Published online Sep 16, 2025. doi: 10.12998/wjcc.v13.i26.108409
Revised: May 18, 2025
Accepted: June 13, 2025
Published online: September 16, 2025
Processing time: 100 Days and 24 Hours
Conjunctival plasmacytoma is an exceedingly uncommon form of extramedullary manifestation of multiple myeloma, with only a handful of cases reported so far.
A 66-year-old male of Indian origin with multiple myeloma presented with a 1-year history of progressive pink mass associated with itching in his left eye. Examination revealed a pinkish conjunctival mass with telangiectasia extending up to the temporal limbus, mimicking ocular surface squamous neoplasia. The patient underwent successful excision of the mass and amniotic membrane grafting. Histopathological examination after excision revealed plasma cell infiltration, confirming an unusual extramedullary manifestation of multiple myeloma. The patient was followed up for one year, with no evidence of recurrence.
This case report highlights the importance of considering multiple myeloma in the differential diagnosis of ocular masses, particularly in patients with a known history of the disease. The presentation of a conjunctival mass in a patient with multiple myeloma is rare, but it is essential to recognize this possibility to ensure timely and appropriate management.
Core Tip: Conjunctival plasmacytoma is a rare extra medullary manifestation of multiple myeloma that can clinically mimic ocular surface squamous neoplasia. This case highlights the importance of including multiple myeloma in the differential diagnosis of atypical conjunctival masses, especially in patients with a known history of the disease, to enable accurate diagnosis and timely intervention.
- Citation: Koppalu Lingaraju T, Panda BB, Sethy M, Achanta SL. Solitary extramedullary plasmacytoma mimicking ocular surface squamous neoplasia in an elderly male: A case report. World J Clin Cases 2025; 13(26): 108409
- URL: https://www.wjgnet.com/2307-8960/full/v13/i26/108409.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i26.108409
Multiple myeloma is a hematological malignancy characterized by clonal proliferation of plasma cells in the bone marrow. It accounts for approximately 10% of hematological malignancies[1]. Extramedullary involvement is rare in patients, with newly diagnosed multiple myeloma incidence ranging from 0.5% to 4.8%, while in relapsed and refractory multiple myeloma the reported incidence is 3.4% to 14%[2], and ocular manifestations are even more uncommon, reported cases include conjunctival masses, orbital involvement[3], retinal abnormalities, optic neuropathy and uveitis[4].
A 66-year-old elderly Indian male presented with a pink mass in the conjunctiva of the left eye for one-year duration.
The patient presented with a one-year history of an insidious onset, gradually progressive, painless, pink colour mass in the left eye, associated with intermittent itching.
There was no history of prior ocular surgeries or trauma. He had a history of treatment for multiple myeloma (International Staging System Stage II) diagnosed three years ago and was currently on maintenance therapy with tablet Lenalidomide 10 mg once daily and injection Denosumab 120 mg twice yearly.
The patient denied any family history of malignancy.
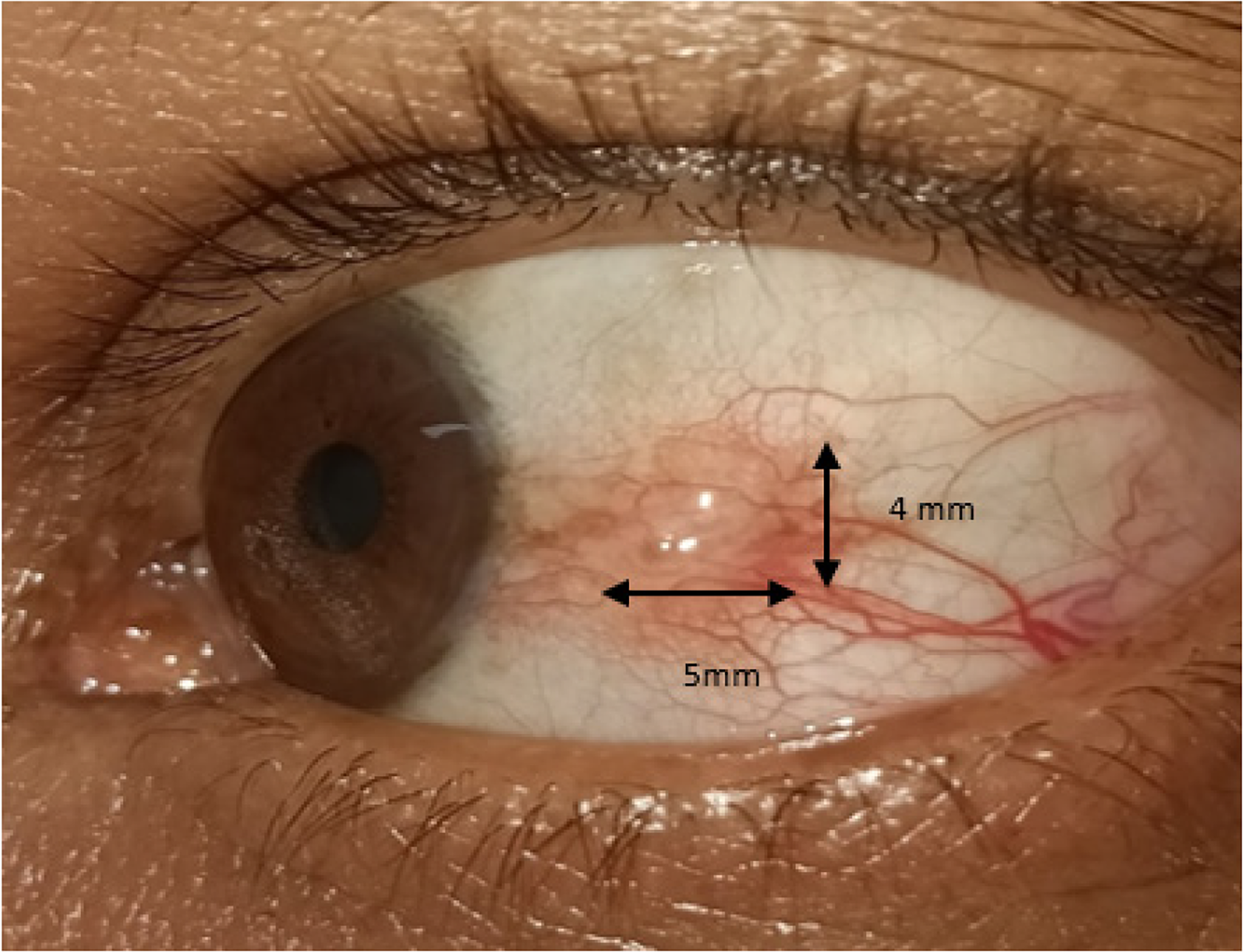
On physical examination, the vital signs were within normal limits. On ocular examination, the best corrected visual acuity in both eyes was 6/9, with a full range of extraocular movement in both eyes. Examination of the left eye revealed a pinkish conjunctival mass extending up to the temporal limbus, with nodularity and telangiectatic vessels of size 5 mm × 4 mm. The mass was painless without any evidence of suppuration or hemorrhage (Figure 1). The right eye exami
At the time of presentation at our clinic, his routine systemic workup for multiple myeloma were above the normal range i.e. Serum kappa-free light chain level was found to be 64.720 mg/L (normal range 3.3-19.4mg/L), Serum lambda free light chain level was 56.890 mg/L (normal range 5.71-26.30mg/L) however the Free Kappa: Lambda ratio 1.138 (normal range 0.26-1.65mg/L) was within normal limit. And Serum Beta 2 Microglobulin level (Nephalometry method) was found to be 3903.99 ng/mL (normal range 800-2340 ng/mL), Complete blood count revealed hemoglobin 12.4 g/dL, white blood counts count of 2.87 × 109/L and RBC count 4.18 × 1012/L. Bone Marrow Aspirate showed a bone marrow plasma cell fraction of 3%. The cytogenetic risk profile could not be done due to financial constraints.
Fluorodeoxyglucose positron emission tomography computed tomography scan showed no evidence of any lytic lesions or any extraosseous disease at the time of presentation.
Mutidisciplinary expert consultation with the pathologist and a medical oncologist was done.
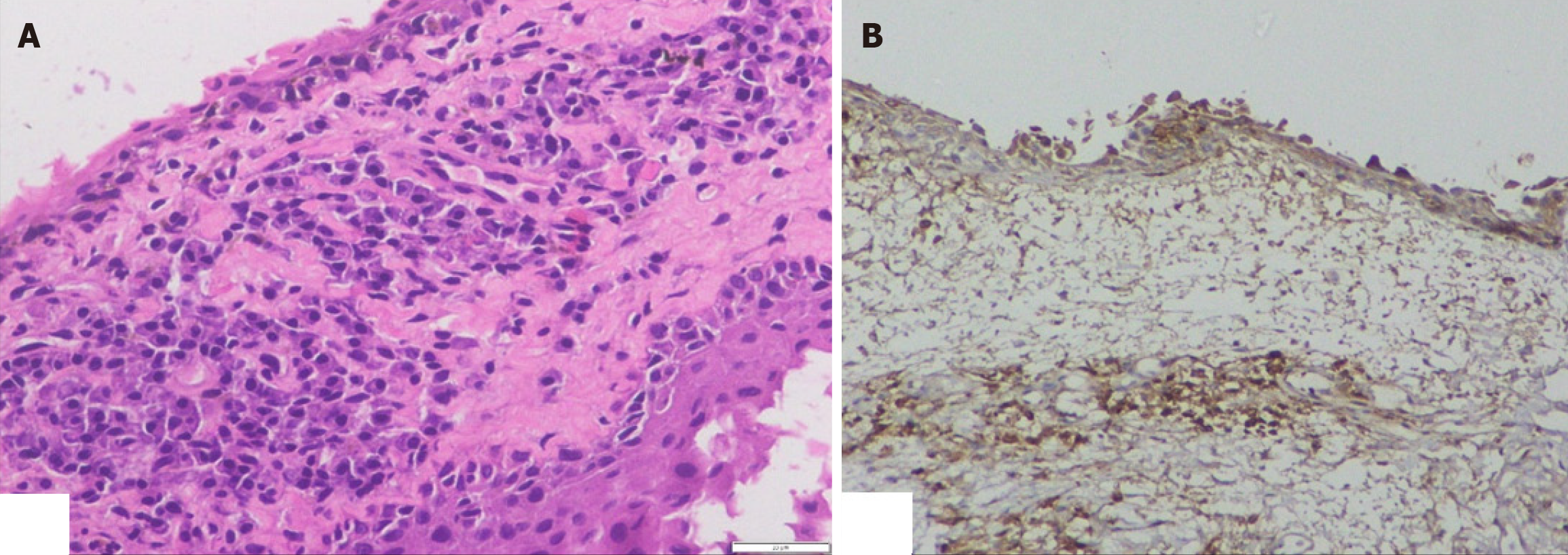
A provisional diagnosis of ocular surface squamous neoplasia was made, and the mass was planned for excision under local anesthesia with wide margins (3 mm). The excised mass was sent for frozen section biopsy. Histopathological examination revealed plasma cell infiltration (Figure 2A). Immunohistochemistry showing positive for CD 138, Kappa and Lambda (Figure 2B), thus confirming the diagnosis of conjunctival plasmacytoma.
Under local anaesthesia, the conjunctival mass was excised with a wide margin of 3 mm of uninvolved tissue. An absolute alcohol soaked swab was applied over the cornea after marking 3 mm of uninvolved margins, followed by debridement of the corneal epithelium (Kerato-epitheliectomy). The excised mass, along with the debrided corneal epithelium, was sent for frozen section examination. After margin clearance was confirmed on frozen section, a double freeze-thaw cryotherapy was applied slowly over the excised conjunctival and corneal margins. The ocular surface reconstruction was then performed with a wet amniotic membrane graft secured with 8-0 Vicryl suture and eye patching were done.
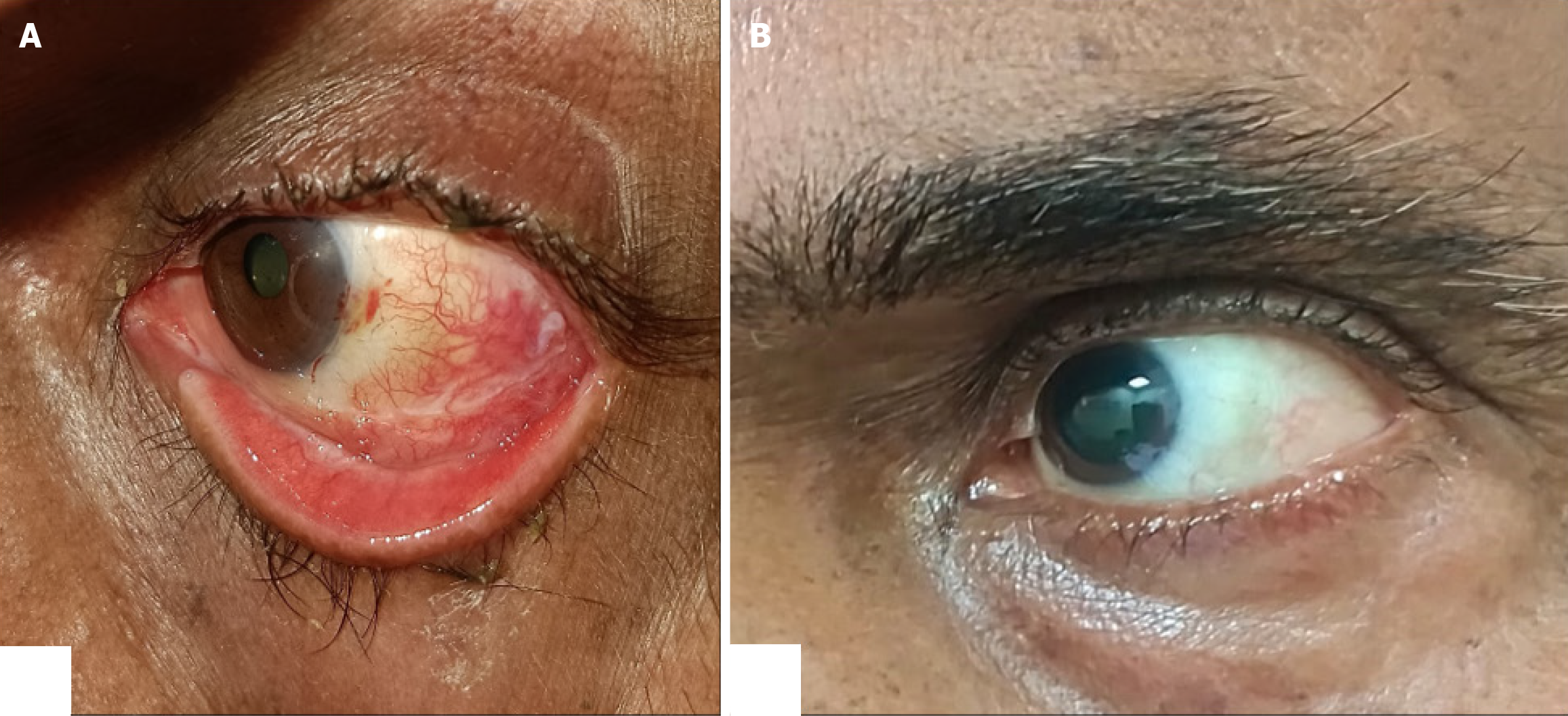
Postoperatively, he was prescribed topical Moxifloxacin+Dexamethasone, tapered over 1 month, and topical lubricant for 3 months. To prevent any recurrence, prophylactic topical chemotherapy with Mitomycin C was planned. He was prescribed to start freshly prepared topical Mitomycin C (0.04%) four times daily for 2 weeks on and 2 weeks off for three cycles. Tab Lenalidomide was continued as maintenance therapy according to the advice of the medical oncologist. Follow-up at two weeks and 6 months showed no signs of recurrence (Figure 3).
This case report presents a rare instance of an extramedullary plasmacytoma manifesting as a conjunctival mass in a patient with multiple myeloma. The occurrence of extramedullary plasmacytoma in patients with multiple myeloma is estimated to be approximately 7%-17%[5]. However, conjunctival involvement is exceedingly uncommon, with only a few reported cases in the literature[6-8]. The diagnosis of an extramedullary plasmacytoma was confirmed by histopathological examination, which revealed clonal plasma cell infiltration. Immunohistochemistry staining showed positivity for CD138, CD56, and kappa light chains[9]. Initially, the clinical appearance of the conjunctival mass was suggestive of ocular surface squamous neoplasia (OSSN), which typically presents as a gelatinous or leukoplakic lesion with irregular surfaces and raised edges. It often arises in the interpalpebral zone, with a predilection for the nasal quadrant. The lesions can be papillary, plaque-like, or nodular, and may exhibit a range of colors, including pink, red, or white[10]. OSSN is a common malignancy of the ocular surface, accounting for approximately 4%-29% of all ocular surface tumors[11].
The uniqueness in our patient was that the intraoperative frozen section and histopathological evaluation in our patient revealed a distinct plasma cell infiltrate, prompting a diagnosis of conjunctival plasmacytoma, which was later confirmed with Immunohistocytochemistry. This highlights the importance of intraoperative frozen section in guiding surgical decisions and altering the course of treatment.
Extramedullary plasmacytoma can involve various organs, with the most common sites being the lungs (30%-40%), liver (20%-30%), and kidneys (10%-20%), other less common sites of involvement include the skin (5%-10%), gastrointestinal tract (5%-10%), and central nervous system (5%).
Managing extramedullary plasmacytoma typically involves a combination of surgery, radiation therapy, and chemo
In conclusion, this case report highlights the importance of considering multiple myeloma in the differential diagnosis of ocular masses, particularly in patients with a known history of the disease. A multidisciplinary approach, including ophthalmology, medical oncology, and pathology, is essential for accurate diagnosis and effective management of such rare and complex cases. The use of intraoperative frozen section in this case was crucial, as it enabled us to differentiate the conjunctival mass from OSSN, which was our initial clinical suspicion. This timely diagnosis allowed for prompt and appropriate management, underscoring the value of intraoperative frozen section in guiding surgical decisions.
| 1. | Rajkumar SV. Multiple myeloma: 2022 update on diagnosis, risk stratification, and management. Am J Hematol. 2022;97:1086-1107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 312] [Cited by in RCA: 433] [Article Influence: 144.3] [Reference Citation Analysis (0)] |
| 2. | Bladé J, Beksac M, Caers J, Jurczyszyn A, von Lilienfeld-Toal M, Moreau P, Rasche L, Rosiñol L, Usmani SZ, Zamagni E, Richardson P. Extramedullary disease in multiple myeloma: a systematic literature review. Blood Cancer J. 2022;12:45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 136] [Article Influence: 45.3] [Reference Citation Analysis (1)] |
| 3. | Shoji MK, Chen Y, Topilow NJ, Abou Khzam R, Dubovy SR, Johnson TE. Orbital Involvement in Multiple Myeloma. Ophthalmic Plast Reconstr Surg. 2023;39:347-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 4. | Singh RB, Singhal S, Sinha S, Cho J, Nguyen AX, Dhingra LS, Kaur S, Sharma V, Agarwal A. Ocular complications of plasma cell dyscrasias. Eur J Ophthalmol. 2023;33:1786-1800. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 5. | Oriol A. Multiple myeloma with extramedullary disease. Adv Ther. 2011;28 Suppl 7:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | McGrath R, Whitlow S, McCabe GA, McElnea EM. An nusual ocular manifestation of multiple myeloma. BMJ Case Rep. 2022;15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Benjamin I, Taylor H, Spindler J. Orbital and conjunctival involvement in multiple myeloma. Report of a case. Am J Clin Pathol. 1975;63:811-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Ben Artsi E, Barkley MR, Khong JJ, Mckelvie PA, McNab AA, Hardy TG. Multiple myeloma manifesting as an ocular salmon patch - a case report. Orbit. 2020;39:379-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Soutar R, Lucraft H, Jackson G, Reece A, Bird J, Low E, Samson D; Guidelines Working Group of the UK Myeloma Forum; British Committee for Standards in Haematology; British Society for Haematology. Guidelines on the diagnosis and management of solitary plasmacytoma of bone and solitary extramedullary plasmacytoma. Br J Haematol. 2004;124:717-726. [PubMed] |
| 10. | Gurnani B, Kaur K. Ocular Surface Squamous Neoplasia. 2023 Jul 31. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2025. [PubMed] |
| 11. | Lee GA, Hirst LW. Incidence of ocular surface epithelial dysplasia in metropolitan Brisbane. A 10-year survey. Arch Ophthalmol. 1992;110:525-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 92] [Article Influence: 2.8] [Reference Citation Analysis (0)] |