Published online Jan 16, 2014. doi: 10.12998/wjcc.v2.i1.1
Revised: December 21, 2013
Accepted: January 6, 2014
Published online: January 16, 2014
Processing time: 112 Days and 19.9 Hours
To report the first case of dellen-like keratopathy with superior corneal thinning associated with implantation of glaucoma drainage devices. A 70-year-old male with a history of primary open angle glaucoma and dry eye disease underwent placement of glaucoma drainage devices with antimetabolite application in both eyes. Prior to placement, minimal refractive error was noted on manifest refraction. Several years later, the patient was referred for decreased vision and corneal irregularity. Examination showed pathologic corneal curvature, superior corneal thinning, and epithelial demarcation lines immediately anterior to the glaucoma drainage devices in both eyes. The epithelium remained intact with no evidence of limbal stem cell deficiency. Manifest refraction revealed a large change in both eyes. Topography was used to confirm the presence of irregular corneal curvature anterior to the glaucoma drainage devices. Dellen-like keratopathy with superior thinning is a rare sequela after implantation of a glaucoma drainage device that must be considered in elderly patients who undergo glaucoma surgery. It is likely related to a combination of tear film alteration related to previously large anterior blebs, antimetabolite application, and aqueous humor flow patterns around the drainage devices. Treatment should focus on lubrication.
Core tip: Corneal abnormalities are not uncommon findings in patients with longstanding glaucoma. Topical medication-related and antimetabolite-related keratopathies are conditions that have been well documented. This case report identifies an entity related to glaucoma drainage devices. Dellen-like keratopathy is a condition similar in appearance to that of a delle, but larger in size. Early identification is important in preventing excessive corneal thinning and irregular corneal curvature.
- Citation: Fenzl CR, Moshirfar M, Gess AJ, Muthappan V, Goldsmith J. Dellen-like keratopathy associated with glaucoma drainage devices. World J Clin Cases 2014; 2(1): 1-4
- URL: https://www.wjgnet.com/2307-8960/full/v2/i1/1.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i1.1
Dellen keratopathy is characterized by localized thinning and dryness in the cornea. It often develops adjacent to areas of ocular surface changes and elevation, such as pterygia. Chronic dellen formation can lead to diffuse thinning. This is the first reported case of delle-like keratopathy with superior corneal thinning resulting from the implantation of glaucoma drainage devices.
A 70-year-old male was referred by his glaucoma specialist for gradual worsening of vision in both eyes. The patient had a history of primary open angle glaucoma for ten years for which he underwent multiple surgeries. He also suffered from moderate dry eye disease for which he was being treated with frequent topical lubrication. The right eye had placement of ExPRESS shunt (Alcon Laboratories, Fort Worth, TX) with use of mitomycin-C (MMC), which required two subsequent revisions in the right eye, both of which also used MMC. The left eye underwent a trabeculectomy with MMC, followed by Ahmed tube shunt (New World Medical, Rancho Cucamonga, CA). The patient was also pseudophakic in both eyes and denied any history of refractive surgery, excessive eye rubbing, bleb massage, and collagen vascular disease.
Eleven months prior to presentation he had stable best corrected visual acuity of 20/40 in the right eye and 20/50 in the left eye. Manifest refraction was -1.25 + 1.50 × 010 and -0.75 + 0.75 × 080 respectively.
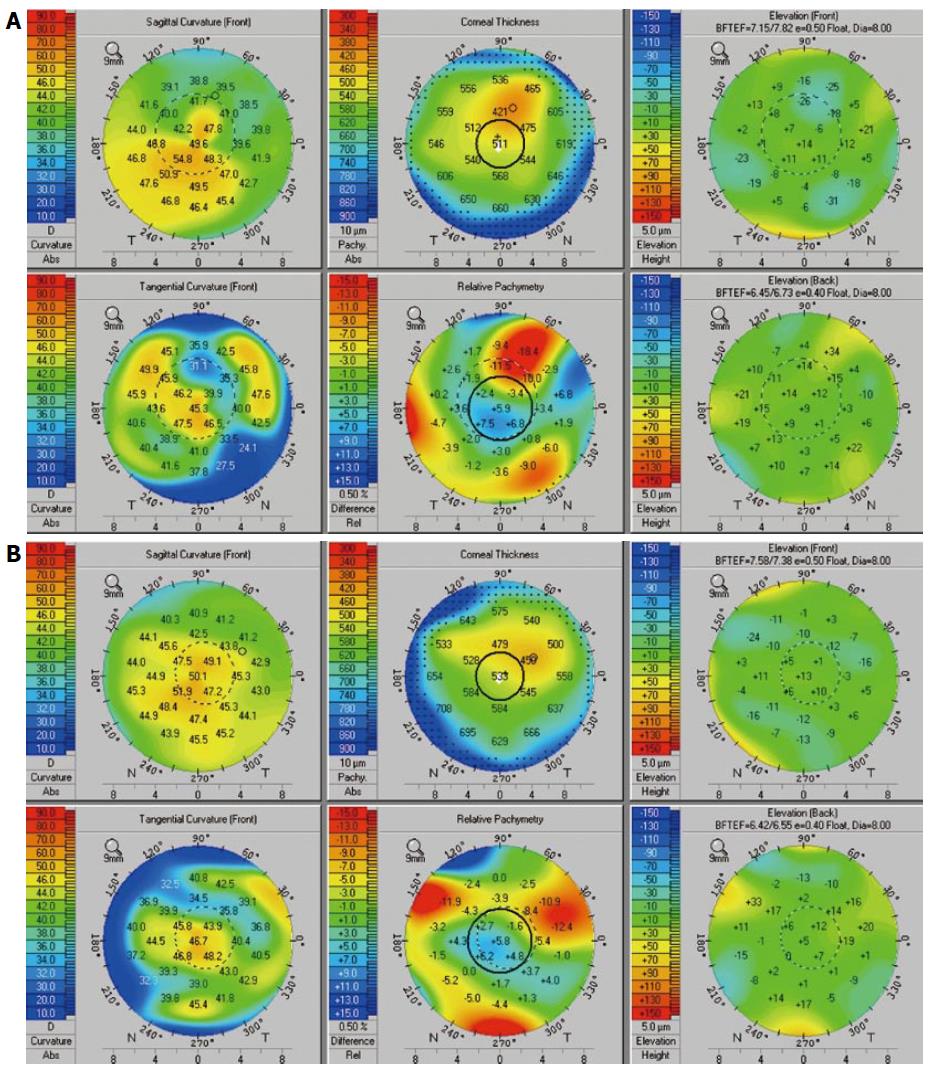
At the time of presentation, the patient was being treated with brinzolamide twice daily, brimonidine/timolol combination twice daily, latanoprost once daily, and preservative free artificial tears three times per hour in both eyes. The patient’s best-corrected visual acuity was 20/70 in the right eye and 20/100 in the left eye with significantly increased astigmatism on manifest refraction: -6.25 + 7.75 × 060 in the right eye and +2.25 + 2.50 × 047 in the left eye. Intraocular pressure was 34 mmHg in the right eye and 18 mmHg in the left eye. Central corneal thickness was 511 microns in the right eye and 533 microns in the left eye.
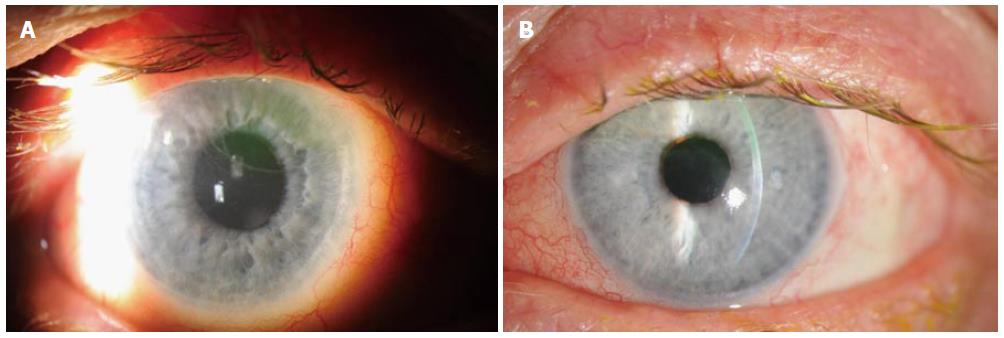
Externally, no eyelid pathology was present. Anterior segment examination revealed thinning of the superior one-third of the corneal stroma with a clear epithelial demarcation line in each eye (Figure 1). The epithelium was intact bilaterally. A slight elevation of the conjunctiva was present posterior to the limbus in each eye, but no perilimbal bleb was identified. The glaucoma drainage device tubes inside each anterior chamber were in appropriate posterior position with no corneal contact. Topographic analysis with Pentacam (Optikgerate GmbH, Wetzlar, Germany) revealed diffuse corneal thinning as well as irregular corneal curvatures adjacent to the glaucoma drainage devices. At the thinnest point, the right cornea was 421 microns and the left cornea was 450 microns (Figure 2).
Corneal dellen are localized areas of drying and thinning in the peripheral cornea, usually adjacent to an area of ocular surface abnormality. With chronic dellen, a keratopathy mimicking ectasia can occur with a combination of drying, thinning, and a reduced corneal tensile strength.
Keratopathy resulting from glaucoma surgery is exceedingly rare. To our knowledge, only two cases of keratopathy after glaucoma surgery have been documented in the literature, both following trabeculectomy (there are no reported cases after tube shunt surgery). One reported case utilized MMC[1] and the other used 5-Fluorouracil (5-FU)[2]. In one bilateral case of superior corneal changes observed 15 years after surgery, the cause was thought to be due to either bleb compression from prominent avascular blebs or chronic corneal toxicity from MMC application[1]. The other case of keratopathy following trabeculectomy was attributed to excessive eye rubbing[2].
MMC and 5-FU have long been used adjunctively in trabeculectomy to improve surgical outcomes. Resultant epitheliopathy is common due to the effect of antimetabolites on actively replicating tissue[3], and effects are seen well beyond the time of surgery[4]. Stromal keratocytes are also affected by antimetabolite medications; in an in vitro human cornea model, Rajan et al[5] documented a significant delay in keratocyte repopulation as well as decreased anterior stromal thickness four weeks after photorefractive keratectomy combined with MMC.
In our patient, thinning and significant alteration in the corneal curvature were present in a location immediately anterior to each drainage device. Given this patient’s history of multiple glaucoma surgeries, it is likely that dellen formed at some stage in each eye. This may have been the result of previously large, anterior blebs causing tear film alteration[6]. In the left eye, a tissue allograft placed adjacent to the limbus during the Ahmed valve placement may have provided a nidus for delle formation. The antimetabolite use during these surgeries may have accelerated this process. It is also possible that the fluid dynamics of the aqueous humor at the opening of the drainage device may play a role in inducing thinning superiorly through low grade inflammation that may impair normal corneal healing, repair, and maintenance functions. Retrograde flow of inflammatory cells has also been postulated as a source of corneal complications[7], and focal endothelial irregularities related to drainage devices have been reported[8].
A combination of chronic dellen formation and low grade inflammation in the posterior cornea likely led to the diffuse superior corneal thinning and resultant astigmatism in this patient. We term this a dellen-like keratopathy, rather than a dellen keratopathy, due to the diffuse nature of the thinning that covered nearly 50% of the superior cornea and encroached into the visual axis, mimicking a superior keratoconus. To the patient, we recommended continued use of frequent lubrication and fitting for rigid gas-permeable contact lenses to maximize his visual potential. He has not followed up with us since his initial visit.
This is the first reported case of dellen-like keratopathy, a rare but serious complication of glaucoma surgery. Keratopathy resulting directly from device placement cannot be proven, and is likely multifactorial. The focal thinning immediately adjacent to both drainage devices suggests a causal relationship. Glaucoma and cornea specialists should be aware of this possibility in patients presenting with worsening vision and corneal changes after glaucoma surgery.
The main symptom was blurry vision.
The main clinical findings include corneal thinning, epithelial demarcation lines, and pathologic corneal curvature.
The differential diagnosis focuses on potential causes of corneal thinning and change in corneal curvature including dellen-like phenomena, antimetabolite complications, and aqueous humor fluid dynamics at the opening of the drainage devices.
No laboratory testing was performed.
Imaging revealed dramatic change in refraction as well as irregular corneal curvature identified by topography.
No specimens were obtained for pathology.
Treatment includes frequent lubrication and gas-permeable contact lenses.
Similar reports are included as references one and two.
A delle is an area of localized thinning and dryness of the cornea adjacent to an elevated area.
Dellen-like areas of corneal thinning can occur anterior to glaucoma drainage implants and should be treated in a similar manner as dellen.
Strengths include evidence of change in manifest refraction as well as significant corneal curvature abnormalities on topographic imaging.
P- Reviewers: Ghaffarieh A, Jhanji V, Shih YF S- Editor: Cui XM L- Editor: A E- Editor: Wang CH
| 1. | Lin CP, Liu YT, Chen CW. Corneal ectasia after trabeculectomy with mitomycin C application. Br J Ophthalmol. 1999;83:629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (1)] |
| 2. | Baldassare RD, Brunette I, Desjardins DC, Amyot M. Corneal ectasia secondary to excessive ocular massage following trabeculectomy with 5-fluorouracil. Can J Ophthalmol. 1996;31:252-254. [PubMed] |
| 3. | Yoon PS, Singh K. Update on antifibrotic use in glaucoma surgery, including use in trabeculectomy and glaucoma drainage implants and combined cataract and glaucoma surgery. Curr Opin Ophthalmol. 2004;15:141-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 2.4] [Reference Citation Analysis (1)] |
| 4. | Tanihara H, Yokoi N, Komuro A, Honda Y, Kinoshita S. Prolonged impairment of peripheral corneal epithelium barrier function after successful trabeculectomy. Am J Ophthalmol. 1997;123:487-493. [PubMed] |
| 5. | Rajan MS, O’Brart DP, Patmore A, Marshall J. Cellular effects of mitomycin-C on human corneas after photorefractive keratectomy. J Cataract Refract Surg. 2006;32:1741-1747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Soong HK, Quigley HA. Dellen associated with filtering blebs. Arch Ophthalmol. 1983;101:385-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Topouzis F, Coleman AL, Choplin N, Bethlem MM, Hill R, Yu F, Panek WC, Wilson MR. Follow-up of the original cohort with the Ahmed glaucoma valve implant. Am J Ophthalmol. 1999;128:198-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 192] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 8. | Kim CS, Yim JH, Lee EK, Lee NH. Changes in corneal endothelial cell density and morphology after Ahmed glaucoma valve implantation during the first year of follow up. Clin Experiment Ophthalmol. 2008;36:142-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 89] [Article Influence: 5.2] [Reference Citation Analysis (0)] |