Published online Jun 26, 2020. doi: 10.12998/wjcc.v8.i12.2667
Peer-review started: February 22, 2020
First decision: May 1, 2020
Revised: May 9, 2020
Accepted: May 27, 2020
Article in press: May 27, 2020
Published online: June 26, 2020
Processing time: 123 Days and 4.6 Hours
Gallbladder torsion is a rare acute abdominal condition that requires emergency surgery. It occurs more commonly in elderly people and in women in the adult population. Diagnosis is a challenge as non-specific symptoms and signs have been reported on ultrasonography, computed tomography and magnetic resonance imaging. Prompt cholecystectomy can decrease the mortality and morbidity of perforation due to gallbladder torsion.
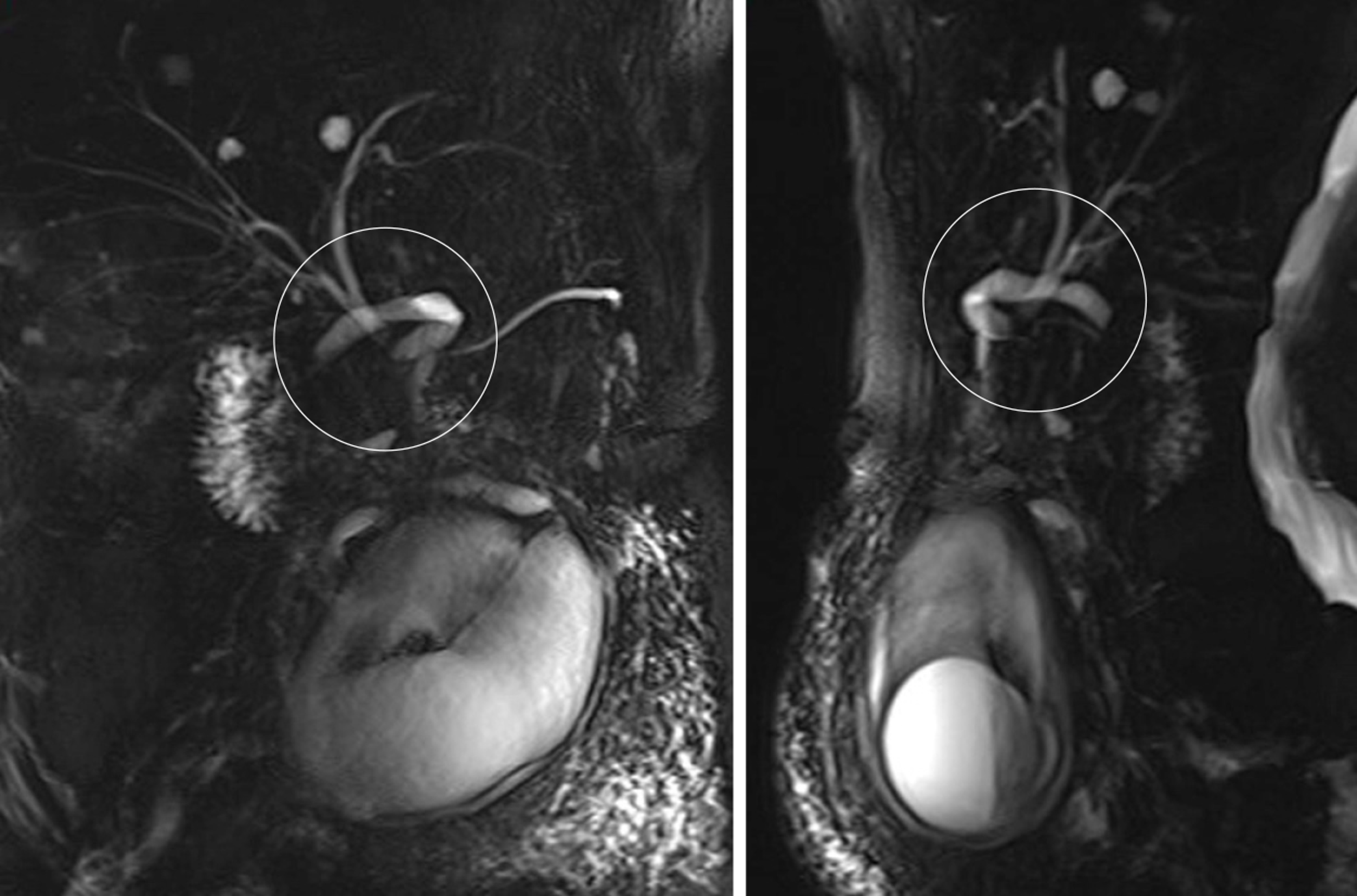
An 82-year-old woman with upper-right quadrant pain and associated nausea and vomiting was diagnosed with ectopic acute calculus cholecystitis. Magnetic resonance cholangiopancreatography (MRCP) showed a V-shaped distortion of the extrahepatic bile ducts and a particularly extended twisted cystic duct, which indicated the presence of gallbladder torsion. Emergency laparoscopic cholecystectomy confirmed the diagnosis and the patient recovered without incident.
Gallbladder torsion can be diagnosed pre-operatively by MRCP. The specific signs are a V-shaped distortion of the extrahepatic bile ducts and a particularly extended twisted cystic duct which can be called twisting signs.
Core tip: Gallbladder torsion is an acute pathological state and it is often difficult to make a definite diagnosis in the early stage. It is mostly identified during emergency surgery. We present a case of gallbladder torsion with typical imaging features, such as V-shaped distortion of the extrahepatic bile ducts, and twisting signs on magnetic resonance cholangiopancreatography, from which we were able to make an early diagnosis. Early confirmation of this emergency will enable prompt surgery with good prognosis.
- Citation: Chai JS, Wang X, Li XZ, Yao P, Yan ZZ, Zhang HJ, Ning JY, Cao YB. Presentation of gallbladder torsion at an abnormal position: A case report. World J Clin Cases 2020; 8(12): 2667-2673
- URL: https://www.wjgnet.com/2307-8960/full/v8/i12/2667.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i12.2667
Gallbladder torsion is a rare acute surgical abdominal condition, with > 500 cases published since it was first reported as floating gallbladder by Wendell in 1898[1-3]. Only 483 articles were obtained when PubMed was searched using the terms “(gallbladder torsion) or gallbladder volvulus”. Gallbladder torsion is defined as the rotation of the gallbladder along the axis of the cystic duct, on its pedicle or any location between the neck and fundus[2,4,5]. The symptoms of incomplete torsion are usually similar to biliary colic, and with complete torsion, there will be a sudden-onset of severe upper abdominal pain and associated vomiting[4]. It is a challenge for radiologists and surgeons to diagnose the condition preoperatively, despite the availability of advanced imaging and laboratory techniques, and most cases are diagnosed during surgery. Prompt surgery decreases the mortality and morbidity of perforation due to gallbladder torsion[6].
Here, we present a case of an abnormally swollen gallbladder twisted in the lower abdomen, which was successfully treated with urgent laparoscopic cholecystectomy, as well as a literature review of gallbladder torsion.
An 82-year-old woman presented to our emergency department with persistent pain in the upper-right quadrant of the abdomen.
The patient reported pain of 6 days duration, with associated nausea and vomiting, without any referred pain. She also complained of chills and her temperature was 38.5°C. There was no jaundice in the skin and sclera.
The patient had a history of hypertension for 10 years, pulmonary embolism 3 years ago and hysterectomy 27 years previously.
There was no personal history of tobacco or alcohol consumption, nor any noteworthy family medical history.
Height and weight of the patient were 155 cm and 42 kg, respectively. Physical examination revealed a longitudinal scar of 10 cm in the lower abdomen, and a fist-sized mass around the umbilicus that was tough, with clear boundaries, poor mobility and obvious tenderness (Figure 1). There were no positive signs in other areas of the abdomen, or a positive Murphy sign.
Laboratory data indicated that her leukocyte count was slightly elevated, C-reactive protein and procalcitonin level were 113.8 mg/L and 0.23 ng/mL, respectively, and liver function tests and pancreatic enzyme concentrations were within normal limits.
