Published online Aug 26, 2019. doi: 10.12998/wjcc.v7.i16.2360
Peer-review started: May 10, 2019
First decision: June 12, 2019
Revised: June 19, 2019
Accepted: July 20, 2019
Article in press: July 20, 2019
Published online: August 26, 2019
Processing time: 109 Days and 12.8 Hours
Severe total colonic necrosis, septic shock and venous thromboembolism secondary to ulcerative colitis (UC) are rare and life-threatening. No such severe complications have been reported in the literature.
We report a 36-year-old woman who developed total colonic necrosis and septic shock secondary to UC. The patient was treated with emergency surgery because computed tomography showed suspicious perforations. Persistent massive ascites occurred after operation and computed tomography angiography demonstrated portal vein, mesenteric vein and splenic vein thrombosis. The patient was discharged from hospital after active treatment.
Clinicians should pay attention to venous thrombosis, colonic necrosis and septic shock in UC patients. Close observation of surgical indications and timely surgical intervention are the key to reduce mortality and complications in UC.
Core tip: Severe total colonic necrosis, septic shock and venous thromboembolism are rare but life-threatening complications of ulcerative colitis. Possibility of colonic necrosis in ulcerative colitis should be considered and close observation of surgical indications and timely surgical intervention are the key to reduce mortality and complications in ulcerative colitis.
- Citation: Zhu MY, Sun LQ. Ulcerative colitis complicated with colonic necrosis, septic shock and venous thromboembolism: A case report. World J Clin Cases 2019; 7(16): 2360-2366
- URL: https://www.wjgnet.com/2307-8960/full/v7/i16/2360.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i16.2360
Ulcerative colitis (UC) is a chronic inflammatory disease, is easy to relapse, and prognosis is poor once there are complications[1]. Patients with UC have mucosal inflammation, which may extend continuously to the entire colon[2]. Total colonic necrosis, a complication in UC, is rarely reported and can be life threating. We present a patient with UC who developed total colonic necrosis, septic shock and venous thromboembolism (VTE) accompanied by acute kidney injury (AKI). The patient was successfully treated with emergency surgery and support therapies. This case suggests that occurrence of colonic necrosis in UC should be noticed, and timely colectomy should be performed to prevent critical complications.
A 36-year-old female was admitted to our hospital with abdominal pain, diarrhea, mucus blood, pus and recurrent tenesmus attacks.
Her condition was improved with fecal microbiota transplantation. Nine days later, she complained of anuria, vomiting and diarrhea, which were more severe than before.
The patient was diagnosed with UC ten years previously. She was maintained on mesalazine and prednisone but without comprehensive treatment.
About 100 mL dark colored urine was drained, and bloody fluid was discharged from the urethral catheter. She appeared dyspneic with cold clammy limbs, increased pulse rate, abdominal cavity pressure of 25 mmHg and grade IV abdominal hypertension[3].
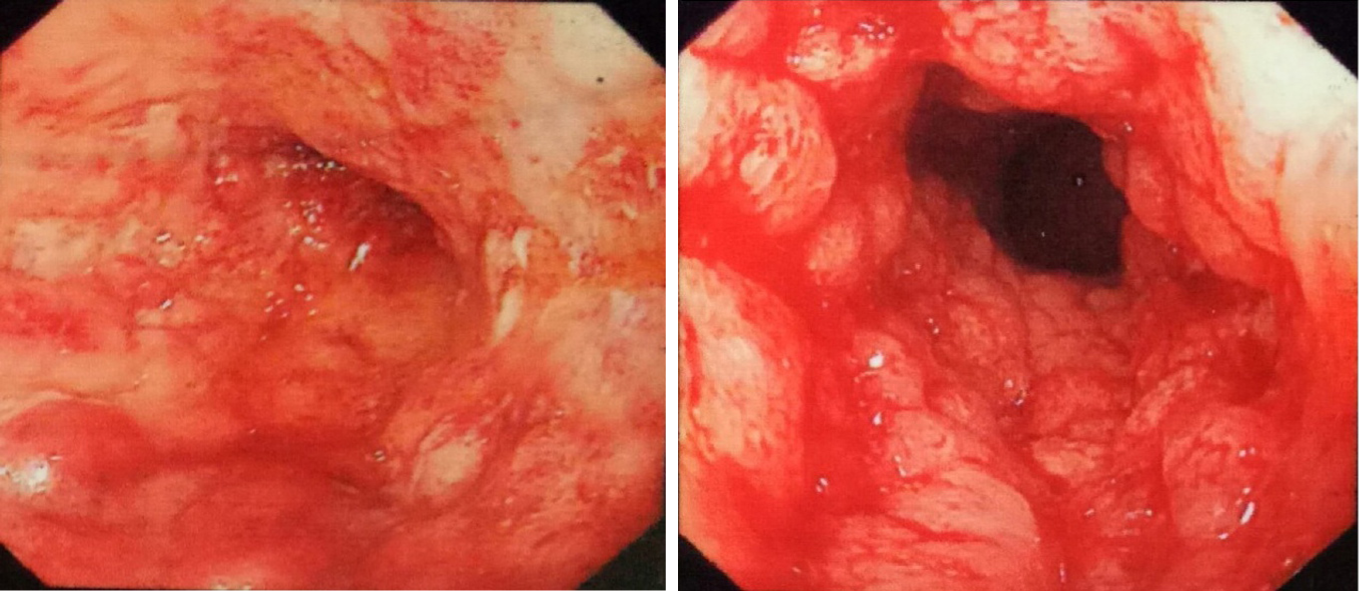
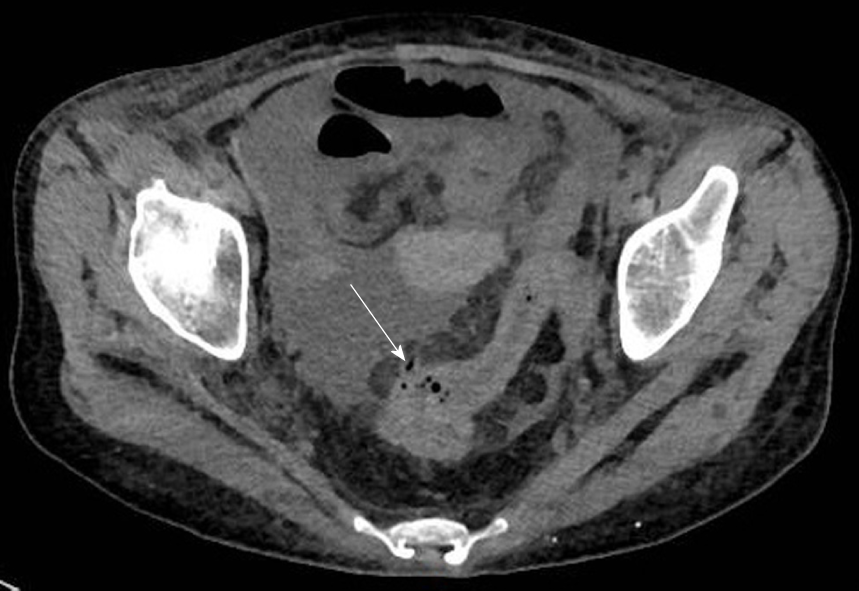
The endoscopy demonstrated total colonic wall thickening, erosions in luminal surface of colon, hyperemia, friability, bleeding and ulcerations (Figure 1). Laboratory tests revealed white blood count of 40.77 × 109/L, red blood count of 2.41 × 1012/L, hemoglobin of 60 G/L and sequential organ failure assessment scores of 10 (Table 1). Emergent computed tomography showed suspicious thin perforations at rectosigmoid colon and massive ascites (Figure 2).
| System | Assessment | Index | Score |
| Respiratory | PaO2/FiO2 (mmHg) | 382 (153/0.4) | 1 |
| Coagulation | Platelets×109/L | 53 | 2 |
| Liver | Bilirubin (mg/dL) | 25.9 | 1 |
| Cardiovascular | Mean arterial pressure | 70 mmHg | 0 |
| Central nervous system | Glasgow coma scale score | 15 | 0 |
| Renal | Creatinine, mg/dL; Urine output, mL/d | 215.2; 100 | 2 4 |
| Total score | 10 |
Septic shock, colonic perforation, UC, acute renal failure, disseminated intravascular coagulation and severe anemia.
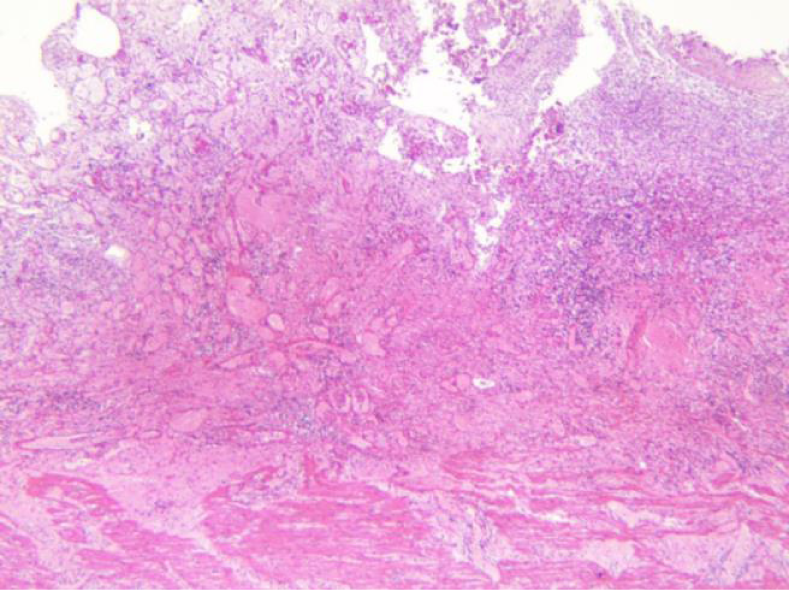
She underwent urgent total proctocolectomy and ileostomy. During surgery, massive ascites, total colonic necrosis, edema and dilatation of small intestine were observed (Figure 3) but with no obvious perforation and arterial thrombosis. The ascites culture was negative. Histopathological examination of the resected colon showed mucosal inflammation, necrosis and hemorrhage (Figure 4). After etiological treatment, the patient was transferred to the intensive care unit. Her symptoms were alleviated, and urine excretion was normal with maintenance of renal perfusion. Ascites fluid of 1880-3880 mL was drained daily for 7 d in the intensive care unit. The possibility of thrombosis was considered. Following anticoagulant therapy, the volume of ascites was reduced gradually. The condition of the patient gradually improved after active treatment. Computed tomography angiography displayed thrombosis in the trunk of portal vein and its intrahepatic branches, the superior mesenteric vein and the splenic vein (Figure 5). The patient recovered and was discharged from the hospital after antibacterial, anticoagulant and nutritional support treatment.
UC affects the colon and most commonly afflicting young adults aged 30-40 years[4]. UC complicated with total colonic necrosis has not been reported, and the mortality rate of septic shock secondary to colon necrosis is extremely high. Such severe UC is potentially a life-threatening condition that requires attention and early recognition[5]. The present patient had a long course of UC involving the whole colon. Fecal microbiota transplantation through the jejunum tube does not damage the colon. Related factors for colon necrosis in this patient included non-occlusive mesenteric ischemia, shock and long-term inflammation. Immediate surgical intervention for refractory UC could improve outcomes[6]. Restorative proctocolectomy with ileal pouch-anal anastomosis is the most commonly performed surgery for UC.
