomy. We performed laparoscopic adrenalectomy during the first surgery and robot-assisted laparoscopic nephrectomy and resection of tumor thrombus during the second surgery.
We report the surgical management of a patient with adrenal pheochromocytoma with tumor thrombus at the entrance of the IVC. Robot-assisted laparoscopic surgery is safe and efficient.
Core tip: We report a rare case of adrenal pheochromocytoma on the left side with delayed detection of tumor thrombus at the entrance of the inferior vena cava and share our experience in surgical management. A similar case has not been reported previously. Nephrectomy is required when the tumor is on the left side and robot-assisted laparoscopic surgery is safe and efficient.
- Citation: Jia Z, Wang BJ, Li X, Zhang X. Pheochromocytoma with delayed tumor thrombus detection in renal vein: A case report. World J Clin Cases 2020; 8(13): 2849-2854
- URL: https://www.wjgnet.com/2307-8960/full/v8/i13/2849.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i13.2849
Pheochromocytomas are rare tumors with an incidence of approximately 0.05% in the population. This tumor is rarer than those that invade the inferior vena cava (IVC) or renal vein, and only a few cases of pheochromocytoma with IVC or renal vein tumor thrombus have been reported in the literature. Surgical management is the first choice for cases without metastasis. We report a case of pheochromocytoma with delayed tumor thrombus detection at the entrance of IVC and present the management of this condition.
A 42-year-old man brought to the hospital presented with an adrenal tumor as shown by abdominal ultrasound examination without any complaints.
The patient had normal blood pressure and no fever, headache, or palpitation.
Abdominal examination showed no palpable mass or tenderness.
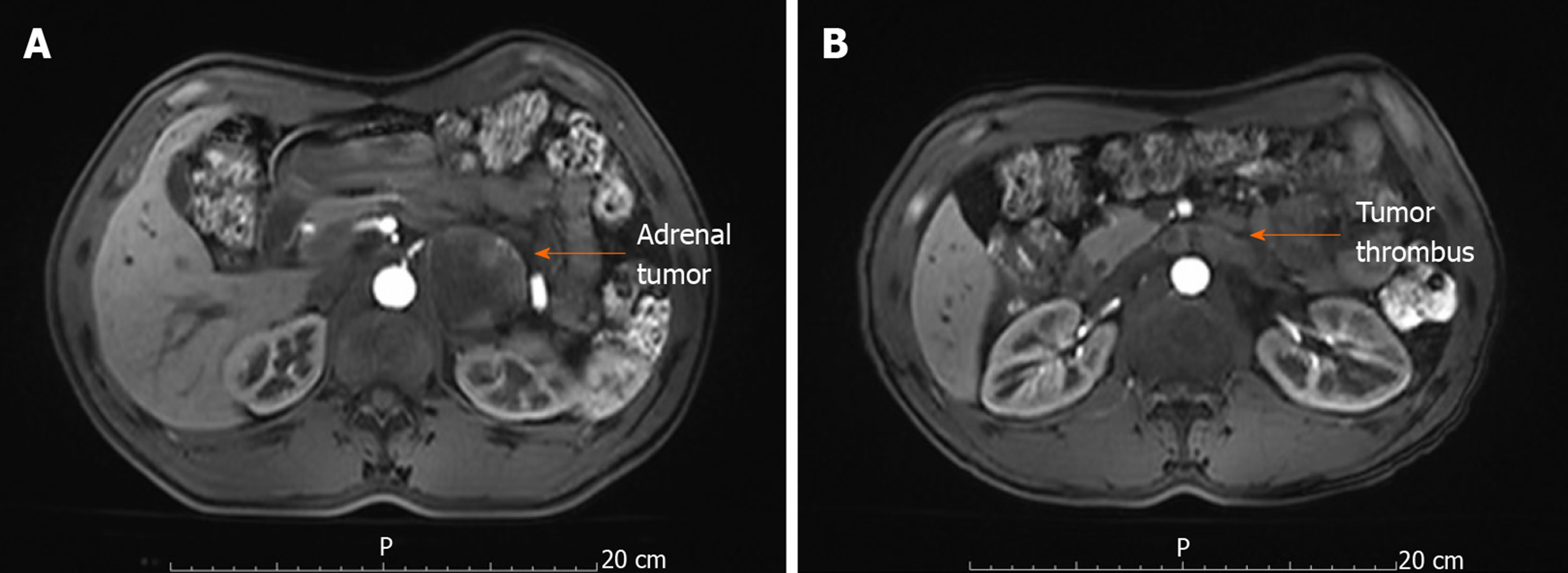
Abdominal magnetic resonance imaging (MRI) revealed a 59 mm × 45 mm adrenal tumor on the left side (Figure 1A). The left renal vein near the IVC entrance was not clearly visible, and whether the tumor had progressed to the left renal vein or IVC was difficult to estimate (Figure 1B). The patient was diagnosed with pheochromocytoma by various endocrine tests and 131-meta-iodobenzylguanidine scintigraphy. No tumor metastasis was found by positron emission tomography-computed tomography (CT).
The patient was given oral adrenergic blockade that consisted of 5 mg phenoxybenzamine three times daily and a beta blocker that consisted of 12.5 mg metoprolol twice daily two weeks before the operation. The patient remained hemodynamically stable.
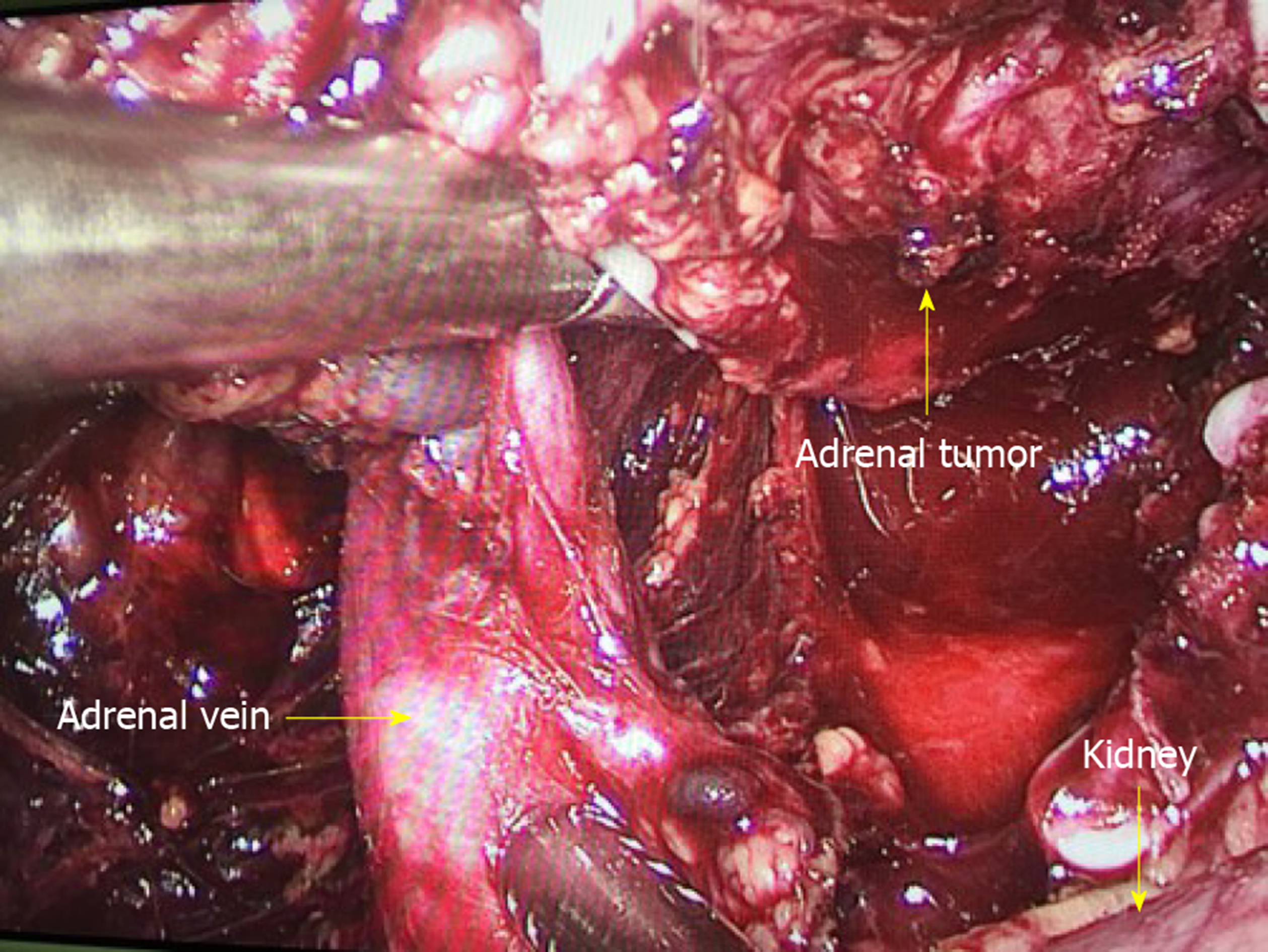
The patient underwent left laparoscopic adrenalectomy via the retroperitoneal approach. During surgery, we found that the adrenal vein was large but contained no solid material (Figure 2). We cut the vein using the Endo-GIA stapler. The patient’s blood pressure reached 248/108 mmHg when the tumor was touched. Hypotensive medicine was administered, and his blood pressure normalized after tumor resection. Pathology confirmed that the tumor was pheochromocytoma, and no tumor thrombus was found in the adrenal vein.
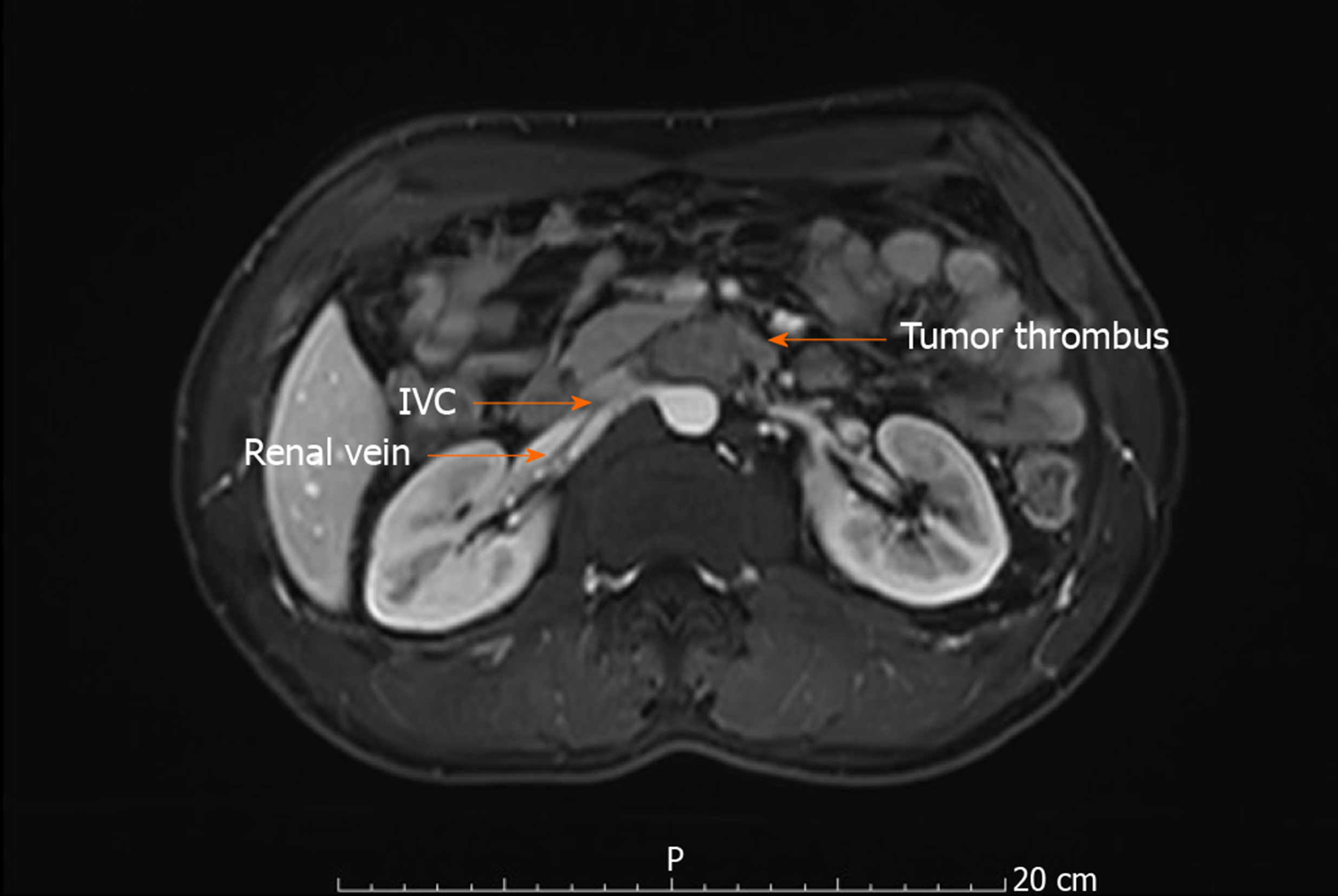
Five months later, the patient was reexamined by abdominal MRI, and the left renal vein clearly exhibited a filling defect near the entrance of the IVC with no marked change compared with the previous MRI (Figure 3). Ultrasound of the IVC showed no abnormality, and renal contrast-enhanced ultrasound revealed a hypoechoic hypervascular mass in the left renal vein. Thus, tumor thrombus in the left renal vein was diagnosed. The patient underwent robot-assisted laparoscopic resection of the tumor thrombus in the left renal vein and left radical nephrectomy.
The patient was diagnosed with left adrenal pheochromocytoma and tumor thrombus in the left renal vein.
The patient underwent robot-assisted laparoscopic nephrectomy and resection of tumor thrombus during second surgery.
The general preoperative preparation included preoperative skin preparation, fasting, water enema, and indwelling gastric tube placement. Special preoperative preparation included renal artery embolization on the related side 2 h before the operation.
The patient underwent preoperative left renal artery embolization. After general anesthesia and Foley catheter placement, the patient was positioned in a modified left lateral decubitus position with a 70° bump.
A 12 mm port was placed at approximately 3 cm from the upper right of the umbilicus for the robot camera. Three 8 mm robotic ports were placed for the three robot arms. The port for the first robot arm was approximately 2 cm under the costal margin at the right midclavicular line. The port for the second robot arm was at the anterior axillary line. The angle composed of the first three ports was 120°. The port for the third robot arm was at the right midclavicular line, which was 8 cm lateral to the second robot port. We used three assistant ports. The first port was placed under the umbilical cord. The second port was placed 6 cm above the umbilical cord. The third port was placed under the xiphoid process for retraction of the liver. The camera and robot arms with the ports were then docked.
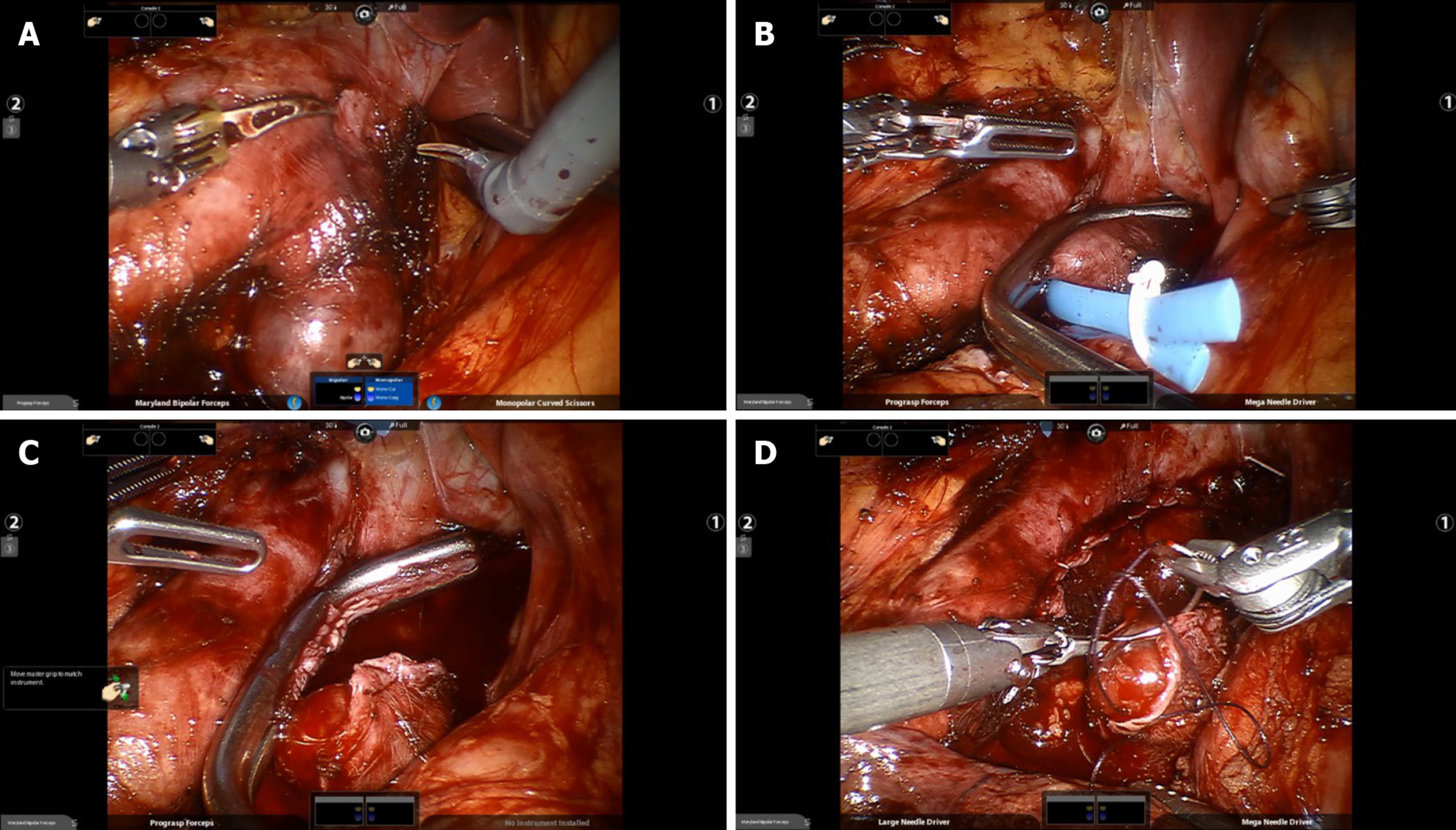
We incised the hepatocolic ligament and medially retracted the ascending colon. The IVC and the left renal vein were then exposed (Figure 4A). The base of the left renal vein was swollen by 2 cm. The root of the left renal vein was clamped 0.5 cm away from the edge of the tumor thrombus using an auricle clamp through the first assistant port (Figure 4B). The renal vein was cut (Figure 4C), and the end of the IVC side was closed using a 4-0 vicryl suture. The auricle clamp was then removed. The end of the left renal vein was also closed to avoid tumor dissemination (Figure 4D).
During surgery, the patient’s blood pressure reached 210/120 mmHg when the tumor thrombus was touched. Hypotensive medicine was administered, and the blood pressure normalized after suturing.
The patient was then converted to the right lateral decubitus position. The first and second assistant ports were preserved, and four new ports for the robot camera and arms were placed similar to that on the right side. The left robot-assisted laparoscopic radical nephrectomy was then performed. Blood loss was less than 100 mL, and the total surgical time was approximately 250 min including docking time.
The patient did not receive blood transfusion or hormone replacement therapy. The patient’s blood creatine increased from 93 μmol/L preoperatively to 125 μmol/L. The patient made an uneventful recovery and was discharged four days after surgery. Pathological tests confirmed that the tumor was a pheochromocytoma thrombus in the left renal vein. The patient was asymptomatic, with no recurrence or metastasis of tumor, and renal function remained normal and stable after a year. The patient was closely followed-up.
Pheochromocytoma with renal vein or IVC thrombus is rare, and only a few cases have been reported in the literature. The clinical manifestations are usually related to the secretion of catecholamine and are often recurrent hypertension, headache, palpitations, and anxiety[1]. However, in this case, the patient had no clinical manifestations, which made the early detection of this tumor difficult.
Contrast-enhanced CT and MRI are useful for recognition of tumor stage and the invasive condition of the circumambient organ and tumor thrombus location level in the renal vein and IVC[2]. The patient also underwent contrast-enhanced ultrasound to evaluate the renal vein and IVC, and vena cava angiography was recommended if the tumor thrombus was located in the IVC. Information on the IVC thrombus location level is important to determine the detailed operative plan, such as skin incision, liver manipulation, or the need for cardiopulmonary bypass or substitution for artificial IVC[3].
The first therapeutic option for pheochromocytoma with IVC thrombus includes adrenalectomy and IVC thrombectomy[2]. Given the anatomic differences of the left and the right adrenal vessels, nephrectomy is recommended when the tumor is on the left. A minimally invasive approach allows the careful and accurate manipulation of the tumor and may help minimize the release of vasoactive substances. Thus, laparoscopic and robot-assisted laparoscopic approaches were performed.
We performed adrenalectomy during the first surgery and nephrectomy and IVC tumor thrombectomy during the second surgery. During the first surgery, we detected that the adrenal vein was large and considered whether the tumor thrombus was located in this vein. However, the postoperative pathological tests showed no tumor thrombus in the adrenal vein.
The tumor thrombus at the root of the renal vein influenced the venous return and caused enlargement of the adrenal vein. The growth pattern of the tumor caused delayed detection of the tumor thrombus.
We used an auricle clamp for renal vein occlusion, which may be selected for tumor thrombus at the root of IVC. Vessel loops were commonly used to clamp the renal vein and IVC. However, the tumor thrombus was near the IVC, and the thrombus was difficult to clamp in this case without squeezing. We tried clamping several times. The auricle clamp was easy to perform using a curve at the front. The step was operated by an assistant and presented a tactile feedback and made it controllable.
Preoperative renal artery embolization was necessary because exposure of the left renal artery was difficult in the left decubitus position[4]. This method can reduce oozing during surgery as this was the second surgery in this patient, and adhesions would be severe.
Before the second surgery, the patient did not receive oral adrenergic blockade or beta blocker. Although the patient was hemodynamically stable pre- and postoperatively, he suffered blood pressure fluctuation during the surgery when handling the tumor thrombus, which was one of shortcomings in our treatment due to the rarity of the disease.
All pheochromocytomas have metastatic potential, and benign and malignant pheochromocytomas have no meaning and have been replaced by risk stratification. However, a widespread risk stratification scheme has never been developed, and predicting the clinical behavior of individual tumors is difficult[5].
In conclusion, pheochromocytoma is a rare tumor, and we report an even rarer case of pheochromocytoma with delayed detection of tumor thrombus at the entrance of the IVC. Nephrectomy is necessary when the tumor is on the left side, and robot-assisted laparoscopic surgery is safe and efficient.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Pandey A S-Editor: Dou Y L-Editor: Webster JR E-Editor: Liu JH
| 1. | Naranjo J, Dodd S, Martin YN. Perioperative Management of Pheochromocytoma. J Cardiothorac Vasc Anesth. 2017;31:1427-1439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 120] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 2. | Shigemura K, Tanaka K, Arakawa S, Hara I, Kawabata G, Fujisawa M. Malignant pheochromocytoma with IVC thrombus. Int Urol Nephrol. 2007;39:103-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Dunn CW, Snyder WH, Ring WS, Latson TW. Pheochromocytoma with extension into the inferior vena cava: a case report. Surgery. 1992;111:472-474. |
| 4. | Wang B, Li H, Ma X, Zhang X, Gu L, Li X, Fan Y, Gao Y, Liu K, Zhu J. Robot-assisted Laparoscopic Inferior Vena Cava Thrombectomy: Different Sides Require Different Techniques. Eur Urol. 2016;69:1112-1119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 84] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 5. | Turchini J, Cheung VKY, Tischler AS, De Krijger RR, Gill AJ. Pathology and genetics of phaeochromocytoma and paraganglioma. Histopathology. 2018;72:97-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 96] [Article Influence: 13.7] [Reference Citation Analysis (0)] |