Published online Jul 26, 2019. doi: 10.12998/wjcc.v7.i14.1865
Peer-review started: March 11, 2019
First decision: May 13, 2019
Revised: May 13, 2019
Accepted: June 26, 2019
Article in press: June 27, 2019
Published online: July 26, 2019
Processing time: 142 Days and 2.5 Hours
Colorectal neuroendocrine carcinoma (NEC) is a rare tumor that demonstrates aggressive growth pattern with ingrowth into the tract, metastasis to the other organs, and invasion to the surrounding organs; these clinical characteristics result in poor prognosis. Surgical resection appears as an effective approach; however, because it is difficult to accurately diagnose NEC during the early stage and owing to its aggressive growth pattern, development of a reliable standard chemotherapy regimen and management strategies are essential.
Here, we report the case of patient with NEC showing an aggressive growth pattern that resulted in the rupture of the tumor to the outside the colon after stenting of the internal colonic stenosis. In addition, the tumor invaded into the duodenum, thereby causing duodenal stenosis that required an additional stent in the duodenum. This aggressive growth pattern is one of the main features of the NEC that is different from adenocarcinoma. To clarify the clinical characteristics, we reviewed 60 recently reported cases, including data on tumor location, size, treatment, and prognosis.
We consider that the information presented here is of great significance for the diagnosis, treatment, and management of symptoms of the patients with NEC.
Core tip: The aggressive growth pattern of the rare tumor colorectal neuroendocrine carcinoma (NEC) results in the rapid growth into the tract, metastasis to the other organs, and invasion to the surrounding organs. The overall prognosis has been poor compared with invasive colon adenocarcinoma. The aggressive growth pattern of this tumor could result in the colonic stenosis, tumor rupture outside the colon, and invasion to the surrounding organs. Because of its rarity and poor prognosis, clinical information has not been yet summarized; we have summarized the information obtained from 60 cases reported to date. The information summarized in the present study would be of great importance to assist physicians for the diagnosis, treatment, and management of the symptoms of patients with NEC.
- Citation: Yoshida T, Kamimura K, Hosaka K, Doumori K, Oka H, Sato A, Fukuhara Y, Watanabe S, Sato T, Yoshikawa A, Tomidokoro T, Terai S. Colorectal neuroendocrine carcinoma: A case report and review of the literature. World J Clin Cases 2019; 7(14): 1865-1875
- URL: https://www.wjgnet.com/2307-8960/full/v7/i14/1865.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i14.1865
Neuroendocrine carcinoma (NEC) of colon and rectum is a rare neuroendocrine tumor (NET) type that accounts for < 1% of all colorectal malignancies[1]. The clinical progression of NECs includes highly aggressive growth and rapid dissemination along with a high tendency for metastasis[2]. Moreover, these tumors could be detected at advanced stage[3]. The 3-year overall survival (OS) was estimated to be 5%–27%[1,4,5], and response to chemotherapy was reported as the only predictive factor in patients with metastasis[1]. Because of its aggressive nature and high recurrence rate of the NEC, adjuvant chemotherapy constitutes a critical part of the treatment and significantly improves survival[4]. Although platinum-based regimens are widely used as first-line chemotherapy for the treatment of patients with advanced NEC, no standard regimen has yet been established. A previous study has reported that some cases who received chemotherapy showed the complete response (CR) or partial response (PR) to the advanced NEC; however, more than half of patients showed progressive response[6].
Additionally, some NEC cases showed aggressive progression and outward growth with the invasion of surrounding tissues. These aggressive tumors lead to serious health issues such as colonic obstruction and internal organ exclusion. The manage-ment of such health issues is sometimes challenging; moreover, an appropriate therapeutic strategy has not yet been proposed because of rareness of the aggressive NEC.
Here, we attempted to present a patient with NEC that showed aggressive tumor progression. Although the patient received various therapeutic options, such as chemotherapy or intestinal self-expandable metallic stent, all those treatments have been unsuccessful yet.
A 55-year-old man was admitted to our hospital with a huge abdominal mass. He complained of palpable abdominal mass, while painless mass two months prior to the presentation.
He had no significant history of past illness.
Physical examination showed a palpable tumor and a relatively soft mass associating with poor movability in the right upper quadrant.
Laboratory findings showed an elevated white blood cell count (9740 /µL), platelet count (37.3 × 104 /µL), C-reactive protein (4.99 mg/dL), lactate dehydrogenase (328 IU/L), and hemoglobin level (9.4 g/dL). Carcinoembryonic antigen showed mild elevation of 9.5 ng/mL, while other tumor markers were in normal range (Table 1).