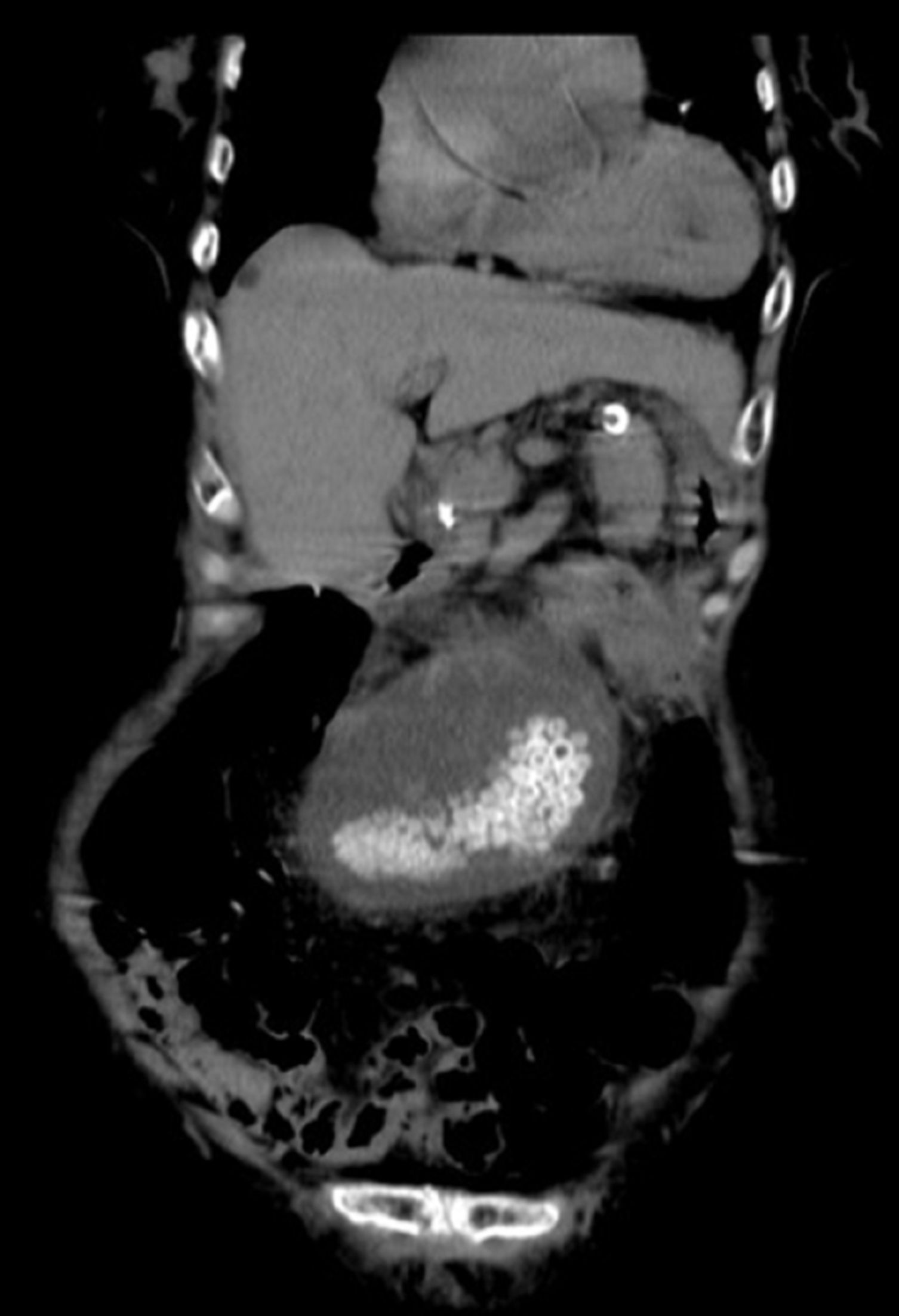
Ultrasonography (US) and computed tomography (CT) showed a cystic mass in the lower abdomen and upper pelvis with multiple nodules of high-density calcifications (Figures 2 and 3), suggesting an abnormally positioned gallbladder with multiple stones and thickening wall, multiple cysts in the liver and kidney, and a small amount fluid in the pelvis. There were no portal vein abnormalities or hepatic deformity. Magnetic resonance imaging (MRI) also demonstrated a cystic mass in the middle of the abdomen with multiple low-intensity T2-weighted signals and edema of the adjacent abdominal wall, suggesting an ectopic enlarged gallbladder with multiple stones and inflammatory changes. Magnetic resonance cholangiopancreatography (MRCP) showed a V-shaped distortion of the extrahepatic bile ducts and a particularly extended twisted cystic duct (Figure 4).
The final diagnosis of this emergency abdominal condition was gallbladder torsion.
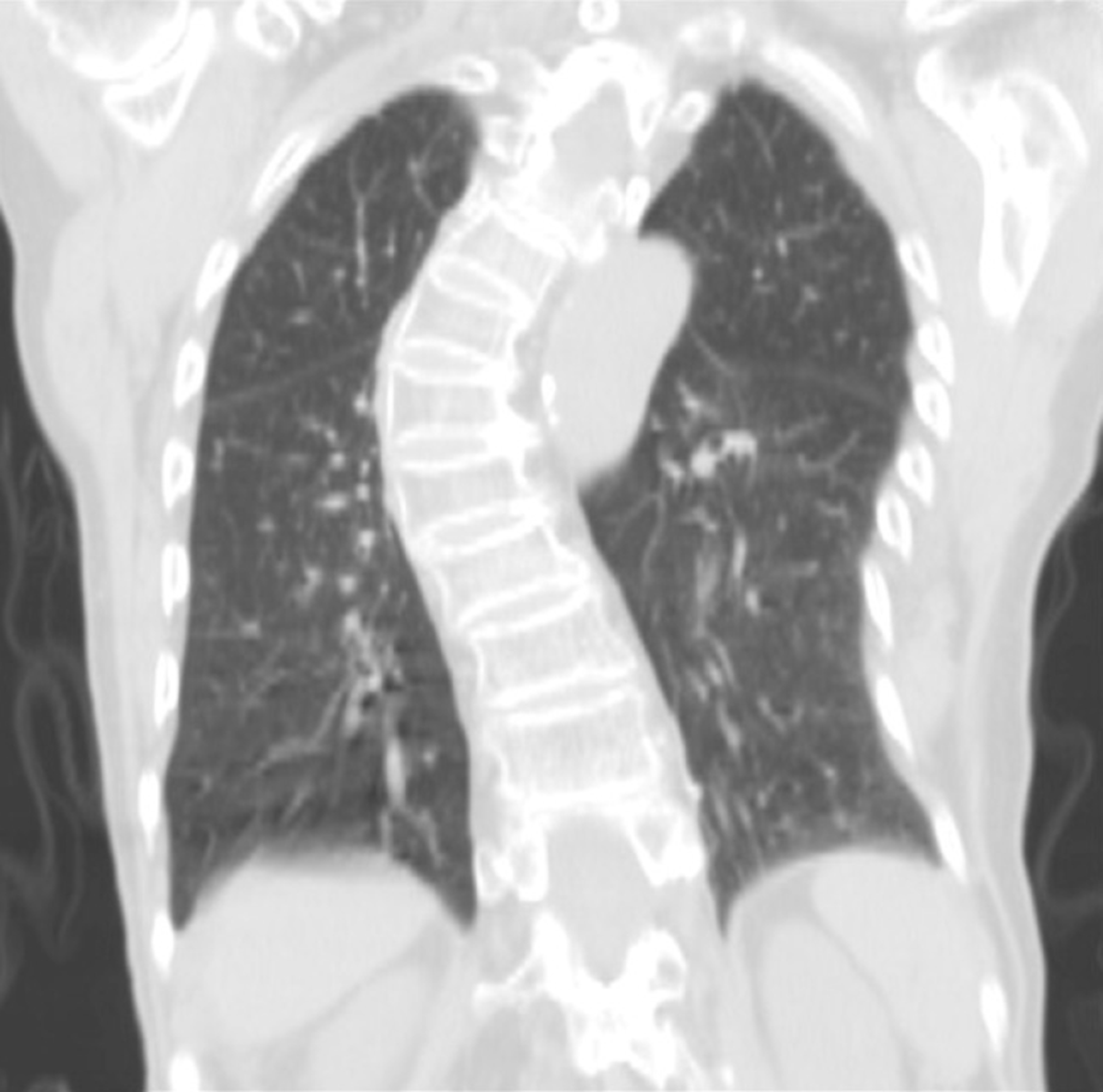
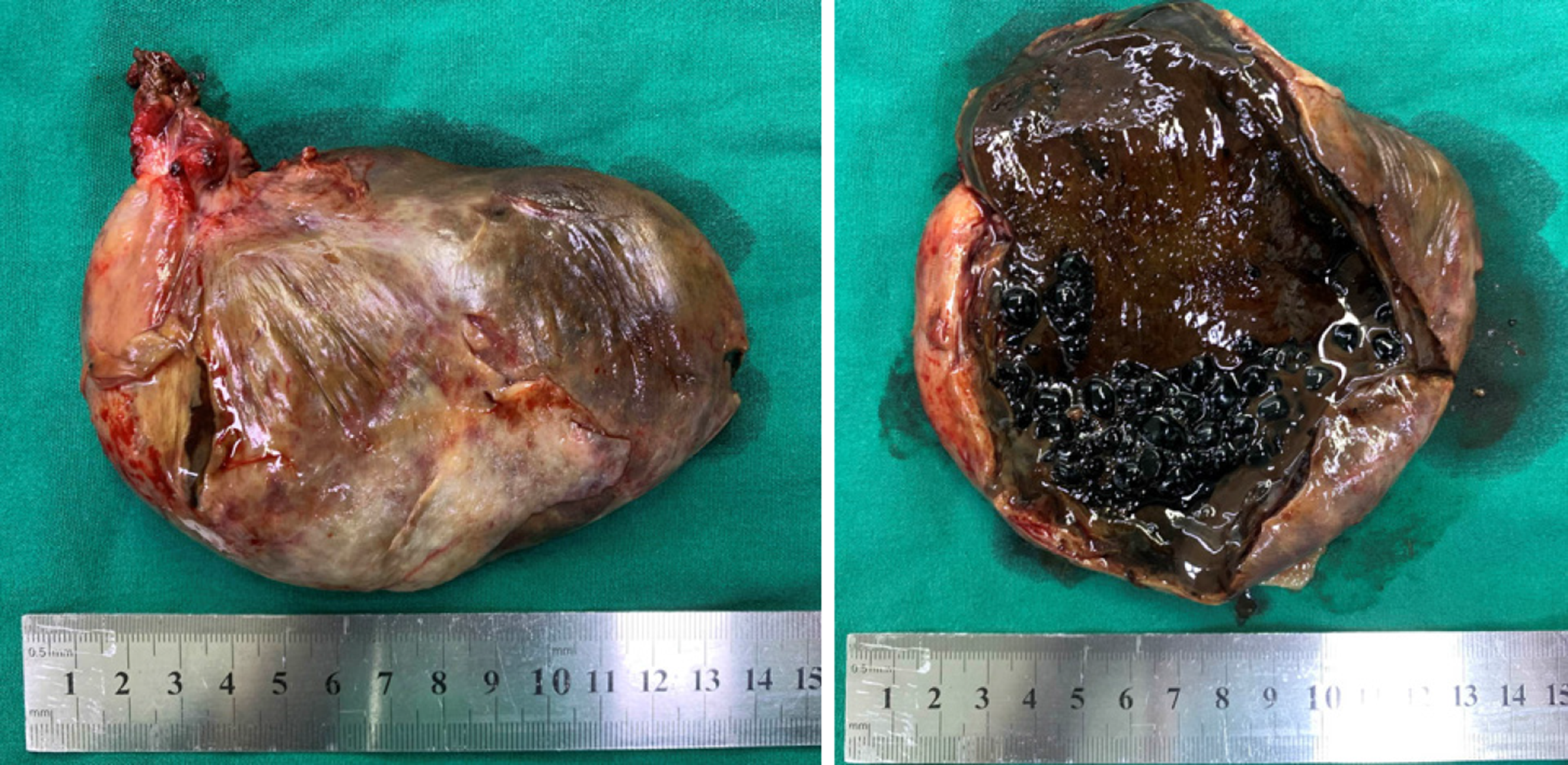
The results indicated an abnormally enlarged ectopic gallbladder with disordered extrahepatic bile ducts, and a diagnosis of gallbladder torsion was considered, which is an indication for emergency surgery. The preoperative evaluation showed spinal deformities (Figure 5), without any contraindications for surgery. Laparoscopic cholecystectomy (LC) was subsequently performed and the surgical investigation indicated that the swollen necrotic gallbladder was twisted approximately 360 degrees in a counterclockwise direction, not adhered to the liver but to the adjacent abdominal wall, with cystic duct and arterial rotation. Torsion of the gallbladder in the middle of the abdomen could not be corrected. Following ligation and severing of the cystic artery and duct, the gallbladder was disconnected from the hepatic hilum. A 3 cm incision was then made to decompress and remove the gallbladder (Figure 6).
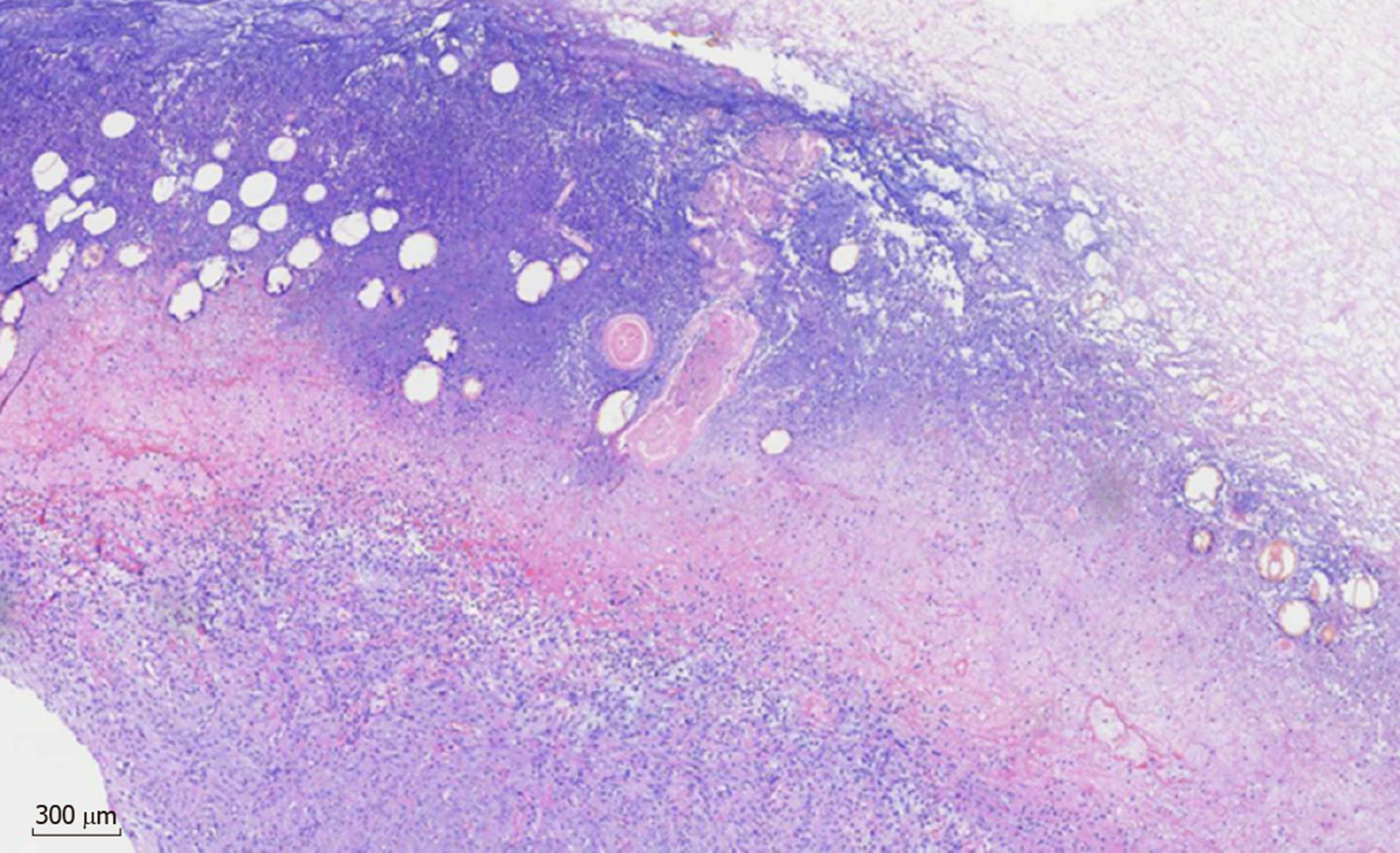
Histopathologic findings of the specimen showed acute gangrenous cholecystitis (Figure 7).
The patient recovered well and was discharged within 5 d, with a good prognosis after 3 mo of follow-up.
Gallbladder torsion is a rare condition and has been reported in all age groups; however, it occurs more commonly in elderly people[7-9], with an incidence of 1 in 365 520 hospital admissions[10]. The incidence increases with age, peaking at 60-80 years[7,11]. The occurrence is higher in women than in men in the adult population, with a ratio of 4:1, which contrasts with a ratio of 1:3 between girls and boys[7,12]. This phenomenon is commonly associated with anatomical variants of the vascular pedicle to the gallbladder and the abnormally elongated mesentery of the gallbladder-to-liver[12]. A decrease in visceral fat is considered to be associated with a higher incidence in the older age group, which explains why it presents in people who are in good health for decades despite a congenitally floating gallbladder[13]. Other contributing factors include peristaltic activity of the stomach, duodenum and surrounding colon, presence of spinal deformity, and even a tortuous atherosclerotic artery of the cyst[4]. The presence of gallstones are considered incidental with a rate of 24.4%-32%, while cholelithiasis has been identified as a major culprit in most gallbladder diseases[3,7,14]. Several risk factors associated with gallbladder torsion are age > 70 years, female sex, weight loss, liver atrophy, scoliosis, atherosclerosis, elongated mesentery, and loss of visceral fat[6].
Gallbladder torsion can be classified into two types. Type I: Incomplete, with gallbladder rotation < 180 degrees, with a long and wide mesentery supporting the gallbladder and cystic duct; and type II: Complete, when gallbladder rotation is > 180 degrees with incomplete mesentery supporting only the cystic duct[4,12,15]. During pathogenesis, the gallbladder can rotate in a clockwise or counterclockwise direction, and no significant relationship was found between the direction and the degree of torsion[7]. Patients usually present to the emergency department with a history of mild to severe right upper quadrant pain and associated nausea or vomiting, and most without associated signs of jaundice or toxemia[4,16]. A palpable mass due to the swollen gallbladder is present in some patients, with obvious tenderness[17]. Patients with incomplete torsion are often misdiagnosed with biliary colic due to non-specific symptoms and signs, whereas complete torsion usually results in compromised blood supply with sudden onset of severe abdominal pain, infarction and gangrene of the gallbladder, which can be fatal[4,12]. The present case, in which the gallbladder rotated 360 degrees was type II and pathological examination verified acute gangrenous cholecystitis.
US and CT findings are generally nonspecific but usually show a floating gallbladder with wall thickening[4]. Enhanced CT and MRI often indicate a reduction in blood flow to the gallbladder, V-shaped distortion of the extrahepatic bile ducts due to cystic duct traction, and even a cystic duct knot sign[18]. Absence of blood flow can also be seen on Doppler US[13]. The specific finding of gallbladder torsion in CT images with a “whirl sign” showing the twisted pedicle of the cystic duct and mesentery is not always present[19]. MRI can indicate hemorrhagic infarction and necrosis of the gallbladder with a high-intensity area within the cystic wall on T1-weighted images[18]. In our case, US and CT images showed an abnormally enlarged gallbladder with multiple stones and thickened wall in the lower abdomen, as well as an elongated mesentery from the hepatic hilum. MRCP showed a V-shaped distortion of the extrahepatic bile ducts and a particularly extended cystic duct, which was twisted and could be called “twisting signs” (Figure 4). To date, there are few reported cases that show the twisting signs clearly. Spinal deformities in our case may have contributed to the pathological appearance. Accumulated typical features of gallbladder torsion have been reported, appearing on US, CT and MRI[18]. However, the preoperative diagnosis of this condition was achieved in only 26% of patients because of its rarity[7]. It is usually diagnosed as acute cholecystitis requiring emergency surgical intervention, although it is difficult to assess the condition exactly[18]. Mortality and morbidity of the cystic perforation are decreased with prompt laparotomy after identification of the indication for surgery[16]. Surgery can be performed via open or laparoscopic approaches. A study showed that gallbladder torsion accounted for 1.5% of patients who underwent urgent LC for acute gallbladder disease, and suggested that emergency LC is feasible for this rare acute abdominal condition[20]. The critical steps are decompression and derotation of the gallbladder to obtain a clear view of the extrahepatic bile ducts. Sometimes it is difficult to perform detailed inspection of the anatomical structures with laparoscopy due to the abnormal position of the biliary tract. Timely conversion to open surgery during LC can avoid iatrogenic bile duct injury.
Gallbladder torsion is an acute surgical condition that is often misdiagnosed, which might result in significant mortality and morbidity due to cystic perforation without prompt laparotomy. Older patients with nonresolving symptoms of acute cholecystitis should be investigated for possible gallbladder torsion. A displaced floating gallbladder seen on US and CT, as well as elongated mesentery, may suggest gallbladder torsion. Specific signs such as V-shaped distortion of the extrahepatic bile ducts, whirl sign or twisting signs on CT or MRCP can indicate the diagnosis. The outcome for this pathological condition is excellent after emergency cholecystectomy.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Lee MJ, Naganuma H S-Editor: Wang J L-Editor: Webster JR E-Editor: Liu JH
| 1. | Wendel AV. VI. A Case of Floating Gall-Bladder and Kidney complicated by Cholelithiasis, with Perforation of the Gall-Bladder. Ann Surg. 1898;27:199-202. [PubMed] |
| 2. | Pu TW, Fu CY, Lu HE, Cheng WT. Complete body-neck torsion of the gallbladder: a case report. World J Gastroenterol. 2014;20:14068-14072. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Kachi A, Nicolas G, Nasser J, Hashem M, Abou Sleiman C. A Rare Presentation of Gall Bladder Volvulus: A Case Report. Am J Case Rep. 2019;20:1466-1470. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Aharoni D, Hadas-Halpern I, Fisher D, Hiller N. Torsion of the fundus of gallbladder demonstrated on ultrasound and treated with ERCP. Abdom Imaging. 2000;25:269-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Pottorf BJ, Alfaro L, Hollis HW. A Clinician's Guide to the Diagnosis and Management of Gallbladder Volvulus. Perm J. 2013;17:80-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Reilly DJ, Kalogeropoulos G, Thiruchelvam D. Torsion of the gallbladder: a systematic review. HPB (Oxford). 2012;14:669-672. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 72] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 8. | García-Hernández C, Archivaldo-García C, Carvajal-Figueroa L, Granados-Macías M, Herrera-Flores I. Acute gallbladder volvulus: laparoscopic treatment in an infant. Cir Cir. 2019;87:58-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Escalard C, Calinghen A, Habchi N. Gallbladder volvulus: A rare cause of acute gallbladder distension. J Gastroenterol Hepatol. 2019;34:1133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Janakan G, Ayantunde AA, Hoque H. Acute gallbladder torsion: an unexpected intraoperative finding. World J Emerg Surg. 2008;3:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Boer J, Boerma D, de Vries Reilingh TS. A gallbladder torsion presenting as acute cholecystitis in an elderly woman: A case report. J Med Case Rep. 2011;5:588. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Abou Sleiman C, Terro JJ, Semaan DB, Nicolas G, El Shami J, El Helou E, Saliba C, Zeidan M, El Chamaa B, Lakkis RS, Charbel C, Zaghrini E. Gallbladder Volvulus: An Unusual Presentation. Am J Case Rep. 2019;20:1879-1882. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Ohkura Y, Hashimoto M, Sasaki K, Watanabe G. Complete acute gallbladder torsion diagnosed with abdominal ultrasonography and colour Doppler imaging. BMJ Case Rep. 2013;2013:2013:bcr2012008460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Younan G, Schumm M, Ali F, Christians KK. Gallbladder Volvulus in a Patient with Type I Choledochal Cyst: A Case Report and Review of the Literature. Case Rep Surg. 2016;2016:5626531. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Matsubara K, Urushihara T, Oshita A, Itamoto T. Single-incision laparoscopic cholecystectomy for gallbladder torsion: A case report and literature review. Asian J Endosc Surg. 2018;11:165-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Wood BE, Trautman J, Smith N, Putnis S. Rare case report of acalculous cholecystitis: Gallbladder torsion resulting in rupture. SAGE Open Med Case Rep. 2019;7:2050313X18823385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Aljoe J. Gallbladder volvulus-acute cholecystitis 'with a twist'. J Surg Case Rep. 2018;2018:rjy303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Moriwaki Y, Otani J, Okuda J, Niwano T. Gallbladder Torsion: US, CT, and MRI Findings. J Gastrointest Surg. 2019;23:1077-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Tajima Y, Tsuneoka N, Kuroki T, Kanematsu T. Clinical images. Gallbladder torsion showing a "whirl sign" on a multidetector computed tomography scan. Am J Surg. 2009;197:e9-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |