Published online Sep 26, 2019. doi: 10.12998/wjcc.v7.i18.2888
Peer-review started: May 9, 2019
First decision: May 30, 2019
Revised: July 12, 2019
Accepted: July 27, 2019
Article in press: July 27, 2019
Published online: September 26, 2019
Processing time: 151 Days and 23.6 Hours
Takayasu arteritis is a rare but intractable chronic disease in young female patients. Percutaneous transluminal angioplasty of the involved renal arteries has been reported; however, few studies have reported the use of drug coated balloon angioplasty in the treatment of Takayasu arteritis. We aimed to demonstrate five young female patients who presented with a history of hypertension due to Takayasu arteritis.
From April 2017 to October 2018, five female patients were diagnosed with hypertension due to Takayasu arteritis by computed tomography angiography (CTA) and laboratory tests. Four patients had a complaint of headache with or without dizziness, and one patient showed no symptom. There was no significant family or past history of hypertension or kidney disease, and the physical examinations were almost normal on admission. We performed a treatment by drug coated balloon angioplasty. Blood pressure decreased dramatically in all patients after balloon angioplasty, and the patency of treated renal artery was demonstrated with CTA over 5 months after the angioplasty procedure.
Drug coated balloon angioplasty is safe and effective for renal artery stenosis due to Takayasu arteritis. A prospective study with a larger sample size is necessary to further demonstrate the effectiveness of the treatment.
Core tip: Percutaneous transluminal angioplasty of the involved renal arteries has been reported; however, few cases were treated by drug coated balloon angioplasty. We aimed to demonstrate five young ladies who presented with a history of hypertension due to Takayasu arteritis. Our data indicated that drug coated balloon angioplasty is safe and effective for renal artery stenosis due to Takayasu arteritis.
- Citation: Bi YH, Ren JZ, Yi MF, Li JD, Han XW. Drug coated balloon angioplasty for renal artery stenosis due to Takayasu arteritis: Report of five cases. World J Clin Cases 2019; 7(18): 2888-2893
- URL: https://www.wjgnet.com/2307-8960/full/v7/i18/2888.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i18.2888
Takayasu arteritis is a rare but intractable chronic disease, with a significantly higher incidence in young female patients[1,2]. The disease course extends over many years and recurrences are frequent even after receiving corticosteroid treatment[2]. Takayasu arteritis shows an unclear disease cause involving inflammation of the aorta and aortic branches, coronary arteries, and pulmonary arteries[3]. The inflammatory process can result in stenosis/occlusion, aneurysm formation, or dilatation in the affected arteries, thus increasing the risk of cardiovascular morbidity and mortality[3]. Takayasu arteritis is a significant cause of hypertension in children and young patients. Early evaluation and diagnosis of this disease can improve the morbidity and mortality, and computed tomography angiography (CTA) is usually used for this purpose[4]. Percutaneous transluminal angioplasty (PTA) of the involved renal arteries has been reported[5]; however, few studies have reported the use of drug coated balloon angioplasty in the treatment of Takayasu arteritis. We herein present five cases of treatable hypertension, which were diagnosed with hypertension due to Takayasu arteritis. They underwent PTA with a drug coated balloon catheter; thereafter, their blood pressure became normal with decreased amount of antihypertensive drug treatment.
Five young female patients were admitted to our department because of hypertension from April 2017 to October 2018. Four patients had a complaint of headache with or without dizziness, and one patient showed no symptom.
There was no significant family or past history of hypertension or kidney disease. The physical examinations were almost normal.
Laboratory tests were revealed as follows: creatinine 27-75 mmol/L (normal range: 20-115 mmol/L). The glomerular filtration rate of the involved kidney was computed as 16.7-25.1 mL/min; glucose, liver function, C-reactive protein (0.78-4.20 mg/L), and erythrocyte sedimentation rate (3.8-43.0 mm/h) were in normal ranges.
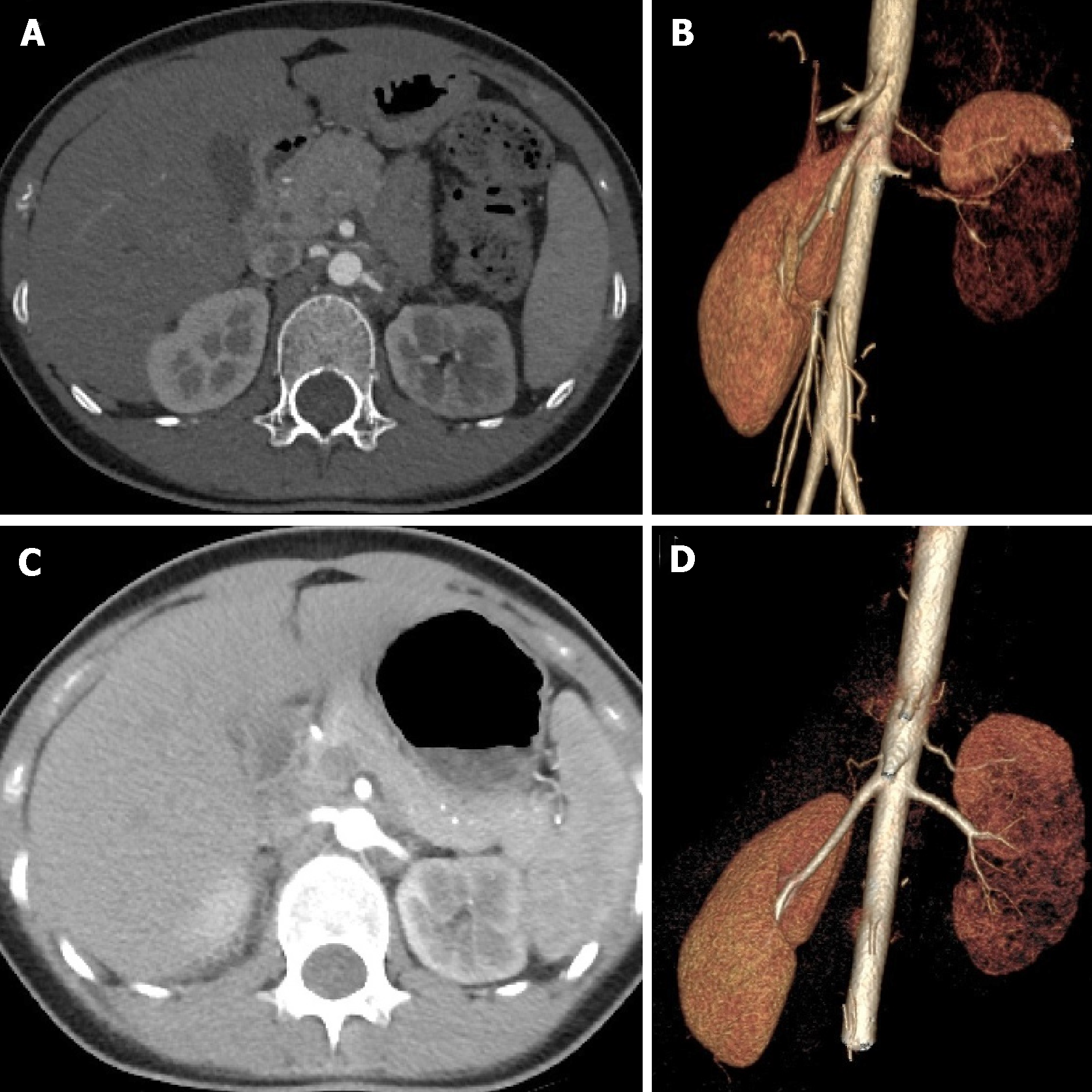
The chest computed tomography (CT) scan was normal. CTA of the aorta showed arterial wall thickening, renal arteries with severe stenosis at the origin in two cases, and renal arteries with occlusion in three cases (Figure 1A, Figure 1B).
All patients were diagnosed as having Takayasu arteritis.
