Published online Nov 26, 2019. doi: 10.12998/wjcc.v7.i22.3792
Peer-review started: June 19, 2019
First decision: September 9, 2019
Revised: October 3, 2019
Accepted: October 15, 2019
Article in press: October 15, 2019
Published online: November 26, 2019
Processing time: 167 Days and 3.1 Hours
Sagliker syndrome (SS) resulting from uncontrolled secondary hyperparathyroidism (SHPT) in chronic renal failure (CRF) is seldom reported.
A 24-year-old woman presented with asymmetric facial deformity and stature shortening. She was diagnosed with SS, SHPT, CRF, and thyroid cancer. The patient underwent a total parathyroidectomy and thyroidectomy with central lymph node dissection. The patient’s condition was stable and was discharged from the hospital.
Undergoing dialysis vintage, presenting high serum phosphate levels, and female gender may be risk factors for SS. Intramembranous ossification in the craniomaxillofacial region is possibly activated in this special pathophysiological condition. What’s more, the choice of surgery mainly depends on the treatment goal and the experience of the individual surgeon.
Core tip: This article reports one case of Sagliker syndrome, a rare complication of secondary hyperparathyroidism, which is characterized by disfiguring facial deformity, resulting in a lion-like face. We review the whole process of diagnosis and treatment in order to bring inspiration to other patients. Related articles are reviewed, and we make reasonable speculation of its risk factors. We also creatively put forward the hypothesis of its manifestation mechanisms and discuss its treatment modalities.
- Citation: Yu Y, Zhu CF, Fu X, Xu H. Sagliker syndrome: A case report of a rare manifestation of uncontrolled secondary hyperparathyroidism in chronic renal failure. World J Clin Cases 2019; 7(22): 3792-3799
- URL: https://www.wjgnet.com/2307-8960/full/v7/i22/3792.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i22.3792
As early as 1864, Virchow described a patient with enlargement of the facial bones as having “leontiasis ossea”[1]. Over time, people realized that leontiasis ossea was not a disease itself but a fairly rare medical condition associated with Paget’s disease, fibrous dysplasia, and gigantism. In 1953, Cohen et al[2] first described the symptoms of secondary hyperparathyroidism (SHPT) in chronic renal failure (CRF) as uremic leontiasis ossea (ULO), which was characterized by disfiguring facial deformity due to progressive bony overgrowth in the craniomaxillofacial region, resulting in a lion-like face. This syndrome has also been associated with a large head or swollen face in other studies[3,4]. To inform and draw attention to this novel disease, Sagliker et al[5] named it Sagliker syndrome (SS) and defined it in detail. The prominent clinical symptoms of SS are remarkable maxilla and mandible protrusion, dental abnormalities, hyperplasia of the soft tissue inside the mouth, destruction of the nasal bones, a short stature, fingertip changes, and even severe psychological manifestations. In Turkey, the incidence of SS is approximately 0.5%[5] in patients receiving haemodialysis; no other country has reported SS incidence. Few cases have been reported, and there is no related research. This article reports one case and discusses the risk factors, manifestation mechanisms, and treatment modalities (Table 1). The relevant literature is reviewed in this article.
| Event | Date |
| Hospitalization | 2018-11-29 |
| Laboratory results | 2018-11-30 |
| Imaging examinations | 2018-11-30, 2018-12-04, 2018-12-10 |
| Surgery | 2018-12-13 |
| Pathologic report | 2018-12-13, 2018-12-24 |
| Discharge | 2019-01-02 |
| Follow-up | 2019-04-15 |
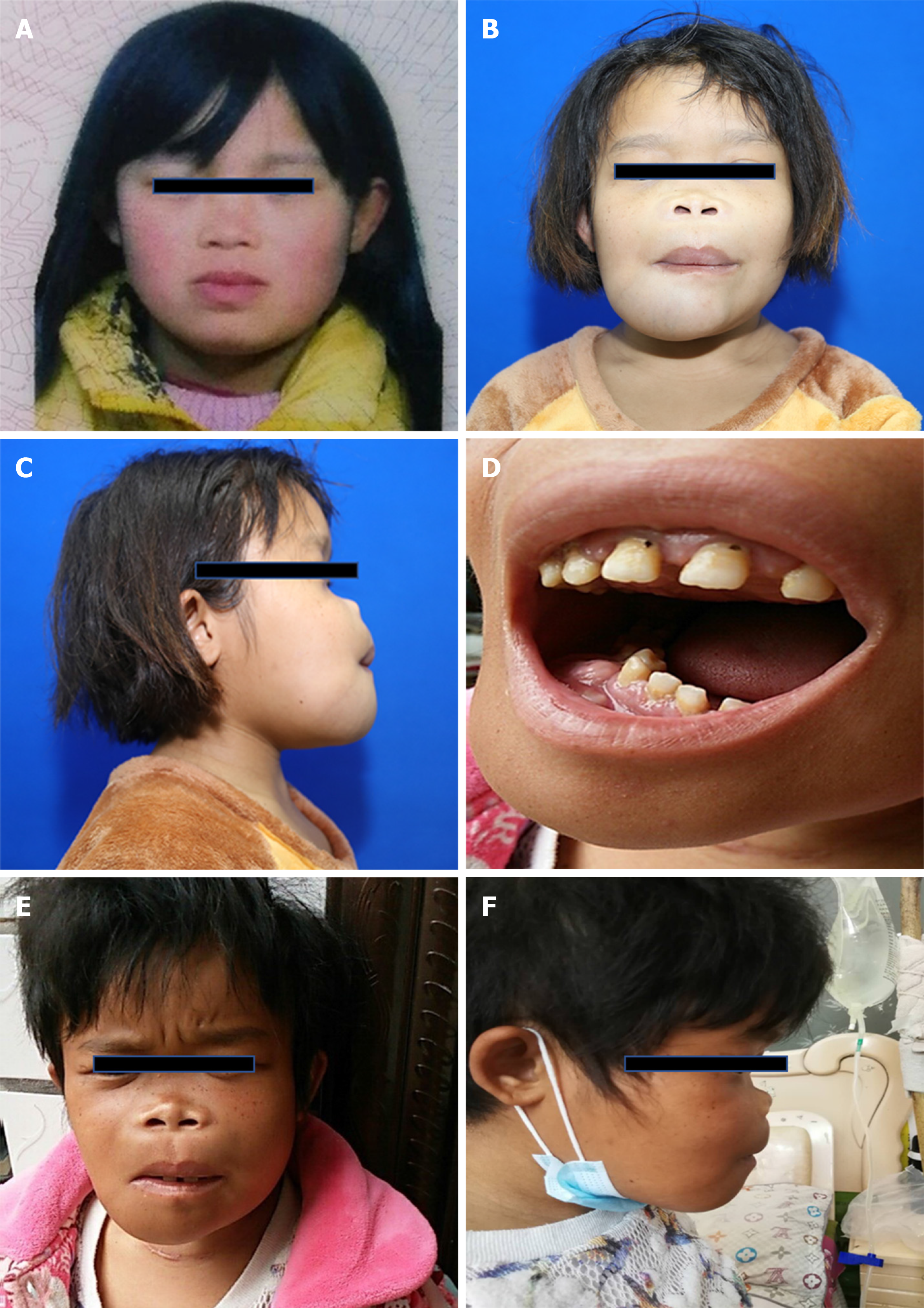
A 20-year-old woman went to local hospital due to nocturia, fatigue, and nausea. It was previously found that her creatinine level was about 600 mmol/L. Then, she was diagnosed with end-stage CRF and had undergone regular peritoneal dialysis since August 2014. Her aetiology of CRF was not clear. She regularly took calcium acetate tablets, vitamin D drops, recombinant human thrombopoietin injection, and calcitriol soft capsules during that time. However, her anemia was difficult to cure mainly because of malnutrition caused by anorexia. Ten months previously, she developed progressive facial deformity with difficultly chewing and swallowing and dyspnoea to some extent. Her facial deformity presented as asymmetric hyperplasia of the maxillary and maxillary bones, bimaxillary protrusion, nasal dorsum collapse, nostril valgus, and zygomatic collapse (Figure 1A-D). She also had a 10-cm shortening of height and severe leg pain when walking. She had no visual, hearing impairment or psychological problems.
The patient denied any history of past diseases.
The patient had no family history of CRF or hyperparathyroidism.
Serum parathyroid hormone (PTH) was 2815.07 pg/mL (normal range: 9.09-90.09 pg/mL), serum total calcium was 2.31 mmol/L (normal range: 2.25-2.75 mmol/L), serum phosphate was 2.08 mmol/L (normal range: 0.97-1.61 mmol/L), haemoglobin was 48 g/L (normal range: 120-160 g/L), and alkaline phosphatase was 2350 U/L (normal range: 50-135 U/L).
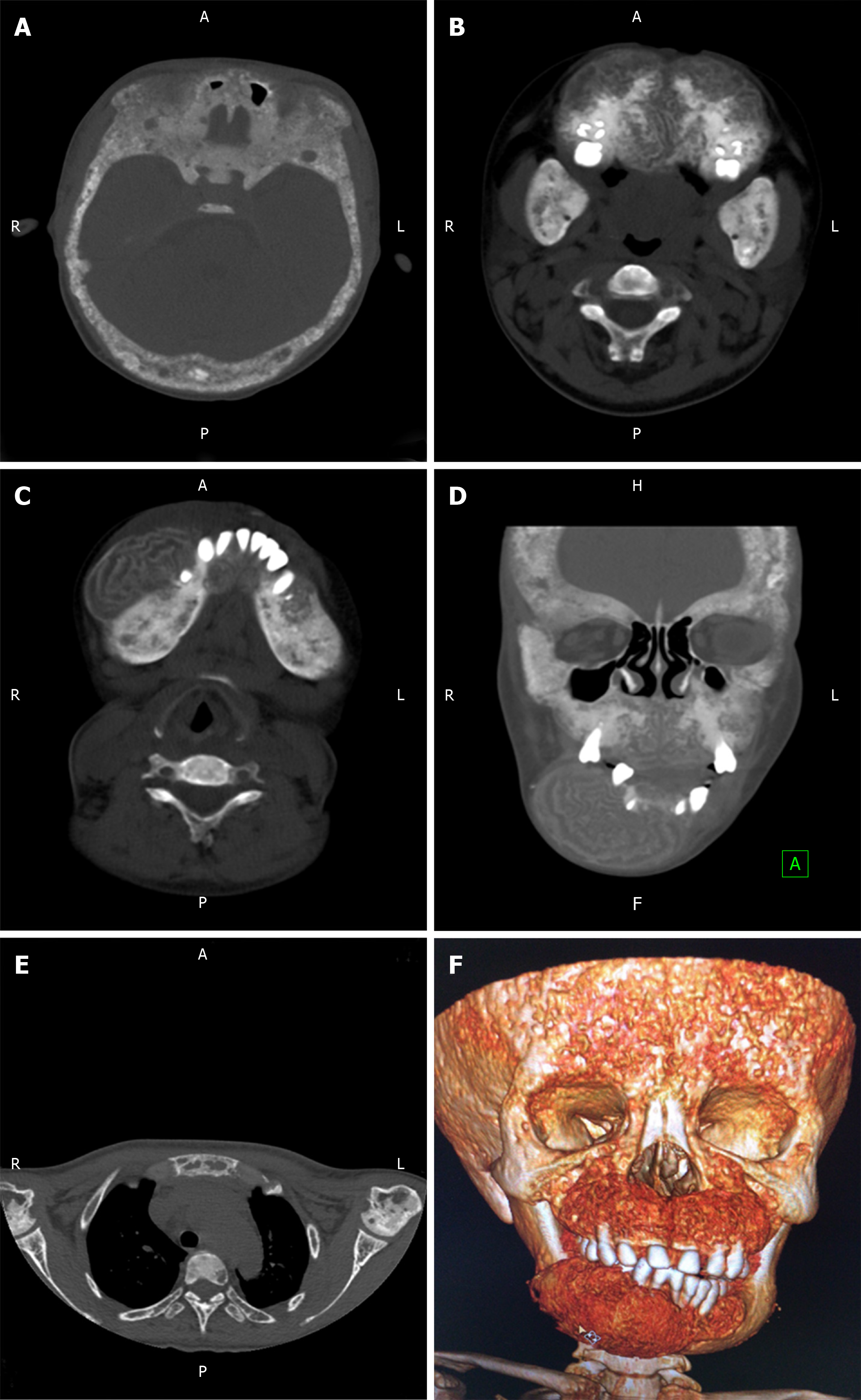
Non-contrast computed tomography (CT) scans showed thickening of the skull bone plates and diffuse mixed sclerotic and lytic changes in the mandible, maxilla, and calvaria. A distinct overgrowth of the maxillofacial bone indicated bone abnormalities and swelling, and the density of the bone marrow cavity was increased with a ground glass appearance (Figure 2). A neck CT scan showed a benign nodule on the right side of the thyroid with bilateral soft tissue signals behind the bilateral thyroid. A pelvic CT scan did not show any abnormal structures.
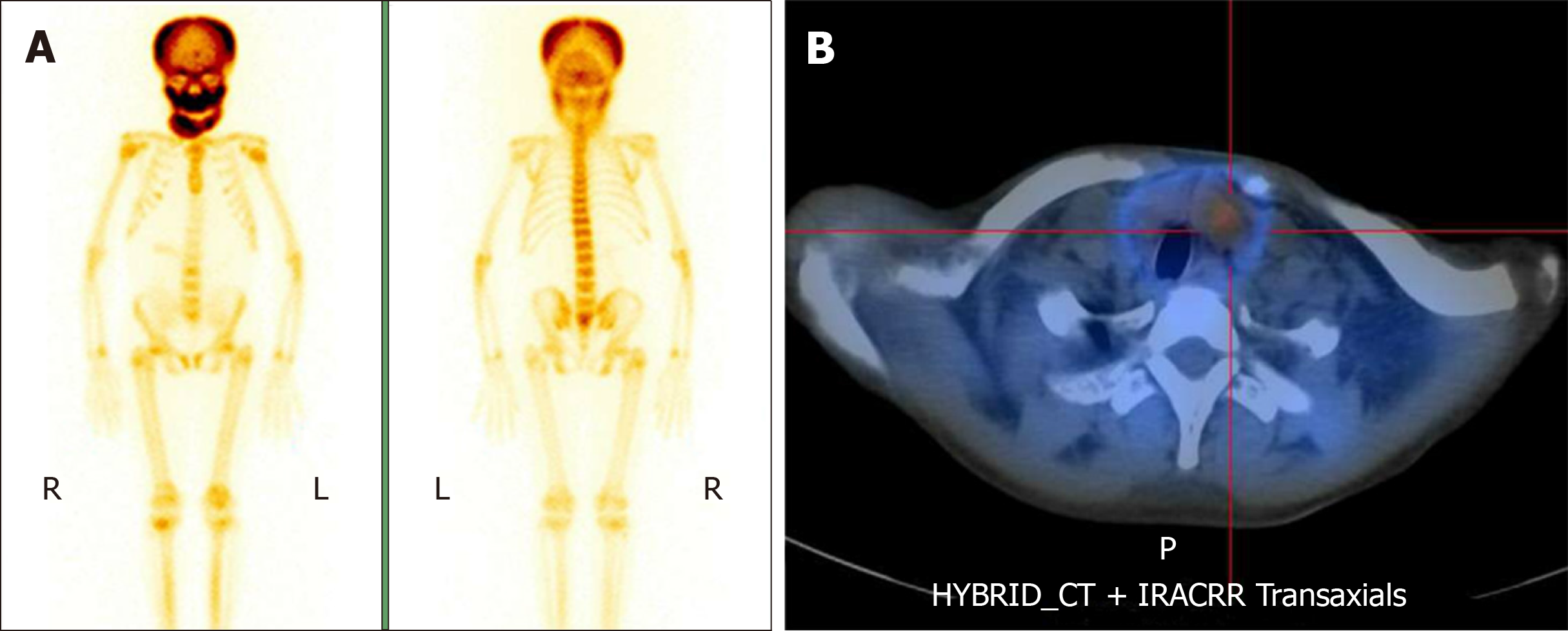
99mTc-methylene diphosphonate bone scintigraphy indicated increased radiotracer in the bilateral parietal, maxilla, and mandible. The signal on the right side of the mandible was the strongest (Figure 3A).
99mTc-sestamibi single-photon emission CT/CT showed only one hyperplastic parathyroid gland on the left side (Figure 3B). Ultrasound showed a 0.5 cm nodule on the left side of the thyroid [thyroid imaging reporting and data system (TI-RADS) 4A], a 1.0 cm nodule on the right side of the thyroid (TI-RADS 3), and one suspected parathyroid adenoma on the left side. Fine needle aspiration showed a left papillary thyroid carcinoma and right thyroid adenoma.
Considering all the information above, the patient was diagnosed with SS, SHPT, CRF, left papillary thyroid carcinoma, and right thyroid adenoma.
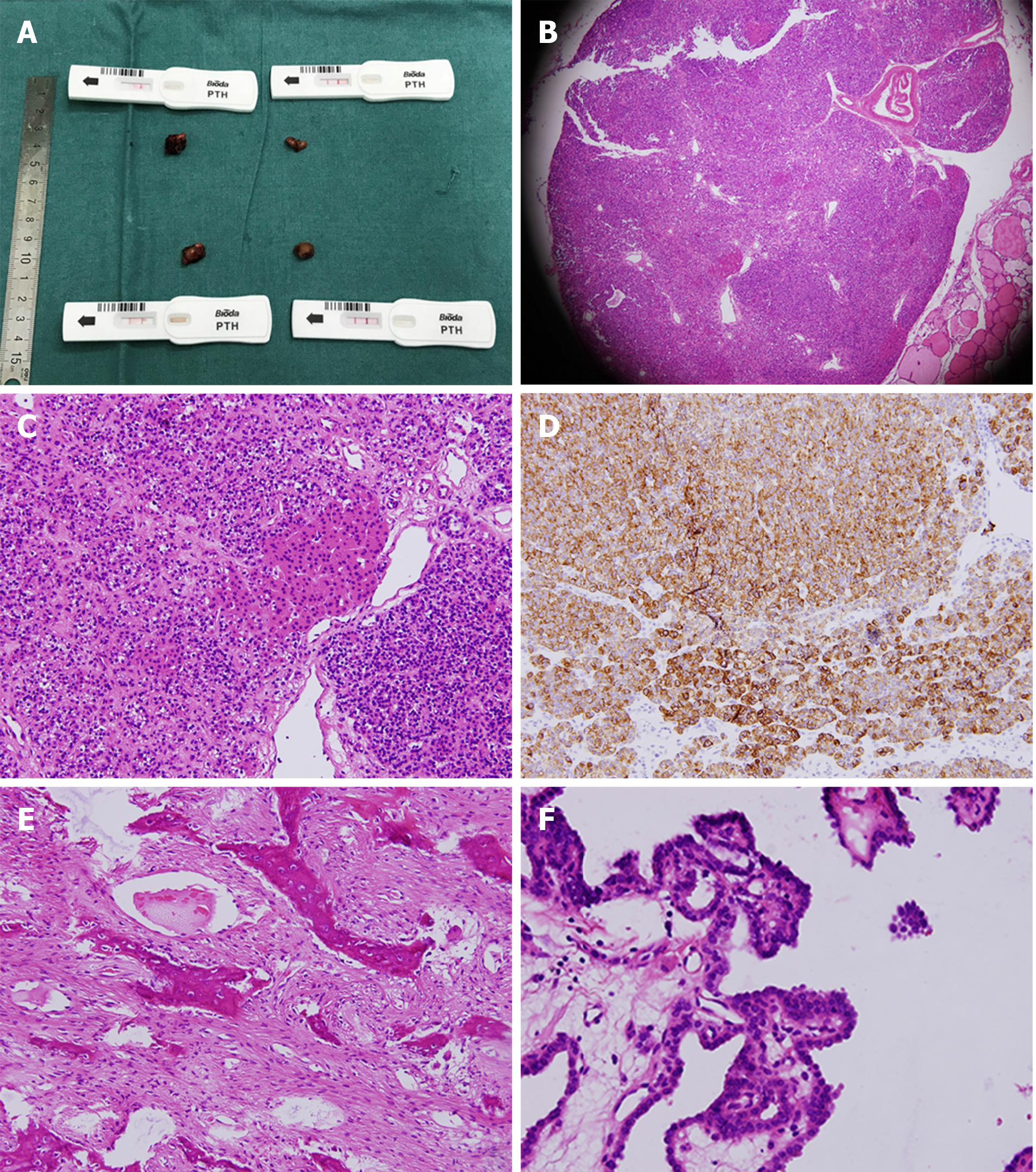
Due to the substantially high perioperative risk, the patient was advised to resume medical therapy. Her condition improved after three weeks. The patient underwent total parathyroidectomy and thyroidectomy with central lymph node dissection. Four parathyroid glands were confirmed by colloidal gold-based immunoassays during the operation. Paraffin pathology confirmed a 0.5 cm left thyroid papillary carcinoma, a 1.0 cm right thyroid adenoma, and four hyperplasia parathyroid glands due to SHPT. No lymph node metastases were observed in the VI region. Mandibular biopsy showed bone changes consistent with SHPT (Figure 4).
Because the serum level of PTH rapidly decreased after parathyroidectomy (Table 2), leading to a sudden drop in serum calcium, the goal was to maintain serum calcium levels within a safe range. The level of serum ionic calcium was instantly detected every two hours after the total parathyroidectomy. Intravenous calcium gluconate was administered to maintain a stable level of scrum ionic calcium (normal range: 1.12-1.32 mmol/L). Intravenous calcium gluconate was gradually replaced by oral calcium carbonate within a few days.
| Time | Content |
| Before operation | 2815 pg/mL |
| Postoperative day 1 | 41.1 pg/mL |
| Postoperative day 5 | 2.55 pg/mL |
| Discharge | 1.51 pg/mL |
| Postdischarge (4 mo later) | 131.01 pg/mL |
The patient was discharged from the hospital when her condition was stable. Four months later, her PTH was 131.01 pg/mL. We made a reasonable speculation that the function of ectopic parathyroid glands, which existed outside the thyroid region, was suppressed by the hyperparathyroidism before the surgery. When the inhibitory factor was removed, together with the stimulation of hypocalcemia, ectopic parathyroid glands began compensatory secretion. We intended to perform the examination of single-photon emission CT/CT, but unfortunately she participated in only online follow-up sessions for economic reasons. She reported a reduction in the protrusion of the maxilla and mandible after the total parathyroidectomy (Figure 1E and F).
It is well known that 40% of patients with CRF develop SHPT without appropriate treatment. Sagliker et al[5] reported 25 patients who developed cephalometric skull changes, maxillary and mandibular bone deformations, irregular and misshaped teeth, soft and tumoural tissues inside the oral cavity, a lion-like appearance, short stature, and fingertip changes. Uzel et al[6] and Giray et al[7] reported that SS might result in class II malocclusions or neurologic manifestations, such as headaches, fatigue, and polyneuropathy. Ozenli et al[8] confirmed that psychiatric morbidities were more severe and common in this population. Hearing loss and bilateral compressive optic neuropathy were also observed in some cases[9,10].
The aetiology of SS is still unclear. SS is regarded as a disastrous complication of uncontrolled SHPT, and it is plausible that the progression of SHPT is responsible for this syndrome[5]. Undergoing dialysis vintage, presenting high serum phosphate levels, and being female are risk factors for this disease[11,12]. Tunc et al[13] proposed that chromosome aberrations are associated with SS. Yildiz et al[14] reported genetic mutations in exons 1, 4, and 10 of the GNAS1 gene are related to SS and are also genetically predisposing factors.
The mechanism of craniofacial bone overgrowth is also unclear. According to the theory of skeletal development, the thickness of the maxilla, anterior mandible, and skull is mainly produced by intramembranous ossification[15]. We speculated that intramembranous ossification in the craniomaxillofacial region is activated in this special pathophysiological condition, which results in this typical craniomaxillofacial deformity.
The optimal surgery for SHPT is a debated topic in the literature. Three types of surgeries, including subtotal parathyroidectomy (sPtx), total parathyroidectomy with auto-transplantation (tPtx + AT), and total parathyroidectomy (tPtx), have been proposed. SPtx and tPtx + AT can retain part of the function of PTH and prevent fatal hypocalcaemia, but a high recurrence of SHPT is associated with these procedures[16-18]. TPtx can induce refractory hypoparathyroidism; however, some studies regard tPtx as a safe and effective procedure in patients with a low risk of renal transplantation[19-21]. All the above surgeries can improve the clinical symptoms, prevent the development of facial deformities, and stop height shortening. The choice of surgery mainly depends on the treatment goal and the experience of the individual surgeon. In this case, we chose tPtx to avoid more serious complications of progressive SHPT because of economic factors. Long-term follow-up is needed to evaluate the quality of life and monitor for recurrence in patients.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mrzljak A, Pedersen EB S-Editor: Wang JL L-Editor: Wang TQ E-Editor: Li X
| 1. | Evans J. Leontiasis ossea; a critical review, with reports of four original cases. J Bone Joint Surg Br. 1953;35-B:229-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Cohen J, Diamond I. Leontiasis ossea, slipped epiphyses, and granulosa cell tumor of testis with renal disease; report of a case with autopsy findings. AMA Arch Pathol. 1953;56:488-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Lee VS, Webb MS, Martinez S, McKay CP, Leight GS. Uremic leontiasis ossea: "bighead" disease in humans? Radiologic, clinical, and pathologic features. Radiology. 1996;199:233-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Fisher D, Hiller N, Drukker A. Nephroquiz for the beginner: A swollen face in a girl on haemodialysis. Diagnosis: renal osteodystrophy. Nephrol Dial Transplant. 1999;14:1797-1798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Sagliker Y, Balal M, Sagliker Ozkaynak P, Paydas S, Sagliker C, Sabit Sagliker H, Kiralp N, Mumin Adam S, Tuncer I, Gonlusen G, Esenturk M, Gocmez E, Taskapan H, Yeksan M, Kobaner E, Ozkaya O, Yuksekgonul M, Emir I, Cengiz N, Onder Isik I, Bilginer O, Guler T, Yakar H, Sarsmaz N, Dilaver S, Akoglu B, Basgumus M, Chirik E. Sagliker syndrome: uglifying human face appearance in late and severe secondary hyperparathyroidism in chronic renal failure. Semin Nephrol. 2004;24:449-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Uzel A, Uzel I, Sagliker Y, Yildiz I, Halvaci I, Paylar N, Ocal F, Balal M, Ozkaynak PS, Paydas S, Sagliker C, Sagliker HS, Kiralp N, Adam SM, Esenturk M, Gocmez E, Taskapan H, Yuksekgonul M, Emir I, Guler T, Yakar H, Sekin O, Kayali E, Caliskan S, Eskiocak AF, Ogruk B, Guzelyurt T, Kurt C. Cephalometric evaluation of patients with Sagliker syndrome: uglifying human face appearance in severe and late secondary hyperparathyroidism in chronic renal failure patients. J Ren Nutr. 2006;16:229-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Giray S, Sagliker Y, Yildiz I, Halvaci I, Paylar N, Ocal F, Balal M, Ozkaynak PS, Paydas S, Sagliker C, Sagliker HS, Kiralp N, Adam SM, Esenturk M, Gocmez E, Taskapan H, Yuksekgonul M, Emir I, Guler T, Yakar H, Sekin O, Kayali E, Caliskan S, Eskiocak AF, Ogruk B, Guzelyurt T, Kurt C. Neurologic manifestations in Sagliker syndrome: uglifying human face appearance in severe and late secondary hyperparathyroidism in chronic renal failure patients. J Ren Nutr. 2006;16:233-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Ozenli Y, Giray S, Sagliker Y, Adam SM. A controlled study of psychiatric manifestations and electroencephalography findings in chronic kidney disease patients with Sagliker syndrome. J Ren Nutr. 2010;20:S51-S55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Erkan AN, Sagliker Y, Yildiz I, Ozluoglu L. Audiological findings in chronic kidney disease patients with Sagliker syndrome. J Ren Nutr. 2010;20:S56-S58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Sundaram ANE, Abhayambika A, Kumar S. Bilateral Compressive Optic Neuropathy from Renal Osteodystrophy Caused by Branchio-oto-renal Syndrome Stabilised After Parathyroidectomy. Neuroophthalmology. 2017;41:321-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Chertow GM, Plone M, Dillon MA, Burke SK, Slatopolsky E. Hyperparathyroidism and dialysis vintage. Clin Nephrol. 2000;54:295-300. [PubMed] |
| 12. | Almaden Y, Felsenfeld AJ, Rodriguez M, Cañadillas S, Luque F, Bas A, Bravo J, Torregrosa V, Palma A, Ramos B, Sanchez C, Martin-Malo A, Canalejo A. Proliferation in hyperplastic human and normal rat parathyroid glands: role of phosphate, calcitriol, and gender. Kidney Int. 2003;64:2311-2317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Tunç E, Demirhan O, Sağliker Y, Yildiz İ, Paylar N, Güzel Aİ. Chromosomal findings and sequence analysis of target exons of calcium-sensingreceptor (CaSR) gene in patients with Sagliker syndrome. Turk J Med Sci. 2017;47:13-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Yildiz I, Sagliker Y, Demirhan O, Tunc E, Inandiklioglu N, Tasdemir D, Acharya V, Zhang L, Golea O, Sabry A, Ookalkar DS, Capusa C, Radulescu D, Garneata L, Mircescu G, Ben Maiz H, Chen CH, Prado Rome J, Benzegoutta M, Paylar N, Eyuboglu K, Karatepe E, Esenturk M, Yavascan O, Grzegorzevska A, Shilo V, Mazdeh MM, Francesco RC, Gouda Z, Adam SM, Emir I, Ocal F, Usta E, Kiralp N, Sagliker C, Ozkaynak PS, Sagliker HS, Bassuoni M, Sekin O. International evaluation of unrecognizably uglifying human faces in late and severe secondary hyperparathyroidism in chronic kidney disease. Sagliker syndrome. A unique catastrophic entity, cytogenetic studies for chromosomal abnormalities, calcium-sensing receptor gene and GNAS1 mutations. Striking and promising missense mutations on the GNAS1 gene exons 1, 4, 10, 4. J Ren Nutr. 2012;22:157-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Sadler TW. Langman’s medical embryology. 7th edition. Baltimore: Williams and Wilkins, 1995. . [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Hargrove GM, Pasieka JL, Hanley DA, Murphy MB. Short- and long-term outcome of total parathyroidectomy with immediate autografting versus subtotal parathyroidectomy in patients with end-stage renal disease. Am J Nephrol. 1999;19:559-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 37] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Gasparri G, Camandona M, Abbona GC, Papotti M, Jeantet A, Radice E, Mullineris B, Dei Poli M. Secondary and tertiary hyperparathyroidism: causes of recurrent disease after 446 parathyroidectomies. Ann Surg. 2001;233:65-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 114] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 18. | Naranda J, Ekart R, Pečovnik-Balon B. Total parathyroidectomy with forearm autotransplantation as the treatment of choice for secondary hyperparathyroidism. J Int Med Res. 2011;39:978-987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Madorin C, Owen RP, Fraser WD, Pellitteri PK, Radbill B, Rinaldo A, Seethala RR, Shaha AR, Silver CE, Suh MY, Weinstein B, Ferlito A. The surgical management of renal hyperparathyroidism. Eur Arch Otorhinolaryngol. 2012;269:1565-1576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | Sakman G, Parsak CK, Balal M, Seydaoglu G, Eray IC, Sarıtaş G, Demircan O. Outcomes of Total Parathyroidectomy with Autotransplantation versus Subtotal Parathyroidectomy with Routine Addition of Thymectomy to both Groups: Single Center Experience of Secondary Hyperparathyroidism. Balkan Med J. 2014;31:77-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Puccini M, Carpi A, Cupisti A, Caprioli R, Iacconi P, Barsotti M, Buccianti P, Mechanick J, Nicolini A, Miccoli P. Total parathyroidectomy without autotransplantation for the treatment of secondary hyperparathyroidism associated with chronic kidney disease: clinical and laboratory long-term follow-up. Biomed Pharmacother. 2010;64:359-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |