Published online Jan 6, 2020. doi: 10.12998/wjcc.v8.i1.194
Peer-review started: October 26, 2019
First decision: November 21, 2018
Revised: November 30, 2019
Accepted: December 13, 2019
Article in press: December 13, 2019
Published online: January 6, 2020
Processing time: 72 Days and 12.1 Hours
Neuroblastoma is an extracranial malignant tumor in children that is most often located in the adrenal gland and sympathetic ganglion. Here, we present a rare case of neuroblastoma originating from the urinary bladder.
A 3-year-old girl presented with lower abdominal pain with micturition. Ultrasound revealed a lower abdominal mass. Abdominal computed tomography scan displayed a solitary mass at the top of the urinary bladder. Blood levels of neuron-specific enolase and lactate dehydrogenase were elevated. We treated the child with partial cystectomy and six courses of chemotherapy, and the outcome at 4-year follow-up was unremarkable.
Neuroblastoma should be considered when tumors are located in the urinary bladder, especially in the dome; although this presentation is rare, the prognosis is very good.
Core tip: Rhabdomyosarcoma is a common bladder malignancy in children. We here report a rare case of bladder neuroblastoma in a child. The patient was treated with a standard strategy and had a good outcome. Our findings suggest that children with neuroblastoma have good prognosis.
- Citation: Cai JB, Wang JH, He M, Wang FL, Xiong JN, Mao JQ, Li MJ, Zhu K, Liang JW. Unusual presentation of bladder neuroblastoma in a child: A case report. World J Clin Cases 2020; 8(1): 194-199
- URL: https://www.wjgnet.com/2307-8960/full/v8/i1/194.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i1.194
Neuroblastoma is the most common extracranial malignancy in pediatric patients which originates from the neural crest. It is most often located at the adrenal gland, followed by the mediastinum, retroperitoneum, neck and pelvis. Pelvic neuroblastoma is rare, and the ordinary site is presacral. Malignant tumors are rare in children, and the most common type is rhabdomyosarcoma. However, neuroblastoma located in the urinary bladder is extremely unusual, with only seven cases previously reported in the world. Intriguingly, unlike the prognosis for neuroblastoma in other sites, all patients with neuroblastoma in the urinary bladder are alive as of the date of this report; this seems to be a favorable prognostic subtype. Here, we report a new case of neuroblastoma located at the dome of the urinary bladder and present a systematic review of the literature.
A 3-year-old girl was transferred to our hospital with lower abdominal pain with micturition for one week.
The patient’s symptoms started one week before recurrent episodes of lower abdominal pain with micturition, without hematuria or fever.
The patient had no prior medical history.
The patient’s medical history and family history were unremarkable.
Physical examination was unremarkable except for a palpable mass in the lower abdomen.
Routine laboratory tests revealed elevated blood neuron-specific enolase (NSE) and lactate dehydrogenase (60 ng/mL and 264 u/L, respectively). However, the values of vanillylmandelic acid and homovanillic acid in the urine were not detected.
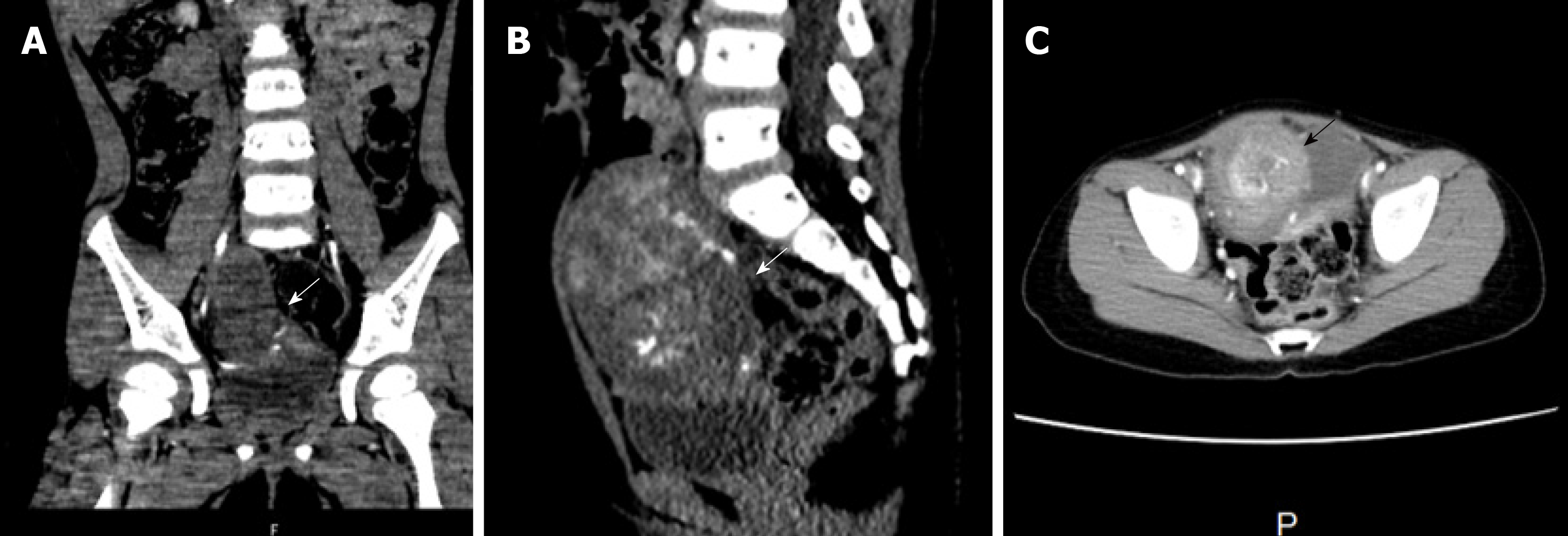
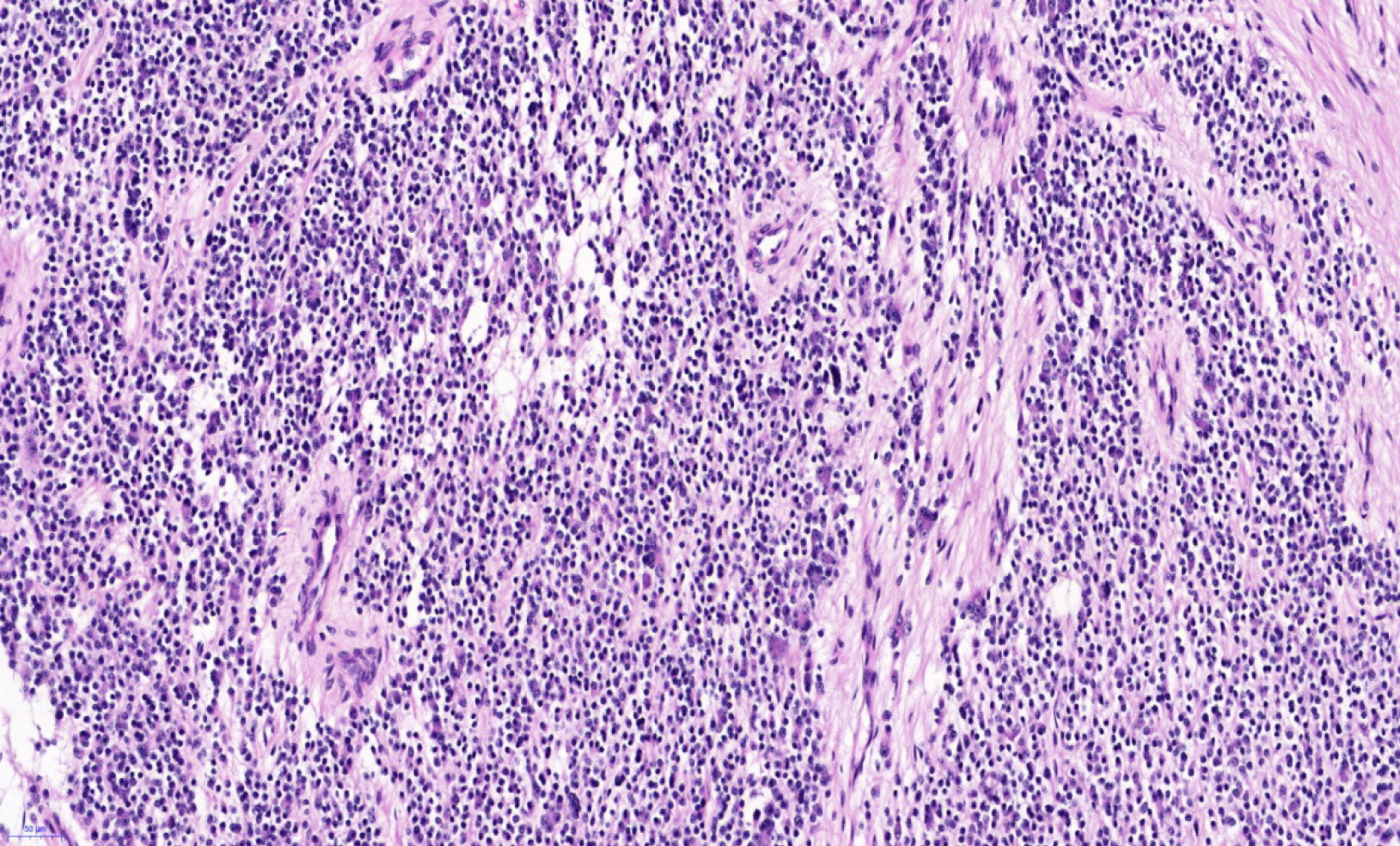
A chest computed tomography (CT) showed unremarkable findings. An abdominal CT scan displayed a solitary mass with a volume of 72 mm × 53 mm × 65 mm at the top of the urinary bladder. The tumor protruded into the bladder cavity, with the margin enhanced in the dynamic phase on contrast-enhanced CT (Figure 1). No other abnormalities were found in other sites. The pathological results of the tumor after resection were nodular ganglioneuroblastoma (Figure 2). With a favorable Shimada histopathologic classification (well-differentiated nodular ganglioneuroblastoma and low mitosis-karyorrhexis index, the tumor cells were intensely immunostained for NSE. N-myc gene amplification was absent in the tumor, implying a favorable prognosis.
Neuroblastoma in the urinary bladder.
After admission, the patient underwent surgery. At laparotomy, a mass was found at the dome of the bladder, and a partial cystectomy was performed. According to the Chinese Children’s Cancer Cooperative Group Study of Neuroblastoma (2015)[1], the patient was classified into a low-risk group, and treated with a modified postoperative chemotherapy regimen consisting of vindesine (3 mg/m2 weekly), carboplatin (150 mg/m2 on days1-2) and doxorubicin (20 mg/m2 on days 1-2) (every three weeks) for three courses, and vindesine (3 mg/m2 weekly), ifosfamide (1200 mg/m2 on days 2-4), and etoposide (100 mg/m2 on days 2-4) (every three weeks) for another three courses.
After operation, the patient’s serum NSE level decreased to a normal range. The patient completed chemotherapy without any complications. The patient was asymptomatic with no tumor recurrence during 4 years of follow-up.
Neuroblastoma is the most common extracranial malignant tumor in children. Originating from the neural crest, neuroblastoma is most often located in the adrenal gland, followed by the mediastinum, retroperitoneum, neck and pelvis. Pelvic neuroblastoma is rare, and they commonly occur in the presacral space while urinary bladder neuroblastoma is extremely uncommon. Most malignant urinary tumors are rhabdomyosarcoma, and urinary bladder malignant tumors are rare; only seven cases have been previously reported in the world[2-8]. Therefore, neuroblastoma is not the common differential diagnosis in pelvic tumors.
Neuroblastoma embryologically arises from the neural crest cells and the sympathetic nervous system. It generally presents in the adrenal gland (40%), abdomen and thorax (both 15%). According to the location and extent of the disease, organ-specific and nonspecific constitutional symptoms are present. Occasionally, patients are asymptomatic with localized disease.
According to the literature, only seven cases of neuroblastoma in the urinary bladder have been reported to date globally. The characteristics of eight patients diagnosed with neuroblastoma in the urinary bladder are presented in Table 1[2]. In these eight patients, including our patient, four presented with gross hematuria[3,4,6,7]. In the remaining patients, two were asymptomatic, and were detected in a mass screening program[2,5], and two patients presented as a palpable mass discovered on physical examination[8].
| Ref. | Gen-der | Age | Symp-tom | Loca-tion | Volume (mm) | INSS | INPC | Shimada type | Prognosis factor | Opera-tion | Che-mo | Progno-sis |
| Sáez et al[4] | M | 3 | H | Ant Wall | 1 | P | UH | Mycn(+), 1P(+) | CE | (+)AR | A | |
| Yokoyama et al[5] | F | 7 | MS | Dome | 35 × 30 × 25 | 1 | P | FH | Mycn(-) | CE | (-) | A |
| Ijiri et al[2] | F | 8 | MS | Dome | 45 × 32 × 23 | 1 | P | FH | Mycn(-), 1P(-) | CE | (-) | A |
| Knoedler et al[8] | 4 | LAM | Dome | 50 × 30 | 1 | GNB | CE | (-) | A | |||
| Entz-Werle et al[7] | F | 15 | H | Dome | 45 × 50 × 29 | 2 | FH | Mycn(-) | CE | (+)BO | A | |
| Kojima et al[3] | M | 4 | H | Dome | 15 × 15 × 15 | 4s | P | FH | Mycn(-) | CE | (+) | A |
| Zhu et al[6] | M | 36 | H | Dome | 2 | D | FH | Mycn(-) | CE | (-) | A | |
| Our case | F | 36 | LAM | Dome | 72 × 53 × 65 | 1 | FH | Mycn(-) | CE | (+) | A |
In these eight patients, the tumors were located at the dome of bladder in seven patients[2,3,5-8], and the tumor in all the patients was at the anterior wall of the bladder[4].
The Shimada type of six patients was favorable, and the N-myc gene was not amplified in seven patients. A 3-mo-old female had an unfavorable Shimada type and N-myc (+)[4]. Six patients were younger than 15 mo, and the other two patients were 36 mo. In these eight patients, five were in stage 1, two were in stage 2, and one was in stage 4s. Four patients were treated immediately with partial cystectomy without chemotherapy or radiotherapy. One was treated with chemotherapy after recurrence, two were treated with chemotherapy after surgery, and one was treated before surgery because of vessel compression and local infiltration.
Additionally, two patients had a urachal neuroblastoma located at the dome of the urinary bladder. The tumor was resected at stage 1, and the patients were free of symptoms after surgery without any chemotherapy or radiation therapy[9,10]. These results also indicate a good prognosis for neuroblastoma originating in the urinary bladder.
According to the International Neuroblastoma Staging System, pediatric neuroblastoma was classified as stage 1-4 and 4s; however, Shimada pathology type, patient age, tumor gene amplification, and neuroblastoma were classified into low (low/very low), intermediate, and high risk groups[11,12]. Patients are treated with surgery, chemotherapy, radiation, hematopoietic stem cell transplantation, or immune therapy according to the defined risk group. For the low-risk group patients, surgery is recommended with or without chemotherapy. The intermediate-risk group patients are treated with surgery and chemotherapy. High-risk group patients are treated with surgery combined with chemotherapy, radiation therapy, hematopoietic stem cell transplantation and immune therapy[12]. Our patient was a 3-year-old child in the low-risk group and she was treated with six courses of chemotherapy. To date, it remains controversial whether the low-risk group patients need chemotherapy, and some experts recommend chemotherapy while others do not. All eight cases of urinary bladder neuroblastoma were grouped into the low-risk group; four of these patients received complete tumor resection only, two patients with unfavorable Shimada pathology type were administered chemotherapy, one patient with N-myc (+) received chemotherapy after tumor recurrence, and one patient received chemotherapy before and after surgery because of vessel compression and local infiltration.
Ghazali demonstrated a group of patients with pelvic neuroblastoma with spontaneous regression and maturation[13]. Observation has become a new option for asymptomatic neuroblastoma patients, especially in those who are diagnosed at an early age and stage 1, 2, and 4s. Therefore, many tumors already regressed spontaneously without any intervention before detection, which may be a reason why so few cases of urinary bladder neuroblastoma have been reported and why there is such a high survival rate in the reported patients. These findings may indicate that urinary bladder neuroblastoma is a favorable subtype.
Neuroblastoma in the urinary bladder is a rare pediatric malignant tumor, and it is associated with a good prognosis, especially when the tumor is located at the dome of the urinary bladder. However, as few cases of this subtype have been reported, further investigations are necessary.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Nagasawa M S-Editor: Dou Y L-Editor: MedE-Ma JY E-Editor: Xing YX
| 1. | Children with Tumor Professional Committee of Chinese Anti-cancer Association. The Chinese Medical Association of Pediatric Surgery Branch of the Surgical Oncology Group. Children neuroblastoma diagnosis expert consensus. Zhonghua Xiaer Waike Zazhi. 2015;36:3-7. [DOI] [Full Text] |
| 2. | Ijiri R, Tanaka Y, Kou K, Nishihira H, Nishi T. Bladder origin neuroblastoma detected by mass screening. Urology. 1998;52:1139-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Kojima S, Yagi M, Asagiri K, Fukahori S, Tanaka Y, Ishii S, Saikusa N, Koga Y, Yoshida M, Masui D, Komatsuzaki N, Nakagawa S, Ozono S, Tanikawa K. Infantile neuroblastoma of the urinary bladder detected by hematuria. Pediatr Surg Int. 2013;29:753-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Sáez C, Márquez C, Quiroga E, Borderas F, Alfaro J, Pineda G, Loizaga JM, Alvarez AM. Neuroblastoma of the urinary bladder in an infant clinically detected by hematuria. Med Pediatr Oncol. 2000;35:488-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Yokoyama S, Hirakawa H, Ueno S, Yabe H, Hiraoka N. Neuroblastoma of the urinary bladder, preclinically detected by mass screening. Pediatrics. 1999;103:e67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Zhu J, Hoag NA, Gustafson P, Afshar K, Macneily AE. Pediatric bladder neuroblastoma: Case report and literature review. Can Urol Assoc J. 2013;7:E609-E611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Entz-Werle N, Marcellin L, Becmeur F, Eyer D, Babin-Boilletot A, Lutz P. The urinary bladder: An extremely rare location of pediatric neuroblastoma. J Pediatr Surg. 2003;38:E10-E12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Knoedler CJ, Kay R, Knoedler JP Sr, Wiig TH. Pelvic neuroblastoma. J Urol. 1989;141:905-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Clapuyt P, Saint-Martin C, De Batselier P, Brichard B, Wese FX, Gosseye S. Urachal neuroblastoma: first case report. Pediatr Radiol. 1999;29:320-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Brichard B, Vermylen C, Cornu G, Clapuyt P, Myant N, Gosseye S, Wese F. Urachal tumor: an unusual presentation of neuroblastoma. Pediatr Hematol Oncol. 2000;17:435-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Brodeur GM, Pritchard J, Berthold F, Carlsen NL, Castel V, Castelberry RP, De Bernardi B, Evans AE, Favrot M, Hedborg F. Revisions of the international criteria for neuroblastoma diagnosis, staging, and response to treatment. J Clin Oncol. 1993;11:1466-1477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1656] [Cited by in RCA: 1587] [Article Influence: 49.6] [Reference Citation Analysis (0)] |
| 12. | Cohn SL, Pearson AD, London WB, Monclair T, Ambros PF, Brodeur GM, Faldum A, Hero B, Iehara T, Machin D, Mosseri V, Simon T, Garaventa A, Castel V, Matthay KK; INRG Task Force. The International Neuroblastoma Risk Group (INRG) classification system: an INRG Task Force report. J Clin Oncol. 2009;27:289-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1159] [Cited by in RCA: 1315] [Article Influence: 77.4] [Reference Citation Analysis (0)] |
| 13. | Ghazali S. Pelvic neuroblastoma: a better prognosis. Ann Surg. 1974;179:115-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.3] [Reference Citation Analysis (0)] |