| WBC | 9740 /μL |
| RBC | 344 × 104 /μL |
| Hb | 9.4 g/dL |
| Ht | 29.1% |
| Plt | 37.3 ×104 /μL |
| TP | 6.7 g/dL |
| Alb | 3.8 g/dL |
| BUN | 12.3 mg/dL |
| Cre | 0.85 mg/dL |
| AST | 12 IU/L |
| ALT | 9.0 IU/L |
| LDH | 328 IU/L |
| ALP | 166 IU/L |
| γ-GTP | 43 IU/L |
| T-bil | 0.4 mg/dL |
| CRP | 5.0 mg/dL |
| CEA | 7.4 ng/mL |
| CA19-9 | 1.0 U/mL |
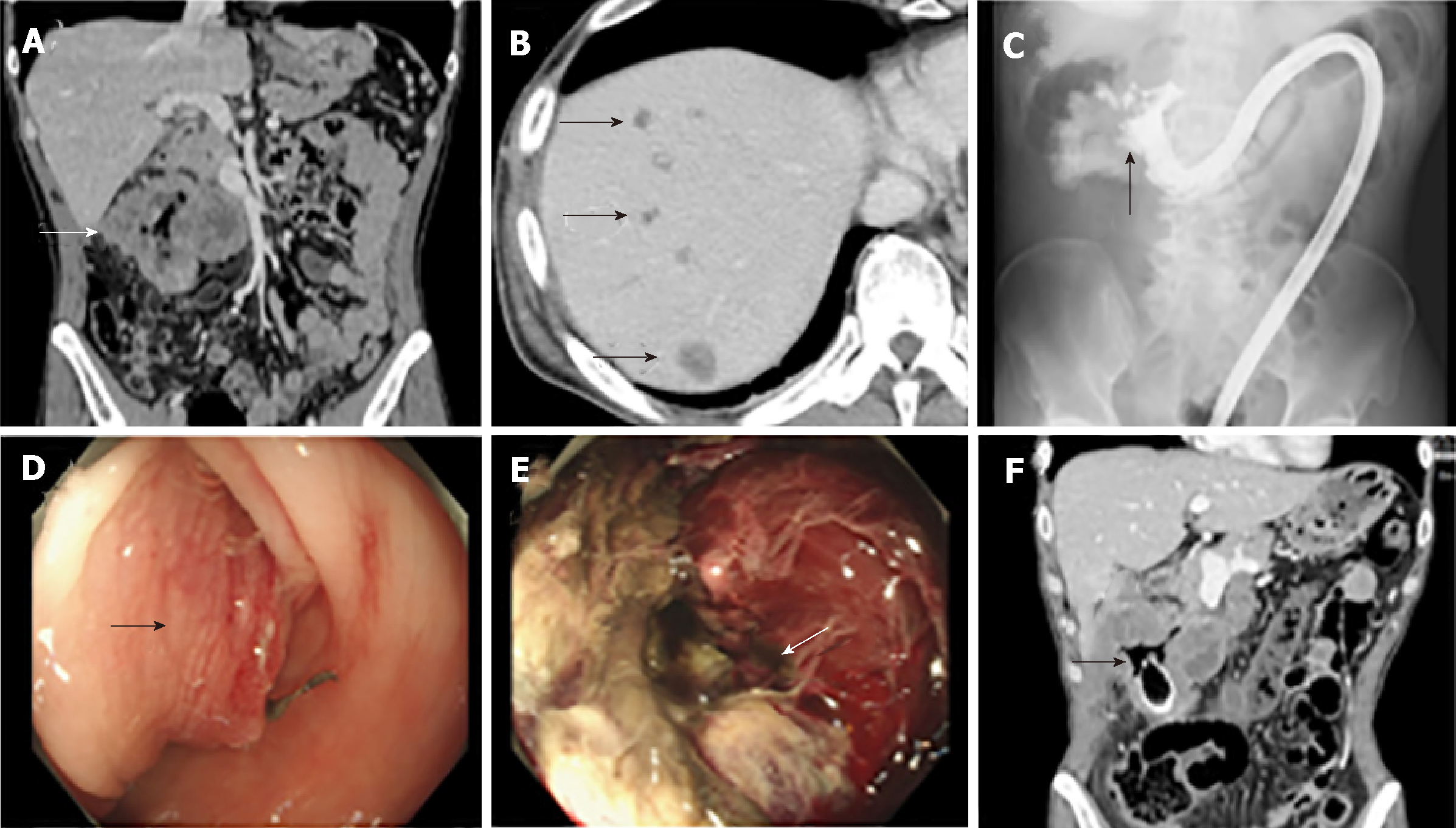
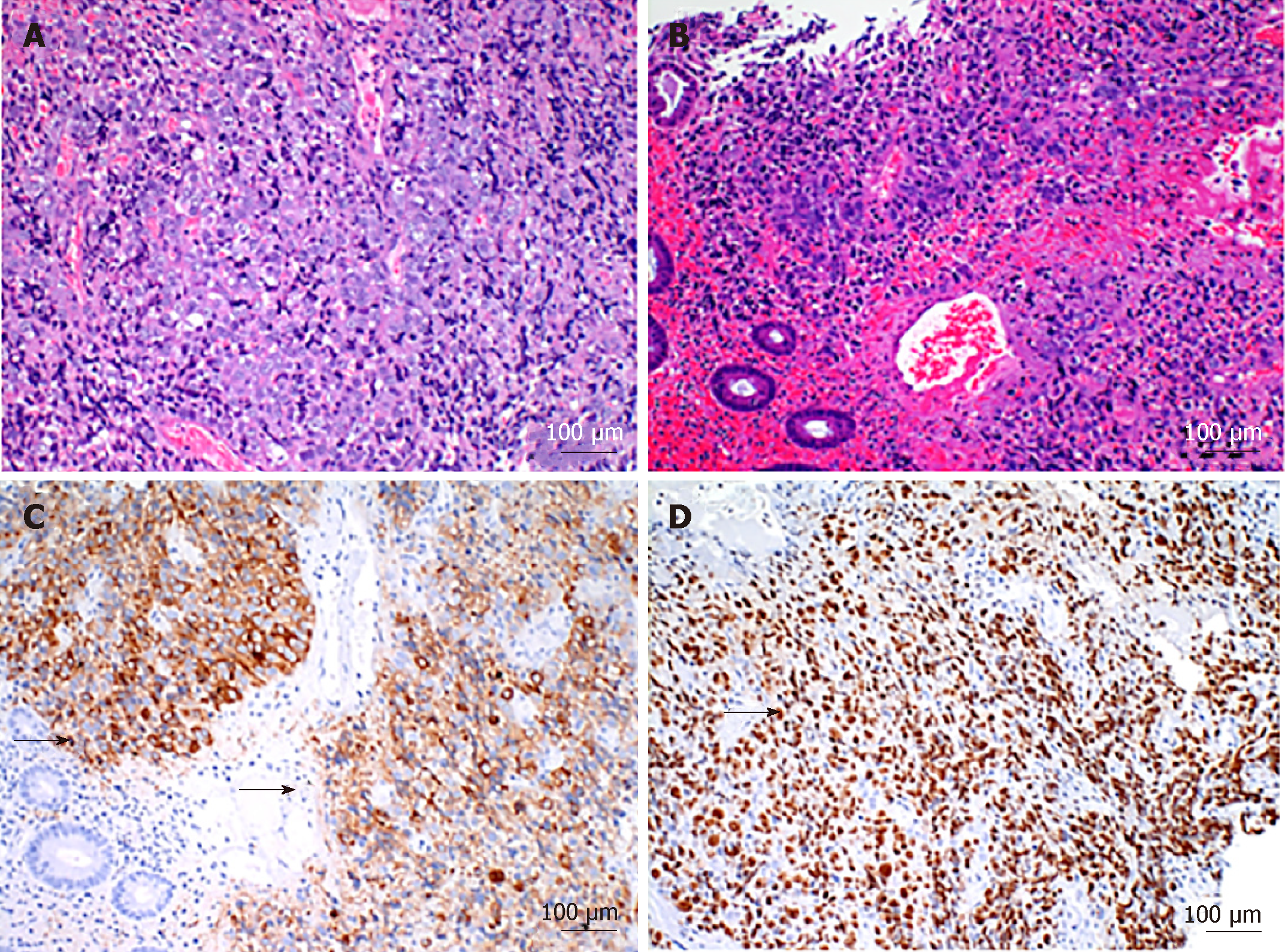
Abdominal contrast-enhanced computed tomography (CT) showed an irregularly shaped, 10 cm, as well as an enhanced mass in the transverse colon at the hepatic flexure (Figure 1A) and suspicious of metastatic tumors in the liver (Figure 1B). Colonoscopy showed the mass in the right transverse colon with significant stenosis (Figure 1C) due to submucosal elevation of the tumor (Figure 1D), while the lumen had a necrotic tissue (Figure 1E) evidenced by colonic enema with water-soluble contrast medium showing an irregular shape in the lumen of colon (Figure 1B). Following the mucosal biopsy for the histological analysis, a self-expandable metallic stent was successfully placed. However, the patient re-admitted to our hospital because of the sudden onset and severe abdominal pain at 5 days after the placement. The contrast-enhanced CT of the abdomen showed intraperitoneal free-air associated with the colon tumor (Figure 1F). The hematoxylin and eosin (HE) staining showed that the tumor cells were poorly differentiated (Figure 2A) with hemorrhage in the tumor (Figure 2B) and significantly stained positively for Synaptophysin (Figure 2C). In addition, Ki67 staining showed a highly proliferative pattern with the Ki67 index of 90% (Figure 2D).
Based on these findings, the tumor was diagnosed with NEC, and the tumor showed perforation to the outside the colon probably due to the expandable growth of the tumor.
The tumor showed severe invasion to the surrounding tissues; therefore, it was considered to be curatively unresectable, and anastomosis between the ileum and left colon was surgically developed that followed by chemotherapy.
Although the patient was treated with multiple chemotherapies, such as irinotecan + cisplatin (as the first-line therapy) and etoposide + carboplatin (as the second-line therapy); however, the tumor showed no significant response, and disease was rapidly progressed due to this invasive growth, in which the tumor induced the bile duct and duodenal obstruction by tumor progression. An additional stent for the duodenal stenosis was also placed; however, the appetite and general condition did not recover and he died 4 mo after the diagnosis.
The World Health Organization classification, published in 2010, divides NETs of the digestive tracts into NET grade (G) 1, NET G2, and NECs, based on mitotic counts and the Ki-67 proliferation index, regardless of tumor size, extent, or location, and also the colorectal NEC is a rare tumor with the incidence rate of 0.1%[1]. In addition, NEC and colorectal mixed adenoneuroendocrine carcinoma (MANEC) revealed high-grade cancer cells evidenced by high level of Ki-67 index (> 20%). The advanced NEC typically associates with the expansive growth pattern similar to that associates with the stage II colon cancer, i.e., yellowish ulcer and raised margin of non-neoplastic mucosa like submucosal tumor[5]. Colorectal NEC involves high malignant potential with poor differentiation and high invasiveness, while its prognosis is worse than colorectal adenocarcinoma. The median survival rate and relative survival (%) at 5 years of NEC and adenocarcinoma were 7.1–14.7 and 36.0 mo, and 8.0%–16.3% and 50.2%, respectively. In addition, MANEC showed significantly poor OS compared with adenocarcinoma[3]. Because of the aggressive progression, NEC was mainly detected at advanced stage in comparison with adenocarcinoma resulted in the fact that 57.9%–67.5% of NEC patients were initially diagnosed with the stage IV compared with the finding that 25.2% of cases with adenocarcinoma were diagnosed with stage IV[1,3,6]. These findings suggest that neuroendocrine differentiation is the cause of higher malignant potential and worse prognosis. Table 2 presents the characteristics of 59 cases with advances NEC and MANEC, while the terms “colon” and “neuroendocrine carcinoma” were searched in PubMed, and the available clinical information was summarized.
| No. | Ref. | Year | Age | Gen-der | Diagn-osis | Loca-tion | Size (mm x mm) | Posit-ive for Ki-67 (%) | Steno-sis (%) | Symp-tom of Obstruc-tion | Inva-sion to Surroun-ding Tissu-e | Metas-tasis | Sur-gery | CT | RT | Chemo-thera-py | Re-sponse to Chemo-thera-py | Over-all Sur-vival (mo) |
| 1 | 12 | 1996 | 65 | F | ECC | A | 150 | N/A | 100 | + | - | + | - | + | - | P | PD | 3 |
| 2 | 13 | 1998 | 70 | M | ECC | R | 80x55 | N/A | 60 | - | - | + | + | + | - | P | PD | 15 |
| 3 | 14 | 1999 | 54 | F | MAENC | S | 60 | N/A | N/A | - | + | + | + | + | - | F | N/A | N/A |
| 4 | 14 | 1999 | 46 | M | NEC | R | 160x130x40 | N/A | 100 | - | - | + | + | + | - | P | PD | 8 |
| 5 | 15 | 2002 | 50 | F | small cell carcinoma | R | 45x55 | N/A | 50 | - | - | + | + | + | - | P | CR | 54, alive |
| 6 | 16 | 2002 | 76 | M | MANEC | C | 45x45x15 | N/A | N/A | - | N/A | + | + | + | - | N/A | N/A | N/A |
| 7 | 17 | 2002 | 67 | F | small cell carcinoma | A | N/A | N/A | N/A | - | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 8 | 18 | 2003 | 61 | F | ECC | R | N/A | N/A | 60 | - | + | + | + | + | - | P | PD | 5 |
| 9 | 19 | 2004 | 78 | M | ECC | R | 47x43 | N/A | 60 | - | - | + | + | + | - | P | PD | 6 |
| 10 | 20 | 2004 | 38 | M | NEC | T | 100 | N/A | 100 | + | + | - | + | + | - | P | PR | 14 |
| 11 | 21 | 2004 | 79 | M | MANEC | R | 30x20 | N/A | 30 | - | - | + | + | + | + | F | PR | 21, alive |
| 12 | 22 | 2006 | 34 | M | ECC | T | 170x110 | N/A | 100 | - | + | + | + | + | - | P | PD | 8 |
| 13 | 23 | 2006 | 48 | M | ECC | R | 120x100 | N/A | 50 | - | + | + | + | + | + | P | SD | 24, alive |
| 14 | 24 | 2006 | 62 | M | NEC | A | 45x25 | N/A | 60 | - | + | + | + | + | - | F | PD | 11 |
| 15 | 25 | 2006 | 71 | M | NEC | D | 40x50 | N/A | 50 | - | - | + | + | + | - | F | PD | 6 |
| 16 | 26 | 2007 | 53 | M | NEC | R | 32x27 | 40 | 30 | - | + | + | + | + | - | P | PR | 51 |
| 17 | 27 | 2007 | 45 | M | ECC | C | 42 | N/A | 50 | - | - | + | + | + | + | P | PR | 67 |
| 18 | 28 | 2007 | 44 | F | MANEC | T | 80x75x50 | N/A | 100 | N/A | N/A | + | + | + | - | N/A | N/A | N/A |
| 19 | 29 | 2007 | 38 | F | ECC | T | 29x27 | N/A | 50 | - | + | + | + | + | - | F | PD | 9 |
| 20 | 30 | 2008 | 63 | M | ECC | A | 50x70 | N/A | 100 | - | - | + | + | + | - | F | PD | 41 |
| 21 | 31 | 2008 | 56 | M | ECC | C | 40x50 | N/A | N/A | - | - | + | + | + | - | P | PD | 6 |
| 22 | 7 | 2008 | 61 | M | ECC | R | 50 | N/A | 100 | + | + | + | + | + | + | F | PR | 50, alive |
| 23 | 32 | 2009 | 79 | F | ECC | S | 115x35 | N/A | 100 | +/- | + | + | + | + | - | P | SD | 14, alive |
| 24 | 33 | 2010 | 78 | M | NEC | S | 82x74 | N/A | N/A | - | + | + | + | + | - | F | SD | 10 |
| 25 | 34 | 2010 | 59 | M | ECC | N/A | N/A | 80 | N/A | N/A | N/A | + | N/A | N/A | N/A | N/A | N/A | N/A |
| 26 | 35 | 2011 | 63 | M | NEC | A | N/A | N/A | N/A | N/A | - | + | + | + | - | F | PR | 11 |
| 27 | 36 | 2011 | 70 | M | NEC | A | 74x51 | N/A | 60 | - | - | + | + | - | - | - | N/A | N/A |
| 28 | 37 | 2011 | 74 | F | NEC | A | N/A | 90 | 100 | + | - | + | + | - | - | - | N/A | 1 |
| 29 | 38 | 2011 | 76 | F | NEC | A | N/A | 66.3 | 50 | - | - | + | + | + | - | P | PR | 27, alive |
| 30 | 39 | 2012 | 54 | M | MANEC | R | 30 | N/A | 50 | - | N/A | N/A | + | + | - | F | N/A | N/A |
| 31 | 40 | 2012 | 76 | F | NEC | T | 183x115 | N/A | 100 | - | + | - | + | + | - | F | PD | 42, alive |
| 32 | 41 | 2012 | 74 | F | NEC | A | N/A | 75 | 30 | - | - | + | - | + | - | P | PR | 8 |
| 33 | 42 | 2012 | 57 | F | NEC | N/A | N/A | 80 | 30 | - | N/A | + | N/A | N/A | N/A | N/A | N/A | N/A |
| 34 | 43 | 2012 | 81 | F | NEC | C,A | N/A | N/A | 100 | N/A | N/A | + | + | - | - | - | N/A | 6 |
| 35 | 44 | 2012 | 68 | F | NEC | S | 30 | N/A | 50 | - | N/A | + | - | - | - | - | N/A | 0.5 |
| 36 | 45 | 2013 | 51 | M | NEC | R | N/A | N/A | 50 | - | - | + | + | + | - | F | PR | 12, alive |
| 37 | 46 | 2013 | 68 | M | NEC | R | N/A | N/A | 50 | - | - | + | + | + | + | P | PR | 7 |
| 38 | 47 | 2014 | 77 | M | NEC | A | 40x35 | 20-30 | 30 | - | - | + | + | + | - | F | PD | 8, alive |
| 39 | 48 | 2014 | 71 | M | MANEC | T | 70x45 | 25 | 80 | + | - | + | + | + | - | F | PD | 13 |
| 40 | 49 | 2014 | 48 | M | MANEC | S | N/A | N/A | 100 | + | + | + | + | + | + | F | PD | 3 |
| 41 | 50 | 2014 | 63 | F | NEC | A | N/A | 60-70 | 100 | + | - | + | + | + | - | P | PD | 10 |
| 42 | 51 | 2014 | 39 | M | MANEC | T | N/A | 80 | 50 | - | - | + | + | + | - | F | PD | 7 |
| 43 | 52 | 2014 | 55 | F | MANEC | A | N/A | N/A | 30 | - | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 44 | 53 | 2014 | 34 | F | MANEC | D | N/A | N/A | 100 | + | + | N/A | + | N/A | N/A | N/A | N/A | N/A |
| 45 | 54 | 2015 | 74 | F | MANEC | C | 70x18 | <20 | 100 | + | + | - | + | + | - | F | SD | 10, alive |
| 46 | 55 | 2015 | 44 | M | NEC | A | 170x110x80 | N/A | 100 | + | + | - | + | + | - | P | SD | 84, alive |
| 47 | 56 | 2016 | 70 | M | MANEC | D | 100 | 82.9 | 100 | - | + | + | + | + | - | F | CR | 30, alive |
| 48 | 57 | 2016 | 48 | F | NEC | S | 93x40 | >90 | 100 | +/- | - | + | - | + | - | P | PR | 2 |
| 49 | 58 | 2016 | 70 | M | NEC | S | 15 | N/A | 25 | - | - | + | - | + | - | P | N/A | N/A |
| 50 | 59 | 2016 | 67 | M | NEC+SCC | C | 60x50 | >40 | 100 | + | + | + | + | + | - | P | PD | 3 |
| 51 | 60 | 2017 | 49 | F | ECC | T | 100x100 | N/A | 100 | - | + | - | + | - | - | - | N/A | 10, alive |
| 52 | 61 | 2017 | 60 | M | NEC | Anus | 20 | 90 | N/A | - | - | + | - | + | - | N/A | PR | N/A |
| 53 | 62 | 2017 | 68 | M | MANEC | A | 30 | 75 | 30 | - | - | - | + | + | - | P | SD | N/A |
| 54 | 63 | 2017 | 32 | M | MANEC | C | 80x55 | N/A | 70 | +/- | - | + | + | + | - | F | SD | 6, alive |
| 55 | 64 | 2017 | 61 | F | NEC | T | 50 | 90 | 100 | + | N/A | - | + | - | - | - | N/A | N/A |
| 56 | 65 | 2018 | 74 | M | NEC | S | 60x50 | 90 | 100 | - | + | + | + | + | - | F | SD | 36, alive |
| 57 | 66 | 2018 | 68 | M | NEC+SCC | D | 35x35 | 80 | 100 | +/- | - | + | + | + | - | P | PD | N/A |
| 58 | 67 | 2018 | 40 | F | NEC | R | 45x36x44 | N/A | 50 | - | N/A | + | - | + | + | P | CR | N/A |
| 59 | 68 | 2018 | 77 | M | ECC | T | N/A | N/A | 100 | + | - | + | + | - | - | - | N/A | 2 |
| 60 | N/A | Our Case | 55 | M | NEC | T | 100x100 | 90 | 100 | + | + | + | - | + | - | P | PD | 4 |
Although a reliable treatment guideline has not presented yet, chemo-therapy plays a key role in treat-ment of patients with advanced NEC. Platinum-based chemotherapy, as a therapeutic strategy, is often used and the response rate is 42% to NEC that is relatively lower than that of 67% for small cell lung cancer[6]. A previous study proposed the effectiveness of 5-fluorouracil (5-FU)-based chemotherapy[7]; however, as mentioned earlier, a standard regimen for NEC has not been developed yet. It has also been reported that a regimen for the MANEC, comprising neoplasms with both neuroendocrine carcinomatous and adenocarcinomatous components, depends on which component dominantly contributes. In the present research, the number of patients with NEC and MANEC was 44 and 13, and the mean age was 61.5 and 56.2 years old, respectively (other two patients were diagnosed as the combination of NEC with squamous cell carcinoma). Besides, 29 patients were died due to these tumors, while 15 patients were saved by treatment with tumor resection and chemotherapy. The OS of 48 patients who received the tumor resection was 19.2 mo, which was significantly higher than 3.4 mo belonged to 7 patients who did not undergo surgical resection. These results highly reveal that surgical resection is essential to prolong prognosis. However, a poor prognosis was observed in the majority of those patients because of the delayed diagnosis similar to our case, and we therefore were unable to perform the surgical treatment. To follow the chemotherapy, an effective stenting for the obstructive tumor is vital for treatment and also for quality of life (QOL) of the patients as significant rapid tumor progression in both inside and outside the colon are clinical features of NEC and may cause intestinal tract obstruction and also stenosis of the surrounding organs, including small intestine. The rapid growth resulted in the huge tumor upon the diagnoses, as our findings showed that the average diameter of NEC was 76.8 mm, and growth toward outside of the colon, outward invasion, which was observed in 42% of the patients, and similar results reported by a previous study[5]. Importantly, MANEC, associating with a rapid growth pattern in NEC, showed 60% of outward growth, indicating that the higher growth rate of the tumor cells represents this aggressive and infiltrative growth pattern. In our case, colonic and duodenum self-expandable metallic stent (SEMS) were inserted for direct colonial obstruction and infiltrative growth toward the duodenum. Generally, stenting in the gastrointestinal tract for malignant obstruction due to the adenocarcinoma has been reported as an effective and safe strategy with the clinical success rate of 90.5%–95.5%, as well as an adverse event rate of 3.5%–7.6%[8-10]. In addition, it is extremely rare to find out the tumor perforation, following the stent placement with the rate of 2% that might occur at the necrotic tissue of the tumor[11]. The main reason of the tumor perforation following SEMS insertion in our case is likely due to the rapid growth of the NEC tumor cells at both inside and outside the colon, evidenced by the tumor necrosis appeared in the endoscopic findings and 90% of positive cells by Ki67 staining that led to the vulnerability of the mass structure. As successful induction of the chemotherapy could lead to the better survival period (Table 2), stenting is of great importance to manage the symptoms and QOL. The summary of the chemotherapy induced in the recent cases are summarized in Table 2[7,12-68]. As shown in Table 2, 24 NEC patients received platinum-based chemotherapy and 11 NEC patients received 5-FU-based chemotherapy as the first-line regimen. In particular, 9 MANEC patients received 5-FU-based chemotherapy, and only 1 patient received platinum-based chemotherapy, probably targeting the component of adenocarcinoma. The responses to the platinum-based and 5-FU-based chemotherapy were (CR, 2; PR, 7; stable disease (SD), 3; and progressive disease (PD), 11; and (CR, 0; PR, 3; SD, 2; and PD, 6), respectively. Therefore, development of an effective chemotherapy-based regimen is essential as well.
Consequently, exertion is essential to detect NEC in early stage, thereby the correct diagnosis is of great importance, while NEC and MANEC are frequently misdiagnosed as adenocarcinoma or another malignant tumor at the first imaging or histological study[5]. Thus, to diagnose accurately, detailed endoscopic observation and histological research are required. A study suggested that fluorodeoxyglucose positron emission tomography (FDG-PET) associates with high-sensitivity to tumor, as well as high-proliferation (e.g., NEC)[12], therefore FDG-PET is precious to diagnose tumor with clinical feature of NEC.
At present, early diagnosis followed by the surgical resection is the most favorable clinical course for better prognosis, and if impossible, careful making decision for chemotherapy and stenting for obstruction is significant. Furthermore, NEC with higher cell proliferation not only may cause the intestinal obstruction, but also the invasive growth to the surrounding organs, leading to the tumor rupture after stenting inside the tract, thus careful consideration is essential for making a right clinical decision. In particular, the placement of stent needs to be highly taken into account as it is significantly different from the colorectal adenocarcinoma in terms of the cell growth pattern, and clinical characteristics.
As a result, as the rapid growth pattern of NEC is difficult to be managed, early diagnosis and careful management with the understanding of the disease are essential. However, accumulated data related to this rare disease may assist physicians to effectively treat patients with the help of development of chemotherapy, stenting method, as well as upgrading medical devices. We hope that the results of the present study can enhance the information related to NEC and also help the scholars to better understand the disease.
Manuscript source: Invited Manuscript
Specialty type: Medicine, research and experimental
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tarnawski AS S-Editor: Cui LJ L-Editor: AE-Editor: Wu YXJ
| 1. | Bertani E, Ravizza D, Milione M, Massironi S, Grana CM, Zerini D, Piccioli AN, Spinoglio G, Fazio N. Neuroendocrine neoplasms of rectum: A management update. Cancer Treat Rev. 2018;66:45-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (2)] |
| 2. | Qiu S, Pellino G, Warren OJ, Mills S, Goldin R, Kontovounisios C, Tekkis PP. Mixed adenoneuroendocrine carcinoma of the colon and rectum. Acta Chir Belg. 2018;118:273-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Shafqat H, Ali S, Salhab M, Olszewski AJ. Survival of patients with neuroendocrine carcinoma of the colon and rectum: a population-based analysis. Dis Colon Rectum. 2015;58:294-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 73] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 4. | Paspala A, Machairas N, Prodromidou A, Spartalis E, Ioannidis A, Kostakis ID, Papaconstantinou D, Nikiteas N. Management of MANEC of the colon and rectum: A comprehensive review of the literature. Mol Clin Oncol. 2018;9:219-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Zhang Y, Xie J, Wang J, Yang D, Jiang Z, Han G, Fu Q, Zhang Y. Clinicopathological and Prognostic Analysis of Neuroendocrine Carcinoma of the Colorectum. Adv Clin Exp Med. 2016;25:719-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Conte B, George B, Overman M, Estrella J, Jiang ZQ, Mehrvarz Sarshekeh A, Ferrarotto R, Hoff PM, Rashid A, Yao JC, Kopetz S, Dasari A. High-Grade Neuroendocrine Colorectal Carcinomas: A Retrospective Study of 100 Patients. Clin Colorectal Cancer. 2016;15:e1-e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Wu Z, Yu D, Zhao S, Gao P, Song Y, Sun Y, Chen X, Wang Z. The efficacy of chemotherapy and operation in patients with colorectal neuroendocrine carcinoma. J Surg Res. 2018;225:54-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Matsuzawa T, Ishida H, Yoshida S, Isayama H, Kuwai T, Maetani I, Shimada M, Yamada T, Saito S, Tomita M, Koizumi K, Hirata N, Sasaki T, Enomoto T, Saida Y. A Japanese prospective multicenter study of self-expandable metal stent placement for malignant colorectal obstruction: short-term safety and efficacy within 7 days of stent procedure in 513 cases. Gastrointest Endosc. 2015;82:697-707.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 74] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 9. | Meisner S, González-Huix F, Vandervoort JG, Repici A, Xinopoulos D, Grund KE, Goldberg P, Registry Group TW. Self-Expanding Metal Stenting for Palliation of Patients with Malignant Colonic Obstruction: Effectiveness and Efficacy on 255 Patients with 12-Month's Follow-up. Gastroenterol Res Pract. 2012;2012:296347. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Han SH, Lee JH. Colonic stent-related complications and their management. Clin Endosc. 2014;47:415-419. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Binderup T, Knigge U, Loft A, Mortensen J, Pfeifer A, Federspiel B, Hansen CP, Højgaard L, Kjaer A. Functional imaging of neuroendocrine tumors: a head-to-head comparison of somatostatin receptor scintigraphy, 123I-MIBG scintigraphy, and 18F-FDG PET. J Nucl Med. 2010;51:704-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 189] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 12. | Nasu J, Kotake, K, Koyama Y, Imura J, Igarashi S, Tsumuraya M. Endocrine cell carcinoma of the colon: Report of a case. J Jpn Soc Coloproctol. 1996;49:161-166. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Shimada K, Ueno S, Oshima Y, Nakamura H, Hiki Y, Kakita A. A case of endocrine cell carcinoma of the rectum. J Jpn Surg Assoc. 1998;59:1346-1349. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Lortholary AH, Cadeau SD, Bertrand GM, Guerin-Meyer VI, Gamelin EC, Audran MJ. Humoral hypercalcemia in patients with colorectal carcinoma: report of two cases and review of the literature. Cancer. 1999;86:2217-2221. [PubMed] |
| 15. | Okuyama T, Korenaga D, Tamura S, Yao T, Maekawa S, Watanabe A, Ikeda T, Sugimachi K. The effectiveness of chemotherapy with cisplatin and 5-fluorouracil for recurrent small cell neuroendocrine carcinoma of the rectum: report of a case. Surg Today. 1999;29:165-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Yukawa N, Akaike M, Sugimasa Y, Takemiya S, Kameda Y, Imada T. 42-month survival following chemotherapy for small-cell rectal carcinoma. Jpn J Gastroenterol Surg. 2002;35:1443-1447. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Ouban A, Nawab RA, Coppola D. Diagnostic and pathogenetic implications of colorectal carcinomas with multidirectional differentiation: a report of 4 cases. Clin Colorectal Cancer. 2002;1:243-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Scherwitz P, Lindenfelser R, Krüger I. [Localization of primary small cell carcinoma with liver metastasis: a rare combination of colonic adenocarcinoma and undifferentiated small cell carcinoma]. Chirurg. 2002;73:859-861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Tsujie M, Shibata N, Nomura T, Okuda H, Nomura T, Takeda M. A Case of endocrine cell carcinoma of the rectum. Jpn J Gastroenterol Surg. 2003;36:240-244. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Yamauchi K, Miyata T, Okada N, Nitta T, Kawai H, Miyasita T. A Case of endocrine cell carcinoma of the rectal. J Jpn Surg Assoc. 2004;65:751-755. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Tsutani Y, Aoki H, Harano M, Sasaki H, Onoda T, Shiozaki S. Effectiveness of neoadjuvant chemotherapy against neuroendocrine carcinoma of the colon with duodenal invasion. Report of a Case. Jpn J Gastroenterol Surg. 2004;37:1485-1490. [RCA] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Kabeshima Y, Takahashi M, Kameyama N, Toizumi A, Tamura Y, Kageyama T. Solitary cervical metastasis of poorly differentiated adenocarcinoma with neuroendocrine differentiation of the rectum. Report of a Case. Jpn J Gastroenterol Surg. 2004;37:241-246. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Yodonawa S, Ogawa I, Goto Y, Ito H, Kitahara M, Asagoe T. A case of juvenile endocrine cell carcinoma of the transverse colon. Jpn J Gastroenterol Surg. 2006;39:406-411. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Sunose Y, Takeyoshi I, Ogawa T, Tomizawa N, Itoh H, Morishita Y. A giant endocrine cell cancer of the rectum that remained progression free for 20 months with multidisciplinary treatment. J Jpn Surg Assoc. 2006;67:1848-1852. [RCA] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Ohnishi T, Kanoh T, Murakami M, Hoshino H, Kimura Y, Iwazawa T. Neuroendocrine carcinoma of the colon - report of two cases. Jpn J Gastroenterol Surg. 2006;39:509-515. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 26. | Morimoto Y, Ookura M, Iwagaki H, Kawamoto K, Yoshida Y, Itou T. A case of rectal neuroendocrine carcinoma metastatic to the brain. J Jpn Soc Coloproctol. 2007;60:167. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Takeshima K, Yamafuji K, Asami A, Hayashi N, Baba H, Okamoto N. A long survival case of endocrine cell carcinoma of the cecum. Jpn J Gastroenterol Surg. 2007;40:757-763. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Butte JM, Torres J, Duarte I, Zúñiga A. [Composite tumor of the colon with liver metastases]. Cir Esp. 2007;82:128-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Ishizuka N, Ishibashi K, Ohsawa T, Yokoyama M, Nakada H, Ishida H. Rapidly growing endocrine cell carcinoma of the colon with elevated expression of vascular endothelial growth factor(VEGF)and VEGF-C: a case report. Nippon Daicho Komonbyo Gakkai. 2007;60:269-275. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 30. | Oshima Y, Isaka N, Takeuchi T, Arita S, Tanaka H, Koikea N. A case of long-term survival after chemotherapy for liver metastasis from endocrine cell carcinoma of the colon. J Jpn Surg Assoc. 2008;69:2331-2336. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Shimakage N, Hasegawa J, Okamura N, Tajima K. A case of primary endocrine cell carcinoma of the cecum with the onset of ileocecal intussusception. J Jpn Surg Assoc. 2008;69:115-119. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 32. | Tanoue Y, Tanaka N, Suzuki Y, Hata S, Yokota A. A case report of endocrine cell carcinoma in the sigmoid colon with inferior mesenteric vein tumor embolism. World J Gastroenterol. 2009;15:248-251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | Kawaguchi T, Itoh T, Toma A, Fuji N, Mazaki T, Naito K, Otsuji E. A Case of Neuroendocrine Cell Carcinoma with Sigmoidovesical Fistula. Case Rep Gastroenterol. 2010;4:178-184. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 34. | Saint-Blancard P, Hervouet M, Chapuis O. [Poorly differentiated endocrine carcinoma of the colon]. Rev Med Interne. 2010;31:e10-e12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 35. | Kikuchi A, Yamauchi S, Ono H, Kato S, Ishiguro M, Ishikawa T, Kobayashi H, Iida S, Uetake H, Higuchi T, Enomoto M, Sugihara K. [A case of colonic neuroendocrine carcinoma with severe liver dysfunction by multiple liver metastases successfully treated with hepatic arterial infusion]. Gan To Kagaku Ryoho. 2011;38:2268-2270. [PubMed] |
| 36. | Kim YN, Park HS, Jang KY, Moon WS, Lee DG, Lee H, Lee MR, Kim KR. Concurrent large cell neuroendocrine carcinoma and adenocarcinoma of the ascending colon: a case report. J Korean Soc Coloproctol. 2011;27:157-161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 37. | Pascarella MR, McCloskey D, Jenab-Wolcott J, Vala M, Rovito M, McHugh J. Large cell neuroendocrine carcinoma of the colon: A rare and aggressive tumor. J Gastrointest Oncol. 2011;2:250-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 38. | Akiyama S, Niitani T, Narasaka T, Ohto T, Gamoh M. [Poorly-differentiated neuroendocrine carcinoma of ascending colon with liver metastases successfully treated with carboplatin and etoposide]. Gan To Kagaku Ryoho. 2011;38:1209-1212. [PubMed] |
| 39. | Kim DW, Kim SH, Yoon JM, Jun TY, Lee SJ, Kim YJ, Kim HY, Lee JS. [A case of colonic collision tumor (adenocarcinoma and neuroendocrine carcinoma)]. Korean J Gastroenterol. 2012;60:325-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 40. | Yabuki H, Suto T, Inoue K, Fujimoto H, Sato T, Ikeda E, Iizawa H. [A case of colorectal neuroendocrine carcinoma effectively treated with bevacizumab+levofolinate+5-FU chemotherapy]. Gan To Kagaku Ryoho. 2012;39:1139-1142. [PubMed] |
| 41. | Yamashita K, Ishikawa D, Nanjo S, Takeuchi S, Yamada T, Mouri H, Ohtsubo K, Yasumoto K, Kumagai M, Ueda Y, Yano S. [A case of poorly-differentiated neuroendocrine carcinoma of the ascending colon with multiple liver metastases successfully treated with cisplatin and irinotecan]. Gan To Kagaku Ryoho. 2012;39:1427-1430. [PubMed] |
| 42. | Andreu V, Chahri N, Vega AB, Muñoz V, Paules MJ, Perelló A, Abad A, Barenys M. [Poorly differentiated neuroendocrine carcinoma of the colon with liver metastases]. Gastroenterol Hepatol. 2012;35:251-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 43. | Portale TR, Branca A, Pesce A, Puleo S. Neuroendocrine carcinoma of colon and rectum: a rare neoplasia with a poor prognosis. Minerva Chir. 2012;67:283-284. [PubMed] |
| 44. | Abdel Samie A, Sun R, Fayyazi A, Theilmann L. Poorly Differentiated Neuroendocrine Carcinoma of the Sigmoid Colon-a Rare Differential Diagnosis of Malignant Colon Tumours. J Gastrointest Cancer. 2012;43 Suppl 1:S211-S214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 45. | Wakatsuki K, Yoshioka S, Shiobara M, Kataoka M, Arai S, Tonooka T, Miyazawa K, Oeda Y. [A case of rectal endocrine cell carcinoma treated by laparoscopic assisted intersphincteric resection after neoadjuvant chemotherapy]. Gan To Kagaku Ryoho. 2013;40:2026-2028. [PubMed] |
| 46. | Vergelí-Rojas JA, Santiago-Caraballo DL, Cáceres-Perkins W, Magno-Pagatzartundua P, Toro DH. Small cell neuroendocrine carcinoma of rectum with associated paraneoplastic syndrome: a case report. P R Health Sci J. 2013;32:51-53. [PubMed] |
| 47. | Yamanashi T, Nishi T, Yamamoto T, Toriumi F, Koshida Y, Mukai K, Shimoyama Y. A case of endocrine cell carcinoma of the ascending colon with liver metastasis treated with hepatectomy after excision of the primary lesion and systemic chemotherapy. Gan To Kagaku Ryoho. 2014;41:107-112. [PubMed] |
| 48. | Kusakabe J, Miki A, Kobayashi H, Uryuhara K, Hashida H, Mizumoto M, Kaihara S, Hosotani R, Yamashita D. [A case of mixed adenoneuroendocrine carcinoma of the transverse colon]. Gan To Kagaku Ryoho. 2014;41:1826-1828. [PubMed] |
| 49. | Takuma K, Ohtsuka H, Shimizu H, Osaka I, Takanishi K. [A case of rapidly progressing treatment-resistant colorectal neuroendocrine carcinoma]. Gan To Kagaku Ryoho. 2014;41:1823-1825. [PubMed] |
| 50. | Tanabe H, Takase T, Morimoto D, Tanaka Y, Shibata A, Yaguchi T. Effective chemotherapy with bevacizumab/FOLFOX4 for neuroendocrine carcinoma of the ascending colon - a case study. Gan To Kagaku Ryoho. 2014;41:661-664. [PubMed] |
| 51. | Ito H, Kudo A, Matsumura S, Ban D, Irie T, Ochiai T, Nakamura N, Tanaka S, Tanabe M. Mixed adenoneuroendocrine carcinoma of the colon progressed rapidly after hepatic rupture: report of a case. Int Surg. 2014;99:40-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 52. | Thosani N, Rao B, Ertan A, Guha S. Wide spectrum of neuroendocrine differentiation in identical appearing colon polyps: A report of 2 mixed endocrine-glandular polyps. Turk J Gastroenterol. 2014;25 Suppl 1:242-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 53. | Bartók Á, Banai Z, Berczi L. [The surgical case of a 34-year-old female patient with a metastatizing double colon tumor with different histological structure, causing mechanical obstruction]. Magy Seb. 2014;67:44-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 54. | Gurzu S, Kadar Z, Bara T, Bara T, Tamasi A, Azamfirei L, Jung I. Mixed adenoneuroendocrine carcinoma of gastrointestinal tract: report of two cases. World J Gastroenterol. 2015;21:1329-1333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 64] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 55. | Kobayashi H, Koizumi N, Takagi T, Fukumoto K. The Case of a Long-Surviving Patient with Colorectal Neuroendocrine Carcinoma with Invasion of the Jejunum and Lymph Node Metastases after Operation. Gan To Kagaku Ryoho. 2015;42:2218-2220. [PubMed] |
| 56. | Kakuta S, Takayama W, Kou T, Satou M, Sugaya M. A Case of Descending Colon Adenocarcinoma with Neuroendocrine Differentiation Successfully Treated with FOLFIRI plus Bevacizumab. Gan To Kagaku Ryoho. 2016;43:129-132. [PubMed] |
| 57. | Fujimoto K, Nakashima T, Sasaki K, Hayashi K, Hanafusa M, Yoshida S, Myojo S, Yoshida SI, Sawai S, Sano N. Ectopic adrenocorticotropic hormone syndrome caused by neuroendocrine carcinoma of the colon. Nihon Shokakibyo Gakkai Zasshi. 2016;113:1752-1760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 58. | Yoshihara T, Shinzaki S, Hiyama S, Murai K, Takehara T. Metastatic colon neuroendocrine carcinoma found in a patient with ulcerative colitis during annual endoscopic surveillance. Gastrointest Endosc. 2016;84:1075-1076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 59. | Hassan U, Mozayani B, Wong NA. Primary combined neuroendocrine carcinoma (small-cell type) and squamous cell carcinoma of the colon. Histopathology. 2016;68:755-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 60. | Takahashi R, Uchima Y, Aomatsu N, Nobori C, Kurihara S, Yamakoshi Y, Wang E, Nagashima D, Hirakawa T, Iwauchi T, Morimoto J, Tei S, Nakazawa K, Takeuchi K. [A Case of Huge Advanced Neuroendocrine Carcinoma of the Transverse Colon Resected Successfully]. Gan To Kagaku Ryoho. 2017;44:1586-1588. [PubMed] |
| 61. | Khan M, Dirweesh A, Alvarez C, Conaway H, Moser R. Anal Neuroendocrine Tumor Masquerading as External Hemorrhoids: A Case Report. Gastroenterology Res. 2017;10:56-58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 62. | Soliman ML, Tiwari A, Zhao Q. Coexisting tubular adenoma with a neuroendocrine carcinoma of colon allowing early surgical intervention and implicating a shared stem cell origin. World J Gastroenterol. 2017;23:1106-1112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 63. | Shin SH, Kim SH, Jung SH, Jang JW, Kang MS, Kim SI, Kim JH, Lee JH. High-Grade Mixed Adenoneuroendocrine Carcinoma in the Cecum: A Case Report. Ann Coloproctol. 2017;33:39-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 64. | Wincewicz A, Kowalik A, Zięba S, Sułkowski S, Góźdź S. Morphology with immunohistochemical and genetic profiling of high-grade neuroendocrine carcinoma of colon - a case report with review of literature. Rom J Morphol Embryol. 2017;58:655-663. [PubMed] |
| 65. | Kim JJ, Park SS, Lee TG, Lee HC, Lee SJ. Large Cell Neuroendocrine Carcinoma of the Colon With Carcinomatosis Peritonei. Ann Coloproctol. 2018;34:222-225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 66. | Munakata S, Murai Y, Koizumi A, Kato H, Yamamoto R, Ueda S, Tokuda S, Sakuraba S, Kushida T, Orita H, Sakurada M, Maekawa H, Sato K. Mixed Neuroendocrine Carcinoma and Squamous Cell Carcinoma of the Colon: Case Report and Literature Review. Case Rep Gastroenterol. 2018;12:240-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 67. | Kaila V, Lager D, Jain R. A Rare Tumor Presenting as a Rectal Mass. Gastroenterology. 2018;155:273-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 68. | Yabe S, Yamamoto E, Masuda T, Sugimoto H, Koshiishi H, Yoshimura T. A Case of Endocrine Cell Carcinoma of the Transverse Colon with Very Poor Prognosis, Onset with Bowel Obstruction. Gan To Kagaku Ryoho. 2018;45:178-180. [PubMed] |