Published online Aug 16, 2015. doi: 10.12998/wjcc.v3.i8.751
Peer-review started: April 8, 2015
First decision: April 27, 2015
Revised: June 3, 2015
Accepted: June 18, 2015
Article in press: July 15, 2015
Published online: August 16, 2015
Processing time: 43 Days and 14.9 Hours
Cleidocranial dysplasia (CD) is an autosomal dominant syndrome which is characterized by several skeletal malformations such as non-closed fontanelles, skeletal abnormalities of the maxilla and mandible and absence of clavicles. Mid-facial hypoplasia and mandibular prognathism are mostly seen jaw abnormalities in CD. In this study, the combined orthodontic-surgical treatment of a patient with CD with class III malocclusion and multiple unerupted primary and deciduous teeth is presented.
Core tip: Cleidocranial dysplasia is a syndromic disease with distinct craniofacial and maxillofacial manifestations. The satisfactory treatment of dental and skeletal deformities in this disease can only be possible with combined orthodontic-surgical approach.
- Citation: Çimen E, Dereci &, Tüzüner-Öncül AM, Yazıcıoğlu D, Özdiler E, Şenol A, Sayan NB. Combined surgical-orthodontic rehabilitation of cleidocranial dysplasia: 5 years follow-up. World J Clin Cases 2015; 3(8): 751-756
- URL: https://www.wjgnet.com/2307-8960/full/v3/i8/751.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i8.751
Cleidocranial dysplasia (CD) is a syndromic disease which is also known as cleidocranial dysostosis or Marie-Sainton disease[1]. It is characterized by multiple or solitary supernumerary teeth, non-closed fontanelles, skeletal abnormalities of the maxilla and mandible, absence of clavicles, presence of open skull sutures, widening of pubic symphysis, multiple impacted permanent teeth and miscellaneous skeletal changes[2,3]. Mutations of the transcription factor RUNX2 which is one of the major regulators of bone maturation, are responsible for the occurrence of CD[2].
A multidiscipliner team approach is needed to overcome the dental abnormalities and facial deformities which are well-known complications that cause morbidity in CD patients. Combined treatment with orthognathic surgery and orthodontic therapy is the mostly-accepted treatment modality to correct mid-face hypoplasia and Class III malocclusion in the treatment of CD patients.
In this study, the combined orthodontic-surgical treatment of a CD patient with class III malocclusion and multiple impacted permanent teeth is presented.
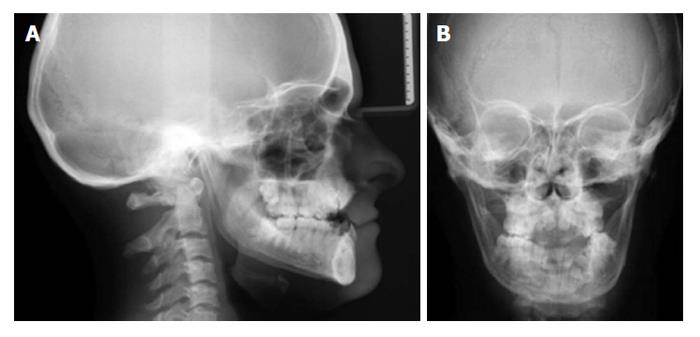
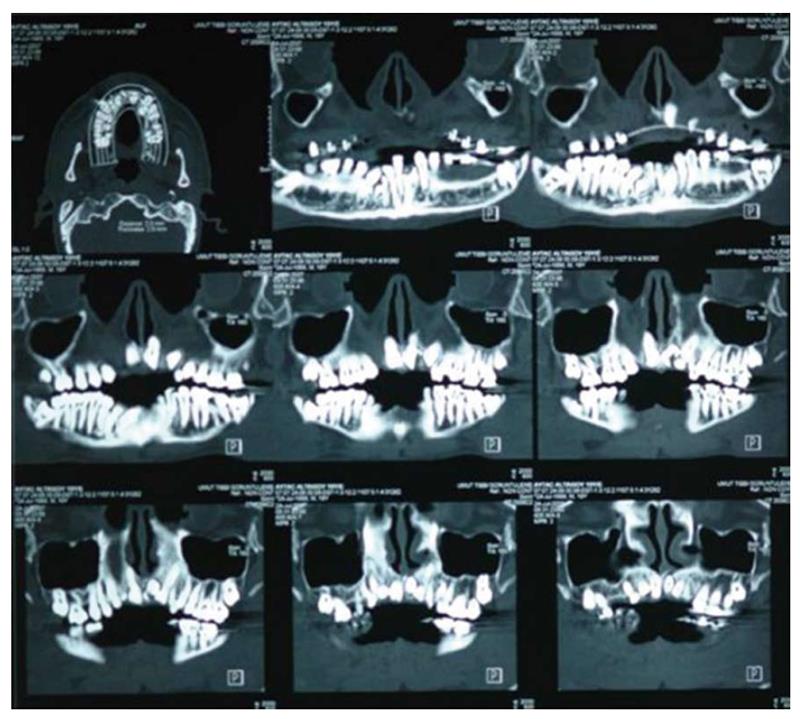
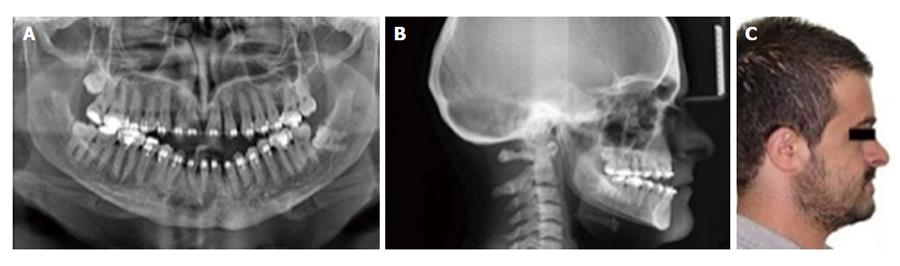
Eighteen years old male with CD was referred to the department of orthodontics with complaints of ineffective chewing, biting and facial asymmetry (Figure 1). Orthopantogram, lateral cephalometric radiograph and antero-posterior radiograph were obtained for examination of skeletal and dental abnormalities (Figures 2 and 3). A diagosis of class III, division 1 malocclusion was made and cone beam computerized tomography (CBCT) was taken to decide the exact shapes and positions of impacted teeth (Figure 4). Multiple permanent and 3 supernumerary impacted teeth were detected in CBCT sections and after orthognatic and surgical consultation, it was decided to erupt the impacted teeth and perform bimaxillary surgery to correct skeletal deformity.
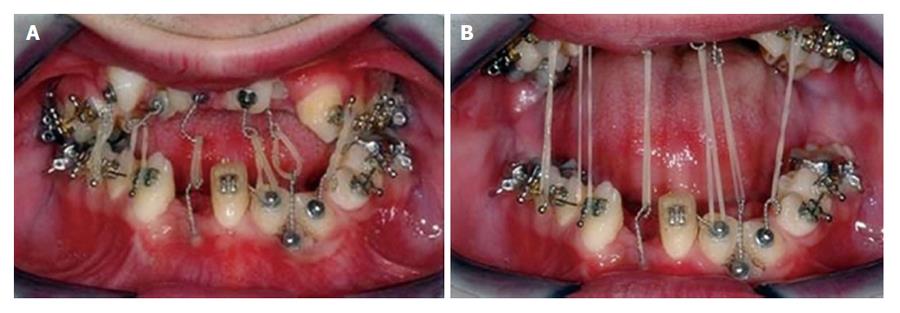
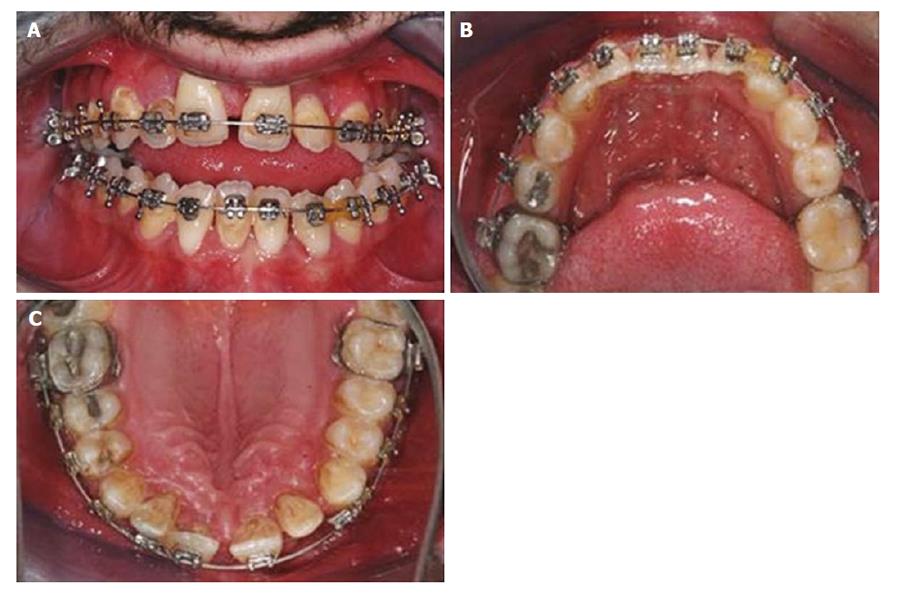
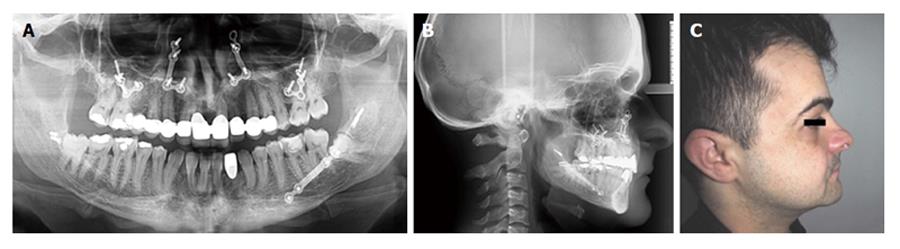
The teeth 42, 31, 32, 33, 13, 12, 11, 21, 22, 23 were surgically exposed and orthodontic buttons were bonded for orthodontic traction under general anesthesia. Three impacted supernumerary teeth were extracted at the time of the exposure of permanent teeth. Missing teeth of the dentition were erupted in 10 mo (Figure 5). After eruption, orthodontic treatment was sustained and the alignment of dental arch was rendered at the end of 12 mo (Figures 6 and 7).
Bimaxillary orthognathic surgery was planned for correction of skeletal open-bite and class III malocclusion. Patient was operated in general anesthesia. Post-operative recovery was non-eventful. Clinical outcome after surgery was satisfying according to the clinical point of view. Patient was undertaken in follow-up period with 6-mo intervals. Facial profile and occlusal appearance were normal and unchanged in 5th year follow-up control (Figure 8).
CD is associated with several heterogenous mutations in RUNX2 which is an osteoblast-specific transcription factor and also takes role in the tooth development[4]. The role of RUNX2 in tooth development partly accounts for dental abnormalities such as impacted permanent or supernumerary teeth[1]. However, the abnormal impaction of permanent and supernumerary teeth could not be fully explained since 40% of the CD cases do not have any apparent genetic mutation[2,5]. Most of CD patients are reported to have open sagittal sutures or fontanelles, multiple erupted or impacted supernumerary or primary teeth[5]. These symptoms are considered pathognomonic in the diagnosis of CD[2].
The treatment of CD varies due to the skeletal or dental abnormalities and the condition of impacted normal or supernumerary teeth. Daskalogiannakis et al[6] suggested that appropriate treatment of CD should be planned with careful consideration of age of the patient, expected duration of the treatment and patient expectation from the treatment. Dental management in CD is challenging in most cases and aims to achieve functional and esthetic results. Dental prosthesis is frequently used method for the functional rehabilitation of CD patients. With increasing attention to craniofacial anomalies in syndromic patients lately, collaborative orthodontic-surgical treatment of dental and skeletal anomalies of the jaws is suggested[6,7]. Several combined treatment regimens were proposed according to the timing and manner of approach to the impacted permanent teeth[8-12]. In our study, a technique similar to the Belfast-Hamburg[10,12] approach is applied to facilitate the eruption of impacted permanent teeth.
The traction of impacted teeth with elastics is a common method that is used in contemporary orthodontics, especially in syndromic cases such as CD. After surgical exposure of impacted or partially impacted tooth, a button or bracket is bonded and elastics are applied between impacted and opposing permanent erupted teeth[10,11]. If there are no opposing teeth or permanent erupted teeth are not suitable for traction, titanium screws may be used as anchorage for the application of traction elastics[13]. Rocha et al[14] suggested the use of a removable partial prosthesis to apply traction forces. In the current case, elastics were applied between lower and upper surgically exposed unerupted incisors and canines. The impacted teeth behaved as self-anchorage systems and full eruption of all impacted teeth were facilitated.
CD patients mostly have skeletal deformations leading to postural deformities. It is suggested that skeletal morphology may have a role in the development of temporomandibular joint (TMJ) disorders[15]. CD patients have jaw deformities and thus, tend to develop TMJ disorders. Physiotherapy or splint therapy is indicated in CD patients with TMJ disorders. The patient in the current study did not suffered from any myofacial pain or TMJ disorders and did not need any treatment on this matter.
CD is a syndromic disease with a prevalance of 1/1000000[16]. Dental manifestations of the disease is well-documented in the literature. Treatment planning in the rehabilitation of CD patients varies according to the degree of dental malocclusion, number of missing teeth and patients’ expectations. The maintenance of force-aligned permanent teeth with elastic traction is also an important matter if the alignment of dental arches are provided with orthodontic treatment. Patients who are treated with combined surgical-orthodontic treatment should be monitored with continuous follow-up periods during early adulthood as in the current case.
This study was presented as poster presentation in 20th. International Congress of Oral and Maxillofacial Surgery, Santiago, Chile.
Cleidocranial dysplasia (CD) is a rare, dominantly inherited autosomal disease.
The main symptoms of CD includes hypoplastic or aplastic clavicles, supernumerary teeth, delayed eruption, impaction of permanent dentition and morphologic abnormalities of the maxilla and mandible.
The differential diagnosis includes Crane-Heise syndrome, mandibuloacral dysplasia and pycnodysostosis.
Laboratory testing methods are not needed in the diagnosis of CD.
Multiple impacted permanent or supernumerary teeth are detected in panoromic radiography or cone-beam computerized tomography sections of patients with CD.
Pathological examination is not needed in the diagnosis of CD.
The treatment of CD includes orthodontics, orthognathic surgery or combined treatment modalities.
The treatment of CD should be handled in a multidisciplinary basis. Follow-up is crucial after combined orthodontic-surgical therapy of cleidocranial dysplasia.
It is a well-written manuscript about a rare case.
P- Reviewer: Hernandez-Sanchez S, Saedi B S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Park TK, Vargervik K, Oberoi S. Orthodontic and surgical management of cleidocranial dysplasia. Korean J Orthod. 2013;43:248-260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 2. | Mundlos S. Cleidocranial dysplasia: clinical and molecular genetics. J Med Genet. 1999;36:177-182. [PubMed] |
| 3. | Ishii K, Nielsen IL, Vargervik K. Characteristics of jaw growth in cleidocranial dysplasia. Cleft Palate Craniofac J. 1998;35:161-166. [PubMed] |
| 4. | Yamashiro T, Aberg T, Levanon D, Groner Y, Thesleff I. Expression of Runx1, -2 and -3 during tooth, palate and craniofacial bone development. Mech Dev. 2002;119 Suppl 1:S107-S110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 66] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 5. | Tanaka JL, Ono E, Filho EM, Castilho JC, Moraes LC, Moraes ME. Cleidocranial dysplasia: importance of radiographic images in diagnosis of the condition. J Oral Sci. 2006;48:161-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Daskalogiannakis J, Piedade L, Lindholm TC, Sándor GK, Carmichael RP. Cleidocranial dysplasia: 2 generations of management. J Can Dent Assoc. 2006;72:337-342. [PubMed] |
| 7. | Becker A, Shteyer A, Bimstein E, Lustmann J. Cleidocranial dysplasia: Part 2--Treatment protocol for the orthodontic and surgical modality. Am J Orthod Dentofacial Orthop. 1997;111:173-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 43] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Smylski PT, Woodside DG, Harnett BE. Surgical and orthodontic treatment of cleidocranial dysostosis. Int J Oral Surg. 1974;3:380-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 23] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Hall RK, Hyland AL. Combined surgical and orthodontic management of the oral abnormalities in children with cleidocranial dysplasia. Int J Oral Surg. 1978;7:267-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Behlfelt K. Cleidocranial dysplasia: diagnosis and treatment concept. Trans Eur Orthod Soc. 1987;63:25. |
| 11. | Richardson A, Swinson T. Combined orthodontic and surgical approach to cleidocranial dysostosis. Trans Eur Ortod Soc. 1987;63:23. |
| 12. | Kelly E, Nakamoto RY. Cleidocranial dysostosis--a prosthodontic problem. J Prosthet Dent. 1974;31:518-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Kuroda S, Yanagita T, Kyung HM, Takano-Yamamoto T. Titanium screw anchorage for traction of many impacted teeth in a patient with cleidocranial dysplasia. Am J Orthod Dentofacial Orthop. 2007;131:666-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Rocha R, Zasso MB, Floriano G, Derech C, Ribeiro GU, Locks A, Ritter D. Orthodontic traction in a patient with cleidocranial dysplasia: 3 years of follow-up. Am J Orthod Dentofacial Orthop. 2014;146:108-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Kobayashi T, Honma K, Izumi K, Hayashi T, Shingaki S, Nakajima T. Temporomandibular joint symptoms and disc displacement in patients with mandibular prognathism. Br J Oral Maxillofac Surg. 1999;37:455-458. [PubMed] |
| 16. | Mahajan PS, Mahajan AP, Mahajan PS. A rare case of cleidocranial dysplasia presenting with failure to thrive. J Nat Sci Biol Med. 2015;6:232-235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |