Published online Apr 26, 2019. doi: 10.12998/wjcc.v7.i8.984
Peer-review started: October 22, 2018
First decision: November 27, 2018
Revised: January 28, 2019
Accepted: February 18, 2019
Article in press: February 18, 2019
Published online: April 26, 2019
Processing time: 189 Days and 0.6 Hours
Over the past years, only few cases of follicular lymphoma diagnosed by laparoscopy have been reported in the world. Since follicular lymphoma related ascites often causes occult disease and lacks specific clinical manifestations, it is often difficult to identify the cause by routine laboratory tests and imaging methods. Diagnostic experience is not sufficient and more cases need to be accumulated for further analysis.
Ascites due to unknown reasons often causes problems for clinical diagnosis and treatment. In this paper, we report one case with ascites in whom the reason causing ascites was not identified through routine examination. Laparoscopic examination of the celiac lesions and histological examination of the lesions were performed and the final diagnosis was peritoneal follicular lymphoma.
Laparoscopic abdominal examination is of great significance for the definite diagnosis of ascites due to an unknown reason.
Core tip: Over the past years, only few cases of follicular lymphoma diagnosed by laparoscopy have been reported in the world. Since follicular lymphoma related ascites often causes occult disease and lacks specific clinical manifestations, it is often difficult to identify the cause by routine laboratory tests and imaging methods. Diagnostic experience is not sufficient and more cases need to be accumulated for further analysis.
- Citation: Wei C, Xiong F, Yu ZC, Li DF, Luo MH, Liu TT, Li YX, Zhang DG, Xu ZL, Jin HT, Tang Q, Wang LS, Wang JY, Yao J. Diagnosis of follicular lymphoma by laparoscopy: A case report. World J Clin Cases 2019; 7(8): 984-991
- URL: https://www.wjgnet.com/2307-8960/full/v7/i8/984.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i8.984
Ascites is a clinical manifestation of many diseases and can be due to a variety of causes. Any pathological condition that results in an intraperitoneal fluid volume of more than 200 mL is called ascites. Since ascites often causes occult disease and lacks specific clinical manifestations, it is often difficult to identify the cause by routine laboratory tests and imaging methods. There are many causes of ascites, and the most common causes are cardiovascular diseases, liver diseases, peritoneal diseases, kidney diseases, connective tissue diseases, and malignant tumors. Identifying the cause of ascites plays a crucial role in the treatment and prognosis of patients. Laparoscopic examination of the abdominal cavity can observe intraperitoneal lesions and allows the pathological biopsy. Using this method, the diagnostic positive rate is high, the trauma is small, and the risk is low. It is very important to diagnose ascites cases due to unknown reasons[1]. Our department used laparoscopic abdominal examination and diagnosed a case of ascites caused by follicular lymphoma. The relevant case data are summarized as follows.
The patient (male, 60 years old) was admitted to our department in May 2017.
Abdominal bloating for one month.
The patient presented abdominal distension without obvious inducement 1 month ago, and was aware that the abdominal distension was more obvious in a few days, which affected breathing and daily life. During the course of the disease, the patient had no diarrhea, abdominal pain, nausea, vomiting, fearlessness, cold, fever, or other discomfort. The patient had been hospitalized in other hospital before. Routine examination of blood in other hospital showed that white blood cell count was 11.5 × 109/L, lymphocyte ratio was 11.3%, and eosinophil count was 39.4%. Immune-related tests showed IgG 38.94 g/L, IgE 7250 g/L, and IgM 0.4 6 g/L. Urine is negative for Bence Jones protein. A full abdominal-pelvic computed tomography (CT) plain scan and three-dimensional reconstruction examination showed: (1) Wide nodular thickening of the peritoneum and multiple soft tissue masses in the abdominal cavity (considering malignant tumors with peritoneal metastasis and multiple lymph node metastasis); (2) The right liver lobe low perfusion area which suggested a possibility of metastases; (3) Mucosal thickening of the gastric antrum (it is recommended to perform gastroscopy); (4) A large amount of peritoneal effusion; and (5) Small renal cysts. Gastroscopy showed chronic non-atrophic gastritis with erosion. During hospitalization in other hospital, symptomatic treatments including absorbing ascites and diuretic treatment were provided. In order to facilitate further treatment, this patient was admitted to our hospital as “ascites to be diagnosed”. Since the onset of the disease, the patient had a systemic rash accompanied by pruritus, which was diagnosed as “eczema” in the other hospital and the effect of drug treatment was poor. In recent 1 mo, the patient had normal defecation and urine, and was mentally stable, with poor appetite, poor sleep, and a weight loss of 10 kg.
The patient had a medical history of “hypertension” for 3 yr, without regular drug treatment, and denied a chronic medical history of diabetes, coronary heart disease, and other diseases, an infectious medical history of hepatitis and tuberculosis, a medical history of surgery, blood transfusion, and trauma, and a history of drug allergy. The patient’s history of preventive inoculation was unknown.
The patient had a drinking history of 20 yr, about 250 mL liquor daily, and had been sober for 3 yr. The rest of the personal and family history sections were unexceptional.
Admission examination showed stable vital signs, visible multiple skin rashes, and itchy skin lesions after pruritus in mucous membranes without obvious abnormalities in heart and lung examinations. Abdominal distention with frog-like ventral appearance was observed. No obvious abnormalities in the liver, kidney and spleen were observed. Shifting dullness was positive. There was no obvious edema in both lower limbs.
After admission, the relevant examinations were performed. Routine blood tests showed that the white blood cell count was 7.89 × 109/L, eosinophils accounted for 22.4%, and absolute eosinophil count was 1.77 × 109/L. High-sensitivity CRP was 12.7 mg/L, and procalcitonin was 0.17 ng/L. Biochemical tests showed that serum potassium was 3.2 mmol/L, serum sodium was 132.0 mmol/L, total protein was 99.5 g/L, albumin was 37.3 g/L, globulin was 62 g/L, immunoglobulin G was 46.04 g/L, IgG1 was 19.5 g/L, IgG4 was 5.93 g/L, and IgG 2 and IgG 3 were normal. Erythrocyte sedimentation rate was 47 mm/h, CA125 was 983.90 U/mL, coagulation function, renal function, hepatitis B, hepatitis C, syphilis, HIV test, tuberculosis immune examination, ANA series, anti-ENA antibody spectrum, vasculitis series, and other tests showed no obvious abnormalities. Ascites examination showed that it was yellow in color, slightly turbid, and qualitatively positive for mucin; the number of cells in ascites was 9829/μL, and the number of nucleated cells was 5829/μL (polymorphonuclear cells accounted for 8.1%, and mononuclear cells accounted for 91.9%). The total protein was 62.2 g/L, albumin was 22.1 g/L, globulin was 40.1 g/L, and adenosine deaminase was 15.9 U/L. CDC examination showed that Schistosoma IgG antibody was positive. Ascites bacteria, fungi, anaerobes, and mycobacteria culture and smears were negative. Ascites cytology showed that the smear had mesothelial cells, phagocytes, a large number of lymphocytes, and a small number of eosinophils.
