Published online Jul 26, 2025. doi: 10.12998/wjcc.v13.i21.103525
Revised: March 5, 2025
Accepted: March 27, 2025
Published online: July 26, 2025
Processing time: 156 Days and 19.3 Hours
Ovarian vein thrombosis (OVT) is a rare condition that most commonly affects postpartum women. It is particularly prevalent in the first 10 days postpartum, a period when women are more prone to developing this condition. The right ovarian vein is often affected due to its tortuous nature and less competent valves. OVT presents similarly to acute abdominal conditions, such as acute appendicitis, especially when the right ovarian vein is involved. Given the overlap in clinical presentation, diagnosis requires high-quality imaging techniques and a high degree of suspicion.
Herein, we report a rare case of OVT in a young postpartum female who presented to the emergency department with signs and symptoms of acute abdomen. The patient had a history of pulmonary tuberculosis treatment. A provisional diagnosis of a perforated appendix was made, and a lower midline exploratory laparotomy was planned. During surgery, the appendix and inte
OVT is most commonly seen in the early postpartum period, especially within the first 10 days. Due to its anatomical characteristics, the right ovarian vein is more commonly involved. The clinical presentation of OVT can closely mimic acute abdomen or acute appendicitis, making diagnosis challenging. Accurate diagnosis requires a high index of suspicion and advanced imaging techniques to differentiate OVT from other conditions with similar presentations.
Core Tip: Ovarian vein thrombosis (OVT) is a rare condition most commonly seen in postpartum women, presenting with acute abdominal symptoms that can mimic more common conditions like acute appendicitis, ovarian torsion, or ectopic pregnancy. The right ovarian vein is more frequently affected due to its anatomical characteristics, and symptoms typically include right lower quadrant abdominal pain, fever, nausea, and vomiting. Accurate diagnosis requires high suspicion and imaging techniques such as ultrasound, computed tomography, or magnetic resonance imaging. In this case, surgical examination revealed a thrombosed right ovarian vein in a 35-year-old postpartum woman who had been initially diagnosed with acute appendicitis. Surgical excision of the vein, followed by anticoagulation therapy with Rivaroxaban, led to an uneventful recovery. OVT should be considered in the differential diagnosis of postpartum abdominal pain to ensure timely intervention and prevent complications. Early detection and appropriate management are key to favorable outcomes.
- Citation: Ali S, Anjum A, Nasir KM, Khalid AR, Shahzad F, Nashwan AJ. Ovarian vein thrombosis mimicking acute appendicitis: A case report. World J Clin Cases 2025; 13(21): 103525
- URL: https://www.wjgnet.com/2307-8960/full/v13/i21/103525.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i21.103525
Ovarian vein thrombosis (OVT) is a rare phenomenon that impacts postpartum women and also those who have a history of gynecological malignancies or infections or who have undergone previous pelvic surgeries[1]. Postpartum women have the highest tendency to get affected by it. 0.05%-0.18% of pregnancies can result in OVT, with the incidence rising to 1%-2% after cesarean section[2]. This case cannot be diagnosed with ease as some other prevalent differentials like acute appendicitis, ovarian torsion, and ectopic pregnancy are prioritized, especially in the case of right-sided OVT. It can present with lower quadrant abdominal pain or mimic an acute abdomen. Different modalities can be used to diagnose, including ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI)[3]. OVT can be easily over
Our patient, a 35-year-old female, presented with severe pain in the right iliac fossa, associated with fever, nausea, and vomiting. The pain began on postpartum day 40.
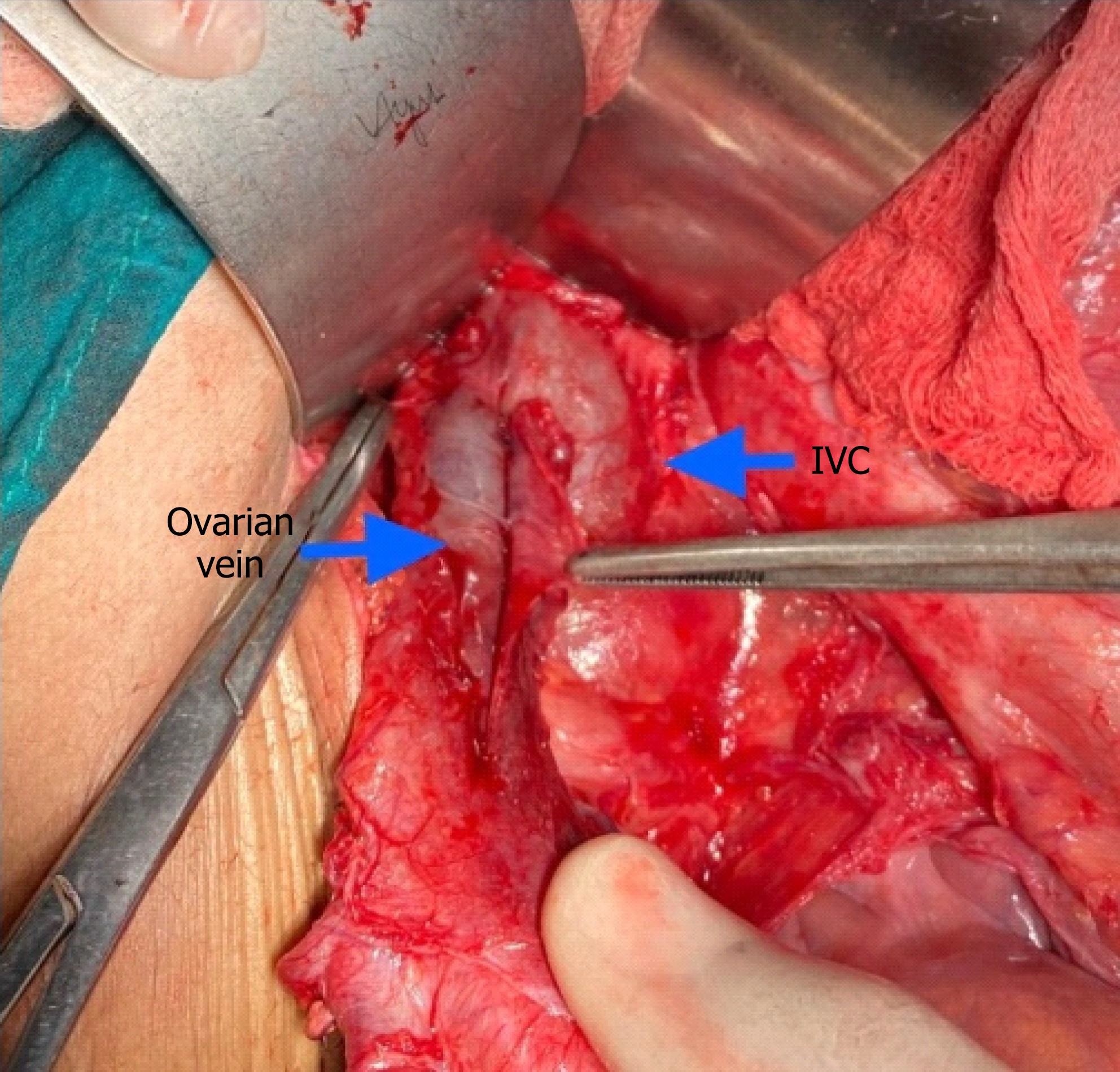
No imaging studies, such as CT or MRI, were performed initially due to the high suspicion of acute appendicitis in the emergency setting. Transvaginal and abdominal ultrasounds were attempted but were non-diagnostic, likely due to bowel gas interference and operator-dependent limitations, highlighting a key diagnostic challenge in this case[3]. In retrospect, advanced imaging such as CT or MRI could have clarified the diagnosis preoperatively and is recommended when feasible to differentiate OVT from other acute abdominal conditions. The lower extremities showed no signs of deep vein thrombosis, and the ultrasound results were non-diagnosed. Based on clinical findings and suspicion, a lower midline exploratory laparotomy was performed. Intraoperative findings revealed a normal appendix and normal intestines, ruling out appendicitis and other gastrointestinal causes. Further exploration of the retroperitoneum revealed a thrombosed and distended right ovarian vein, which was surgically examined (Figure 1).
Laboratory tests showed an elevated total leukocyte count of 17876/μL, indicating systemic inflammation. Other unremarkable preoperative parameters, including liver function tests, renal function tests, and basic coagulation profiles (Prothrombin time/international normalized ratio (INR), activated partial thromboplastin time). However, C-reactive protein and D-dimer were not assessed due to the urgency of surgical intervention. Postoperatively, D-dimer was elevated at 1.2 μg/mL (normal < 0.5 μg/mL) on day 1, supporting the thrombotic diagnosis, and normalized to 0.4 μg/mL by day 7 with anticoagulation, correlating with symptom resolution.
Upon examination, the patient appeared acutely ill. Her vital signs were as follows: Heart rate 125/min, blood pressure 100/75 mmHg, respiratory rate 18/min, and temperature 38.5 °C (fever noted at presentation). Before admission, she had reported a fever of 38.3 °C (equivalent to 101 °F). Localized tenderness was present in the right lower quadrant of the abdomen, with positive rebound tenderness in the right iliac fossa, suggesting peritoneal irritation. A chest examination revealed normal vesicular breathing with equal bilateral air entry. The rest of the physical examination was unremar
No relevant family or personal history was available, and the patient had no known family history of chronic illnesses or genetic disorders.
The patient had previously been treated for pulmonary tuberculosis (TB) two years ago and was considered cured following a standard six-month regimen of antitubercular therapy (2 months of isoniazid 300 mg, rifampicin 600 mg, pyrazinamide 1500 mg, and ethambutol 1000 mg daily, followed by 4 months of isoniazid 300 mg and rifampicin 600 mg daily), with no evidence of recurrence based on prior follow-up chest radiography and clinical assessment. At presentation, no respiratory symptoms or signs suggestive of active TB were noted, and thus, no further TB-specific investigations (e.g., chest radiography, Mantoux test, or sputum microbiology) were pursued in the acute setting.
The patient, who had a spontaneous vaginal delivery of a live-term fetus, experienced an uneventful postpartum period initially. However, on postpartum day 40, she developed acute right lower abdominal pain, fever (38.3 °C, equivalent to 101 °F), and systemic symptoms, including nausea and vomiting. At presentation, there was no vaginal bleeding or other significant symptoms. The pain was localized to the right iliac fossa and associated with rebound tenderness.
The final diagnosis was OVT, confirmed during surgery after ruling out other common causes of acute abdominal pain, such as appendicitis and abdominal TB.
The patient underwent surgical exploration, during which the thrombosed right ovarian vein was excised. Post-operative recovery was unremarkable, and the patient was discharged on the 3rd post-operative. Postoperatively, she was started on anticoagulation therapy with Rivaroxaban 15 mg Per Oral twice daily for 21 days, and Heparin was administered for 72 hours in the immediate postoperative period.
The patient’s post-operative recovery was uneventful, and she was discharged on the third post-operative. She continued on Rivaroxaban for six months, with no complications reported during follow-up visits. Follow-up at 1, 3, and 6 months included coagulation studies (D-dimer decreased from 1.2 µg/mL postoperatively to 0.3 µg/mL at 6 months; INR remained within 1.0-1.2), and a gynecological ultrasound at 6 months showed no residual ovarian vein abnormalities, confirming resolution of the thrombosis.
In 1956, Austin first described the case of OVT in a postpartum woman[4]. In the first 10 days of postpartum, the majority of the women, about 90%, are more prone to having OVT[5]. Between the two, most commonly, the right ovarian vein gets affected. Only 11 to 14% of cases are of bilateral OVT, meaning the right is more prone as it is more protracted and tortuous, and valves are less competent on the right side[6]. OVT does not appear to have a strong age-specific prevalence among postpartum women, as the primary risk is driven by the postpartum state rather than age alone. However, older age may increase baseline thrombotic risk due to comorbidities, while younger age, as in our 35-year-old patient, does not confer specific protection and may reflect fewer confounding factors.
The pathophysiology of OVT aligns with Virchow's triad because there is: (1) A hypercoagulable state in pregnancy; (2) Venous stasis caused by the uterus compressing the inferior vena cava; and (3) Endothelial trauma during delivery[7]. Additional risk factors include: (1) Cesarean section (increasing incidence to 1%-2% compared to 0.05%-0.18% in vaginal deliveries)[2]; (2) Infections such as endometritis; (3) Gynecological malignancies; (4) Previous pelvic surgeries; and (5) Coagulation disorders (e.g., systemic lupus erythematosus, antiphospholipid syndrome, factor V Leiden, protein C and S deficiency, paroxysmal nocturnal hemoglobinuria, and heparin-induced thrombocytopenia)[1]. In our case, the patient’s youth did not preclude OVT, highlighting the importance of considering this diagnosis irrespective of age in the postpartum setting.
Presentation of OVT is similar to some other conditions like appendicitis, tubo-ovarian abscess, endometritis, ovarian torsion, ectopic pregnancy, pyelonephritis, ureteric stones, ovarian cysts, or any gynecological malignancy. Rather than simply mimicking an acute abdomen, OVT poses diagnostic pitfalls due to overlapping symptoms such as right lower quadrant pain, fever, and leukocytosis, which can lead to misdiagnosis as appendicitis or other surgical emergencies, especially in the absence of specific imaging findings. No histopathological analysis or specific staining (e.g., Ziehl-Neelsen for TB) of the resected ovarian vein was performed, as there was no clinical or intraoperative evidence sugges
In our patient, the clinical picture was very similar to acute appendicitis with right iliac fossa pain, leukocytosis, fever, nausea, and vomiting (MANTRELS score 7/10). Ultrasound abdomen was nonspecific. Overlying the bowel with gas may limit adequate visualization by ultrasound, so ultrasonographic findings are highly operator-dependent, but still, it is the primary imaging technique[3]. CT scan or MRI can also be used as diagnostic imaging techniques, with magnetic resonance angiography having the best sensitivity and specificity but is not a cost-effective test[1]. While driven by clinical urgency, this approach underscores a limitation in our case, as preoperative imaging could have reduced diagnostic uncertainty and aligned with contemporary defensive medicine practices to mitigate litigation risks. Where time and resources permit, we advocate for CT or MRI to confirm the diagnosis preoperatively. Hence, in our case, the abdomen was opened on the line of acute appendicitis. Still, on finding a normal appendix, the retroperitoneum was explored, and the thrombosed vein was identified as the right ovarian vein during surgery.
This case underscores the broader clinical context of postpartum thrombotic diseases, where OVT represents a rare but critical entity within the spectrum of venous thromboembolism. Its significance lies in differentiating it from appendicitis and optimizing the diagnostic process for gynecological-related acute abdomen. The patient’s prior TB history raises intriguing questions about immune-mediated coagulation changes, as chronic infections may alter thrombotic risk through inflammatory pathways, a link warranting further research[7]. By highlighting OVT in a postpartum woman with unexplained abdominal pain, this case can enhance clinician awareness, reduce misdiagnosis rates, and refine diagnostic algorithms to include OVT earlier in the differential.
While the diagnostic and treatment approach, in this case, was conventional due to the emergency presentation, potential predisposing factors beyond typical postpartum risks warrant exploration. The patient’s history of treated pulmonary TB, though resolved, may suggest an immune-mediated or inflammatory contribution to her hypercoagulable state. This hypothesis could be investigated in future studies with larger cohorts. Additionally, the choice of Rivaroxaban over other anticoagulants (e.g., warfarin) was individualized based on its direct oral administration and favorable postpartum safety profile, avoiding the need for frequent monitoring in a young, otherwise healthy patient. OVT is a rare phenomenon, and if not addressed immediately, it can result in grave complications. Its diagnosis requires high-quality imaging techniques and a high degree of suspicion.
OVT is a rare but essential condition to consider in postpartum women, especially when presenting with symptoms resembling an acute abdomen. In this case, the patient’s presentation was initially thought to be acute appendicitis, but surgical exploration revealed thrombosis of the right ovarian vein. The patient’s postoperative recovery was uneventful, and anticoagulation therapy with Rivaroxaban was successfully administered for six months, preventing further complications. This case highlights the need for high clinical suspicion and advanced imaging techniques to accurately diagnose OVT, particularly in postpartum women, to avoid unnecessary surgical interventions.
| 1. | Arkadopoulos N, Dellaportas D, Yiallourou A, Koureas A, Voros D. Ovarian vein thrombosis mimicking acute abdomen: a case report and literature review. World J Emerg Surg. 2011;6:45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Sharma P, Abdi S. Ovarian vein thrombosis. Clin Radiol. 2012;67:893-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Jenayah AA, Saoudi S, Boudaya F, Bouriel I, Sfar E, Chelli D. Ovarian vein thrombosis. Pan Afr Med J. 2015;21:251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Basili G, Romano N, Bimbi M, Lorenzetti L, Pietrasanta D, Goletti O. Postpartum ovarian vein thrombosis. JSLS. 2011;15:268-271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Harris K, Mehta S, Iskhakov E, Chalhoub M, Maniatis T, Forte F, Alkaied H. Ovarian vein thrombosis in the nonpregnant woman: an overlooked diagnosis. Ther Adv Hematol. 2012;3:325-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Trang N, Kalluri M, Bajaj T, Petersen G. Idiopathic Left Ovarian Vein Thrombosis. J Investig Med High Impact Case Rep. 2020;8:2324709620947257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Levi M, van der Poll T. Inflammation and coagulation. Crit Care Med. 2010;38:S26-S34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 587] [Cited by in RCA: 655] [Article Influence: 43.7] [Reference Citation Analysis (0)] |