Oral antihypertensives (1-3 kinds of drug) were administered in four patients before balloon dilation, and the patients’ blood pressure fluctuated between 146-176 mmHg for systolic blood pressure and 69-117 mmHg for diastolic blood pressure (Table 1).
| Patient No. | Age, (yr) | Gender | Blood pressure, mm Hg | No. of antihypertensive drugs | Serum creatinine, mg/dL | eGFR, mL/min/1.73 m2 | ESR, mm/h | CRP, mg/L | Diameter of involved artery, mm |
| 1 | 18 | F | 149/69 | 0 | 51 | 16.7 | 12.0 | 4.20 | Occlusive |
| 2 | 16 | F | 146/90 | 1 | 69 | 24.4 | 7.7 | 3.52 | Occlusive |
| 3 | 14 | F | 170/115 | 1 | 55 | 18.6 | 43.0 | 1.50 | Occlusive |
| 4 | 13 | F | 176/104 | 2 | 27 | 19.3 | 3.8 | 1.11 | 0.9 |
| 5 | 17 | F | 174/117 | 3 | 75 | 25.1 | 4.3 | 0.78 | 2.5 |
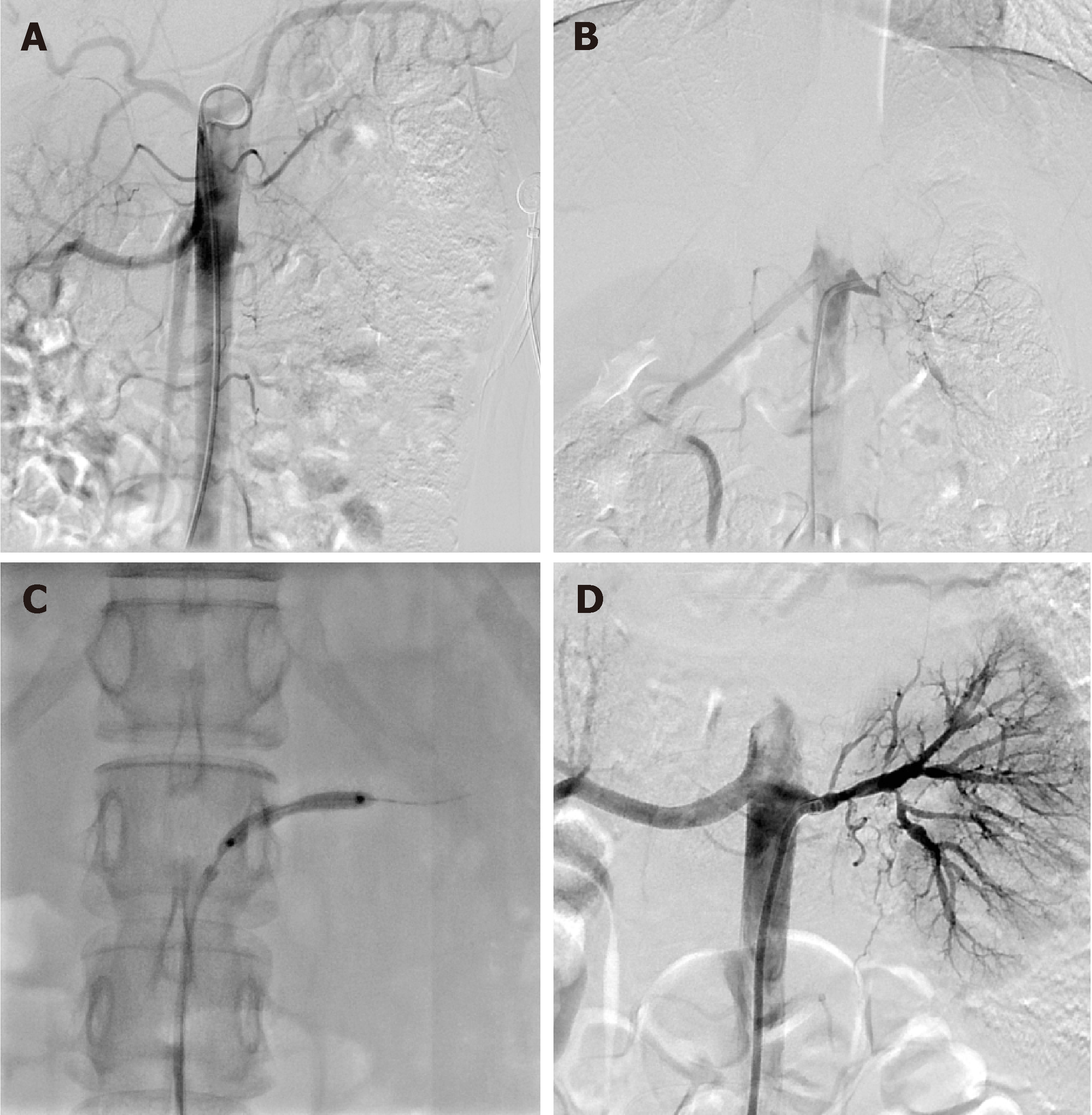
After the discussion among vascular and interventional specialists, we decided to perform PTA with a drug coated balloon catheter. PTA was performed on days 3-5 of hospitalization. A 7-F sheath was inserted into the femoral artery under local anesthesia. Nonselective angiography revealed severe stenosis of renal artery origin in two cases and occlusion of the proximal segment of renal arteries in three cases. A 7-F guiding catheter and 5-F Cobra catheter (Asahi Intec Co, Aichi, Japan) were introduced along a guide wire. The involved renal arteries were dilated with a 3.5-6 mm balloon catheter (Figure 2).
Repeated angiography revealed that the stenosis or occlusion at the involved renal artery origin was relieved obviously after angioplasty. Preoperative CTA showed a diameter of 0-2.5 mm of the renal artery, which increased to 3.0-7.0 mm after balloon dilatation.
In the postoperative reexamination, the erythrocyte sedimentation rate was 2.6-8.9 mm/h, the C-reactive protein was 0.18-0.70 mg/L (normal range: 0-5 mg/L), and serum creatinine was 24-67 mg/dL. The patients received cyclophosphamide pulse therapy during a 5-mo follow-up period after the procedure(Table 2). A follow-up performed 5.1-23.8 mo showed that the blood pressure fluctuated between 114-126 for systolic blood pressure and 65-80 mmHg for diastolic blood pressure. The amount of oral antihypertensives decreased obviously, and only two patients needed to take one kind of antihypertensive. The creatinine concentration was 24-67 mg/dL, and glomerular filtration rate was 35.29-101.98 mL/min. The uptake functions and blood perfusion of the kidneys were almost normal. CTA imaging showed an improvement of the stenosis at the involved renal arteries (Figure 1C, Figure 1D).
| Patient No. | Blood pressure, mm Hg | No. of antihypertensive drugs | Serum creatinine, mg/dL | eGFR, mL/min/1.73 m2 | ESR, mm/h | CRP, mg/L | Diameter of involved artery, mm | Follow-up, mo |
| 1 | 115/75 | 0 | 67 | 35.29 | 8.9 | 0.30 | 6.0 | 23.8 |
| 2 | 126/65 | 0 | 61 | 76.70 | 5.1 | 0.70 | 3.3 | 21.1 |
| 3 | 114/72 | 0 | 56 | 91.87 | 7.0 | 0.58 | 4.1 | 5.1 |
| 4 | 121/74 | 1 | 24 | 86.27 | 3.5 | 0.33 | 3.0 | 14.4 |
| 5 | 123/80 | 1 | 62 | 101.98 | 2.6 | 0.18 | 7.0 | 5.2 |
Takayasu arteritis was documented as aortoarteritis in 1830[4], and was named in honor of the professor who firstly reported this disease. Takayasu arteritis is a common disease in Japan, India, Southeast Asia, and Mexico[6]. Takayasu arteritis often show nonspecific clinical manifestations, such as fever, headache, dyspnea, anemia, joint and muscle pains, thoracic pain and so on. The severity classification of Takayasu arteritis is based on the outcomes of CTA[6-8]. Patients with Takayasu arteritis often show marked stenosis or occlusion of renal arteries.
PTA is a promising treatment for patients with Takayasu arteritis. Gumus et al[5] reported a case of Takayasu arteritis with stenosis of bilateral renal arteries that underwent a balloon angioplasty. Endovascular stent implantation can improve the prognosis for patients who experience restenosis after balloon angioplasty. However, few studies have reported the use of drug coated balloon angioplasty in the treatment of Takayasu arteritis. We successfully performed PTA with a drug coated balloon catheter in five young patients with Takayasu arteritis. The patient’s blood pressure decreased dramatically in all patients after balloon angioplasty, and patency of the involved renal artery was confirmed by CTA over a 5-mo period after angioplasty procedure. Our treatment protocol, like other studies[5], has achieved satisfactory results. However, owing to a short period of follow-up, long-term effects of this intervention treatment on patient’s blood pressure, glomerular filtration rate, or creatinine concentration could not be assessed, and further long-term follow-up is needed.
Identifying disease activity for Takayasu arteritis is quite challenging. CTA is a high-quality imaging tool for the diagnosis and grading of vascular disease[9]. Quantitative characterization is useful for identifying disease activity, and relative enhancement ratio and maximal wall thickness have a high sensitivity and specificity for detecting its activity[2]. Besides, Razek et al[10] reported that time resolved imaging of contrast kinetics MR angiography is useful for evaluation and treatment planning of arteriovenous malformations. The merits of MR angiography are needed to investigate for Takayasu arteritis.
Our results indicated that drug coated balloon angioplasty is safe and effective for renal artery stenosis due to Takayasu arteritis. A prospective study with a larger sample size is necessary to further demonstrate the effectiveness of the treatment.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: El-Razek AA, Gheita TA, Shrestha B S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Zhou BX
| 1. | Watanabe Y, Miyata T, Tanemoto K. Current Clinical Features of New Patients With Takayasu Arteritis Observed From Cross-Country Research in Japan: Age and Sex Specificity. Circulation. 2015;132:1701-1709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 160] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 2. | Chen B, Wang X, Yin W, Gao Y, Hou Z, An Y, Li Z, Ren X, Zhao S, Das P, Lu B. Assessment of disease activity in Takayasu arteritis: A quantitative study with computed tomography angiography. Int J Cardiol. 2019;289:144-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | He Y, Lv N, Dang A, Cheng N. Pulmonary Artery Involvement in Patients with Takayasu Arteritis. J Rheumatol. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 4. | Numano F, Okawara M, Inomata H, Kobayashi Y. Takayasu's arteritis. Lancet. 2000;356:1023-1025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 201] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 5. | Gumus B, Cevik H, Vuran C, Omay O, Kocyigit OI, Turkoz R. Cutting balloon angioplasty of bilateral renal artery stenosis due to Takayasu arteritis in a 5-year-old child with midterm follow-up. Cardiovasc Intervent Radiol. 2010;33:394-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Johnston SL, Lock RJ, Gompels MM. Takayasu arteritis: a review. J Clin Pathol. 2002;55:481-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 455] [Cited by in RCA: 433] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 7. | Smetana GW, Shmerling RH. Does this patient have temporal arteritis? JAMA. 2002;287:92-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 217] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 8. | McCulloch M, Andronikou S, Goddard E, Sinclair P, Lawrenson J, Mandelstam S, Beningfield SJ, Millar AJ. Angiographic features of 26 children with Takayasu's arteritis. Pediatr Radiol. 2003;33:230-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 54] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Abdel Razek AA, Denewer AT, Hegazy MA, Hafez MT. Role of computed tomography angiography in the diagnosis of vascular stenosis in head and neck microvascular free flap reconstruction. Int J Oral Maxillofac Surg. 2014;43:811-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Razek AA, Gaballa G, Megahed AS, Elmogy E. Time resolved imaging of contrast kinetics (TRICKS) MR angiography of arteriovenous malformations of head and neck. Eur J Radiol. 2013;82:1885-1891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 80] [Article Influence: 6.7] [Reference Citation Analysis (0)] |