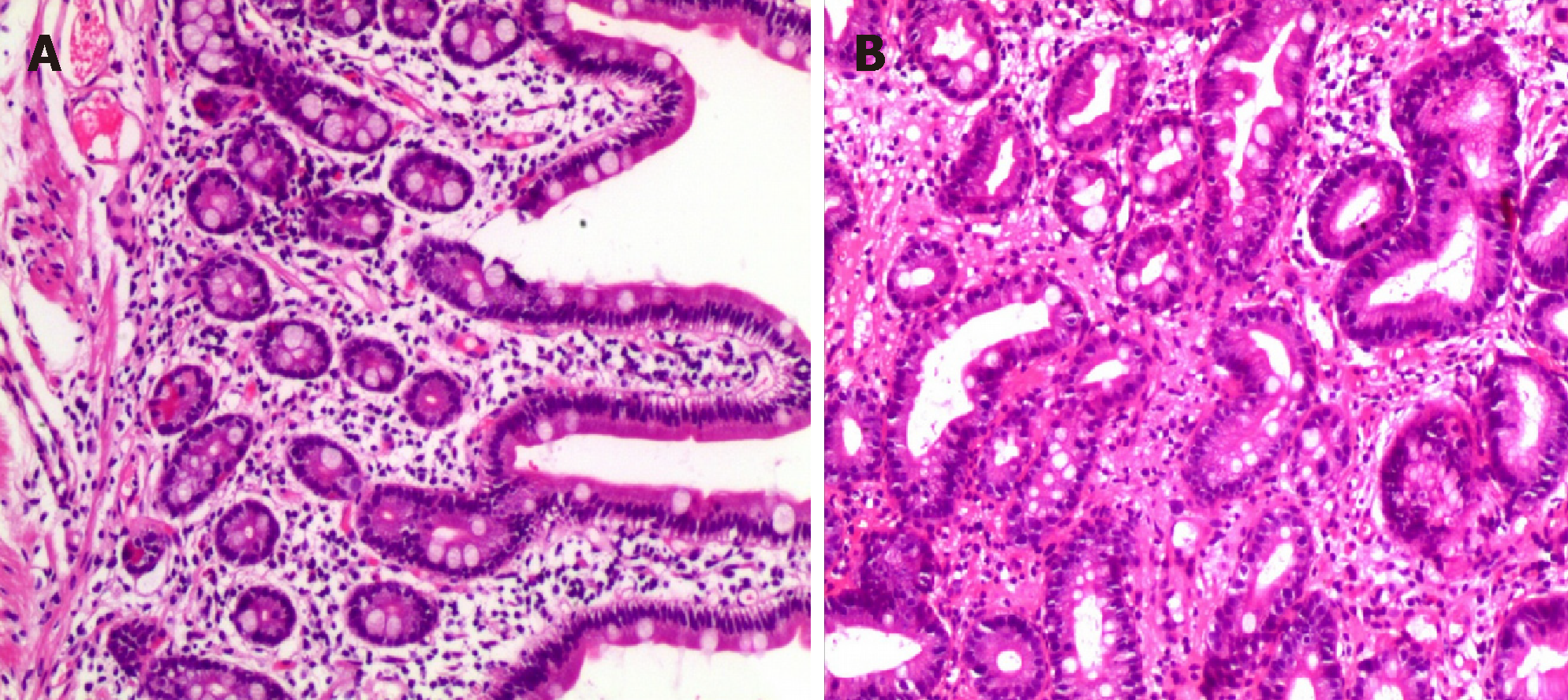
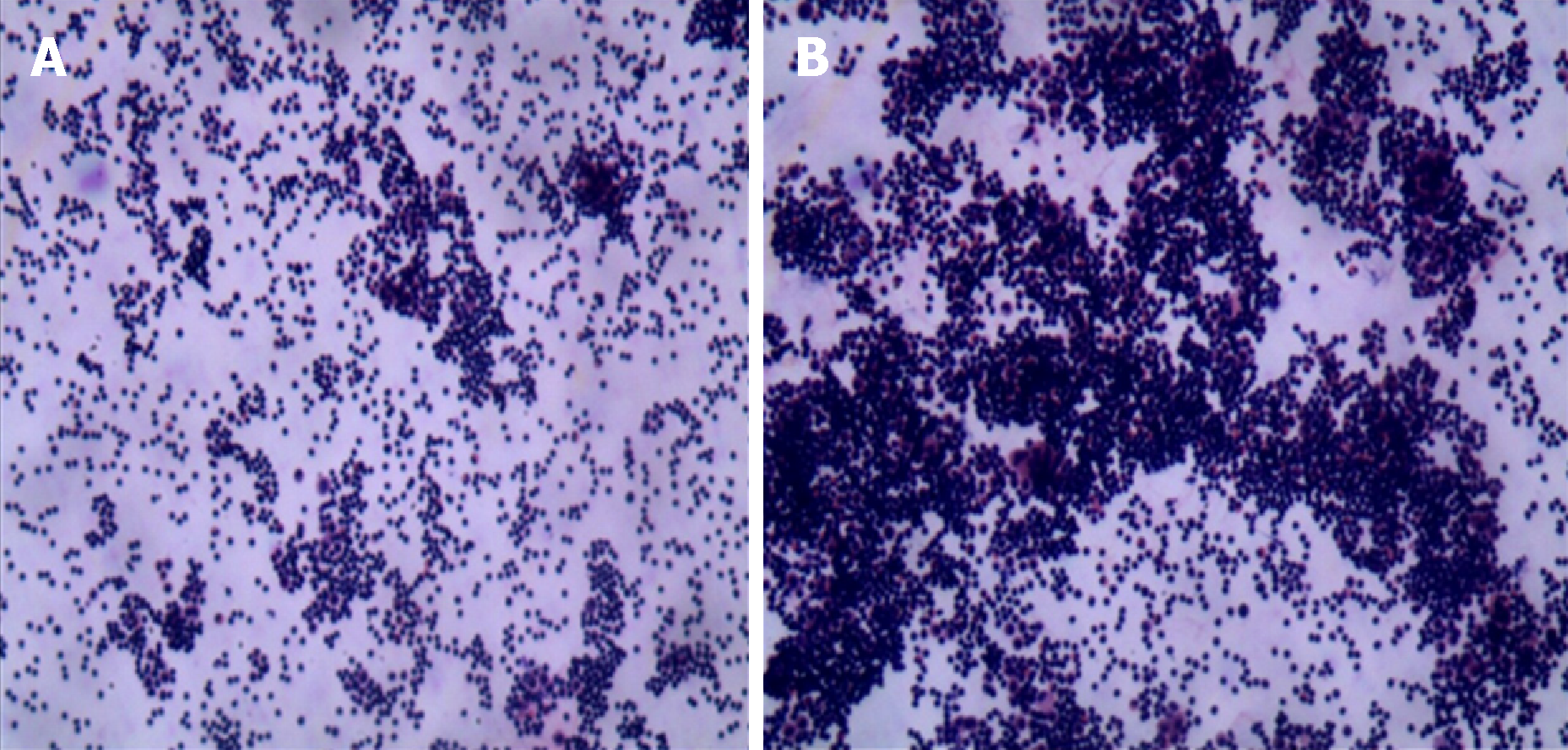
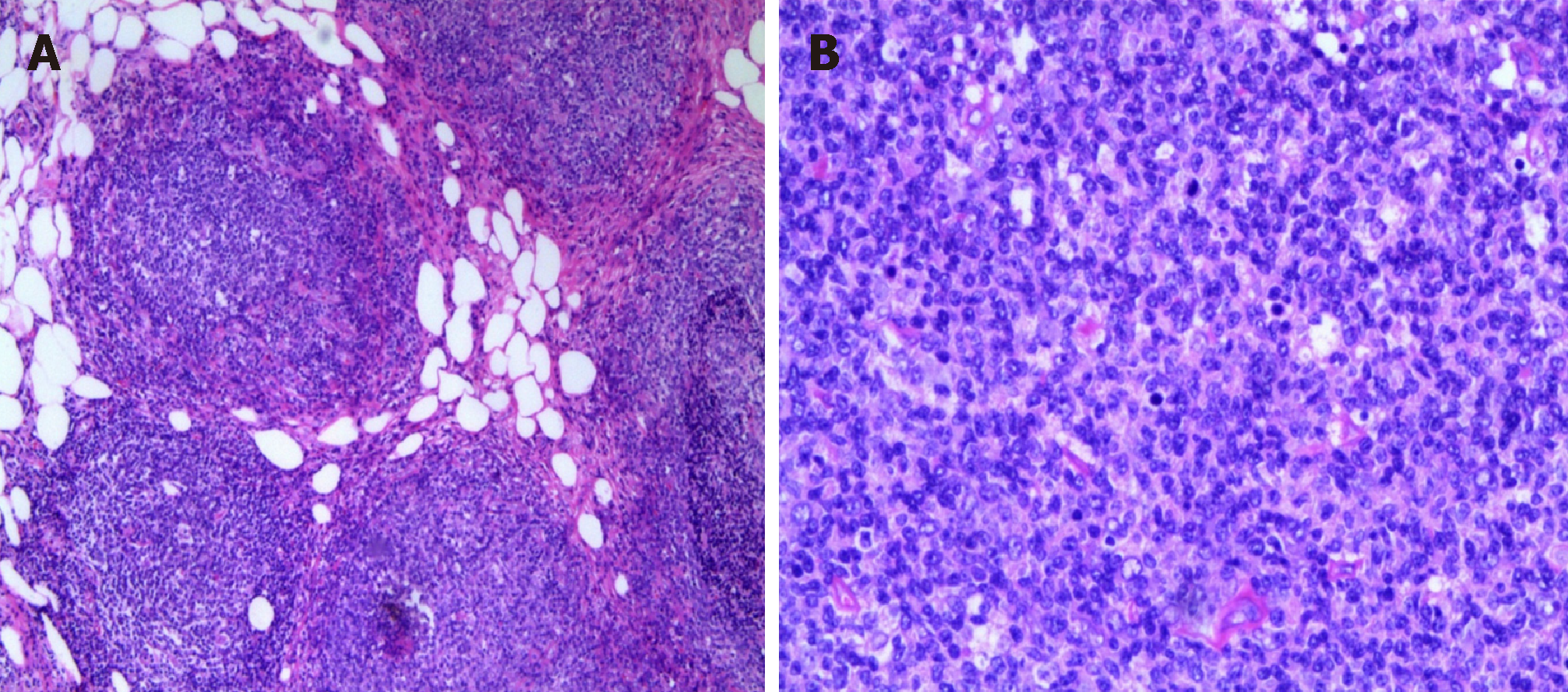
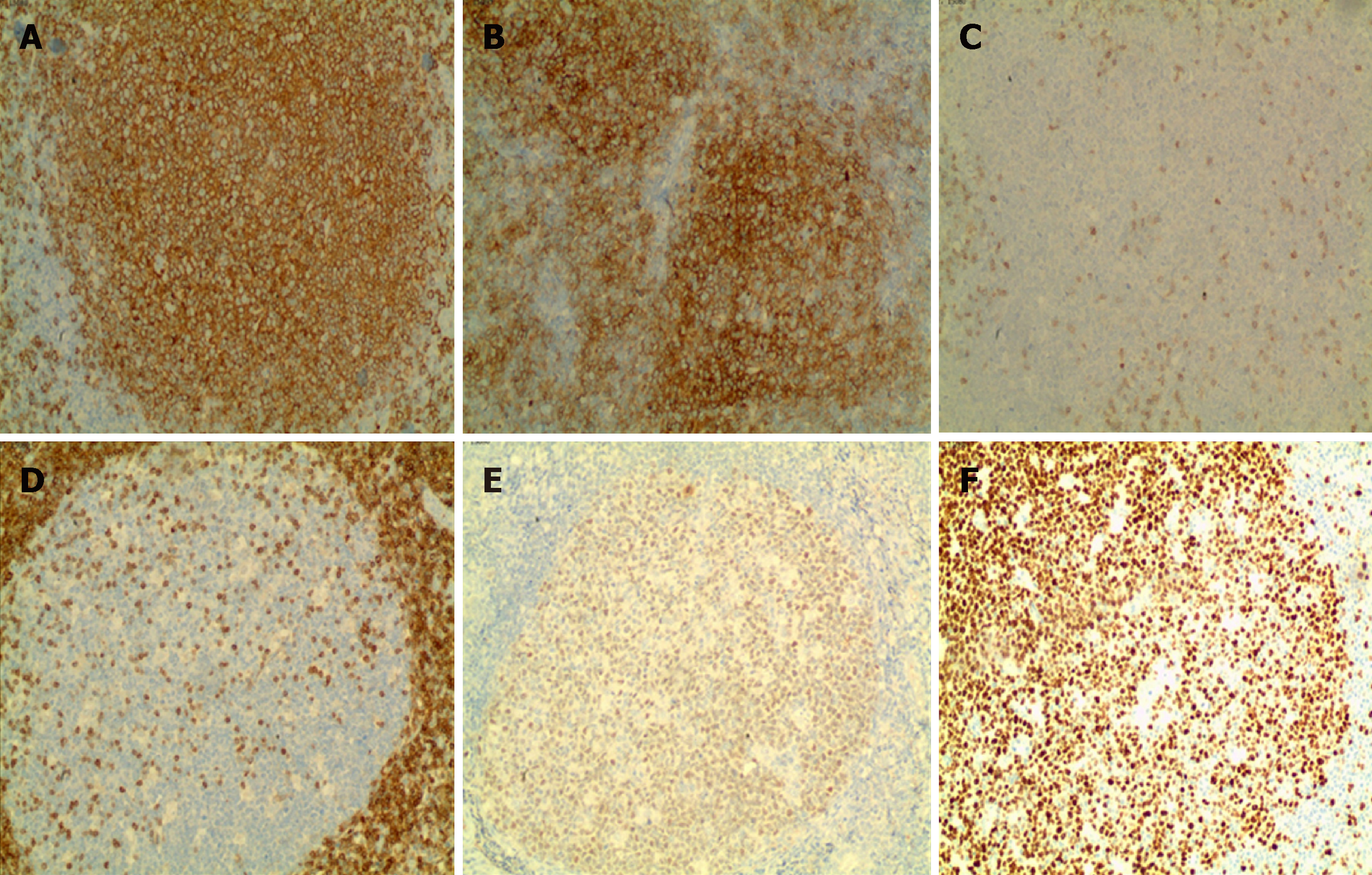
After the patient was admitted to the hospital, we performed gastrointestinal endoscopy and multi-point biopsy of the gastrointestinal mucosa. Gastroscopy revealed chronic superficial gastritis. Biopsy was performed for the gastric fundus, gastric body, gastric antrum, duodenal bulb, and duodenum descending area. Pathological diagnosis was chronic superficial gastritis in the fundus (eosinophil count < 20/HPF [high-power fields]); chronic superficial gastritis with intestinal metaplasia in gastric body (eosinophil count < 20/HPF); chronic superficial gastritis and focal glandular epithelial metaplasia in the gastric antrum (eosinophil count < 20/HPF), and chronic inflammation in the duodenal bulb and descending area (eosinophil count < 20/HPF) (Figure 1). Colonoscopy showed no obvious ab-normalities in the ileum and colon mucosa. Multi-point biopsy by colonoscopy was performed in the distal ileum, ascending colon, transverse colon, descending colon, sigmoid colon, and rectum. Pathological diagnosis was chronic inflammatory changes in mucus (eosinophil count < 20/HPF) (Figure 2). The smear showed mesothelial cells, phagocytic cells, a large number of lymphocytes, and a small amount of eosinophils (Figure 3). The routine examination failed to identify the cause. In order to further diagnose, the patient completed laparoscopy with full communication and informed consent of the patient and her family. The patient underwent intravenous general anesthesia and tracheal intubation. Under the umbilicus, a long observation hole of about 10 mm was constructed, and pneumoperitoneum was built with the pressure of 12-14 mmHg. A laparoscope was placed through the sheath for examination. According to the nature and location of the lesion, two additional holes were made as surgical operation holes. Under the laparoscope, we found that the abdominal cavity was scattered with a large number of nodular lesions. Part of the omentum resection was sent for pathological examination. Histopathology showed that there was diffuse lymphoid cell infiltration in omentum tissues. Thus, we consider lymphoproliferative disease. Immunohistochemistry showed that there was lymphoid tissue hyperplasia that was closely arranged in a follicular shape. No typical cuff structure was observed. Focal follicular fusion was observed. Central cells and centroblasts (>15/HPF) were seen in the follicles. Thus, we considered follicular lymphoma (grade 3a, follicular type) (Figure 4). Immunohistochemistry results showed CD20 (+), 20/HPF CD10 (+), Bcl-6 (+), Bcl-2 (-), CD3 (-), CD38, IgG, IgG4 (follicle cell plasma +), Ki-67 (60%), and CK (-) (Figure 5). After operation, the patient had no complications such as bleeding or infection. The final diagnosis was peritoneal follicular lymphoma. The patient was immediately transferred to the local hematology department for further treatment. The patient was followed once a month for 11 mo. He had no ascites and was generally in good condition currently.
Follicular lymphoma.
We diagnosed the patient with ascites due to follicular lymphoma. After consultation with the Department of Hematology, the patient was transferred to the local hospital for further treatment. Since the patient was transferred to a local hospital, and the patient and his family members did not clearly describe the specific treatment plan, the emphasis was placed on the integrated treatment of traditional Chinese and Western medicine in the local hospital.
After 11 mo of follow-up, the patient's current condition was stable, and follicular lymphoma conversion was avoided.
Ascites is a common clinical manifestation. Common causes include cirrhosis, tuberculous peritonitis, and malignant tumors in the abdominal cavity. Cases with intractable ascites and/or ascites due to unknown reasons often have poor clinical outcomes or recurrent attacks, causing pain and increased medical burden to patients[2,3]. For clinically unexplained ascites, it is difficult to identify the cause relying only on clinical symptoms, serology, ascites puncture, cytology, ascites culture, imaging examination. This case in this report belongs to refractory ascites of unknown origin. Analysis of routine examination results, we first ruled out the possibility of tuberculous ascites and ascites due to cardiovascular, liver, kidney, and connective tissue diseases. This is because PPD test was negative, and chest X-ray findings were negative. Based on the patient’s history, there was no tuberculosis. Hepatitis B surface antigen was negative, rheumatoid immunity, and vasculitis were negative, and heart and kidney functions were normal. We also ruled out the possibility of eosinophilic gastroenteritis. The patient's blood routine examination showed a significant increase in the ratio of lymphocytes and eosinophils. The CT performed in other hospital indicated mucosal thickening in the gastric antrum. We have improved gas-trointestinal endoscopy and multi-point biopsy of the gastrointestinal tract, but the gastrointestinal mucosa pathology suggested that the eosinophil count was less than 20/HPF. In addition, during the course of treatment, the patient has a large amount of ascites, and ascites repeatedly occurred after drainage or diuretics treatment. Because the therapeutic effect was poor, it was possible to consider tumoral ascites. However, cytology of ascites did not identify tumor cells. We have seen a large number of lymphocytes in the patient's ascites, and we still consider the possibility of lymphoma. At the same time, the patient's abdominal-pelvic CT examination showed that the peritoneum had extensive nodular thickening, and multiple intra-abdominal soft tissue masses, leading to the consideration of the malignant tumor, peritoneal metastasis, and multiple lymph node metastasis. Finally, we decided to give patients laparoscopy to further confirm the diagnosis. The abdominal cavity was scattered with the nodular lesions and tissues were collected for biopsy during operation. Pathology indicated lymphoproliferative disorders. Immunohistochemistry indicated follicular lymphoma (grade 3a, follicular type). Finally, the patient was diagnosed with follicular lymphoma. We diagnosed the patient with ascites due to follicular lymphoma. After consultation with the Department of Hematology, the patient was transferred to the local hospital for further treatment. After 11 mo of follow-up, the patient's current condition was stable, and follicular lymphoma conversion was avoided. In the diagnosis of follicular lymphoma-induced ascites, we had the following experience. First, the patient had large amounts of ascites with systemic skin pruritus and skin lesions, and there was no significant remission with common anti-histamine treatment. Second, blood tests suggested that eosinophils were elevated significantly; IgG and IgE levels were significantly elevated, especially IgE. Third, laparoscopy and the rapid diagnosis are of great value for the treatment and prognosis.
It has been reported that laparoscopy can increase the rate of diagnosis for ascites of unknown origin. Laparoscopy plays a critical role in diagnosing and differentially diagnosing ascites of unknown origin through biopsy of the lesion. In particular, laparoscopy has higher value for atypical cases[4,5]. First, abnormalities can be visually detected. It can observe the color, exudation, nodule, mass, and blood vessel distribution of the peritoneum in the parietal and visceral layers. Second, laparoscopic image enlargement function can detect miliary nodules with a diameter of 1-2 mm for small lesions with high resolution, while B-mode ultrasound, CT, and magnetic resonance imaging can only find lesions with a diameter of 1-2 cm or more. Third, it is highly targeted and has little damage. It can accurately take suspicious tissues to avoid damage to normal organs. Tissue biopsy can provide important evidence for treatment and prognosis.
When it is difficult to confirm the diagnosis through laboratory examinations and various imaging diagnostic techniques, laparoscopy shows its unique and accurate diagnostic effect, which can make up for the deficiencies of these examinations. Laparoscopic examination has fewer complications and less pain. It can not only directly observe normal organs and diseased tissues, but also can perform biopsy under direct vision and obtain evidence of medical examinations to assist treatment. Laparoscopy has been applied to the diagnosis of abdominal trauma, hepatitis, tuberculosis, ascites, abdominal masses, metastatic cancer in the abdominal cavity, and liver cancer. Laparoscopy can also be used for accurate staging of intra-abdominal malignancies, which can avoid unnecessary laparotomy.
Currently, there are very few peritoneal follicular lymphoma cases diagnosed by laparoscopy. Follicular lymphoma accounts for 22% of non-Hodgkin lymphomas in the world. The most common manifestation of follicular lymphoma is painless lymphadenopathy, typically characterized by multiple sites of lymphoid tissue invasion. Most patients do not have fever, night sweats, or weight loss[6,7]. A suitable biopsy evaluated by the hematology and pathology experts is sufficient to make a diagnosis of follicular lymphoma. Follicular lymphoma is one of malignant tumors that are most sensitive to chemotherapy and radiotherapy. Follicular lymphoma has a high rate of conversion to diffuse large B-cell lymphoma (7% per year).
About 40% of patients undergoing a repeat biopsy at some time during the course of the disease have been confirmed to have conversion, and almost all patients at the time of death had conversion. This conversion is often foreseen due to rapid lymph node growth and systemic symptoms such as fever, night sweats, and weight loss[8-10]. Laparoscopy is very useful for diagnosing ascites due to unexplained reasons, and it is sometimes important for determining the treatment plan for those patients and predicting the prognosis.
Laparoscopic abdominal examination is of great significance for the definite diagnosis of ascites due to an unknown reason.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Abadi ATB, Yamamoto K S-Editor: Ji FF L-Editor: Wang TQ E-Editor: Wu YXJ
| 1. | Bedioui H, Ksantini R, Nouira K, Mekni A, Daghfous A, Chebbi F, Rebai W, Fteriche F, Jouini M, Kacem M, Ben Mami N, Filali A, Bensafta Z. Role of laparoscopic surgery in the etiologic diagnosis of exsudative ascites: a prospective study of 90 cases. Gastroenterol Clin Biol. 2007;31:1146-1149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | ForŢofoiu MC, Popescu DM, Pădureanu V, Dobrinescu AC, Dobrinescu AG, Mită A, Foarfă MC, Bălă VS, Muşetescu AE, Ionovici N, ForŢofoiu M. Difficulty in positive diagnosis of ascites and in differential diagnosis of a pulmonary tumor. Rom J Morphol Embryol. 2017;58:1057-1064. [PubMed] |
| 3. | Caly WR, Abreu RM, Bitelman B, Carrilho FJ, Ono SK. Clinical Features of Refractory Ascites in Outpatients. Clinics (Sao Paulo). 2017;72:405-410. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Maeda S, Yabuuchi J, Nobuta H, Makiishi T, Hirose K. Characteristics of Patients and Their Ascites Who Underwent Repeated Cell-Free and Concentrated Ascites Reinfusion Therapy. Ther Apher Dial. 2015;19:342-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Valle SJ, Alzahrani NA, Alzahrani SE, Liauw W, Morris DL. Laparoscopic hyperthermic intraperitoneal chemotherapy (HIPEC) for refractory malignant ascites in patients unsuitable for cytoreductive surgery. Int J Surg. 2015;23:176-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Seike T, Inamura K, Okuno N, Asaumi Y, Takata Y, Okamura T, Matano S, Terahata S, Sakatoku K, Kawai H. [A case of gastric follicular lymphoma resected and diagnosed with laparoscopy and endoscopy cooperative surgery]. Nihon Shokakibyo Gakkai Zasshi. 2017;114:1996-2004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Prettyjohns M, Hoskin P, McNamara C, Linch D; NICE non-Hodgkin Lymphoma Clinical Guideline Committee. The cost-effectiveness of immediate treatment or watch and wait with deferred chemotherapy for advanced asymptomatic follicular lymphoma. Br J Haematol. 2018;180:52-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Lackraj T, Goswami R, Kridel R. Pathogenesis of follicular lymphoma. Best Pract Res Clin Haematol. 2018;31:2-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 9. | Hess G. The role of stem cell transplantation in follicular lymphoma. Best Pract Res Clin Haematol. 2018;31:31-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Cheah CY, Fowler NH. Novel agents for relapsed and refractory follicular lymphoma. Best Pract Res Clin Haematol. 2018;31:41-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |