Published online Sep 16, 2025. doi: 10.12998/wjcc.v13.i26.108211
Revised: April 24, 2025
Accepted: June 13, 2025
Published online: September 16, 2025
Processing time: 106 Days and 21.6 Hours
Nocardiosis remains a rare and often underdiagnosed bacterial infection, particularly in immunocompromised individuals. The case report by Zhang et al high
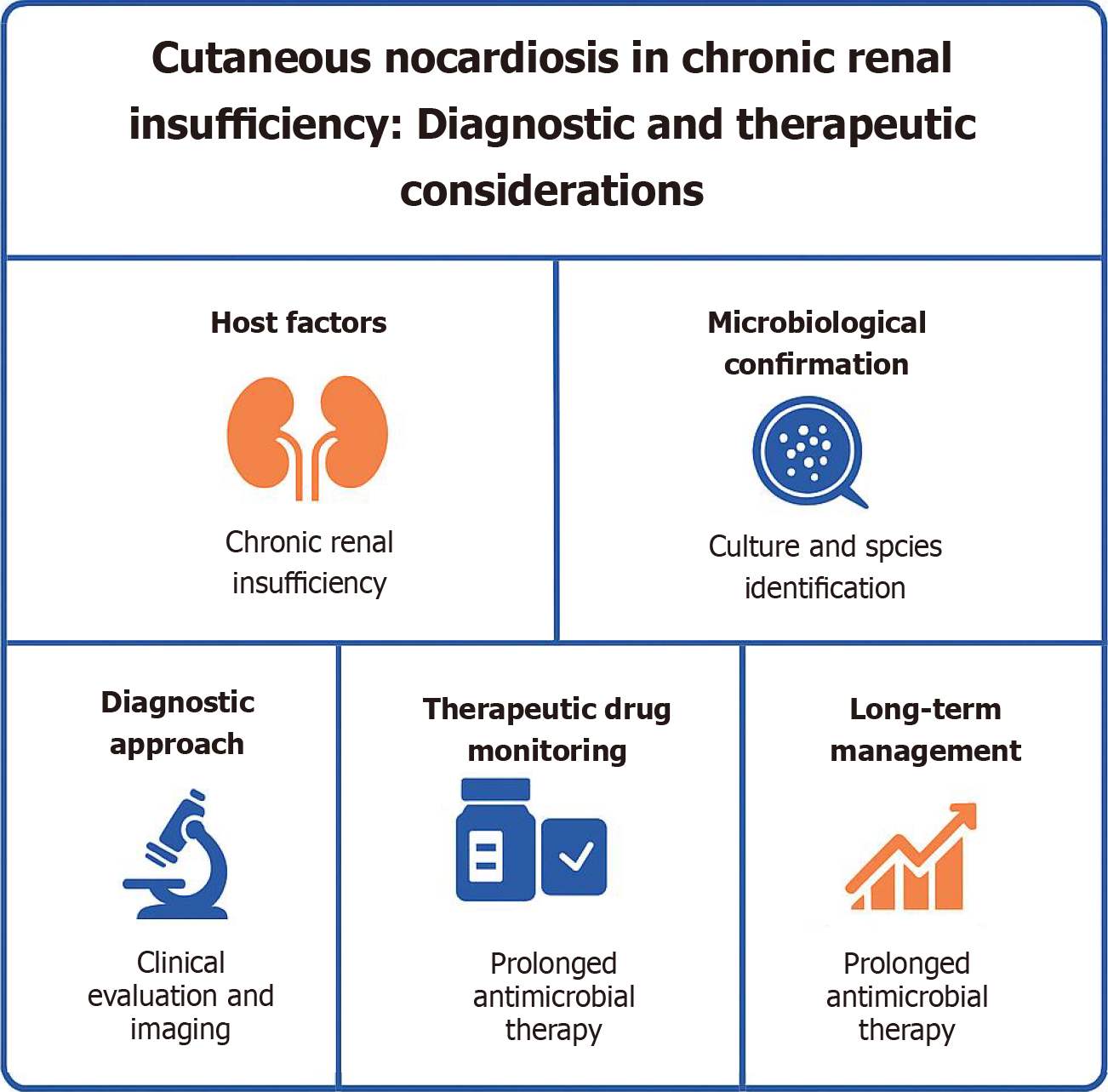
Core Tip: This editorial unravels the diagnostic and therapeutic challenges of nocardiosis in immunocompromised patients. It emphasizes the power of microbiological precision, tailored antibiotic regimens, and immune status assessment. A compelling case of Nocardia brasiliensis in chronic renal insufficiency offers key takeaways for clinicians tackling similar hurdles.
- Citation: Nagoba BS, Dhotre SV, Gavkare AM, Mumbre SS, Dhotre PS. Cutaneous nocardiosis in chronic renal insufficiency: Diagnostic and therapeutic considerations. World J Clin Cases 2025; 13(26): 108211
- URL: https://www.wjgnet.com/2307-8960/full/v13/i26/108211.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i26.108211
Nocardiosis, caused by the genus Nocardia, is an uncommon and potentially life-threatening bacterial infection[1]. Despite advancements in diagnostic techniques and antimicrobial therapy, the disease remains underrecognized, particularly in immunocompromised patients[2]. Nocardia brasiliensis, a species predominantly responsible for cutaneous infections, poses diagnostic and therapeutic challenges[3]. The clinical manifestations of nocardiosis vary widely, ranging from localized cutaneous infections to severe disseminated disease involving the lungs, central nervous system (CNS), and other organs[4].
Patients with chronic renal insufficiency, malignancies, organ transplants, or those undergoing immunosuppressive therapy are at heightened risk for nocardial infections[5]. The opportunistic nature of Nocardia complicates the diagnosis, often leading to delayed treatment[6]. Zhang et al's case report highlights the importance of early recognition, microbiological confirmation, and individualized management strategies in improving outcomes for patients with nocardiosis[7]. Although nocardiosis is rare, its incidence is rising, particularly among immunocompromised individuals. Studies estimate the incidence at 0.3%-1.8% among solid organ transplant recipients and up to 2% in human immunodeficiency virus (HIV)-positive populations[4]. The non-specific presentation and indolent course often lead to delayed diagnosis, which increases the risk of dissemination, especially to the lungs and CNS. Prompt recognition and early initiation of appropriate therapy are crucial in improving the clinical outcomes[5,6].
This editorial further explores the epidemiology, pathophysiology, clinical presentations, diagnostic challenges, thera
Nocardia species are environmental saprophytes found in soil, organic matter, and water[9]. Human infection primarily occurs through direct inoculation of contaminated material via skin trauma or through inhalation, leading to pulmonary or disseminated nocardiosis[10]. Nocardia brasiliensis, a leading cause of primary cutaneous nocardiosis, is predominantly reported in tropical and subtropical regions[11].
Although nocardiosis is rare, its incidence is increasing, particularly among immunocompromised populations[12]. Studies indicate that up to 60% of nocardiosis cases occur in patients with weakened immune systems, including those with HIV, organ transplant recipients, and individuals receiving corticosteroids or cytotoxic chemotherapy[13]. However, sporadic cases have also been reported in immunocompetent individuals following traumatic inoculation[14].
Given the limited epidemiological data on nocardiosis, establishing accurate incidence rates remains challenging. Continuous surveillance and improved diagnostic capacities are essential to determine the true disease burden and identify emerging resistance patterns[15].
Nocardia species are facultative intracellular pathogens capable of surviving within phagocytes, thereby evading host immune responses[16]. Upon entry through skin abrasions or inhalation, Nocardia organisms trigger localized infections, which can disseminate, if not promptly controlled[17].
The primary virulence factors include catalase and superoxide dismutase, which neutralize reactive oxygen species, allowing bacterial survival within macrophages[3]. Additionally, the production of trehalose dimycolate, a surface glycolipid, inhibits phagosome-lysosome fusion, further enhancing intracellular persistence[18].
In immunocompromised hosts, the diminished ability of macrophages and neutrophils to eliminate Nocardia leads to uncontrolled bacterial proliferation. Cutaneous nocardiosis often manifests as localized cellulitis, nodules, or abscesses with draining sinuses, resembling other bacterial or fungal infections[19]. In cases of systemic dissemination, the bacteria may spread hematogenously, leading to pulmonary, cerebral, or soft tissue involvement[20].
Understanding the pathogen's immune evasion mechanisms is critical for tailoring effective therapeutic strategies, particularly in vulnerable patient populations[21].
Cutaneous nocardiosis typically presents as a localized infection following traumatic inoculation, particularly in indivi
Systemic symptoms such as fever, lymphadenopathy, and malaise may accompany cutaneous lesions, especially in cases of disseminated disease[25]. Immunocompromised individuals, including those with chronic renal insufficiency, are at greater risk for dissemination to the lungs, brain, or other organs[26]. The clinical course is often indolent, leading to delays in diagnosis and treatment.
The diagnosis is further complicated by the polymorphic appearance of nocardial skin infections, which can mimic cellulitis, pyoderma gangrenosum, or deep fungal infections[27]. High clinical suspicion and prompt microbiological investigations are essential for early diagnosis and effective management.
Diagnosing nocardiosis remains a challenge due to its nonspecific clinical manifestations and the slow growth of Nocardia in culture. The time to identify Nocardia species may range from several days to weeks, delaying appropriate treatment[28]. Misdiagnosis is common, particularly in resource-limited settings where specialized diagnostic facilities are unavailable[29].
Laboratory confirmation requires microbiological culture, often utilizing selective media such as buffered charcoal yeast extract or Sabouraud dextrose agar[30]. Additionally, molecular methods, including 16S rRNA gene sequencing and polymerase chain reaction (PCR), offer higher sensitivity and specificity for species identification[31].
Histopathological examination with modified acid-fast staining can support diagnosis by revealing characteristic acid–fast branching filamentous bacteria. Radiological imaging, such as computed tomography or magnetic resonance imaging, may aid in evaluating disseminated disease[32].
Given the diagnostic complexities, a multidisciplinary approach involving infectious disease specialists, microbiologists, and pathologists is essential to ensure accurate diagnosis and timely initiation of therapy[33].
The cornerstone of nocardiosis treatment is prolonged antibiotic therapy. Empirical treatment often includes trime
In immunocompromised individuals, the duration of therapy typically extends to 6-12 months to prevent relapse. Therapeutic drug monitoring (TDM) ensures adequate serum drug levels; particularly important for agents like linezolid, which may cause hematological toxicity with prolonged use[37].
Considerations in elderly and frail patients: While TMP-SMX remains effective, its long-term use can lead to adverse effects such as bone marrow suppression, nephrotoxicity, and hepatotoxicity. In elderly or frail patients, dose adjustments based on renal function, along with regular monitoring of blood counts and hepatic/renal parameters, are essential[34]. Alternative agents such as minocycline, moxifloxacin, or linezolid may be considered in cases of TMP-SMX intolerance or contraindication. Clinical decision-making should carefully balance antimicrobial efficacy with the potential for toxicity in these vulnerable populations[35,36].
Surgical intervention: Surgical debridement may be necessary in cases of extensive cutaneous involvement or abscess formation[38].
Emerging therapies and mechanisms of drug resistance: Emerging therapies targeting bacterial resistance mechanisms; such as novel beta-lactamase inhibitors, are under investigation and may offer new options in refractory or multidrug-resistant cases. Nocardia species exhibit a range of resistance mechanisms. Resistance to sulfonamides like TMP-SMX may occur due to mutations in the dihydropteroate synthase gene. Other mechanisms include overexpression of efflux pumps, reduced permeability of the bacterial cell wall, and enzymatic modification of target sites, contributing to resistance against beta-lactams and aminoglycosides. Given the molecular variability across Nocardia species, species-level identification and susceptibility testing are essential to guide effective therapy[39].
The successful management of nocardiosis in immunocompromised individuals, as highlighted in Zhang et al's case report, underscores the importance of early diagnosis and individualized treatment[7]. Clinicians must maintain a high index of suspicion for nocardiosis in patients presenting with non-healing skin lesions, particularly those with underlying conditions like chronic renal insufficiency or those on immunosuppressive therapy[40]. Delayed diagnosis can lead to disease progression, dissemination, and increased morbidity and mortality.
Accurate microbiological identification is crucial for targeted antimicrobial therapy. Molecular diagnostic tools, including PCR and 16S rRNA sequencing, offer rapid and specific identification of Nocardia species, aiding in early therapeutic decisions[41]. Enhanced access to these diagnostics in resource-limited settings can significantly improve patient outcomes.
Furthermore, TDM plays a pivotal role in ensuring optimal drug concentrations while minimizing adverse effects. Regular monitoring of serum levels of TMP-SMX and linezolid can prevent toxicity, particularly in elderly and renaly impaired patients[42]. Clinicians should remain vigilant for adverse effects, including myelosuppression, hepatotoxicity, and nephrotoxicity, necessitating dose adjustments as appropriate.
From a public health perspective, understanding the epidemiology of nocardiosis through continuous surveillance is essential. Increased awareness and reporting will enable the identification of emerging resistance patterns, ensuring the effective use of antimicrobials. Multidisciplinary collaboration between infectious disease specialists, microbiologists, and pharmacists remains crucial in developing region-specific treatment guidelines.
Lastly, patient education on recognizing early symptoms, especially in immunocompromised individuals, can facilitate prompt medical attention. Comprehensive follow-up care is necessary to monitor treatment response, manage drug toxicity, and prevent relapse. Personalized management plans, incorporating immune status assessments and drug susceptibility testing, represent the cornerstone of successful treatment of nocardiosis.
The insights from this case report provide valuable guidance for clinicians managing similar cases, reinforcing the importance of timely diagnosis, targeted therapy, and multidisciplinary care in the management of Nocardia brasiliensis infections.
Preventive measures in high-risk groups: Immunocompromised individuals, including those with organ transplants, hematologic malignancies, or long-term corticosteroid use, are particularly susceptible to nocardial infections[41]. Preventive strategies include minimizing exposure to soil and organic dust, especially during gardening, landscaping, or construction activities. While routine screening is not currently recommended, heightened clinical awareness and early evaluation of non-healing lesions or unexplained pulmonary symptoms are critical in high-risk patients[4]. Patient education plays a pivotal role in reducing exposure and promoting timely medical consultation.
The case report by Zhang et al[7] serves as a critical reminder of the diagnostic and therapeutic complexities associated with nocardiosis. It highlights the necessity of maintaining a high index of suspicion in immunocompromised individuals presenting with atypical skin lesions. Early microbiological identification and species-level differentiation remain paramount in guiding targeted therapy.
Furthermore, this case underscores the importance of a personalized approach to antimicrobial management, considering patient-specific factors such as immune status, renal function, and potential drug toxicities. Collaborative decision-making involving infectious disease specialists, dermatologists, and microbiologists can optimize treatment outcomes and minimize therapeutic failures.
Nocardiosis, particularly cutaneous Nocardia brasiliensis infection, presents significant diagnostic and therapeutic challenges in immunocompromised patients. Early clinical suspicion, prompt microbiological diagnosis, and individualized antibiotic therapy are essential for successful management. For patients with chronic renal insufficiency, careful drug selection and monitoring are crucial to minimize adverse effects. Multidisciplinary collaboration and continued research on antimicrobial resistance and novel treatments will further improve patient outcomes.
Authors are thankful to Prof. Anant Kale, Stratizen Research & Innovation Services Pvt. Ltd., Pune, India for revising this article for syntax and scientific language style. Authors are also thankful to Mr. Vinod Jogdand for technical support in the preparation of manuscript.
| 1. | Brown-Elliott BA, Brown JM, Conville PS, Wallace RJ Jr. Clinical and laboratory features of the Nocardia spp. based on current molecular taxonomy. Clin Microbiol Rev. 2006;19:259-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 692] [Cited by in RCA: 787] [Article Influence: 41.4] [Reference Citation Analysis (0)] |
| 2. | Wilson JW. Nocardiosis: updates and clinical overview. Mayo Clin Proc. 2012;87:403-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 524] [Cited by in RCA: 483] [Article Influence: 37.2] [Reference Citation Analysis (0)] |
| 3. | Smego RA Jr, Gallis HA. The clinical spectrum of Nocardia brasiliensis infection in the United States. Rev Infect Dis. 1984;6:164-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 79] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Beaman BL, Beaman L. Nocardia species: host-parasite relationships. Clin Microbiol Rev. 1994;7:213-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 548] [Cited by in RCA: 553] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 5. | Ambrosioni J, Lew D, Garbino J. Nocardiosis: updated clinical review and experience at a tertiary center. Infection. 2010;38:89-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 245] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 6. | Rawat D, Rajasurya V, Chakraborty RK, Sharma S. Nocardiosis. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526075/. |
| 7. | Zhang S, Lu Y, Fu W. Chronic renal insufficiency complicated by skin infection with Nocardia brasiliensis: A case report. World J Clin Cases. 2025;13. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Restrepo A, Clark NM; Infectious Diseases Community of Practice of the American Society of Transplantation. Nocardia infections in solid organ transplantation: Guidelines from the Infectious Diseases Community of Practice of the American Society of Transplantation. Clin Transplant. 2019;33:e13509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 111] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 9. | Nonthakaew N, Sharkey LKR, Pidot SJ. The genus Nocardia as a source of new antimicrobials. NPJ Antimicrob Resist. 2025;3:5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Lerner PI. Nocardiosis. Clin Infect Dis. 1996;22:891-903; quiz 904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 422] [Cited by in RCA: 421] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 11. | Minero MV, Marín M, Cercenado E, Rabadán PM, Bouza E, Muñoz P. Nocardiosis at the turn of the century. Medicine (Baltimore). 2009;88:250-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 251] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 12. | Besteiro B, Coutinho D, Fragoso J, Figueiredo C, Nunes S, Azevedo C, Teixeira T, Selaru A, Abreu G, Malheiro L. Nocardiosis: a single-center experience and literature review. Braz J Infect Dis. 2023;27:102806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 13. | Palomba E, Liparoti A, Tonizzo A, Castelli V, Alagna L, Bozzi G, Ungaro R, Muscatello A, Gori A, Bandera A. Nocardia Infections in the Immunocompromised Host: A Case Series and Literature Review. Microorganisms. 2022;10:1120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 14. | Duggal SD, Chugh TD. Nocardiosis: A Neglected Disease. Med Princ Pract. 2020;29:514-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 15. | Rehman A, Olayiwola A, Vu CA, Bhatt P, Joseph JA, Ayoade F. Nocardia brasiliensis Pyomyositis in an Immunocompetent Patient Following Gardening Activity. J Investig Med High Impact Case Rep. 2024;12:23247096241261508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Thakur A, Mikkelsen H, Jungersen G. Intracellular Pathogens: Host Immunity and Microbial Persistence Strategies. J Immunol Res. 2019;2019:1356540. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 117] [Cited by in RCA: 228] [Article Influence: 38.0] [Reference Citation Analysis (0)] |
| 17. | Galar A, Martín-Rabadán P, Marín M, Cercenado E, Sánchez-Carrillo C, Valerio M, Bouza E, Muñoz P. Revisiting nocardiosis at a tertiary care institution: Any change in recent years? Int J Infect Dis. 2021;102:446-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Silva CL, Tincani I, Brandão Filho SL, Faccioli LH. Mouse cachexia induced by trehalose dimycolate from Nocardia asteroides. J Gen Microbiol. 1988;134:1629-1633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Palmieri JR, Santo A, Johnson SE. Soil-acquired cutaneous nocardiosis on the forearm of a healthy male contracted in a swamp in rural eastern Virginia. Int Med Case Rep J. 2014;7:41-47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Yamamoto H, Kuroda H, Hiramoto N, Hasuike T, Doi A, Nishioka H. Successful maintenance treatment of disseminated nocardiosis with cerebral abscess in a severely immunocompromised patient allergic to trimethoprim-sulfamethoxazole using moxifloxacin and high-dose minocycline: A case report. J Infect Chemother. 2024;30:1319-1323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Engelbrecht A, Saad H, Gross H, Kaysser L. Natural Products from Nocardia and Their Role in Pathogenicity. Microb Physiol. 2021;31:217-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 22. | Xue K, Zhang A, Liu S, Chen D. Multiple brain abscesses caused by Nocardia farcinica infection after hand injury: A case report and literature review. Medicine (Baltimore). 2024;103:e39019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | De La Hoz I, De La Hoz G, Singh G, Manoucheri M. Sporotrichoid Nocardiosis in an Immunocompetent Patient: A Case Report. Cureus. 2024;16:e75453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | Saoji VA, Saoji SV, Gadegone RW, Menghani PR. Primary cutaneous nocardiosis. Indian J Dermatol. 2012;57:404-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Martínez-Barricarte R. Isolated Nocardiosis, an Unrecognized Primary Immunodeficiency? Front Immunol. 2020;11:590239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 26. | Steinbrink J, Leavens J, Kauffman CA, Miceli MH. Manifestations and outcomes of nocardia infections: Comparison of immunocompromised and nonimmunocompromised adult patients. Medicine (Baltimore). 2018;97:e12436. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 112] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 27. | Traxler RM, Bell ME, Lasker B, Headd B, Shieh WJ, McQuiston JR. Updated Review on Nocardia Species: 2006-2021. Clin Microbiol Rev. 2022;35:e0002721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 76] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 28. | Yang J, Ren HT, Wang J, Dong AY, Chen YL, Hu DX, Wang H, Ji HM, Wen HN, Chen Y, Shi DY. Clinical characteristics, susceptibility profiles, and treatment of nocardiosis: a multicenter retrospective study in 2015-2021. Int J Infect Dis. 2023;130:136-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 29. | Pan L, Pan XH, Xu JK, Huang XQ, Qiu JK, Wang CH, Ji XB, Zhou Y, Mao MJ. Misdiagnosed tuberculosis being corrected as Nocardia farcinica infection by metagenomic sequencing: a case report. BMC Infect Dis. 2021;21:754. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 30. | Garrett MA, Holmes HT, Nolte FS. Selective buffered charcoal-yeast extract medium for isolation of nocardiae from mixed cultures. J Clin Microbiol. 1992;30:1891-1892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | Conville PS, Fischer SH, Cartwright CP, Witebsky FG. Identification of nocardia species by restriction endonuclease analysis of an amplified portion of the 16S rRNA gene. J Clin Microbiol. 2000;38:158-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 86] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 32. | Yadav P, Kumar D, Meena DS, Bohra GK, Jain V, Garg P, Dutt N, Abhishek KS, Agarwal A, Garg MK. Clinical Features, Radiological Findings, and Treatment Outcomes in Patients with Pulmonary Nocardiosis: A Retrospective Analysis. Cureus. 2021;13:e17250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 33. | Mustafa Alhashimi F, Salim S, Iqbal A, Balila M, Chishti MK. Disseminated Nocardia farcinica Infection in a Renal Transplant Patient: A Case Report. Cureus. 2024;16:e54963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 34. | Tashiro H, Takahashi K, Kusaba K, Tanaka M, Komiya K, Nakamura T, Aoki Y, Kimura S, Sueoka-Aragane N. Relationship between the duration of trimethoprim/sulfamethoxazole treatment and the clinical outcome of pulmonary nocardiosis. Respir Investig. 2018;56:166-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 35. | Davidson N, Grigg MJ, Mcguinness SL, Baird RJ, Anstey NM. Safety and Outcomes of Linezolid Use for Nocardiosis. Open Forum Infect Dis. 2020;7:ofaa090. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 36. | McTaggart LR, Doucet J, Witkowska M, Richardson SE. Antimicrobial susceptibility among clinical Nocardia species identified by multilocus sequence analysis. Antimicrob Agents Chemother. 2015;59:269-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 64] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 37. | Lin B, Hu Y, Xu P, Xu T, Chen C, He L, Zhou M, Chen Z, Zhang C, Yu X, Fang L, Zhu J, Ji Y, Lin Q, Cao H, Dai Y, Lu X, Shi C, Li L, Wang C, Li X, Fang Q, Miao J, Zhu Z, Lin G, Zhan H, Lv S, Zhu Y, Cai X, Ying Y, Chen M, Xu Q, Zhang Y, Xu Y, Federico P, Jiang S, Dai H. Expert consensus statement on therapeutic drug monitoring and individualization of linezolid. Front Public Health. 2022;10:967311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 34] [Reference Citation Analysis (0)] |
| 38. | Mora A, Oyenusi O, Abbasi S, Mitzov N, Randhawa A. Complex Management of Septic Joint and Cutaneous Nocardiosis in an Immunocompromised Patient: A Case Report. Cureus. 2024;16:e57810. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 39. | Lebeaux D, Ourghanlian C, Dorchène D, Soroka D, Edoo Z, Compain F, Arthur M. Inhibition Activity of Avibactam against Nocardia farcinica β-Lactamase FAR(IFM10152). Antimicrob Agents Chemother. 2020;64:e01551-e01519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 40. | Han Y, Huang Z, Zhang H, He L, Sun L, Liu Y, Liu F, Xiao L. Nocardiosis in glomerular disease patients with immunosuppressive therapy. BMC Nephrol. 2020;21:516. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 41. | Toyokawa M, Ohana N, Ueda A, Imai M, Tanno D, Honda M, Takano Y, Ohashi K, Saito K, Shimura H. Identification and antimicrobial susceptibility profiles of Nocardia species clinically isolated in Japan. Sci Rep. 2021;11:16742. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 42. | Liu T, Yuan Y, Wang C, Wu J, Wang Y, Na P, Chen X, Rao W, Zhao J, Wang D, Wang H, Duan Z, Xie F, Fang X, Xie L, Li H. Therapeutic drug monitoring of linezolid and exploring optimal regimens and a toxicity-related nomogram in elderly patients: a multicentre, prospective, non-interventional study. J Antimicrob Chemother. 2024;79:1938-1950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 6.0] [Reference Citation Analysis (0)] |