Published online Mar 26, 2019. doi: 10.12998/wjcc.v7.i6.778
Peer-review started: November 12, 2018
First decision: December 12, 2018
Revised: January 17, 2019
Accepted: February 26, 2019
Article in press: February 26, 2019
Published online: March 26, 2019
Processing time: 136 Days and 20.5 Hours
Angiolipoma is a benign tumor and is generally found in subcutaneous tissues. Angiolipomas are rare in the gastrointestinal tract, including the stomach. Preoperative diagnosis of the tumor is difficult, although there are several radiological examinations such as computed tomography and endoscopic ultrasound.
We report a 24-year-old Chinese man with multiple gastric angiolipomas, with a positive stool occult blood examination. Endoscopic biopsy only showed nonspecific inflammation. Histological examination of the specimen by endoscopic snare resection showed that the tumor consisted of adipose tissues and blood vessels. We also performed a literature review. After the use of proton pump inhibitor, the fecal occult blood test was negative. Due to the difficulty of resecting multiple lesions in the stomach completely and the benign characteristics of angiolipoma, we chose to have regular upper gastrointestinal endoscopy evaluation of the lesion. No evidence of significant change in lesion size was detected after 3-years follow-up.
Gastric angiolipoma is rare, and benign neoplasm should be considered when lesions occur submucosally in the gastrointestinal tract.
Core tip: Angiolipoma in the gastrointestinal system is a rare entity, and angiolipoma in the stomach is extremely rare, with difficult preoperative diagnosis. We report a patient with multiple gastric angiolipomas with weakly positive stool occult blood examination. Endoscopic and radiological examinations, such as computed tomography, were used. The specimen was obtained by endoscopic snare resection for histopathological evaluation. Multiple angiolipomas in the gastrointestinal system are extremely rare in the recent literature. We also performed a brief review to investigate the clinical characteristics, diagnosis, and management of gastric angiolipoma.
- Citation: Lou XH, Chen WG, Ning LG, Chen HT, Xu GQ. Multiple gastric angiolipomas: A case report. World J Clin Cases 2019; 7(6): 778-784
- URL: https://www.wjgnet.com/2307-8960/full/v7/i6/778.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i6.778
Angiolipomas are benign tumors made up of adipose tissue and proliferated blood vessels. They are subcutaneous tumors and are commonly found in the arms and trunk[1]. They are rarely seen in the gastrointestinal system[2]. Although endoscopic and radiological examinations can demonstrate the lesion in the gastrointestinal tract, preoperative diagnosis of angiolipomas is still difficult and the final diagnosis is dependent on histopathological evaluation[3]. According to the current literature, only four cases of gastric angiolipoma, which all occurred as a solitary lesion, have been reported[4-7] (Table 1). Here, we describe a case of multiple gastric angiolipomas diagnosed after endoscopic snare resection.
| Literature | Age/sex | Size in cm | Symptom | Imaging | Follow-up |
| DeRidder et al[4], 1989 | 59/M | 0.6 | Black stool | Nil | 1 years; No; Recurrence |
| McGregor et al[5], 1993 | 69/M | 5 × 4 × 2 | Severe anemia | Nil | 2.5 years; No recurrence |
| Hunt et al[6], 1996 | 27/F | 8 × 5.5 × 4.5 | Acute gastrointestinal hemorrhage | Nil | Not given |
| Nam et al[7], 2014 | 58/F | 1.6 × 1.5 × 1.4 | Melena and anemia | CT: Submucosal lesion, diffuse fluid density; EUS: A polypoid mass, superficial ulceration covered with whitish exudates | Not given |
A 24year-old man visited our hospital due to a 4-year history of a space-occupying lesion in the stomach that was detected at another hospital. He had no complaint of abdominal pain, bloody stools, or weight loss.
He had upper gastrointestinal hemorrhage 4 years ago and underwent an operation for right carpal tunnel syndrome. The postoperative pathology showed fibrous tissue hyperplasia collagen and adipose tissue with vascular proliferation.
He underwent an operation on his right arm.
His family history and past medical history were both unremarkable. He had no history of using nonsteroidal anti-inflammatory drugs or other drugs that cause gastrointestinal bleeding.
During hospitalization, stool occult examination was weakly positive, and other routine laboratory parameters were within the normal range. Tumor markers including carcinoembryonic antigen and cancer antigen 125 were negative.
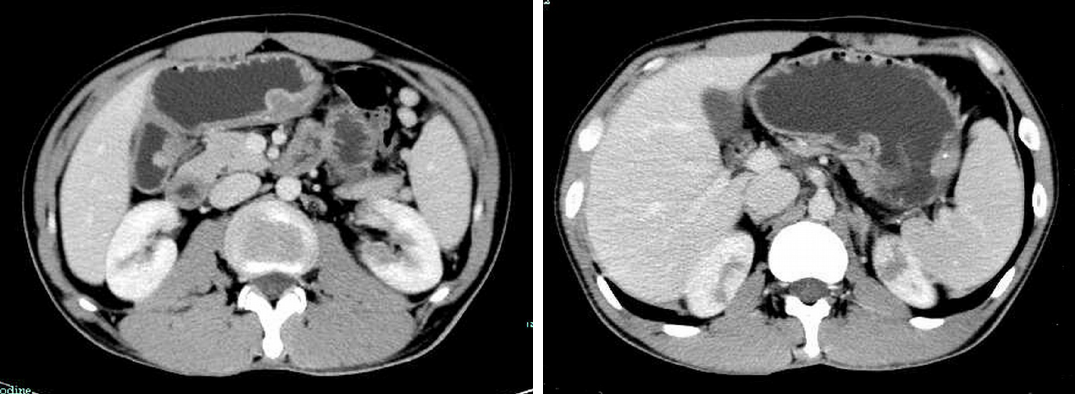
Computed tomography (CT) (Figure 1) showed that the walls of the greater curvature of the stomach and the antrum were significantly thickened, and some parts had protruding nodules. Spotted calcification could be seen inside the stomach. A lesion measuring 2.7 cm in diameter was located on the greater curvature. After contrast enhancement, the lesion was progressively enhanced. The serous membrane and surrounding fat space were still clear, and there were several small lymph nodes around the stomach. Mesenchymal tumors, neurogenic tumors, and vascular-derived tumors were considered.
Magnetic resonance imaging (MRI) revealed that the wall of the greater curvature was thickened and the antrum had outwardly protruding nodules. The boundary was clear and had longer signal intensity on T2-weighted images and high signal intensity on diffusion-weighted imaging.
Positron emission tomography (PET)-CT showed irregular thickening of the antrum wall, with multiple nodular shadows protruding outward. Some of them had calcifications and showed mildly increased uptake of fluorodeoxyglucose with standardized uptake value of 2.3. The differential diagnosis included low-metabolic tumor, mesenchymal tumor, and lymphoma.
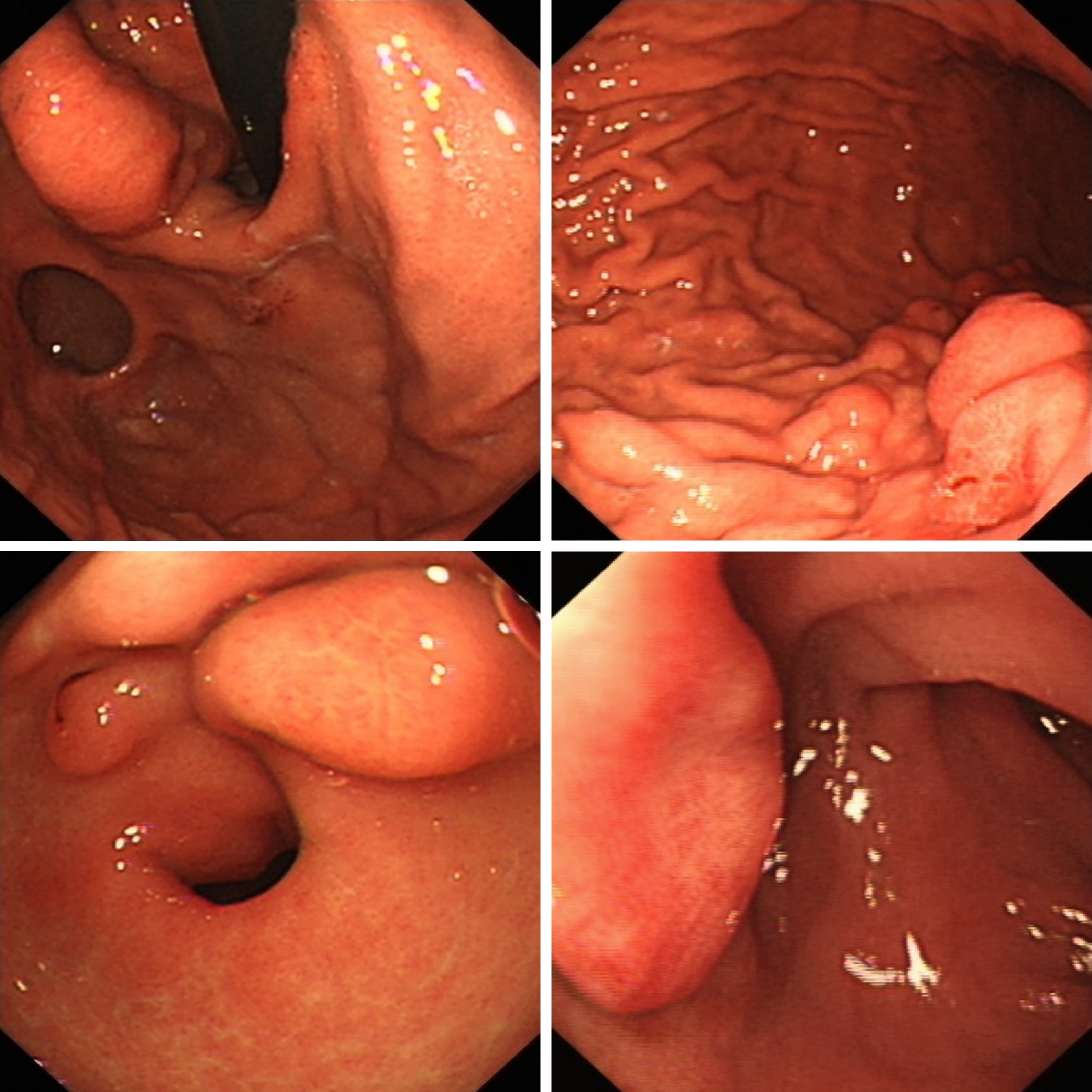
At upper gastrointestinal endoscopy (Figure 2), mucosal thickening of the stomach wall was identified in the gastric corpus, and biopsy showed a hard texture. Multiple submucosal nodules were seen in the antrum, the duodenal bulb, and the gastric corpus extended to the cardia. Some nodules had superficial congestion and hemorrhagic spots. Other parts of the stomach appeared normal. Endoscopic biopsy of the lesion only observed unspecific chronic inflammation of the mucosa without colonization by Helicobacter pylori.
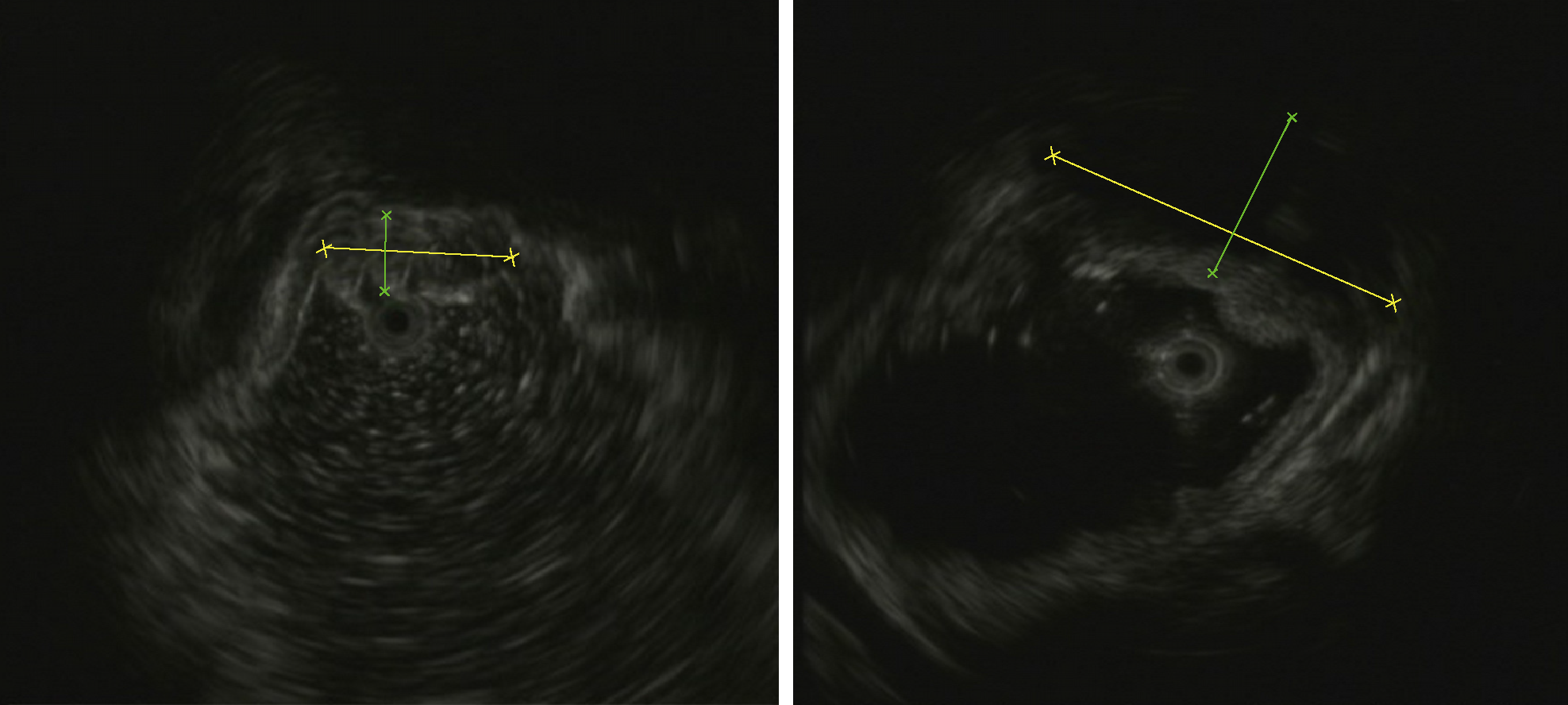
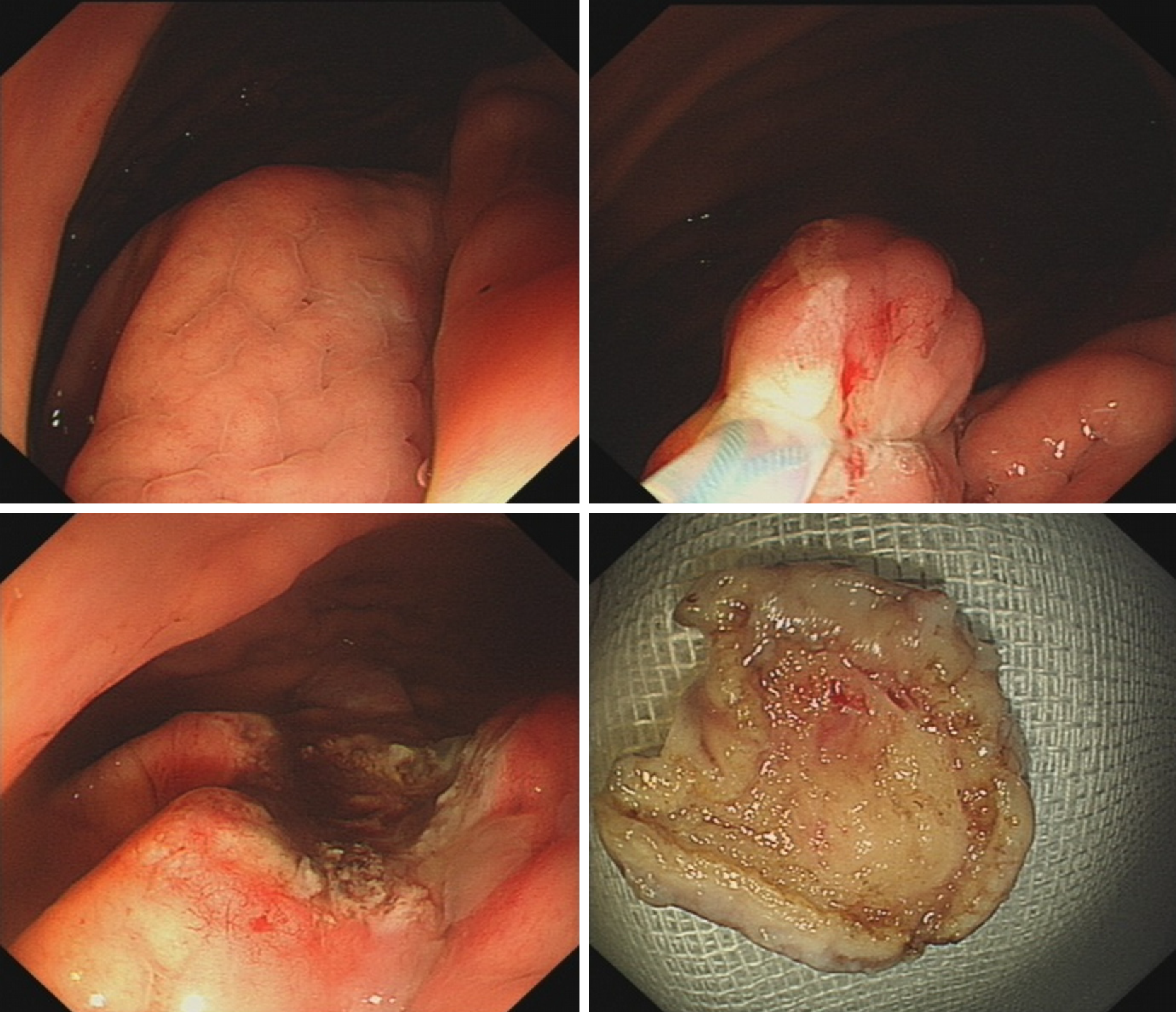
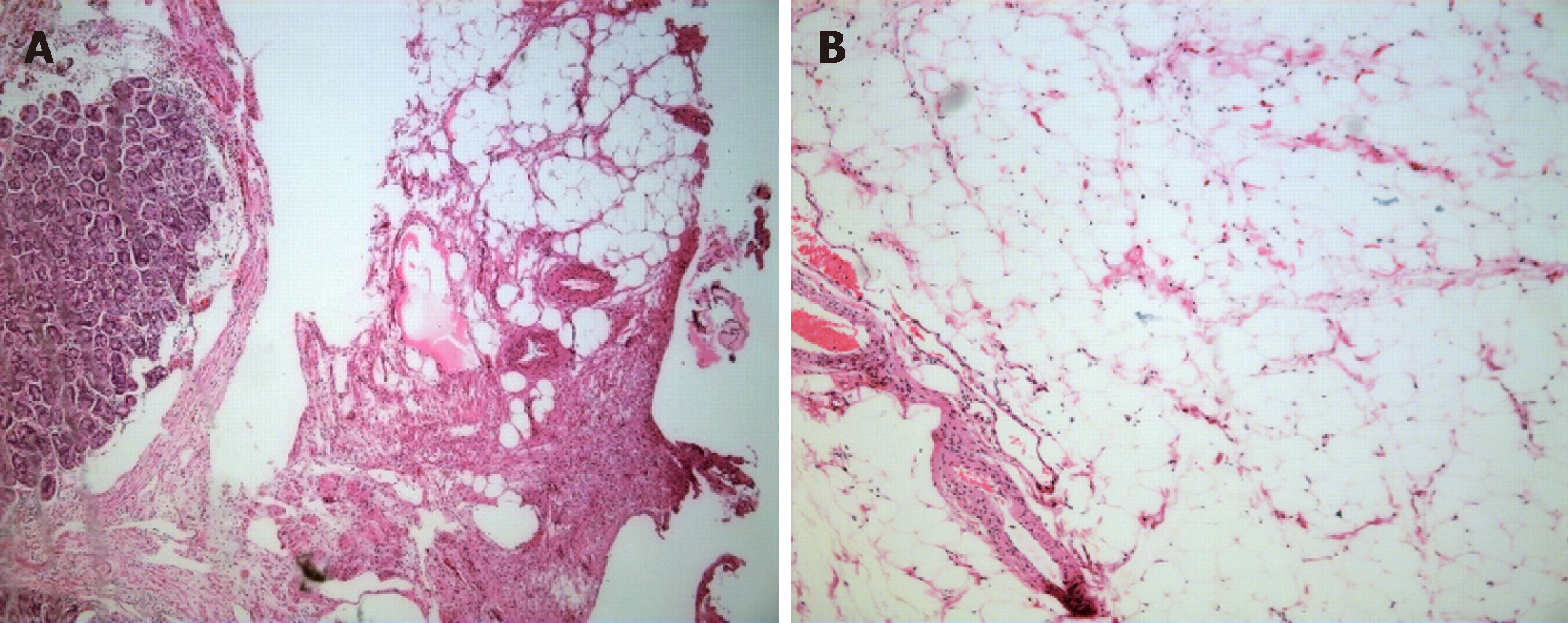
At endoscopic ultrasound (EUS) (Figure 3), multiple submucosal nodularities were seen in the antrum, with a smooth surface. These nodules were located in the mucosal layer, submucosa, and muscularis propria layer and were heterogeneous mixed hypoechoic and isoechoic lesions with hyperechoic spots. The lesion was not well defined, and multiple mucosal nodes were seen on the greater curvature of the stomach. The mucosal lesion appeared hyperemic and had old bleeding spots. The mucosal layer, the submucosa, and the muscularis propria were thickened inhomogeneously, and the lesion was hypoechoic yet heterogeneous. Histological examination by diagnostic endoscopic polypectomy snare (Figure 4 and Figure 5) showed that the gastric corpus had tumor-like hyperplasia of blood vessels and adipose tissue. There was no definite fibrin thrombus, and all cells investigated cytogenetically had a normal karyotype.
According to the imaging findings and histopathologic examination, this patient was diagnosed with multiple angiolipomas of the stomach.
After the use of proton pump inhibitor, the fecal occult blood test was negative. Due to the difficulty of resecting multiple lesions in the stomach completely and the benign characteristics of angiolipoma, it was inappropriate to undertake gastrectomy. Therefore, the patient chose to have regular upper gastrointestinal endoscopy evaluation of the lesion.
During outpatient follow-up, he had no characteristic clinical symptoms, and the routine examinations were repeatedly normal. No evidence of significant change in lesion size was detected after 3-years follow-up.
Bowen[8] first defined angiolipomas in 1912, and Howard et al[9] distinguished them from lipomas histopathologically in 1960. Angiolipomas are generally subcutaneous and capsulated, most commonly on the arms and trunk in young adults[10]. They are rarely found in the gastrointestinal tract. In a literature review, we found only four cases of angiolipomas involving the stomach, and all gastric lesions were solitary. Only one case of gastrointestinal angiolipomas reported a patient with duodenal and colonic angiolipomas[11]. To the best of our knowledge, our case is the first of multiple gastric angiolipomas diagnosed after endoscopic snare resection.
Gastrointestinal angiolipomas can be detected by many imaging methods including EUS, CT, or MRI before histopathological diagnosis[12,13]. EUS shows hyperechoic or isoechoic lesions in the submucosal layer[7,14,15]. Post-contrast CT does not show significant enhancement in some studies[16,17], but high-density lesions can be seen because of the different tissue composition of the lesions[13]. MRI shows the peripheral signal isointensity with a central high-intensity signal on T1-weighted and T2-weighted images[18]. PET-CT is less used for diagnosing angiolipomas and mildly increased fluorodeoxyglucose uptake can be visible on whole-body PET. The PET-CT findings are helpful to distinguish angiolipomas from malignant lesions[19-21]. We reported the first imaging findings of PET-CT of gastrointestinal angiolipomas. However, because of the lack of characteristic clinical presentations and specific findings on imaging studies, it is difficult to diagnose gastrointestinal angiolipomas before surgery. The final diagnosis is usually confirmed by surgical pathology.
In our case, although gastroscopy showed multiple bulges in the stomach, the biopsy specimen obtained only revealed chronic and moderate inflammation of the mucosa without tumor cells. Combined with the CT, EUS, and PET-CT findings, we doubted the presence of tumor in the stomach and chose to obtain a specimen by endoscopic snare resection. Finally, the histopathological evaluation showed a benign lesion with proliferated blood vessels and mature adipose tissue. Three years ago, the patient complained of a swollen right hand and underwent an operation for “right carpal tunnel syndrome”. Pathologic examination showed fatty tissue with vascular proliferation that was similar to the lesion in the stomach. Angiolipomas usually occurred in the trunk and the extremity, so we suspected it was an angiolipoma in the arm. Considering the multiple lesions and benign nature, the patient and we chose to follow up any change in the lesions rather than undergo radical resection.
Upper gastrointestinal examination to obtain a biopsy specimen is limited to superficial mucosa, and the features of gastric angiolipomas are nonspecific. For instance, our patient only showed weakly positive stool occult blood examination because of ulceration. Hence, the accuracy of preoperative diagnosis is not high, and the final diagnosis is mostly dependent on surgical excision.
Surgical resection is the main treatment option for gastrointestinal angiolipomas, and the recurrence rate is low when the tumor is completely removed. In reported cases, patients were treated by exploratory laparotomy with mass resection[4,5]. A case of a solitary Peutz–Jeghers-type polyp with an angiolipoma in the stomach[6] was treated with distal partial gastrectomy with Bilroth I reconstruction and resection of the polyp, due to the presence of intussusception and acute bleeding. In one case, laparoscopic wedge resection was also performed successfully[7]. The size of the reported angiolipomas ranges from 0.5 cm up to 5 cm in diameter. Three cases of gastric angiolipomas were presented with moderate or severe anemia. Surgery was performed in four previous cases because all of them had bleeding. There is no international standard. So, when considering the optimal treatment, the levels of urgency and lesion size are crucial factors. During follow-up, none of the cases in the literature recurred, and the prognosis was good. However, our patient diagnosed by histopathological evaluation did not choose to have surgical excision. Because our patient has multiple gastric angiolipomas invading the muscularis propria, it would have been difficult to resect the lesions completely by endoscopic submucosal dissection. Moreover, the patient in our case was not presented with anemia and only presented with a weakly positive fecal occult blood test. In addition, angiolipoma is universally benign and symptoms are mild, and gastrectomy would lead to a deteriorating quality of life.
In conclusion, gastric angiolipoma is rare, and we should be aware of the benign neoplasm when we find lesions occurring submucosally in the gastrointestinal tract. However, we should also pay attention to the pre- and/or intraoperative histological features to avoid an erroneous diagnosis and radical resection.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aghakhani A, Chiu CC, Ieni A S-Editor: Wang JL L-Editor: Filipodia E-Editor: Wu YXJ
| 1. | Lin JJ, Lin F. Two entities in angiolipoma. A study of 459 cases of lipoma with review of literature on infiltrating angiolipoma. Cancer. 1974;34:720-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Kacar S, Kuran S, Temucin T, Odemis B, Karadeniz N, Sasmaz N. Rectal angiolipoma: a case report and review of literature. World J Gastroenterol. 2007;13:1460-1465. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Liu YJ, Karamchandani DM. Gastric Angiolipoma: A Rare Entity. Arch Pathol Lab Med. 2017;141:862-866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | DeRidder PH, Levine AJ, Katta JJ, Catto JA. Angiolipoma of the stomach as a cause of chronic upper gastrointestinal bleeding. Surg Endosc. 1989;3:106-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | McGregor DH, Kerley SW, McGregor MS. Case report: gastric angiolipoma with chronic hemorrhage and severe anemia. Am J Med Sci. 1993;305:229-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Hunt J, Tindal D. Solitary gastric Peutz-Jeghers polyp and angiolipoma presenting as acute haemorrhage. Aust N Z J Surg. 1996;66:713-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Nam YH, Park SC, Kim HJ, Lee SW, Kim J, Choi DH, Kang CD, Lee SJ, Lee S. Angiolipoma of the stomach presenting with anaemia. Prz Gastroenterol. 2014;9:371-374. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Bowen JT. Multiple subcutaneous hemangiomas, together with multiple lipomas, occurring in enormous numbers in an otherwise healthy, muscular subject. Am J Med Sci. 1912;144:189-192. [RCA] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Howard WR, Helwig EB. Angiolipoma. Arch Dermatol. 1960;82:924-931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 236] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 10. | Punia RS, Jain P, Amanjit, Mohan H, Singh R. Subcutaneous angiolipomas: a clinicopathological study of 12 cases. Indian J Pathol Microbiol. 2005;48:197-198. [PubMed] |
| 11. | Mohl W, Fischinger J, Moser C, Remberger K, Zeuzem S, Stallmach A. Duodenal angiolipoma -- endoscopic diagnosis and therapy. Z Gastroenterol. 2004;42:1381-1383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Jung IS, Jang JY, Ryu CB, Hong SJ, Kim JO, Cho JY, Lee JS, Lee MS, Jin SY, Shim CS, Kim BS. Angiolipoma of the duodenum diagnosed after endoscopic resection. Endoscopy. 2004;36:375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Chen YY, Soon MS. Preoperative diagnosis of colonic angiolipoma: a case report. World J Gastroenterol. 2005;11:5087-5089. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Tang X, Tan Y, Liu D. Angiolipoma: a rare esophageal submucosal tumor. Gastrointest Endosc. 2017;86:399-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Jensen EH, Klapman JB, Kelley ST. Angiolipoma of the esophagus: a rare clinical dilemma. Dis Esophagus. 2006;19:203-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Molinares B, Goldstein A, Varela GJ, Mesa S. Colonic angiolipoma - a rare finding in the gastrointestinal tract. Case report and review of literature. J Radiol Case Rep. 2012;6:23-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Hang Y, Zhu CQ. Angiolipoma of the colon: A case report and literature review. J Dig Dis. 2014;15:154-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Kwak HS, Kim CS, Lee JM. Small intestinal angiolipoma: MR imaging appearance. Abdom Imaging. 2003;28:515-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Maurea S, Mainolfi C, Wang H, Varrella P, Panico MR, Klain M, Rossi R, Cremona F, Bazzicalupo L, Salvatore M. [Positron emission tomography (PET) with fludeoxyglucose F 18 in the study of adrenal masses: comparison of benign and malignant lesions]. Radiol Med. 1996;92:782-787. [PubMed] |
| 20. | Hsu CH, Yang CM, Cheng CJ. Angiolipoma detected by F-18 FDG positron emission tomography. Clin Nucl Med. 2003;28:604-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Suzuki R, Watanabe H, Yanagawa T, Sato J, Shinozaki T, Suzuki H, Endo K, Takagishi K. PET evaluation of fatty tumors in the extremity: possibility of using the standardized uptake value (SUV) to differentiate benign tumors from liposarcoma. Ann Nucl Med. 2005;19:661-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 56] [Article Influence: 2.9] [Reference Citation Analysis (0)] |