Published online Jan 16, 2016. doi: 10.12998/wjcc.v4.i1.30
Peer-review started: May 8, 2015
First decision: July 26, 2015
Revised: August 26, 2015
Accepted: November 3, 2015
Article in press: November 4, 2015
Published online: January 16, 2016
Processing time: 253 Days and 8.3 Hours
We would like offering our experience about a very rare and underestimated type of gastrointestinal lipoma, which is the lipoma with precancerous or frankly malignant features of the mucosal epithelium, the so-called atypical lipoma. So far, only few cases have been described in the world literature. Recently, we grappled with what we think the first case of atypical colonic lipoma presenting with adenocarcinomatous transformation of the overlying epithelium, as discussed in more detail below. We propose a new definition and classification for this kind of lesions and discuss about their diagnosis, treatment and prognosis.
Core tip: We report a case of atypical lipoma of the colon with malignant transformation of the mucosal epithelium. No standardized treatment exists. Endoscopic resection with close follow-up is probably the most appropriate management to pursue for this kind of lesions.
- Citation: Virgilio E, Mercantini P, Cavallini M. Is endoscopic resection a correct treatment for atypical gastrointestinal lipomas? World J Clin Cases 2016; 4(1): 30-32
- URL: https://www.wjgnet.com/2307-8960/full/v4/i1/30.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i1.30
We read with great interest the article written by Yeom et al[1] on an unusual case of lipoma of the right colon covered by hyperplastic epithelium. As for us, we would like to offer our experience about another very rare type of gastrointestinal lipoma, which is the lipoma covered with precancerous or frankly malignant features of the overlying epithelium, the so-called atypical lipoma. Recently, in fact, we grappled with what we think the first case of colonic lipoma with malignant transformation of the mucosal epithelium, as discussed in more detail below.
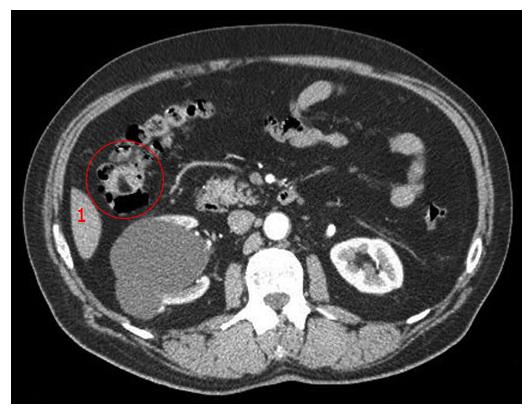
A 64-year-old man was referred to us for surgical evaluation of an ulcerated mass of the right colic flexure measuring 3.5 cm in diameter (Figure 1); preoperative biopsies showed both tubule-villous adenoma with focal severe dysplasia and abundant granulation tissue. We performed a right hemicolectomy; histology yielded the unsuspected diagnosis of well-differentiated colonic lipoma with an ulcerated overlying mucosa and 22 reactive lymph nodes. Follow-up is now 8 mo with no evidence of recurrence.
Colonic lipoma is a benign tumor well-known from the literature[2,3]. However, its oncological significance is not so simple as generally argued. The term “atypical” was introduced by Snover[4] in 1984 and has always been referred to those lipomas showing cytological alterations in fat cells (hyperchromasia, pleomorphism and mitosis) suggestive of sarcomatous changes. However, what appears to us still underestimated is the fact that atypical lipomas have a double malignant potential represented not only by liposarcoma (as assessed by Snover), but also adenocarcinoma. The former represents the direct malignant counterpart deriving from the same mesenchymal cell line whereas the latter affects a different layer, the epithelium of the overlying mucosa. In this viewpoint, the term “atypical” should be extended to include those lesions with hyperplastic, precancerous or frankly malignant features of the covering epithelium. Hence, we propose a classification of atypical lipomas: Atypical type-A lipoma could indicate the original lipomatous alterations described by Snover, type-B those lesions with mucosal changes and type-C the lipomas presenting alterations in both components. According to this three-tier classification system, atypical type-A lesions are somewhat uncommon, type-B lipomas have been reported 6 times and type-C lesions only 2 times[1,3-6]. In atypical lipomas, mucosal hyperplasia and hyperplastic polyps are secondary to ischemia and inflammation; furthermore, polyps may develop adenocarcinomas. In such cases, endoscopic ultrasound can help achieve the diagnosis of atypical lipoma saving the patient from the risk and complications of major surgery[3,5]. Actually, preoperative diagnosis of colonic lipoma (typical or not) is rarely obtained by endoscopic biopsy: Since lipomas are located in the inner layers of colonic wall (90% of cases in submucosa, 10% in subserosa, less than 1% in muscularis propria), most times biopsies result non-contributory as they cannot get the adipose tissue lying beneath the lamina propria[1]. Furthermore, they should not be performed for oozing lesions. On the other hand, they can discover the epithelial benign and malignant changes occurring in the overlying mucosa[1,3,5]. Biopsy can also take part in the so-called “self-amputation” of colonic lipomas: When the overlying mucosa of a large lipoma becomes damaged due to biopsy, enucleation can occur through the ulcerated region and the lesion can be expelled naturally from the rectum. This unusual presentation was first described in 1940 and only 20 cases have been reported so far[7]. Recently, resorting to the same principle, Soares and colleagues successfully treated a large colonic lipoma through an endoscopic unroofing technique[8]. As for treatment, there is general consensus that small (< 2 cm) asymptomatic colonic lipomas do not need any intervention as they show no significant risk of malignant degeneration[2-4]. However, in the light of our experience, we think such lesions do possess a malignant potential and prophylactic endoscopic removal is probably the most correct management to pursue.
P- Reviewer: Kim BW
S- Editor: Song XX L- Editor: A E- Editor: Li D
| 1. | Yeom JO, Kim SY, Jang EC, Yu JY, Chang ED, Cho YS. Colonic lipoma covered by hyperplastic epithelium: Case report. World J Clin Cases. 2013;1:124-127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Kosaka R, Noda T, Tsuboi J, Tanaka K. Successful endoscopic removal of a large colonic lipoma causing intussusception. Endoscopy. 2014;46 Suppl 1 UCTN:E551-E552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Radhi JM, Haig TH. Lipoma of the colon with overlying hyperplastic epithelium. Can J Gastroenterol. 1997;11:694-695. [PubMed] |
| 4. | Snover DC. Atypical lipomas of the colon. Report of two cases with pseudomalignant features. Dis Colon Rectum. 1984;27:485-488. [PubMed] |
| 5. | Vasiliadis K, Katsamakas M, Nikolaidou A, Christoforidis E, Tsalis K, Tsalikidis A. Submucosal lipoma of the ascending colon as a source of massive lower gastro-intestinal bleeding: a case report. Acta Chir Belg. 2008;108:356-359. [PubMed] |
| 6. | Adachi S, Hamano R, Shibata K, Yoshida S, Tateishi H, Kobayashi T, Hanada M. Colonic lipoma with florid vascular proliferation and nodule-aggregating appearance related to repeated intussusception. Pathol Int. 2005;55:160-164. [PubMed] |
| 7. | Kouritas VK, Baloyiannis I, Koukoulis G, Mamaloudis I, Zacharoulis D, Efthimiou M. Spontaneous expulsion from rectum: a rare presentation of intestinal lipomas. World J Emerg Surg. 2011;6:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Soares JB, Gonçalves R, Rolanda C. Endoscopic resection of a large colonic lipoma by unroofing technique. Endoscopy. 2011;43 Suppl 2 UCTN:E407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |