Published online Jun 26, 2020. doi: 10.12998/wjcc.v8.i12.2629
Peer-review started: March 16, 2020
First decision: April 29, 2020
Revised: May 12, 2020
Accepted: June 3, 2020
Article in press: June 3, 2020
Published online: June 26, 2020
Processing time: 99 Days and 18.5 Hours
Sick sinus syndrome is a common disease in cardiology. Typical symptoms include palpitations, dizziness, shortness of breath, chest tightness, and amaurosis. However, to date, there are no known reports of sick sinus syndrome presenting with headache. Whether there is a correlation between headache and sick sinus syndrome merits further research. In this report, we describe a case of headache induced by sick sinus syndrome.
A 73-year-old female patient presented to our department with the chief complaint of recurrent paroxysmal headache for more than 7 years. The patient described paroxysmal palpations, usually headache occurring after palpitation. Her blood pressure was normal when the most recent headache occurred. A magnetic resonance imaging study and magnetic resonance angiography of the head at another center were normal. A clinical neurological examination was negative. A 24-h Holter electrocardiogram monitoring study showed sick sinus syndrome. The patient received dual chamber pacing implantation and was administered drug therapy to control ventricular rate. The patient’s paroxysmal headaches and palpitations had resolved within 1 year, confirmed via a follow-up telephone call.
After dual-chamber pacing implantation and drug therapy administration to control the ventricular rate, the patient’s paroxysmal headaches and palpitations had resolved within 1 year, confirmed via a follow-up telephone call. We believe that the headaches were related to the patient’s sick sinus syndrome.
Core tip: We report a patient who had headaches induced by sick sinus syndrome. To the best of our knowledge, this finding has not been previously reported. It provides new ideas for clinical diagnosis and treatment of both headache and sick sinus syndrome in the future.
- Citation: Bi YC, Gong L. Headache and sick sinus syndrome: A case report. World J Clin Cases 2020; 8(12): 2629-2633
- URL: https://www.wjgnet.com/2307-8960/full/v8/i12/2629.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i12.2629
Headache is a common neurological symptom with a multitude of different causes such as intracranial hemorrhage, infection, and migraine. Sick sinus syndrome is an arrhythmia phenotype attributed to sinus node dysfunction. The clinical symptoms of sick sinus syndrome include palpitations, dizziness, chest tightness, weakness, shortness of breath, amaurosis, and Adams-Stokes syndrome, among others. In this report, we describe a case of headache induced by sick sinus syndrome.
On July 30, 2018, a 73-year-old female patient presented to our department with the chief complaint of recurrent paroxysmal headache for more than 7 years.
The headaches lasted from minutes to hours, and presented with moderate swelling and recurrent paroxysmal pain through the whole brain. The patient had paroxysmal palpations as well, usually followed by the headache episodes. However, headaches did not always occur every time after palpations. The patient’s blood pressure was normal when the headaches occurred.
The patient has documented hypertension and type 2 diabetes, although blood pressure and glucose were well managed.
The patient’s family history was unremarkable.
The patient′s heart auscultation was absolutely arrhythmic, heart sound intensities differed, and her pulse was deficient. Her blood pressure was 132/75 mmHg. The clinical neurological examination was negative.
The patient′s thyroid function was normal. The liver and kidney function examination was also negative.
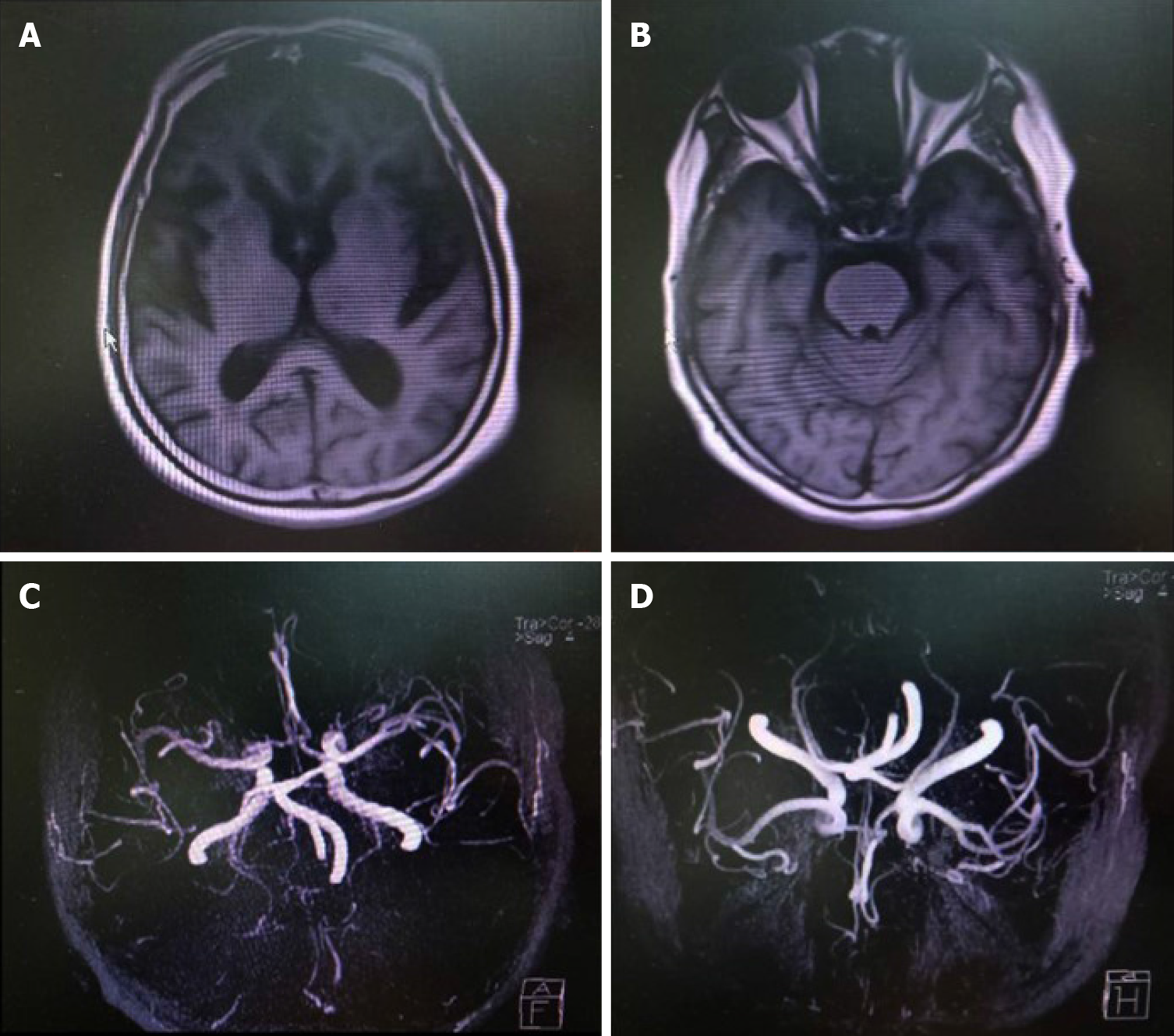
A magnetic resonance imaging study and magnetic resonance angiography of the head performed at another center were normal (Figure 1).
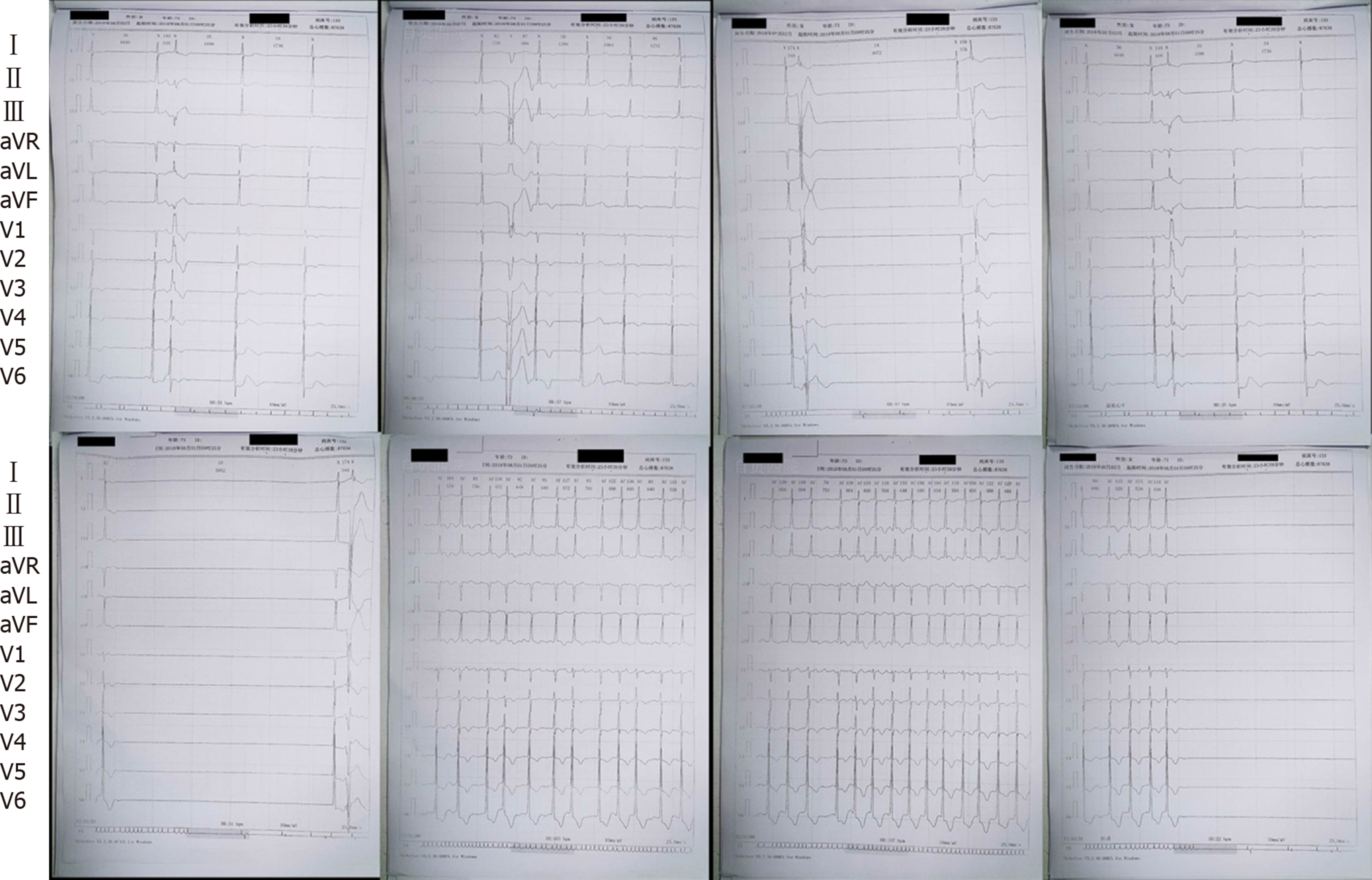
The 24-h Holter electrocardiogram (ECG) monitoring study showed sinus bradycardia, sinus pause, AV junctional escape beats, ventricular escape, paroxysmal atrial flutter, and paroxysmal atrial fibrillation. The longest RR interval was 5.952 s (Figure 2).
We arrived at a final diagnosis of sick sinus syndrome.
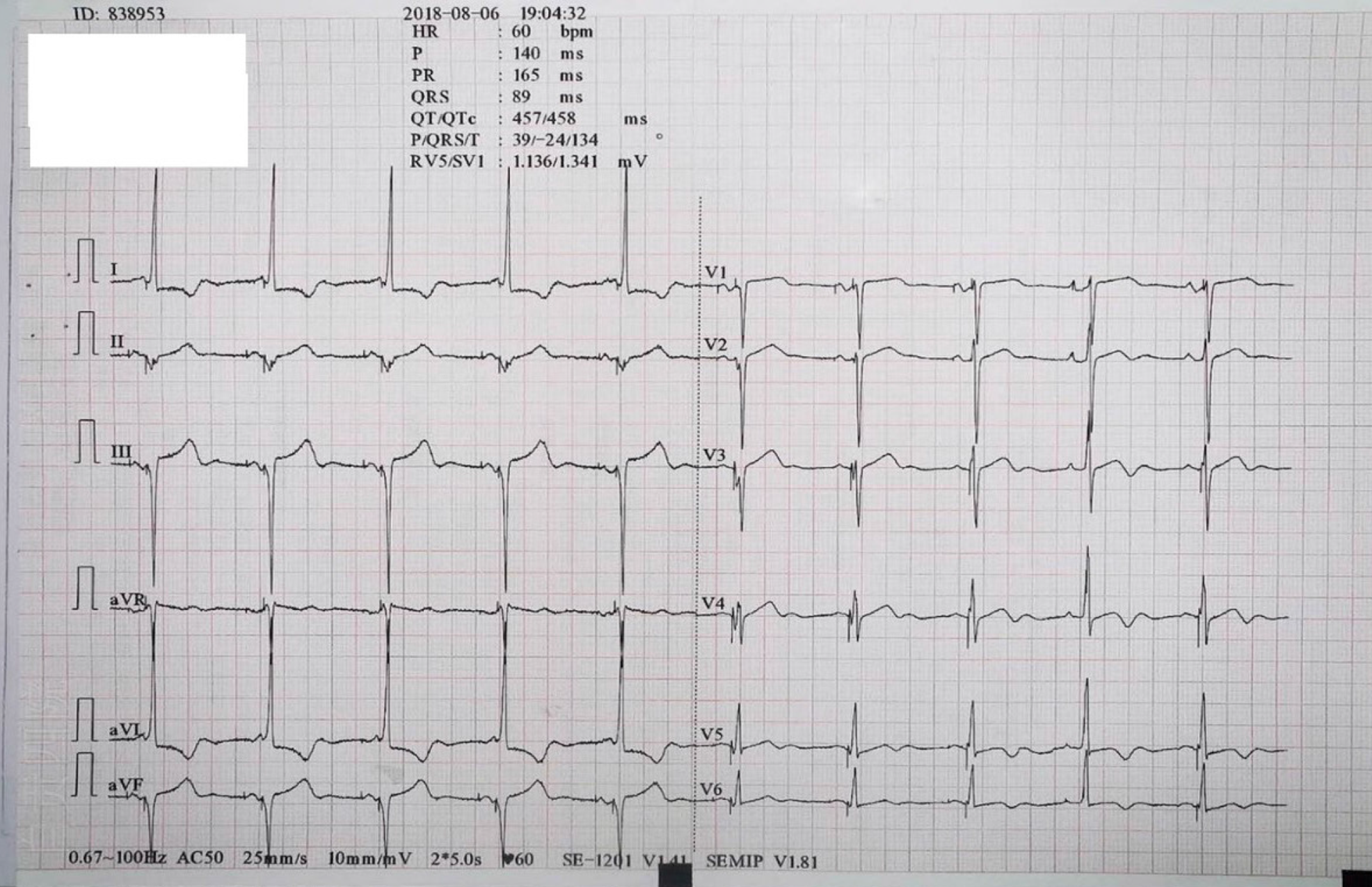
The patient received dual-chamber pacing implantation on August 6, 2018. The patient was prescribed Metoprolol Succinate Sustained-Release Tablets 47.5 mg twice a day and Amiodarone Hydrochloride Tablets once a day to control ventricular rate.
The patient’s paroxysmal headaches and palpitations had resolved within 1 year, confirmed by a follow-up telephone call. The ECG was normal after implantation of dual-chamber pacing (Figure 3).
In this case, the organic lesion had not been considered when auxiliary examinations and a clinical neurological examination were both negative. Migraine was not considered on account of the patient’s age. When the patient described headaches following palpitations, we hypothesized that the headaches may have been related to an arrhythmia. After dual-chamber pacing implantation and pharmaceutical anti-arrhythmic therapy, the patient was followed up via a telephone call at 1 year. At that time, the patient reported resolution of her symptoms. Therefore, we believe that her headaches were related to sick sinus syndrome.
Common mechanisms of headache include: (1) Constriction, dilatation and extension of intracranial blood vessels caused by various pathologies; (2) Cranial and cervical nerve stimulation; (3) Elevated resting tension of the head and neck muscles; (4) Ophthalmologic and otorhinolaryngologic disorders, and cervical spine disease; (5) Biochemical factors and endocrine disorders; and (6) Neurological disorders.
The incidence of headache as a symptom of sick sinus syndrome was not definite. No similar report was found in the literature.
Asvestas et al[1] reported a case of headache as a primary symptom of acute myocardial infarction. Huang et al[2] reported a similar case of a patient, who had been diagnosed with myocardial infarction and complained of headache without chest discomfort. Furthermore there have been multiple case reports of headache as the sole or cardinal symptom of myocardial infarction[3-6]. Thus, the concept of headache being induced by cardiac factors has been presented.
Cardiac cephalgia is defined in The International Classification of Headache Disorders: 2nd edition[7] and The International Classification of Headache Disorders: 3rd edition[8,9].
There are four theories regarding the proposed pathogenesis of cardiac cephalgia. First, the heart is mediated by the autonomic nerve, visceral, and somatic fibers, which can converge on the same neurons in the spinal cord. Then the information induced by visceral afferents is relayed to the higher somatic region. Second, the reduction of cardiac output elevates left ventricular and right atrial pressure, which decreases cerebral venous refluxing and elevates intracranial pressure[10,11]. Third, neurochemical mediators produced by myocardial ischemia can induce vasodilatation of the cerebral vessels and pain[10,11]. Fourth, it is assumed that vasospasms can concomitantly occur in both coronary and cerebral vessels[10,12].
In this case, we hypothesized that arrhythmia led to myocardial ischemic and reduction of cardiac output. As a result of the arrhythmias, headache could be induced by stimulating visceral nerves and neurochemical mediators because of myocardial ischemia, and could also be induced by elevated intracranial pressure because of the reduction of cardiac output. Unfortunately, we did not monitor the variation of this patient’s cardiac output; thus, the possibility of other causes remains to be considered.
This case provides two novel insights. First, clinicians should pay close attention to predisposing symptoms and conditions. Second, it appears that arrhythmias can cause headaches.
We thank the cardiologist for the expiation for the ECG.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rigatelli G S-Editor: Dou Y L-Editor: Filipodia E-Editor: Liu JH
| 1. | Asvestas D, Vlachos K, Salachas A, Letsas KP, Sideris A. Headache: An unusual presentation of acute myocardial infraction. World J Cardiol. 2014;6:514-516. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 2. | Huang CC, Liao PC. Heart Attack Causes Head-Ache - Cardiac Cephalalgia. Acta Cardiol Sin. 2016;32:239-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 3. | Dell'Aquila A, Sciatti E, Vizzardi E, Metra M. The brain-heart connection: a multiple sclerosis relapse presenting as Takotsubo Syndrome. A case report and literature review. Monaldi Arch Chest Dis. 2020;90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Chowdhury AW, Saleh MAD, Hasan P, Amin MG, Khan TA, Sabah KMN, Kabir SR. Cardiac cephalgia: A headache of the heart. J Cardiol Cases. 2015;11:139-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Wassef N, Ali AT, Katsanevaki AZ, Nishtar S. Cardiac Cephalgia. Cardiol Res. 2014;5:195-197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | MacIsaac R, Jarvis S, Busche K. A Case of a Cardiac Cephalgia. Can J Neurol Sci. 2019;46:124-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24 Suppl 1:9-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 798] [Cited by in RCA: 2427] [Article Influence: 115.6] [Reference Citation Analysis (0)] |
| 8. | Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38:1-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6960] [Cited by in RCA: 5919] [Article Influence: 845.6] [Reference Citation Analysis (0)] |
| 9. | He L, Cheng GS, Du YJ, Zhang YS. Clinical relevance of atrial septal aneurysm and patent foramen ovale with migraine. World J Clin Cases. 2018;6:916-921. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Bini A, Evangelista A, Castellini P, Lambru G, Ferrante T, Manzoni GC, Torelli P. Cardiac cephalgia. J Headache Pain. 2009;10:3-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Lipton RB, Lowenkopf T, Bajwa ZH, Leckie RS, Ribeiro S, Newman LC, Greenberg MA. Cardiac cephalgia: a treatable form of exertional headache. Neurology. 1997;49:813-816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 72] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Ramadan NM. Headache caused by raised intracranial pressure and intracranial hypotension. Curr Opin Neurol. 1996;9:214-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |