Published online Dec 26, 2019. doi: 10.12998/wjcc.v7.i24.4366
Peer-review started: August 12, 2019
First decision: October 24, 2019
Revised: November 8, 2019
Accepted: November 15, 2019
Article in press: November 15, 2019
Published online: December 26, 2019
Processing time: 134 Days and 23.3 Hours
Inflammatory myofibroblastic tumor (IMT) is a rare mesenchymal tumor that is characterized by spindle cells differentiated from muscle fibroblasts and infiltration of various types of inflammatory cells. IMT can occur at any age and at any anatomic site. The most common location of IMT is the bladder in the genitourinary tract. Only scarce cases of kidney IMT have been reported in the literature.
A 77-year-old woman, with a history of bilateral renal calculus for 15 years, was admitted to the Department of Urology of our hospital complaining of recurrent painless gross hematuria for one month. The treatment with cephalosporin was ineffective. Computed tomography imaging showed a mixed density and slightly heterogeneously enhanced lesion in the middle pole of the left kidney and ipsilateral adrenal enlargement. The patient underwent surgical treatment by retroperitoneoscopic left radical nephrectomy plus adrenalectomy. A large number of typical spindle cells surrounded by plasma cells and lymphocytes were observed microscopically. Immunohistochemical analyses indicated that these spindle cells were positive for vimentin, cytokeratin (CK), Ki-67, CK7, CD34, and CD31 and were focally positive for CD10 and anaplastic lymphoma kinase (ALK-1). Thus, a diagnosis of IMT was made definitively. The patient recovered well after operation, and no recurrence or metastasis was noted during the 22-mo follow-up.
Since kidney IMT is very rare and lacks characteristic clinical manifestation, it is easily misdiagnosed as a malignant tumor before operation. Surgery remains the best choice for diagnosis and treatment, and such cases must be followed carefully because of the uncertain biological behavior of this tumor. This report suggests that renal calculus may be one of the causes of IMT, but further investigation is necessary to prove it.
Core tip: Herein, we present an elderly woman with kidney inflammatory myofibroblastic tumor (IMT) characterized by painless gross hematuria and misdiagnosed as a malignant tumor with ipsilateral adrenal metastases. Kidney IMT is a rare tumor entity with unknown etiology, diverse clinical symptoms, and imaging manifestations. Renal calculus was suspected to be one of the causes or drivers of IMT because of the constant destruction of the kidney mucosa. The diagnosis of IMT is considered a great challenge before operation. However, the awareness of its existence and deep understanding of its clinical characteristics are essential to avoid misdiagnosis in the differential diagnosis of a renal mass and to provide better management of such cases. Despite the uncertain biological behavior of this type of tumor, most patients get a favorable prognosis after surgery.
- Citation: Zhang GH, Guo XY, Liang GZ, Wang Q. Kidney inflammatory myofibroblastic tumor masquerading as metastatic malignancy: A case report and literature review. World J Clin Cases 2019; 7(24): 4366-4376
- URL: https://www.wjgnet.com/2307-8960/full/v7/i24/4366.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i24.4366
Inflammatory myofibroblastic tumor (IMT) is a tumor subset belonging to the inflammatory pseudotumor family, which is a generic term for spindle cell proliferation in an uncertain anatomic location with diversified infiltrative inflammatory components. Although recent studies have suggested that IMT is a type of borderline neoplasm, it is still uncertain whether this type of tumor originates from an inflammatory or a cancerous process[1]. The most common anatomic location of IMT is the lungs, but there have been many reports of extrapulmonary IMT in recent years[1-9]. In the urinary system, the most common site of IMT is the bladder[10]; its occurrence in the kidney is extremely rare. To the best of our knowledge, only 48 cases of kidney IMT have been reported in the English literature between 1972 and 2019. Herein, we report an additional case of kidney IMT with a history of renal calculus and review the relevant literature to summarize the characteristics to increase our understanding of this disease and provide such patients with better management.
A 77-year-old woman who presented with recurrent painless gross hematuria was admitted to the Department of Urology of The Second Affiliated Hospital of Shenzhen University (Shenzhen, China).
The patient’s symptom started one month ago without other discomfort. She visited a local hospital for treatment two weeks ago. Ultrasound (US) examination revealed bilateral renal calculus, and routine urinalysis was positive for leukocytes. At that time, the physician suspected that the symptom was caused by calculous pyelonephritis, but treatment with cephalosporin was ineffective.
The patient had a medical history of renal calculus for 15 years.
The patient’s personal history and family history were unremarkable.
The results of the physical examination were nothing unusual.
Routine blood results suggested mild anemia and infection, with a hemoglobin level of 10.0 g/dL and a leukocyte count of 12.2 × 109 cells/L. Urinalysis showed a large number of red blood cells. Other laboratory results were within the normal limits, and no malignant cells were found in three urine cytopathologic analyses.
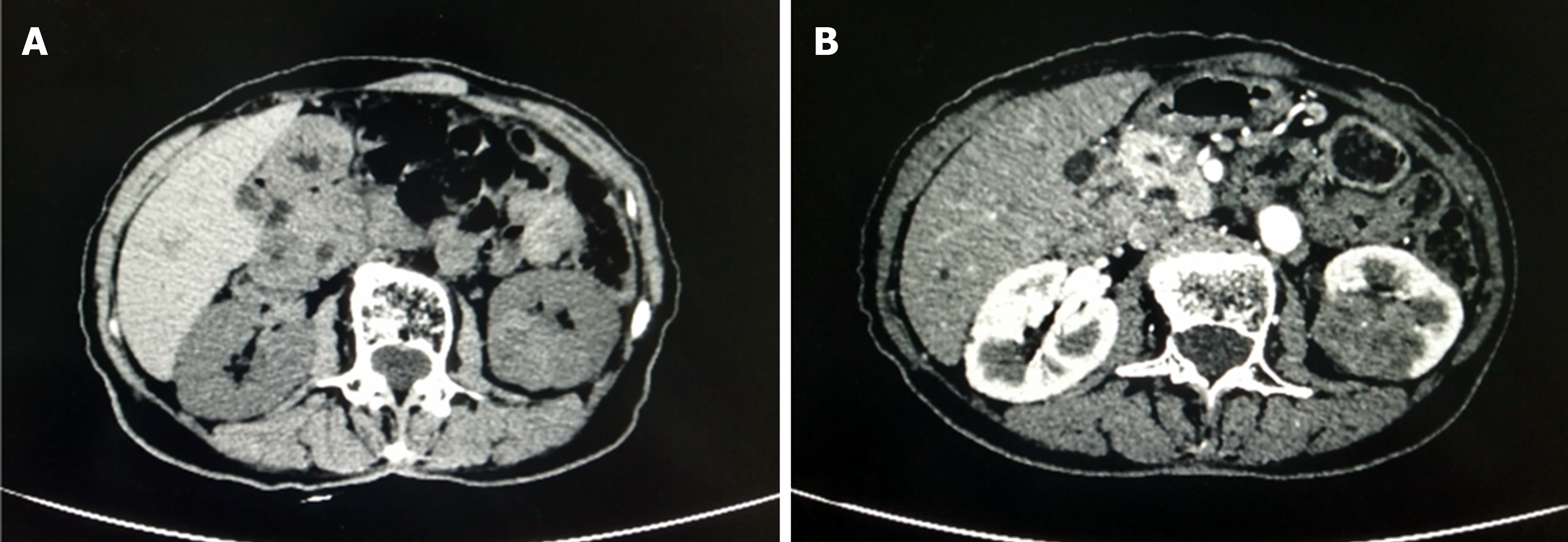
Abdominal ultrasound revealed only bilateral renal calculus, but no space-occupying lesions were observed. Computed tomography (CT) imaging showed a slightly heterogeneously enhancing mass in the middle pole of the left kidney and ipsilateral adrenal enlargement, which was suspected to be a metastatic lesion (Figure 1).
Considering the clinical symptoms and imaging findings, a malignancy, particularly renal cancer, was highly suspected.
A retroperitoneoscopic left radical nephrectomy plus adrenalectomy was performed.
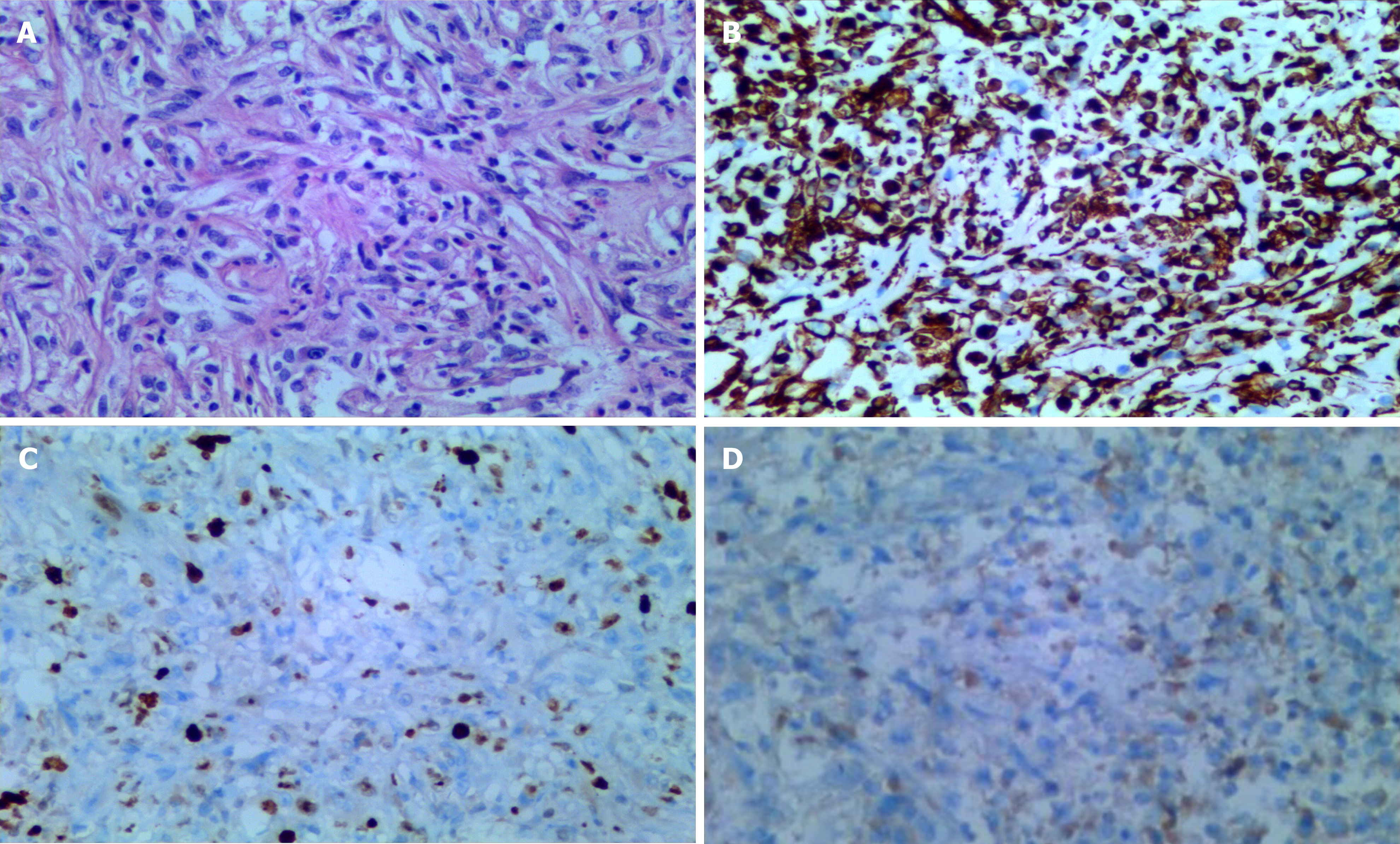
A grayish-white, well-defined, and stiff mass measuring 4 cm × 3 cm × 3 cm was discovered in the middle pole of the removed kidney specimens. Microscopically, typical spindle cells were widely distributed, with various types of infiltrating inflammatory cells, capillary hyperplasia, and local necrosis observed (Figure 2).
Immunohistochemical analyses revealed that these spindle cells were diffusely positive for vimentin, cytokeratin (CK), Ki-67, CK7, CD34, and CD31 and were focally positive for CD10 and anaplastic lymphoma kinase (ALK-1) (Figure 2).
This patient was diagnosed with IMT finally. The surgical margins were negative, and the adrenal gland was unremarkable.
The patient recovered well, and no complications occurred. No other treatment was performed after surgery. After 22 mo of follow-up, she was still alive, without symptoms or imaging evidence of recurrence or metastasis.
IMT, a type of rare mesenchymal tumor with intermediate biological potential, is mainly composed of spindle cells and inflammatory cell infiltration. It was first reported in 1937. The early literature suggested that the spindle cell proliferation was mainly a reactive hyperplasia that occurred after inflammation, and thus, IMT was thought to be an inflammatory pseudotumor. Later, as the research progressed, spindle cells were found to be the main component of these lesions; thus, it was classified as a tumor, typically a borderline tumor. However, the potential for local invasion, recurrence, and metastasis of IMT cannot be ignored[3,4]. Therefore, some scholars suggested that IMT should be redefined as a low-grade malignant tumor[3,4]. In recent years, in addition to the lungs, IMT has also been reported in extrapulmonary tissues, including the head and neck, ventricles, liver, retroperitoneum, pelvis, and spinal canal[1-9]. In the genitourinary system, IMT was found to occur in the bladder, ureter, urachal, renal pelvis, and kidney[11-15] . Although most commonly found in the bladder[10], IMT in the kidney is extremely rare. IMT is found more frequently in children than in adults and has no gender predilection, but the extrapulmonary forms occur more commonly in adult women[1].
According to our investigation, few scholars have systematically analyzed the clinical features of kidney IMT. To further study the characteristics of this type of IMT, we reviewed case reports published in MEDLINE and PubMed databases between 1972 and 2019, including 48 cases occurring in the renal parenchyma (37 cases) and renal pelvis (11 cases) (Table 1). Although the patients ranged in age from 3 to 75 years[6,7], those aged over 40 years accounted for 73% (35/48) of cases. Only five patients were younger than 14 years old. Fifty-four percent of these cases occurred in males. Fifty percent of kidney IMT occurred in the left kidney, while the other 50% occurred in the right kidney. Notably, kidney IMT was more inclined to the upper pole than the lower pole (ratio, 13:7). The clinical manifestations included low back or abdominal pain (54%), gross or microscopic hematuria (29%), incidental findings (23%), fever (19%), and weight loss (17%). The tumor sizes reported in the literature varied from 1.5 cm to 13.5 cm (median, 4.85 cm) based on imaging or pathological specimens. The majority of patients opted for radical surgery, while three patients were treated by partial resection, two treated with corticosteroids, and three with antibiotics. All patients achieved satisfactory outcomes, and no clinical or radiographic evidence of recurrence or metastasis was noted during 3 to 66 mo of observation.
| Case | Ref. | Age (yr)/gender | Clinical features | Location | Size (cm) | Treatment | Follow-up (mo) | Recurrence |
| 1 | Heerwagen et al[6] | 75/M | Accident finding, anemia | Rt lower | 10 | Nephrectomy | 10 | No |
| 2 | Gwynn et al[10] | 46/M | Abdominal discomfort, gastrointestinal symptoms | Rt | 13 | Nephrectomy | 13 | No |
| 3 | Tarhan et al[23] | 10/F | Recurrent high fever, headache | Rt middle | NA | Nephrectomy | 18 | No |
| 4 | Wu et al[32] | 43/M | Low back pain, hematuria | Lt renal pelvis | 1.5 | Nephrectomy | 26 | No |
| 5 | Li et al[36] | 61/M | Lethargy, night sweats, weight loss | Rt and Lt | NA | Biopsy, corticosteroid | 48 | No |
| 6 | Liang[28] | 60/F | Accident finding | Lt upper | 10.1 | Partial nephrectomy | 63 | No |
| 7 | Li et al[9] | 48/F | Accident finding | Lt upper | 2.9 | Nephrectomy | 6 | No |
| 8 | Dogan et al[7] | 3/M | Low back pain, recurrent fever | Rt upper | 6 | Nephrectomy | 6 | No |
| 9 | Ho et al[14] | 3/F | Abdominal pain, intermittent fever | Lt UPJ | 8 | Conservative surgery | 9 | No |
| 10 | Sun et al[21] | 54/F | Accident finding | Rt upper | 1.5 | Nephrectomy | NA | NA |
| 11 | Nakamura et al[26] | 60/M | Accident finding | Lt middle | 5.5 | Nephrectomy | NA | No |
| 12 | Tazi et al[15] | 56/M | Low back pain, weight loss | Rt lower | 6 | Nephrectomy | NA | NA |
| 13 | Sugimoto et al[35] | 20/F | High fever, right lumbago | Rt renal pelvis | 2.5 | Antibiotics | NA | NA |
| 14 | Babu et al[24] | 51/M | Low back pain | Lt upper | 8.2 | Nephrectomy | NA | NA |
| 15 | Ishikawa et al[25] | 38/M | Accident finding | Lt upper | 11 | Nephrectomy | NA | NA |
| 16 | Khallouk et al[39] | 57/M | Low back pain, hematuria | Rt middle | 9 | Nephrectomy | 14 | No |
| 17 | Taheri et al[40] | 15/F | Low back pain, hematuria, weight loss | Lt upper | 13.5 | Nephrectomy and adrenalectomy | 12 | No |
| 18 | Selvan et al[41] | 56/M | Accident finding | Lt middle | NA | Nephrectomy | 12 | No |
| 19 | Leroy et al[42] | 37/M | Low back pain, hematuria | Rt renal pelvis | NA | Nephrectomy | 12 | No |
| 20 | Navale et al[30] | 32/M | Lower abdominal pain, urinary tract symptoms | Rt lower | 4.5 | Nephrectomy | 18 | No |
| 21 | Bektas et al[43] | 51/F | Low back pain | Lt upper | 4.5 | Nephrectomy and adrenalectomy | 18 | No |
| 22 | Heerwagen et al[6] | 40/F | Accident finding | Rt lower | 7 | Nephrectomy | 24 | No |
| 23 | Pothadiyil et al[44] | 50/M | Low back pain | Lt | NA | Nephrectomy | 24 | No |
| 24 | Vujanić et al[45] | 8/M | Painless gross hematuria | Rt lower | 6 | Nephrectomy | 36 | No |
| 25 | Epaulard et al[46] | 60/M | Fever, weight loss, weakness, night sweats | Rt middle | 3 | Nephrectomy | 3 | No |
| 26 | Sugimoto et al[47] | 61/M | Abdominal pain | Rt renal pelvis | 3 | Nephrourete-rectomy | 3 | No |
| 27 | Ryu et al[48] | 61/F | Accident finding, weight loss, gastrointestinal symptoms | Lt lower | 3 | Nephrectomy | 3 | No |
| 28 | Iida et al[49] | 54/F | Painless gross hematuria | Rt renal pelvis | 4.7 | Nephrourete-rectomy | 44 | No |
| 29 | Wang et al[50] | 74/F | Low back pain, weight loss | Lt upper | 8 | Nephrectomy | 66 | No |
| 30 | Boo et al[51] | 9/F | intermittent abdominal pain, weight loss | Lt upper | 5.5 | Nephrectomy and enlarged lymph dissection | 6 | No |
| 31 | Leroy et al[42] | 54/F | Low back pain, hematuria | Lt renal pelvis | 1.5 | Nephrectomy | 7 | No |
| 32 | Petrescu et al[52] | 57/M | Hematuria, minimal grade fever, right flank pain | Rt middle | 2 | Nephrourete-rectomy | NA | NA |
| 33 | Mukkamala et al[53] | 54/M | Accident finding | Lt middle | 4.7 | Nephrectomy | NA | NA |
| 34 | Hori et al[54] | 24/F | Accident finding | Lt | 7.5 | Nephrectomy | NA | NA |
| 35 | Yoshida et al[55] | 44/M | Painless gross hematuria | Lt UPJ | NA | Nephrourete-rectomy | NA | NA |
| 36 | Bildirici et al[56] | 42/F | Low back pain | Rt upper | 7 | Nephrectomy | NA | NA |
| 37 | Kobayashi et al[57] | 50/M | Accident finding | Rt middle | 3 | Corticosteroid | NA | NA |
| 38 | Lee et al[58] | 48/M | Accident finding | Rt middle | 3.5 | Partial nephrectomy | NA | NA |
| 39 | Iwaki et al[59] | 73/M | General malaise, minimal grade fever | Lt lower | 3.5 | Nephrectomy | NA | NA |
| 40 | Kim et al[60] | 60/M | Painless gross hematuria | Rt renal pelvis | 1.6 | Nephrectomy | NA | NA |
| 41 | Satoh et al[61] | 61/M | Painless gross hematuria | Rt | 1.8 | Nephrourete-rectomy | NA | NA |
| 42 | Shah et al[62] | 42/F | Abdominal pain, hematuria | Rt renal pelvis | 6 | Nephrectomy | NA | NA |
| 43 | Bildirici et al[56] | 42/F | Low back pain | Rt upper | 7 | Nephrectomy | 12 | No |
| 44 | Dogan et al[7] | 15/F | Abdominal pain, recurrent fever | Lt upper | 7 | Biopsy, antibiotics | 8 | No |
| 45 | Bell et al[63] | 37/M | Abdominal pain, hematuria, fever | Lt upper | 2.5 | Nephrectomy | 8 | No |
| 46 | Ma et al[64] | 42/F | Abdominal pain, nausea, fatigue, weight loss | Rt and Lt | NA | Biopsy, corticosteroid | NA | No |
| 47 | Tambo et al[65] | 46/F | Accident finding, microscopic haematuria | Rt | 5 | Retroperitoneal tumor resection and additional right nephrectomy | 9 | No |
| 48 | Hattori et al[66] | 60/F | Low back pain | Lt renal pelvis | 4 | Nephrourete-rectomy | NA | NA |
| 49 | Present case | 77/F | Painless gross hematuria | Lt middle | 4 | Nephrectomy and adrenalectomy | 22 | No |
The causes of IMT remain unclear. According to the literature, chronic inflammation, surgery, and trauma are considered predisposing factors for IMT. Some scholars believe that it is related to Epstein-Barr virus infection[8], while others have found an association between IMT and hepatitis B virus infection[9]. Specific pathogen infections, such as Mycobacterium tuberculosis infection and Eikenella corrodens infection, are also reputed to be a cause[16,17]. The pathogenesis of IMT is also a controversial topic. Most scholars consider that chromosomal aberrations, especially kinase fusions or rearrangements, are the genetic basis of IMT tumorigenesis. The most common gene involved in IMT is the ALK gene, which is located on 2p23 and has been implicated in 50% of patients. Fusion partners, including the tropomyosin (TPM3/4), clathrin heavy chain, and ran-binding protein 2 (RANBP2) genes, have been found in patients with ALK-positive IMT, while the reactive oxygen species (ROS-1) and platelet-derived growth factor (PDGFRβ) genes were found to be involved in ALK-negative IMT[18,19]. ALK is more commonly expressed in children and is associated with tumor aggressiveness and high recurrence rates[20]. Fibroblast proliferation is proposed to be the intermediate process of IMT formation, but the specific relationship remains to be elucidated[21]. In our case, kinase fusions of ALK gene might be a main mechanism. More importantly, based on the view that chronic inflammation is believed to be the cause, we proposed a new point of view that renal calculus is one of the causes of IMT. Chronic injury and inflammation of the kidney mucosa, promoting the process of tumorigenesis, were considered to be the intermediate stages of tumor formation. But more case studies are needed to support this opinion.
Kidney IMT lacks specific clinical symptoms. This disease starts insidiously and develops slowly, mainly occurring in middle-aged and elderly individuals, without a sex predilection. Kidney IMT is frequently circumscribed and confined to a single organ. Pain and hematuria are the most common symptoms, while some patients showed simple low back pain or abdominal pain, some showed simple gross hematuria, and others presented with both types of symptoms. A small number of cases were accompanied by systematic and biological symptoms, such as weight loss, intermittent fever, anemia, naupathia, urinary tract symptoms, weakness, night sweats, and thrombocytosis, which gradually resolved after treatment. In our case, the patient presented with painless gross hematuria and had a history of kidney calculi for 15 years, which was misdiagnosed as urinary calculi or urothelial neoplasms based on the initial examinations.
The imaging manifestations of kidney IMT are also nonspecific and inconclusive. Hypoechoic and intratumoral vascular distribution are shown on US imaging, which is difficult to differentiate from malignant tumors[22]. CT and magnetic resonance imaging (MRI) are more accurate for the diagnosis of kidney lesions. By CT imaging, most kidney IMTs frequently show ill-defined, hypodense, hypovascular, slightly homogeneously enhanced lesions or enhanced thick-wall cystic lesions[23,24]. An area of calcification can be seen in the tumor entities[25]. Kidney IMT often exhibits variable signal intensity on MRI T1-weighted imaging (T1WI) and low signal intensity on T2WI[26]. Although fluorodeoxyglucose (FDG) uptake in IMT vary, positron emission tomography/CT (PET/CT) may possess considerable advantages for detecting primary tumors as well as recurrence and distant metastasis[27]. In our case, the lesion exhibited mixed density, clear boundaries, and uneven enhancement on CT imaging, which is difficult to differentiate from renal malignant tumors. Unfortunately, MRI or PET/CT was not performed, as we did not suspect IMT. Thus, effectively identifying this rare disease by imaging alone is challenging.
Kidney IMT needs to be differentiated from malignant tumors, such as renal pelvic carcinoma, renal cell carcinoma (RCC), sarcomatoid renal cell carcinoma, cystic renal carcinoma, inflammatory fibrosarcoma, low-grade neurogenic tumor, malignant fibrous histiocytoma, and dendritic cell tumors and benign tumors, such as angiomyolipoma, xanthogranuloma pyelonephritis, and plasma cell granuloma. It is most important to distinguish renal IMT from RCC and sarcomatoid renal cell carcinoma. Cystic renal IMT should be carefully differentiated from cystic renal cancer[28]. In our case, the lesion was assumed to be a renal malignant tumor that had most likely metastasized to the ipsilateral adrenal gland before surgery. In actuality, it is often misdiagnosed as a malignancy, which accounts for at least 67% (33/49) according to our calculations.
The final diagnosis usually depends on histopathological and immun-ohistochemical features. The most common histomorphology is characterized by the differentiation of myofibroblast-derived spindle cells and abundant infiltrative chronic inflammatory components, such as eosinophils and lymphocytes. Mucinous, vascular, and inflammatory areas and dense plate-like collagen are also important histologic features[29]. In addition, osteoblastic cells and heteromorphic bone composition are observed in certain cases[30]. Immunohistochemical analyses confirmed that vimentin, muscle-specific actin, smooth muscle actin (SMA), and CK were positive in IMT[29]. Furthermore, Li et al[31] described that the positive rates of vimentin, SMA, desmin, ALK, and CK in 30 patients with extrapulmonary IMT were 100%, 70%, 27%, 27%, and 13%, respectively.
In clinical practice, surgical resection of the lesion is recommended as the first-line treatment for IMT. For patients with only one kidney, bilateral masses, or kidney insufficiency, a biopsy and intraoperative rapid pathological examination were strongly advocated by some authors because of the advantages in excluding malignant tumors and avoiding unnecessary removal[14]. But these approaches are still controversial, as the correct diagnosis is usually made only after nephrectomy[15]. Fortunately, with the widespread application of partial nephrectomy, the function of kidneys are saved gradually.
In addition to surgery, targeted therapy and chemotherapy are also important adjuvant therapies. Based on the importance of the ALK pathway in the progression of IMT, ALK-targeted inhibitors, such as crizotinib, which are mostly used in the treatment of patients with metastatic or unresectable ALK-positive IMT, are effective and even offer surgical opportunities for these patients[32]. However, tumor cells may acquire resistance during the treatment process, which may limit their efficacy[33]. Anti-inflammatory therapy, such as nonsteroidal anti-inflammatory drugs (NSAIDs), is reported to be effective in ALK-negative patients for whom ALK inhibition is not an option[34]. NSAIDs may shrink the tumor and possibly cure the disease, and thus could be used as a diagnostic treatment[34]. If antibiotics cure IMTs, an inflammatory origin may be suggested[35]. Corticosteroids are also a great treatment option, especially for young patients and bilateral renal-infiltrating IMT[36].
Radiotherapy is mainly used for the treatment of IMT in the head and neck; the use of radiotherapy for kidney IMT has not been reported. Studies have shown that high-dose fractional radiotherapy is effective and safe for nasopharynx and skull IMT[37]. Therefore, radiation therapy may be an option in cases where anti-inflammatory drugs, steroids, and surgery are ineffective in controlling kidney IMT. The patient in our case underwent surgery, no other follow-up treatments were performed, and the patient recovered well. Surprisingly, antibiotics were not effective in this case.
The outcome of kidney IMT is quite favorable. Recurrence or metastasis has not yet been discovered from the cases we reviewed, which is consistent with Kapusta's study with the longest follow-up period being 17 years[29]. However, IMT has been simultaneously detected in multiple tissues, but it was not clear whether they were primary tumors or whether one had metastasized from the other[7]. Worryingly, local recurrence and distant metastasis have been reported in IMT outside of the kidney. The risk factors for recurrence mainly include positive surgical margins, nuclear atypia, ganglion-like cells, DNA aneuploidy, and the abnormal expression of p53[38]. However, there is no consensus on the reliable predictors of the biological behavior of IMT. Although IMT is not a malignant tumor, it is reported to be associated with RCC, which might affect the management and prognosis of patients[10]. Therefore, close follow-up must be advocated in such cases.
Kidney IMT is an uncommon neoplasm with an unknown etiology and diverse clinical manifestations. Renal calculus is suspected to be one of the causes or drivers. Despite its rarity, awareness of its existence is essential to avoid misdiagnosis in the differential diagnosis of a renal mass. Surgery and adjuvant chemotherapy are the current mainstream treatments. Although most patients obtain satisfactory results, follow-up is still indispensable because of the potential for recurrence and metastasis.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Stavroulopoulos A S-Editor: Gong ZM L-Editor: Wang TQ E-Editor: Liu MY
| 1. | Attili SV, Chandra CR, Hemant DK, Bapsy PP, RamaRao C, Anupama G. Retroperitoneal inflammatory myofibroblastic tumor. World J Surg Oncol. 2005;3:66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Shetty SJ, Pereira T, Desai RS. Inflammatory myofibroblastic tumor of the oral cavity: A case report and literature review. J Cancer Res Ther. 2019;15:725-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Duan J, Wang Y. A case report of recurrent thyroid inflammatory myofibroblastic tumor and its metastasis in soft tissue. Medicine (Baltimore). 2017;96:e8485. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Na YS, Park SG. Inflammatory myofibroblastic tumor of the pleura with adjacent chest wall invasion and metastasis to the kidney: a case report. J Med Case Rep. 2018;12:253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Wang S, Chen L, Cao Z, Mao X, Zhang L, Wang B. Inflammatory myofibroblastic tumor of the lumbar spinal canal: A Case Report With Literature Review. Medicine (Baltimore). 2017;96:e6488. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Heerwagen ST, Jensen C, Bagi P, Rappeport ED. Renal inflammatory myofibroblastic tumor: a rare tumor indistinguishable from renal cell carcinoma—report of two cases. Acta Radiol. 2007;48:1143-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Dogan MS, Doganay S, Koc G, Gorkem SB, Unal E, Ozturk F, Coskun A. Inflammatory Myofibroblastic Tumor of the Kidney and Bilateral Lung Nodules in a Child Mimicking Wilms Tumor With Lung Metastases. J Pediatr Hematol Oncol. 2015;37:e390-e393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | You Y, Shao H, Bui K, Bui M, Klapman J, Cui Q, Coppola D. Epstein-Barr virus positive inflammatory pseudotumor of the liver: report of a challenging case and review of the literature. Ann Clin Lab Sci. 2014;44:489-498. [PubMed] |
| 9. | Li Z, Wang W, Wang Y, Zhai X, Tian Y, Fu Y, Zhou H. Inflammatory myofibroblastic tumor of the kidney with viral hepatitis B and trauma: A case report. Oncol Lett. 2013;6:1741-1743. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Gwynn ES, Clark PE. Inflammatory myofibroblastic tumor associated with renal cell carcinoma. Urology. 2005;66:880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Song D, Jiao W, Gao Z, Liu N, Zhang S, Zong Y, Fang Z, Fan Y. Inflammatory myofibroblastic tumor of urinary bladder with severe hematuria: A Case report and literature review. Medicine (Baltimore). 2019;98:e13987. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Li F, Guo H, Qiu H, Hou Y. Ureteral inflammatory myofibroblastic tumor: A case report and literature review. Medicine (Baltimore). 2018;97:e13177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Wang K, Zhou H, Lu Y, Lu Q, Zhang C, Zhou X, Xia S, Wang G. ALK-negative urachal inflammatory myofibroblastic tumor in an elderly female: A case report. Medicine (Baltimore). 2018;97:e13619. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Ho PH, Chen SY, Hsueh C, Lai MW, Chao HC, Chang PY. Inflammatory myofibroblastic tumor of renal pelvis presenting with prolonged fever and abdominal pain in children: report of 1 case and review of literature. J Pediatr Surg. 2005;40:e35-e37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Tazi K, Ehirchiou A, Karmouni T, Maazaz K, el Khadir K, Koutani A, Ibn Attiya AI, Hachimi M, Lakrissa A. [Inflammatory pseudotumors of the kidney: a case report]. Ann Urol (Paris). 2001;35:30-33. [PubMed] |
| 16. | Androulaki A, Papathomas TG, Liapis G, Papaconstantinou I, Gazouli M, Goutas N, Bramis K, Papalambros A, Lazaris AC, Papalambros E. Inflammatory pseudotumor associated with Mycobacterium tuberculosis infection. Int J Infect Dis. 2008;12:607-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Lee SH, Fang YC, Luo JP, Kuo HI, Chen HC. Inflammatory pseudotumour associated with chronic persistent Eikenella corrodens infection: a case report and brief review. J Clin Pathol. 2003;56:868-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Surabhi VR, Chua S, Patel RP, Takahashi N, Lalwani N, Prasad SR. Inflammatory Myofibroblastic Tumors: Current Update. Radiol Clin North Am. 2016;54:553-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 108] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 19. | Lovly CM, Gupta A, Lipson D, Otto G, Brennan T, Chung CT, Borinstein SC, Ross JS, Stephens PJ, Miller VA, Coffin CM. Inflammatory myofibroblastic tumors harbor multiple potentially actionable kinase fusions. Cancer Discov. 2014;4:889-895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 320] [Article Influence: 29.1] [Reference Citation Analysis (0)] |
| 20. | Coffin CM, Hornick JL, Fletcher CD. Inflammatory myofibroblastic tumor: comparison of clinicopathologic, histologic, and immunohistochemical features including ALK expression in atypical and aggressive cases. Am J Surg Pathol. 2007;31:509-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 627] [Cited by in RCA: 623] [Article Influence: 34.6] [Reference Citation Analysis (0)] |
| 21. | Sun Z, Wang H, Guo X, Jiang S, Jing C. Inflammatory myofibroblastic tumor of kidney together with ipsilateral perinephric and periureteric fibrosis: A case report and literature review. Medicine (Baltimore). 2017;96:e8807. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Ascenti G, Zimbaro G, Mazziotti S, Gaeta M, Lamberto S, Scribano E. Contrast-enhanced power Doppler US in the diagnosis of renal pseudotumors. Eur Radiol. 2001;11:2496-2499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Tarhan F, Gül AE, Karadayi N, Kuyumcuoğlu U. Inflammatory pseudotumor of the kidney: a case report. Int Urol Nephrol. 2004;36:137-140. [PubMed] |
| 24. | Babu P, Kalpana Kumari MK, Nagaraj HK, Mysorekar VV. Inflammatory pseudotumor of kidney masquerading as renal carcinoma. J Cancer Res Ther. 2015;11:668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Ishikawa T, Fujisawa M, Tamada H, Inoue T, Shimatani N. Inflammatory pseudotumor of the kidney. Int J Urol. 2004;11:337-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 26. | Nakamura Y, Urashima M, Nishihara R, Matsuura A, Bekku K, Iguchi H, Uesugi T, Saegusa M, Aramaki K. Inflammatory pseudotumor of the kidney with renal artery penetration. Radiat Med. 2007;25:541-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Dong A, Wang Y, Dong H, Gong J, Cheng C, Zuo C, Lu J. Inflammatory myofibroblastic tumor: FDG PET/CT findings with pathologic correlation. Clin Nucl Med. 2014;39:113-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 28. | Liang W. A Renal Inflammatory Myofibroblastic Tumor Similar to Cystic Renal Cell Carcinoma: One Case Report. Medicine (Baltimore). 2015;94:e1181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 29. | Kapusta LR, Weiss MA, Ramsay J, Lopez-Beltran A, Srigley JR. Inflammatory myofibroblastic tumors of the kidney: a clinicopathologic and immunohistochemical study of 12 cases. Am J Surg Pathol. 2003;27:658-666. [PubMed] |
| 30. | Navale P, Menon S, Bakshi G, Pruthy R, Desai S. Inflammatory myofibroblastic tumor of kidney with heterotopic bone formation: An unusual case mimicking a renal malignancy. Indian J Med Paediatr Oncol. 2013;34:320-322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | Li H, Shen Q, Xia Q, Shi S, Zhang R, Yu B, Ma H, Lu Z, Wang X, He Y, Zhou X, Rao Q. [Clinicopathologic features of extrapulmonary inflammatory myofibroblastic tumor]. Zhonghua Bing Li Xue Za Zhi. 2014;43:370-374. [PubMed] |
| 32. | Wu S, Xu R, Zhao H, Zhu X, Zhang L, Zhao X. Inflammatory myofibroblastic tumor of renal pelvis presenting with iterative hematuria and abdominal pain: A case report. Oncol Lett. 2015;10:3847-3849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 33. | Brivio E, Zwaan CM. ALK inhibition in two emblematic cases of pediatric inflammatory myofibroblastic tumor: Efficacy and side effects. Pediatr Blood Cancer. 2019;66:e27645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 34. | Chavez C, Hoffman MA. Complete remission of ALK-negative plasma cell granuloma (inflammatory myofibroblastic tumor) of the lung induced by celecoxib: A case report and review of the literature. Oncol Lett. 2013;5:1672-1676. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 35. | Sugimoto K, Hayashi T, Imanishi M, Kadowaki T, Kurita T. [A case of inflammatory pseudotumor of renal pelvis showing a complete response to antibiotics]. Hinyokika Kiyo. 2004;50:629-631. [PubMed] |
| 36. | Li JY, Yong TY, Coleman M, Astill D, Passaris G, Juneja R, Siddins M, Barbara JA. Bilateral renal inflammatory pseudotumour effectively treated with corticosteroid. Clin Exp Nephrol. 2010;14:190-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 37. | Gabel BC, Goolsby M, Hansen L, U HS. Inflammatory Myofibroblastic Tumor of the Left Sphenoid and Cavernous Sinus Successfully Treated with Partial Resection and High Dose Radiotherapy: Case Report and Review of the Literature. Cureus. 2015;7:e328. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 38. | Hussong JW, Brown M, Perkins SL, Dehner LP, Coffin CM. Comparison of DNA ploidy, histologic, and immunohistochemical findings with clinical outcome in inflammatory myofibroblastic tumors. Mod Pathol. 1999;12:279-286. [PubMed] |
| 39. | Khallouk A, Ahallal Y, Tazi MF, Elfatemi H, Tazi E, Elammari J, Elfassi MJ, Farih MH. Inflammatory pseudotumor of the kidney: a case report. J Med Case Rep. 2011;5:411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 40. | Taheri D, Soleimani N, Fesharakizadeh M, Dolatkhah S, Kabiri M, Gholipour A. Inflammatory myofibroblastic tumor: report of a rare case in kidney. Iran J Kidney Dis. 2014;8:333-335. [PubMed] |
| 41. | Selvan DR, Philip J, Manikandan R, Helliwell TR, Lamb GH, Desmond AD. Inflammatory pseudotumor of the Kidney. World J Surg Oncol. 2007;5:106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 42. | Leroy X, Copin MC, Graziana JP, Wacrenier A, Gosselin B. Inflammatory pseudotumor of the renal pelvis. A report of 2 cases with clinicopathologic and immunohistochemical study. Arch Pathol Lab Med. 2000;124:1209-1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 43. | Bektas S, Okulu E, Kayigil O, Ertoy Baydar D. Inflammatory myofibroblastic tumor of the perirenal soft tissue misdiagnosed as renal cell carcinoma. Pathol Res Pract. 2007;203:461-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 44. | Pothadiyil AJ, Bhat S, Paul F, Mampatta J, Srinivas M. Inflammatory Myofibroblastic Tumor of the Kidney: A Rare Renal Tumor. J Clin Diagn Res. 2016;10:ED17-ED18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 45. | Vujanić GM, Berry PJ, Frank JD. Inflammatory pseudotumor of the kidney with extensive metaplastic bone. Pediatr Pathol. 1992;12:557-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 46. | Epaulard O, Fabre M, Barnoud R, Pasquier B, Massot C. [Renal inflammatory pseudotumor manifesting as a prolonged fever]. Rev Med Interne. 2000;21:889-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 47. | Sugimoto T, Miwa S, Sugata T, Zen Y. [A case of inflammatory myofibroblastic tumor recognized in the retroperitoneum and the kidney]. Hinyokika Kiyo. 2008;54:5-7. [PubMed] |
| 48. | Ryu KH, Im CM, Kim MK, Kwon D, Park K, Ryu SB, Choi C. Inflammatory myofibroblastic tumor of the kidney misdiagnosed as renal cell carcinoma. J Korean Med Sci. 2010;25:330-332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 49. | Iida K, Hosokawa Y, Itami Y, Shinohara M, Hayashi Y, Fujimoto K. [Case of inflammatory pseudotumor occurring in the renal pelvis]. Hinyokika Kiyo. 2014;60:555-559. [PubMed] |
| 50. | Wang Y, Qi X, Xue P, Zhang C, Cai C, Tu C, Wang K. Inflammatory myofibroblastic tumors in the kidney and abdominal wall mimicking malignancy: A case report. Medicine (Baltimore). 2018;97:e11994. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 51. | Boo YJ, Kim J, Kim JH, Kim CS, Suh SO. Inflammatory myofibroblastic tumor of the kidney in a child: report of a case. Surg Today. 2006;36:710-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 52. | Petrescu A, Berdan G, Hulea I, Gaitanidis R, Ambert V, Jinga V, Popescu M, Andrei F, Niculescu L. Renal inflammatory myofibroblastic tumor - a new case report. Rom J Morphol Embryol. 2007;48:437-442. [PubMed] |
| 53. | Mukkamala A, Elliott RM, Fulton N, Gulani V, Ponsky LE, Autorino R. Inflammatory pseudotumor of kidney: a challenging diagnostic entity. Int Braz J Urol. 2018;44:196-198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 54. | Hori J, Komiyama M. A case of inflammatory myofibroblastic tumor of the kidney with cystic change. Jpn J Clin Oncol. 2009;39:410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 55. | Yoshida S, Watanabe T, Yoshinaga A, Ohno R, Ishii N, Terao T, Hayashi T, Yamada T. [Inflammatory myofibroblastic tumor of the renal pelvis]. Hinyokika Kiyo. 2006;52:31-33. [PubMed] |
| 56. | Bildirici K, Dönmez T, Gürlek E. Inflammatory pseudotumor of the kidney. Int Urol Nephrol. 2004;36:141-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 57. | Kobayashi TK, Ueda M, Nishino T, Kushima R, Kato K, Katsumori T. Inflammatory pseudotumor of the kidney: report of a case with fine needle aspiration cytology. Acta Cytol. 2000;44:478-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 58. | Lee NG, Alexander MP, Xu H, Wang DS. Renal Inflammatory Myofibroblastic Tumor: A Case Report and Comprehensive Review of Literature. World J Oncol. 2011;2:85-88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 59. | Iwaki H, Kajita Y, Shimizu Y, Yamauchi T. [Inflammatory pseudotumor of the kidney: report of a case]. Nihon Hinyokika Gakkai Zasshi. 2001;92:589-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 60. | Kim TJ, Kim SH. Radiologic findings of renal inflammatory pseudotumor: a case report. Korean J Radiol. 2000;1:219-222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 61. | Satoh E, Arai H, Gotoh T, Nishimura K, Honda M, Fujioka H, Tsujimoto M. [Renal inflammatory pseudotumor after embolization for arteriovenous malformation: a case report]. Hinyokika Kiyo. 2000;46:23-26. [PubMed] |
| 62. | Shah VB, Anchinmane VT, Savant D. Inflammatory myofibroblastic tumor of renal pelvis: a rare entity. Indian J Pathol Microbiol. 2011;54:856-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 63. | Bell ND, Gavras JN, Donnell CA, Rodning CB. Renal inflammatory pseudotumor. South Med J. 1998;91:1050-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 64. | Ma Y, Zieske AW, Fenves AZ. Bilateral infiltrating renal inflammatory pseudotumor responsive to corticosteroid therapy. Am J Kidney Dis. 2008;51:116-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 65. | Tambo M, Kondo H, Kitauchi T, Hirayama A, Cho M, Fujimoto K, Yoshida K, Ozono S, Hirao Y, Yamada E, Ichijima K. [A case of inflammatory myofibroblastic tumor of the retroperitoneum]. Hinyokika Kiyo. 2003;49:273-276. [PubMed] |
| 66. | Hattori S, Takagi K, Uno M, Nezasa S, Komeda H, Fujimoto Y. [Case report of inflammatory pseudotumor that occurred at the ureteropelvic junction]. Hinyokika Kiyo. 2008;54:737-740. [PubMed] |