Sepsis is defined as life-threatening organ dysfunction caused by an overwhelming immune response to infection[7]. Septic shock is associated with a greater risk of mortality than sepsis alone[8]. Sepsis with a sequential organ failure assessment score of ≥ 2 in a patient with suspected infection indicates a risk of death[9]. The sequential organ failure assessment score of our patient was 10 and was highly associated with serious infection. Total colonic necrosis is the etiology of sepsis. Tissue hypoperfusion accompanied by septic shock, if persistent may lead to organ dysfunction and failure[10]. The cases of AKI account for more than 50% in sepsis[11]. Septic AKI is diagnosed with an increase in serum creatinine or a decrease in urinary output[12]. The patient developed anuria after abdominal pain, which is a sign of renal dysfunction. The compression of the renal artery by abdominal hypertension is also one of the causes of AKI. In this case, the renal function recovered, making computed tomography angiography imaging possible. Source control measures are important in the treatment of abdominal sepsis[13]. Removal of total colonic necrosis helps alleviate septic shock and lower the abdominal pressure. Volume resuscitation, vasopressor and antimicrobial therapy are the main treatments for septic shock[14]. Manifestations of sepsis depends on the infection, the organ dysfunction, the underlying health condition of the patient and the aggressive treatment used[15]. Septic shock in this patient was caused by abdominal infection and characterized by coagulation disorders and AKI rather than circulatory and respiratory dysfunctions.
The risk of VTE in patients with UC is 3-4 times higher than that in the normal population with an overall incidence up to 7%[16], especially in those with a long-term use of prednisone. VTE is associated with disease activity in UC[17]. Portal vein thrombosis and mesenteric venous thrombosis in our patient were severe complications associated with UC and surgery. The prevalence of portal vein thrombosis in the general population is about 1%[18]. A large amount of ascites before, during and after surgery was considered to be associated with portal vein thrombosis, but angiography could not be performed in these patients because of AKI. Patients with mesenteric venous thrombosis can present with acute abdominal pain, but most of them have vague clinical presentation, which makes it difficult to be diagnosed in time[19]. VTE is often a critical condition and anti-coagulate therapy should be given as soon as the diagnosis is made[20]. It is important to prevent VTE during hospitalization.
Early computed tomography angiography is necessary in patients with severe UC. Total colonic necrosis is a rare complication in UC. If medical therapy fails, close observation of surgical indications and timely colectomy should be performed to prevent critical complications.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lambrecht NW S-Editor: Cui LJ L-Editor: Filipodia E-Editor: Liu JH
| 1. | Yamada Y, Sugimoto K, Yoshizawa Y, Arai Y, Otsuki Y, Arai T, Kobayashi Y, Sato Y, Hosoda Y. Mesenteric inflammatory veno-occlusive disease occurring during the course of ulcerative colitis: a case report. BMC Gastroenterol. 2018;18:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF. Ulcerative colitis. Lancet. 2017;389:1756-1770. [PubMed] |
| 3. | Kirkpatrick AW, Roberts DJ, De Waele J, Jaeschke R, Malbrain ML, De Keulenaer B, Duchesne J, Bjorck M, Leppaniemi A, Ejike JC, Sugrue M, Cheatham M, Ivatury R, Ball CG, Reintam Blaser A, Regli A, Balogh ZJ, D'Amours S, Debergh D, Kaplan M, Kimball E, Olvera C; Pediatric Guidelines Sub-Committee for the World Society of the Abdominal Compartment Syndrome. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013;39:1190-1206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 841] [Cited by in RCA: 850] [Article Influence: 70.8] [Reference Citation Analysis (2)] |
| 4. | Adams SM, Bornemann PH. Ulcerative colitis. Am Fam Physician. 2013;87:699-705. [PubMed] |
| 5. | Hindryckx P, Jairath V, D'Haens G. Acute severe ulcerative colitis: from pathophysiology to clinical management. Nat Rev Gastroenterol Hepatol. 2016;13:654-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 125] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 6. | Leeds IL, Truta B, Parian AM, Chen SY, Efron JE, Gearhart SL, Safar B, Fang SH. Early Surgical Intervention for Acute Ulcerative Colitis Is Associated with Improved Postoperative Outcomes. J Gastrointest Surg. 2017;21:1675-1682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Simpson N, Lamontagne F, Shankar-Hari M. Septic shock resuscitation in the first hour. Curr Opin Crit Care. 2017;23:561-566. [PubMed] |
| 8. | Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15803] [Cited by in RCA: 17016] [Article Influence: 1890.7] [Reference Citation Analysis (2)] |
| 9. | Fernando SM, Rochwerg B, Seely AJE. Clinical implications of the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). CMAJ. 2018;190:E1058-E1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 88] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 10. | Yuki K, Murakami N. Sepsis pathophysiology and anesthetic consideration. Cardiovasc Hematol Disord Drug Targets. 2015;15:57-69. [PubMed] |
| 11. | Ma S, Evans RG, Iguchi N, Tare M, Parkington HC, Bellomo R, May CN, Lankadeva YR. Sepsis-induced acute kidney injury: A disease of the microcirculation. Microcirculation. 2019;26:e12483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 129] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 12. | Lameire N, Kellum JA; KDIGO AKI Guideline Work Group. Contrast-induced acute kidney injury and renal support for acute kidney injury: a KDIGO summary (Part 2). Crit Care. 2013;17:205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 108] [Cited by in RCA: 138] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 13. | Leppaniemi A, Kimball E J, De Laet I, Malbrain M L, Balogh Z J, De Waele J J. Management of abdominal sepsis--a paradigm shift? Anaesthesiol Intensive Ther. 2015;47:400-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Leppäniemi A, Kimball EJ, De Laet I, Malbrain ML, Balogh ZJ, De Waele JJ. Management of abdominal sepsis--a paradigm shift? Anaesthesiol Intensive Ther. 2015;47:400-408. [PubMed] |
| 15. | Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369:840-851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2315] [Cited by in RCA: 2548] [Article Influence: 212.3] [Reference Citation Analysis (0)] |
| 16. | Higgins PD, Skup M, Mulani PM, Lin J, Chao J. Increased risk of venous thromboembolic events with corticosteroid vs biologic therapy for inflammatory bowel disease. Clin Gastroenterol Hepatol. 2015;13:316-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 78] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 17. | Harbord M, Annese V, Vavricka SR, Allez M, Barreiro-de Acosta M, Boberg KM, Burisch J, De Vos M, De Vries AM, Dick AD, Juillerat P, Karlsen TH, Koutroubakis I, Lakatos PL, Orchard T, Papay P, Raine T, Reinshagen M, Thaci D, Tilg H, Carbonnel F; European Crohn’s and Colitis Organisation. The First European Evidence-based Consensus on Extra-intestinal Manifestations in Inflammatory Bowel Disease. J Crohns Colitis. 2016;10:239-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 619] [Cited by in RCA: 544] [Article Influence: 60.4] [Reference Citation Analysis (0)] |
| 18. | Basit SA, Stone CD, Gish R. Portal vein thrombosis. Clin Liver Dis. 2015;19:199-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 19. | Blumberg SN, Maldonado TS. Mesenteric venous thrombosis. Clin Liver Dis. 2016;4:501-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Van Assche G, Dignass A, Bokemeyer B, Danese S, Gionchetti P, Moser G, Beaugerie L, Gomollón F, Häuser W, Herrlinger K, Oldenburg B, Panes J, Portela F, Rogler G, Stein J, Tilg H, Travis S, Lindsay JO; European Crohn's and Colitis Organisation. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 3: special situations. J Crohns Colitis. 2013;7:1-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 381] [Cited by in RCA: 339] [Article Influence: 28.3] [Reference Citation Analysis (0)] |