Published online Sep 6, 2018. doi: 10.12998/wjcc.v6.i9.291
Peer-review started: March 25, 2018
First decision: April 26, 2018
Revised: June 18, 2018
Accepted: June 27, 2018
Article in press: June 27, 2018
Published online: September 6, 2018
Processing time: 167 Days and 18.8 Hours
Acute pancreatitis is rarely associated with drugs. Acetaminophen overdose is a well-known cause of hepatic toxicity, but drug-induced pancreatitis is rarely reported, especially after mild overdose. A 32-year-old woman presented with nausea and vomiting for 12 h, but no abdominal pain following an overdose of eight Tylenol tablets containing acetaminophen (325 mg acetaminophen per tablet). Laboratory results on admission showed abnormal amylase and lipase levels but completely normal liver function. Magnetic resonance cholangiopancreatography revealed mild swelling of the pancreas without fluid collection around the pancreas. The patient complained of severe abdominal pain five days after admission when attempting to drink water and liquids. Eight days after admission, fluid around the pancreas was observed by computed tomography. The patient was subsequently diagnosed with acetaminophen-induced acute pancreatitis after exclusion of common causes. Routine treatment for pancreatitis and N-acetylcysteine were administered to prevent disease progression. The patient was discharged in good condition.
Core tip: This case shows that a dose of acetaminophen of less than 4 g can cause acute pancreatitis without liver damage, and that the mechanism of pancreatitis is different from that of hepatitis, and acetaminophen-induced acute pancreatitis may not be related to the drug dose. Although drug-induced acute pancreatitis is rare and the detailed underlying mechanism is unknown, physicians should consider this etiology after ruling out other causes of pancreatitis, especially in young women who are at high risk of overdosing on Class I and Class II drugs.
- Citation: He YH, Lu L, Wang YF, Huang JS, Zhu WQ, Guo Y, Li CX, Li HM. Acetaminophen-induced acute pancreatitis: A case report and literature review. World J Clin Cases 2018; 6(9): 291-295
- URL: https://www.wjgnet.com/2307-8960/full/v6/i9/291.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i9.291
Acute pancreatitis is a common disease in the clinic, and the mortality rate in patients with severe pancreatitis is high. Biliary stones, alcohol consumption, metabolic disorders and tumors are the most frequent causes of acute pancreatitis. Drug-induced acute pancreatitis is implicated in only a minority of cases, with an incidence of 0.1%-2%[1]. To date, over 130 kinds of drugs have been reported to cause acute pancreatitis, including acetaminophen[2]. It is well known that acetaminophen overdose causes hepatic toxicity, but it is a rare cause of acute pancreatitis. Only 11 cases of pancreatitis and hepatic impairment have been associated with acetaminophen at doses ranging from 4 to 120 g. Unlike previous reported cases, we report a case of acute pancreatitis caused by low doses of acetaminophen but without liver damage (Tables 1 and 2).
| Year | Age/gender | APAP (g) | Serum APAP | AMS (IU/L) | ALT (IU/L) | TBil | NAC | Ref. |
| 1977 | 31/F | 60 | NA | 1440 | 300 | H | No | [7] |
| 1977 | 41/F | 25 | NA | 1250 | NA | H | No | [8] |
| 1986 | 19/M | 25 | 62 μg/mL | 1500 | 380 | NA | Yes | [9] |
| 1991 | 34/F | 9.37-13 | 77.7 μg/mL | 936 | 225 | NA | Yes | [10] |
| 1995 | 48/F | 25 | NA | 300 | 8700 | NA | No | [11] |
| 1997 | 74/F | NAa | 31 μg/mL | 787 | 3070 | H | Yes | [12] |
| 2001 | 47/M | 4 | NA | 498 | 408 | H | No | [13] |
| 2009 | 35/F | 3.97-5.3b | NA | 1414 | 75 (H) | Normal | No | [14] |
| 2009 | 17/F | 15 | Below | 529 | Normal | Normal | No | [15] |
| 2012 | 40/F | H | NA | NAc | Normal | Normal | Yes | [16] |
| 2014 | 19/F | 78-120 | 208.4 μg/mL | 638 | 9689 | H | NA | [17] |
| Causes of acute pancreatitis | |
| Common causes | Gallstones, alcohol misuse, hyperlipidemia |
| Other causes | Hypercalcemia, autoimmune, idiopathic, drugs, trauma, tumor |
A 32-year-old woman presented with nausea and vomiting for 12 h associated with dizziness and epigastric pain. Before attending the hospital, she took eight Tylenol tablets containing acetaminophen (325 mg acetaminophen per tablet) after quarreling with her husband. She denied taking other drugs, alcohol consumption, gallbladder stones, trauma, autoimmune diseases and diabetes mellitus. The upper abdomen was soft with mild tenderness. Jaundice, hepatosplenomegaly, ascites, and Murphy’s sign were absent.
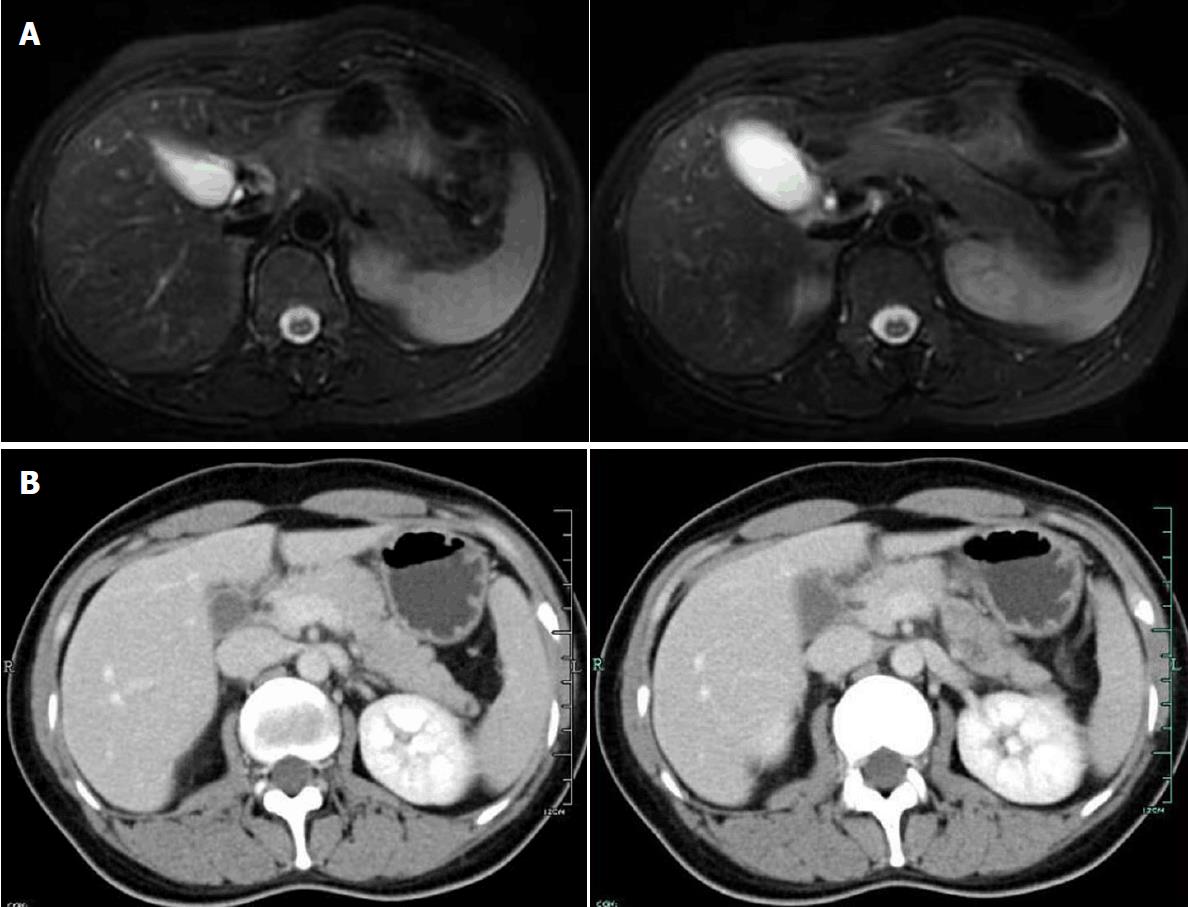
Laboratory examinations showed the following: Hemoglobin 10.8 g/dL, white blood cells 5.5 × 10-9/L, neutrophils 65%, and platelets 169 × 10-9/L. Emergency biochemical tests showed aspartate aminotransferase 13 U/L (7-40 U/L), glutamic oxaloacetic transaminase 13 U/L (13-35 U/L), serum albumin 3.3 g/dL, serum amylase 990 U/L (0-96 U/L), serum lipase 49.5 U/L (13-60 U/L) and triglycerides 0.6 mmol/L (0.34-1.70 mmol/L). Two days later, blood biochemistry showed aspartate aminotransferase 13 U/L, glutamic oxaloacetic transaminase 13 U/L, alkaline phosphatase 52 U/L (35-100 U/L), serum albumin 40.9 g/L, serum amylase 433 U/L, serum lipase 136.6 U/L, triglycerides 0.6 mmol/L, and serum creatinine 53 μmol/L (45-84 μmol/L). Viral hepatitis markers (A, B, C, D and E), antinuclear antibody Hep-2, antineutrophil cytoplasmic antibody (ANCA), peripheral-ANCA and cytoplasmic-ANCA were negative. Serum IgG4 was 1.08 (0.03-2) g/L. Abdominal ultrasonography showed no abnormalities in the pancreas. However, magnetic resonance cholangiopancreatography (MRCP) showed that the pancreas was bulky without exudation. In addition to routine treatment for pancreatitis, N-acetylcysteine was administered to the patient to prevent disease progression. Five days after admission, she was able to drink water and take a liquid diet. Her serum amylase level decreased and abdominal pain resolved. However, that night she complained of severe upper abdominal pain radiating to the midcentral back with nausea and hypoglycemia. Contrast-enhanced computed tomography (CT) demonstrated swelling of the pancreas, especially the head of the pancreas, with fluid collection around the pancreas (Figure 1). Therefore, the patient was fasted again. In the following days, abdominal pain gradually alleviated and her diet gradually transitioned to semi-liquids as laboratory examinations revealed serum amylase of 281 U/L and lipase of 263.7 U/L with normal aminotransferase (13 U/L) after three days of pancreatic secretion/enzyme activity suppression and symptomatic treatment. On day 10 after admission, the patient requested early discharge as she had no abdominal pain or other feelings of discomfort. The patient was seen as an outpatient and laboratory examinations revealed serum amylase of 97 U/L and lipase of 15 U/L two weeks later. The patient refused further CT examination.
Drug-induced acute pancreatitis is rare with a reported incidence of 0.1%-2%, but should not be overlooked[1,3]. However, drug-induced pancreatitis remains a difficult and challenging diagnosis due to atypical clinical and laboratory tests, which is usually established by excluding other causes. A positive rechallenge is the most effective proof but cannot be performed due to ethical reasons. Our patient took an overdose of a drug containing acetaminophen in a suicide attempt. However, during the follow-up period, the typical conditions associated with acetaminophen overdose did not occur. In general, drug-induced acute pancreatitis is more frequent in children, women, the elderly, and in patients with advanced HIV infection and inflammatory bowel disease[4,5]. A single-center study with about 328 patients with acute pancreatitis from Australia revealed that drug-induced acute pancreatitis appeared to be more common in middle-aged women, which was attributed to the estrogens by an unclear mechanism[6]. Our patient was a young woman and thus a high-risk individual. Based on the weight of evidence including the presence of a rechallenge, latency, and the number of case reports, Badalov et al[3] divided drugs into five categories including acetaminophen, which was categorized as Class II. It has been reported that drugs belonging to Class I and Class II have the “most evidence” of causing acute pancreatitis as shown by published case reports[2].
Acetaminophen is frequently used for pain and fever in the clinic and is easily obtained from any pharmacy without prescription. Acetaminophen, when taken in an overdose, is a well-known cause of hepatic toxicity, but is rarely the etiologic agent of acute pancreatitis. To date, 11 case reports have been published describing acetaminophen-induced pancreatitis (Table 1)[7-17]. The first case was reported by Gilmore and Tourvas in 1977. Since then, another ten cases of acetaminophen-induced pancreatitis have been described. In most of these cases, a positive rechallenge was not performed. However, Hisato Igarashi et al[14] reported a 35-year-old woman who experienced a similar situation each time after three overdoses of acetaminophen due to severe pain in the lower limbs after experiencing high levels of stress. In our case, the diagnosis of acute pancreatitis was made based on clinical findings in combination with blood test results and confirmed by image examinations. MRCP indicated pancreatitis by its advantage over CT or ultrasound (US) because of its T1-weighted images with an advantage to differentiate between simple effusion and hemorrhagic necrosis of the peripancreatic fatty tissue and to depict acute pancreatic hemorrhage and its T2-weighted images with better sensibility of upper abdominal fluid collections[18,19]. Secondly, the diagnosis of acetaminophen-induced pancreatitis was established by excluding common etiologies such as gallstone pancreatitis, hyperlipidemic pancreatitis and ethanol-induced acute pancreatitis and other suspicious drugs that have been reported to cause pancreatitis.
In nine of these cases, different degrees of abnormal liver function were present and two cases had no evidence of hepatotoxicity (Table 1). Our patient showed no liver damage but pancreatitis, which may be related to the dose of acetaminophen and the different underlying mechanisms of liver toxicity and pancreatic toxicity. The recommended maximum therapeutic dose of acetaminophen is 4 g/d for an adult, and asymptomatic elevations in aminotransferases are sometimes seen with chronic use at the maximum recommended daily dose of 4 g[20,21]. In our patient, the maximum therapeutic dose was not reached and was lower than 3 g. In contrast, all other patients took more than 3 g acetaminophen, the highest dose being 120 g and the lowest dose approximately 4 g[17,13]. A reliable dose-dependent relationship between acetaminophen poisoning and severity of acute pancreatitis is lacking, which was also stated in the case reported by Praveen Jinnur[16,17,22]. He believed that normal liver function was attributed to individual susceptibility rather than dose-related drug toxicity[16]. Similarly, a retrospective study, which included 814 patients with acetaminophen poisoning, showed that acetaminophen-associated acute pancreatitis occurred in patients without fulminant hepatic failure and in two patients without significant hepatotoxicity[23]. Consistent with these findings is the theory that acetaminophen-induced pancreatitis is related to an idiosyncratic reaction rather than intrinsic drug toxicity, which is in line with Gilmore and Tourvasa who considered that pancreatitis and hepatitis have different viral causes, as did Hisato Igarashi and Zachary Cavanaugh[7,14,17]. Interestingly, 5 of 11 cases were similar to ours that patients took an excess of acetaminophen at a time, which made us doubt whether the frequency and single overdose of acetaminophen were related with pancreatic toxicity. Unfortunately, no adequate evidence-based basis has been found because understanding of drug-induced acute pancreatitis is largely based on case reports and critical reviews.
This patient was fortunately taken to the hospital in time and treated with N-acetylcysteine, which can prevent hepatotoxicity following acetaminophen overdose by replenishing hepatic glutathione stores. In patients who receive N-acetylcysteine within the first eight hours after an acute overdose, the risk of hepatotoxicity is less than 5%, whereas delays beyond 10 h are associated with an increased risk of hepatic injury[20]. In other cases, they either took a large dose of acetaminophen or did not receive timely treatment, or they were patients at high risk, such as those with known alcohol consumption, which may have led to drug-induced pancreatitis with different levels of liver damage.
In conclusion, less than 4 g acetaminophen can cause acute pancreatitis without liver damage, which indicates that the mechanism of pancreatitis is different from that of hepatitis, and the severity of acute pancreatitis may not have a reliable dose-dependent relationship. Although drug-induced acute pancreatitis is rare and easily ignored, we should be aware of this condition in high-risk patients with a history of drug overdose, especially Class I and Class II drugs, and both timely and appropriate treatment should be administered.
A 32-year-old woman presented with nausea and vomiting for 12 h associated with dizziness and epigastric pain.
Acetaminophen-induced acute pancreatitis.
Biliary pancreatitis, alcohol-induced pancreatitis, hyperlipidemic pancreatitis and codeine-induced pancreatitis.
Laboratory workup revealed a significant elevation of serum amylase of 990 U/L but normal aminotransferases.
Magnetic resonance cholangiopancreatography showed that the pancreas was bulky without exudation. Computed tomography demonstrated swelling of the pancreas, especially the head of the pancreas, with fluid collection around the pancreas.
Abrosia, routine treatment for pancreatitis, and N-acetylcysteine were administered to the patient.
A total of eleven cases of acetaminophen-induced acute pancreatitis have been reported in the literature but this case took the lowest dose of acetaminophen without liver damage.
Acetaminophen-induced acute pancreatitis is rare and should be considered in the differential diagnosis of acute pancreatitis, especially in high-risk patients with an overdose of suspected drugs.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Dambrauskas Z, Zaky A S- Editor: Ji FF L- Editor: Filipodia E- Editor: Tan WW
| 1. | Jones MR, Hall OM, Kaye AM, Kaye AD. Drug-induced acute pancreatitis: a review. Ochsner J. 2015;15:45-51. [PubMed] |
| 2. | Tenner S. Drug induced acute pancreatitis: does it exist? World J Gastroenterol. 2014;20:16529-16534. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 48] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Badalov N, Baradarian R, Iswara K, Li J, Steinberg W, Tenner S. Drug-induced acute pancreatitis: an evidence-based review. Clin Gastroenterol Hepatol. 2007;5:648-661; quiz 644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 348] [Cited by in RCA: 364] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 4. | Balani AR, Grendell JH. Drug-induced pancreatitis: incidence, management and prevention. Drug Saf. 2008;31:823-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 145] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 5. | Vinklerová I, Procházka M, Procházka V, Urbánek K. Incidence, severity, and etiology of drug-induced acute pancreatitis. Dig Dis Sci. 2010;55:2977-2981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 84] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 6. | Barreto SG, Tiong L, Williams R. Drug-induced acute pancreatitis in a cohort of 328 patients. A single-centre experience from Australia. JOP. 2011;12:581-585. [PubMed] |
| 7. | Gilmore IT, Tourvas E. Paracetamol-induced acute pancreatitis. Br Med J. 1977;1:753-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Coward RA. Paracetamol-induced acute pancreatitis. Br Med J. 1977;1:1086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Caldarola V, Hassett JM, Hall AH, Bronstein AB, Kulig KW, Rumack BH. Hemorrhagic pancreatitis associated with acetaminophen overdose. Am J Gastroenterol. 1986;81:579-582. [PubMed] |
| 10. | Mofenson HC, Caraccio TR, Nawaz H, Steckler G. Acetaminophen induced pancreatitis. J Toxicol Clin Toxicol. 1991;29:223-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Larsen FS, Clemmesen JO, Hansen BA. [Hemorrhagic pancreatitis. A rare complication of paracetamol poisoning]. Ugeskr Laeger. 1995;157:898-899. [PubMed] |
| 12. | Farrell J, Schmitz PG. Paracetamol-induced pancreatitis and fulminant hepatitis in a hemodialysis patient. Clin Nephrol. 1997;48:132-133. [PubMed] |
| 13. | Lederman JC, Nawaz H. Toxic interaction of didanosine and acetaminophen leading to severe hepatitis and pancreatitis: a case report and review of the literature. Am J Gastroenterol. 2001;96:3474-3475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Igarashi H, Ito T, Yoshinaga M, Oono T, Sakai H, Takayanagi R. Acetaminophen-induced acute pancreatitis. A case report. JOP. 2009;10:550-553. [PubMed] |
| 15. | Fernandes R. Acute pancreatitis following paracetamol overdose. BMJ Case Rep. 2009;2009:pii: bcr08.2009.2224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Jinnur P, Vasudevan V, Ali R, Arjomand F, Tiwary T, Vanam V, Abbas Q. A rare case of acetaminophen induced acute pancreatitis, ARDS, and anion gap metabolic acidosis. Chest. 2012;142:309A-309C. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Cavanaugh Z, Naut ER. Acetaminophen-induced pancreatic pseudocyst: first case report. Conn Med. 2014;78:37-39. [PubMed] |
| 18. | Kim YK, Kim CS, Han YM. Role of fat-suppressed t1-weighted magnetic resonance imaging in predicting severity and prognosis of acute pancreatitis: an intraindividual comparison with multidetector computed tomography. J Comput Assist Tomogr. 2009;33:651-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 19. | Robinson PJ, Sheridan MB. Pancreatitis: computed tomography and magnetic resonance imaging. Eur Radiol. 2000;10:401-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 63] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Hodgman MJ, Garrard AR. A review of acetaminophen poisoning. Crit Care Clin. 2012;28:499-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 190] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 21. | Tylenol [package insert]. Washington, DC: McNeil Consumer Healthcare, Division of McNEIL-PPC, Inc; 2010. . |
| 22. | Chen SJ, Lin CS, Hsu CW, Lin CL, Kao CH. Acetaminophen Poisoning and Risk of Acute Pancreatitis: A Population-Based Cohort Study. Medicine (Baltimore). 2015;94:e1195. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Schmidt LE, Dalhoff K. Hyperamylasaemia and acute pancreatitis in paracetamol poisoning. Aliment Pharmacol Ther. 2004;20:173-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |