Published online Jun 16, 2025. doi: 10.12998/wjcc.v13.i17.99924
Revised: December 22, 2024
Accepted: January 14, 2025
Published online: June 16, 2025
Processing time: 199 Days and 5.2 Hours
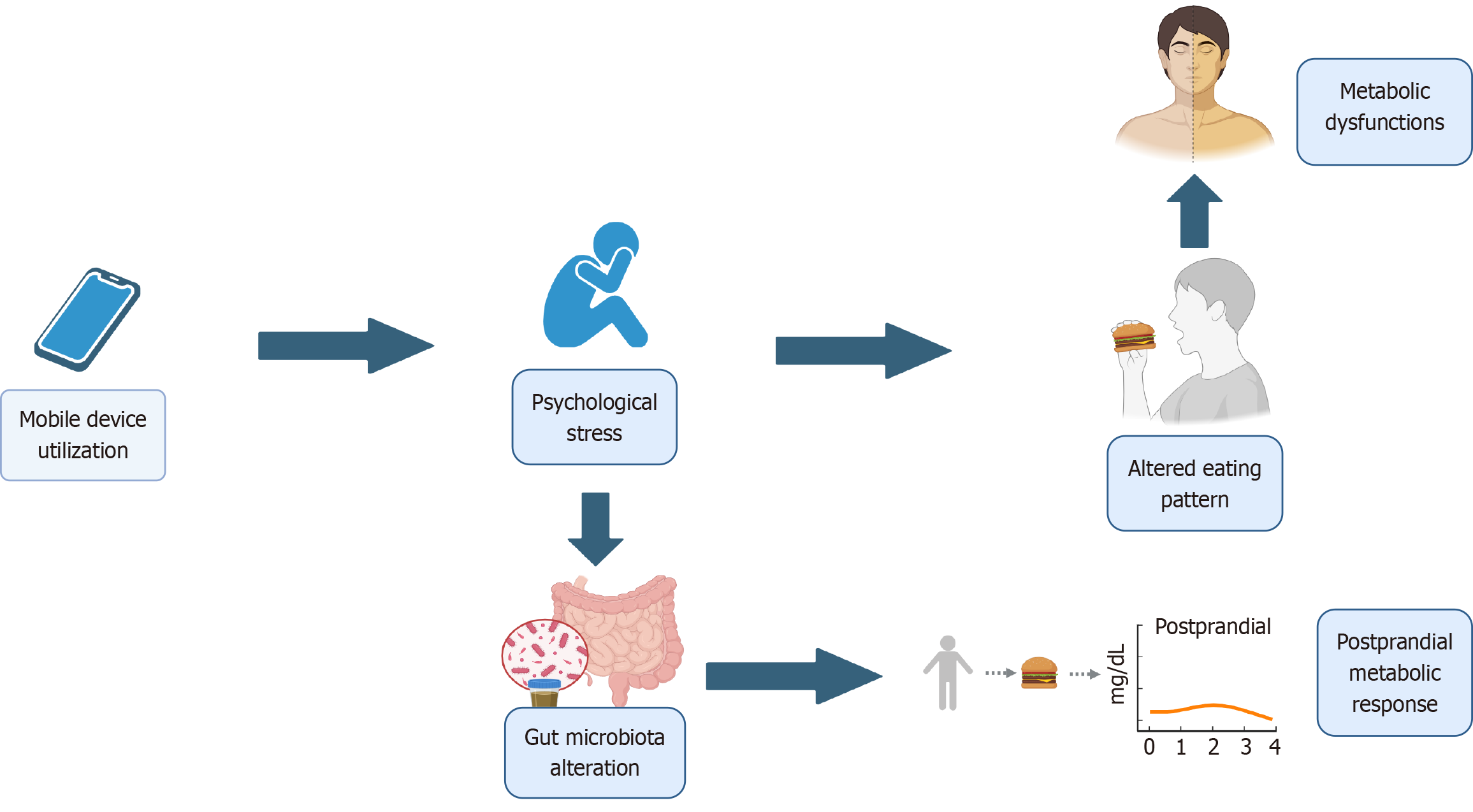
The habitual use of smartphones during meals has become a common behavior, raising concerns about its potential impact on eating habits and metabolic health. The present narrative review investigates how using a smartphone or tablet during meals can cause distractions and negatively affect metabolic health. A comprehensive narrative review was conducted by synthesizing peer-reviewed studies on the interplay between smartphone use during meals, eating behaviors, and metabolic health. Relevant literature was identified through searches in electronic databases and organized thematically to highlight trends and research gaps. By synthesizing evidence from existing literature, this review highlights that smartphone use during meals is associated with increased caloric intake, altered food composition, and disruptions in postprandial metabolic responses. These effects are mediated by reduced meal awareness and psychological distractions, including multitasking. Variability in findings arises from differences in study designs and populations. This review identifies critical research gaps, including the lack of longitudinal studies and the need to explore mechanisms underlying these relationships. By summarizing trends and patterns, this narrative review offers valuable insights into the complex interplay between digital device use, eating habits, and metabolic health, providing a foundation for future research and interventions.
Core Tip: This minireview explores the impact of using smartphones and tablets during meals on metabolic health. By analyzing various studies, it identifies key factors such as postprandial metabolic responses, food composition, and calorie consumption. Findings reveal a complex relationship between mealtime technology use and metabolic health, underscoring the need for further research. This review offers valuable insights for academics and practitioners into the interactions between technology, eating habits, and metabolic health.
- Citation: Aslam MS. Exploring the impact of mobile device use on mealtime distractions and its consequences for metabolic health: A narrative minireview. World J Clin Cases 2025; 13(17): 99924
- URL: https://www.wjgnet.com/2307-8960/full/v13/i17/99924.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i17.99924
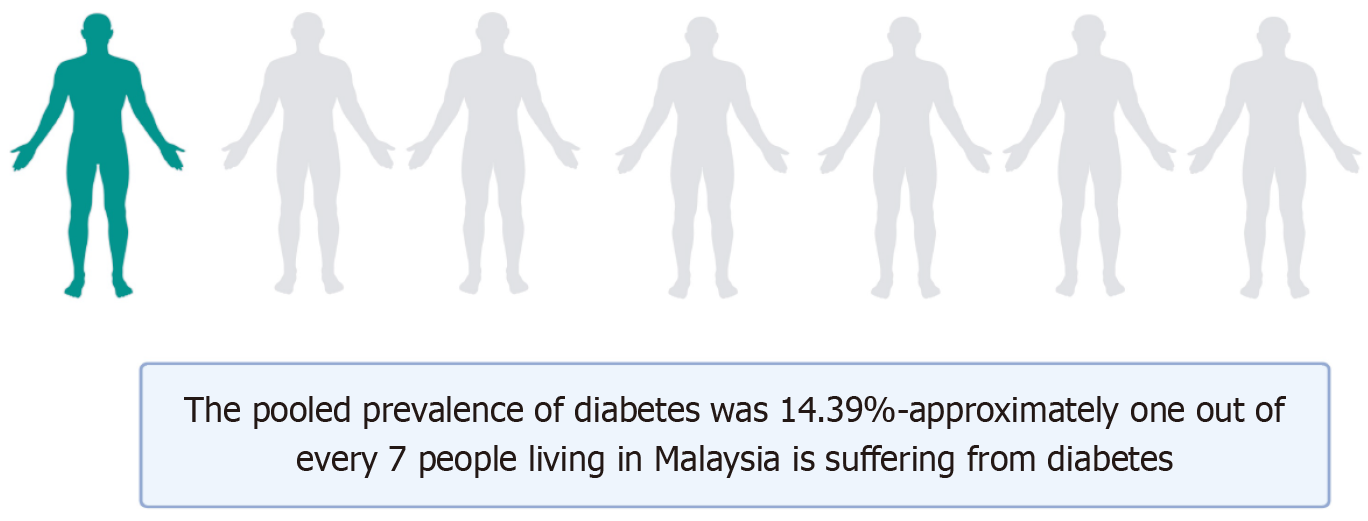
Diabetes is a significant health concern in Malaysia, with a pooled prevalence of 14.39%, equating to approximately 1 in every 7 Malaysians (Figure 1)[1]. Looking at the landscape in India, Ranasinghe et al[2] presented information from 69 studies, totaling 1778706 adult Indians, whose surveys were carried out between 1972 and 2017. Between the years of 2015 and 2019, the prevalence of diabetes in India's rural areas rose from 2.4% and 3.3% in 1972 to 15.0% and 19.0%, respec
Diabetes has a significant social effect, but it also comes with extremely high financial expenses for governments and healthcare systems. Patients with diabetes have severe direct and indirect repercussions that are amplified. The indirect costs primarily consist of financial losses from fatalities and disabilities, travel expenditures, nutritional costs, lost pro
A sedentary lifestyle, elevated waist circumference, family history of T2DM, obesity, especially abdominal obesity, hypertension, and fatty liver are factors linked to insulin resistance (Figure 2)[11-14].
As of 2024, approximately 4.88 billion people worldwide own smartphones, accounting for about 60.42% of the global population[15]. Specific global data on the percentage of adults using smartphones or tablets during meals is limited. In the United States, a 2016 study from the University of Michigan surveyed 1163 individuals aged 8 to 88 in English-speaking countries and found that attitudes toward mobile phone use during meals varied depending on the activity and the people present[16]. Additionally, a 2015 survey by the Pew Research Center found that 88% of respondents believe that it is generally not acceptable to use a cell phone during dinner[17]. While these studies provide insight into device usage during meals, comprehensive global statistics are not readily available.
In conducting this narrative review, a comprehensive approach was adopted to explore and synthesize existing literature on the relationship between eating behavior, smartphone use, inflammation pathways and type 2 diabetes (T2D). The selection of relevant literature was based on the author's expertise in the field, and an extensive search was conducted across various databases to identify studies published since the beginning till 2023. The search encompassed a range of sources, including peer-reviewed articles, review papers, and clinical studies. Keywords searched were related to “Eating”, “Smartphone”, “Energy Intake”, “Digestive System” and “Oral Physiology”. The inclusion criteria were broad, allowing for the incorporation of diverse perspectives on inflammatory processes associated with T2D, pathogenesis, potential new diagnostic biomarkers and biotherapeutics. In this work, articles were chosen based on the following criteria: Inflammatory pathways in the evaluation of antidiabetic activity in human. Only articles published in English were considered. The synthesis of information followed a narrative format, organized thematically to provide a comprehensive overview of the current understanding. This methodology acknowledges the qualitative nature of the review, leveraging the author's interpretative skills to offer insights into the relationships between eating behavior, smartphone use, inflammation pathways and T2D, while also recognizing the inherent subjectivity of a narrative synthesis.
To identify relevant literature for this narrative review, a comprehensive search of electronic databases was conducted. The search strategy was designed to capture articles focusing on the interplay between eating behavior, smartphone usage, energy intake, digestive system, mouth, and physiology. The search was performed on PubMed Central and PubMed using a combination of MeSH terms and text words. The inclusion and exclusion criteria were applied to filter the retrieved articles, ensuring that only relevant studies addressing the intersection of the identified topics were included in the review. The search was conducted up to the first quarter of 2024, and no language restrictions were applied. Duplicate studies were removed, and the remaining articles were screened for eligibility based on titles and abstracts. Full-text assessment was performed on potentially relevant articles to finalize the selection for inclusion in the review. The search strategy was employed for PubMed Central and PubMed (Table 1).
| Database | Search strategy |
| PubMed central | (("eating"[MeSH Terms] OR "eating"[All Fields]) AND ("smartphone"[MeSH Terms] OR "smartphone"[All Fields]) AND ("energy intake"[MeSH Terms] OR ("energy"[All Fields] AND "intake"[All Fields]) OR "energy intake"[All Fields]) AND ("digestive system"[MeSH Terms] OR ("digestive"[All Fields] AND "system"[All Fields]) OR "digestive system"[All Fields]) AND (("mouth"[MeSH Terms] OR "mouth"[All Fields] OR "oral"[All Fields]) AND ("physiology"[Subheading] OR "physiology"[All Fields] OR "physiology"[MeSH Terms]))) |
| PubMed | ("eating"[MeSH Terms] OR "eating"[All Fields]) AND ("smartphone"[MeSH Terms] OR "smartphone"[All Fields] OR "smartphones"[All Fields] OR "smartphone s"[All Fields]) AND ("energy intake"[MeSH Terms] OR ("energy"[All Fields] AND "intake"[All Fields]) OR "energy intake"[All Fields]) AND ("digestive system"[MeSH Terms] OR ("digestive"[All Fields] AND "system"[All Fields]) OR "digestive system"[All Fields]) AND (("mouth"[MeSH Terms] OR "mouth"[All Fields] OR "oral"[All Fields]) AND ("physiologies"[All Fields] OR "physiology"[MeSH Subheading] OR "physiology"[All Fields] OR "physiology"[MeSH Terms])) |
Gonçalves et al[18] investigated the influence of smartphone usage during meals on caloric intake, with a specific focus on the impact on lipid consumption. A cohort of 62 adults participated in experimental snack tests conducted over 4 d, during which various physical parameters (masticatory performance, swallowing threshold, masticatory frequency, and body mass index), environmental factors (presence or absence of distraction through smartphone use), and psychological variables (stress levels) were evaluated as potential confounding factors. The results revealed a significant effect of the experimental condition on both total caloric intake (P = 0.007) and lipid intake (P = 0.002). Specifically, when compared to the condition without distraction, smartphone usage led to a noteworthy increase in caloric intake (591 Kcal, P = 0.05), while reading a text further elevated caloric intake to 622 Kcal (P = 0.002). Concerning lipid intake, there was an interaction effect between the experimental condition and sex (P = 0.020), indicating a variation in the impact of smart
Studies comparing time-restricted high-fat feeding with ad libitum high-fat feeding have primarily used rat models to examine the effects of time-restricted eating (TRE) on physiological systems (Figure 4). Notably, many studies have difficulty distinguishing the effects of TRE from those of negative energy balance. Notwithstanding this restriction, a substantial amount of data indicates that TRE has positive effects on several organ systems and cardiometabolic para
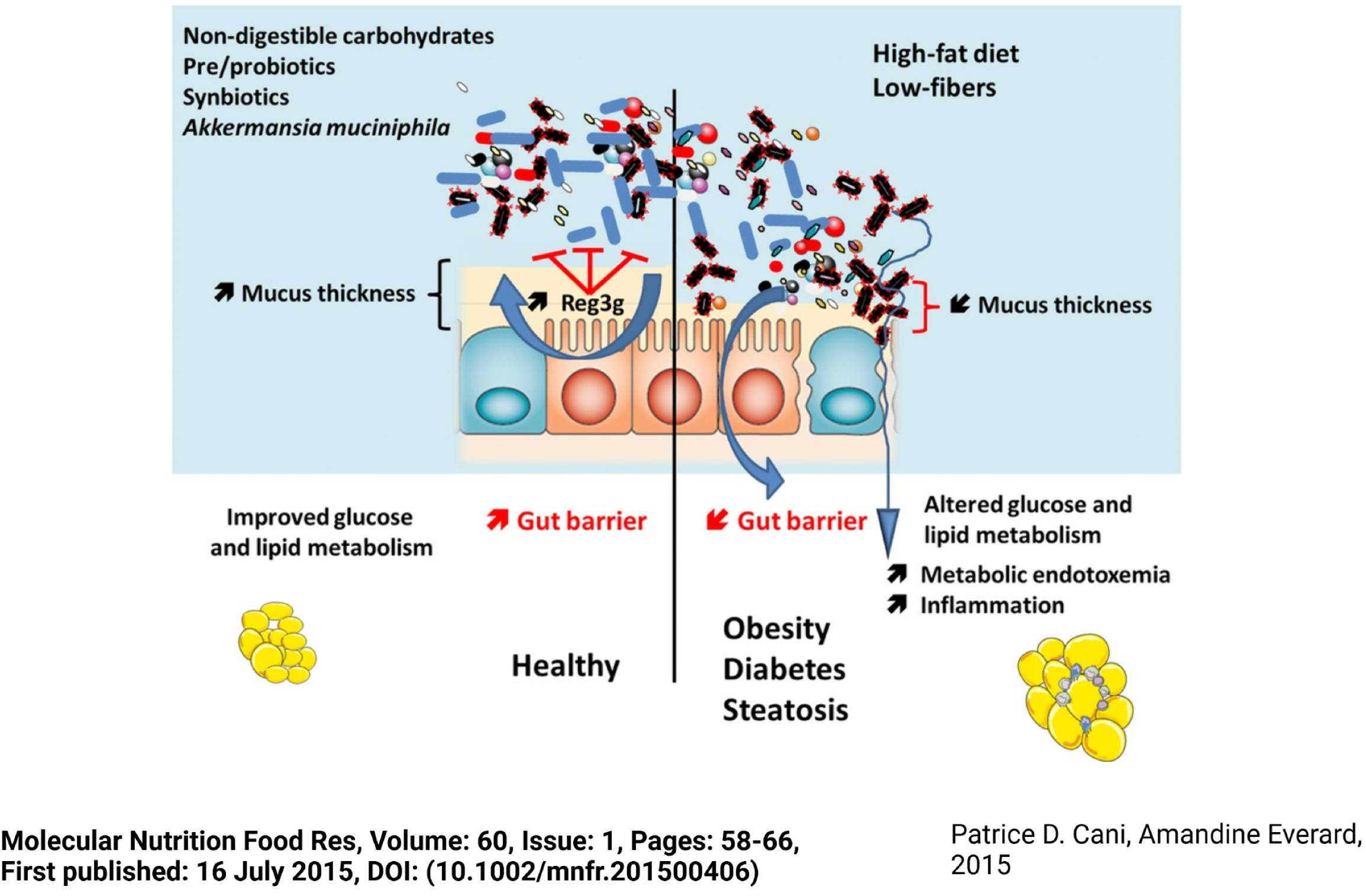
The current epidemic of obesity and diabetes has sparked a broad investigation into the variables affecting energy balance. Apart from well-established factors such as food patterns and physical exercise, new research emphasizes the critical function of gut microorganisms in the complex control of metabolism. The habitual use of digital devices, including smartphones and tablets, during meals has become a prevalent aspect of modern lifestyles. This behavior introduces a layer of complexity to dietary habits, potentially influencing the composition of nutrient intake and meal patterns. Entotypes, an exciting idea established by human gut microbiota studies, offer a framework for stratifying the population based on dominating bacterial profiles. In addition, studies on microbiome gene richness have provided further information on the makeup and variety of the gut microbial community. As we continue to explore the subtleties of gut-microbe interactions, it has become clear that nutrition has a major impact on the gut microbial ecology (Figure 5)[20].
Metabolic syndrome, obesity and T2D are more common in mood disorders compared to the general population[21]. Excessive use of smartphones, especially in the form of prolonged screen time, social media engagement, or gaming, has been linked to higher stress levels [22]. Problematic smartphone use (PSU) is associated with several types of psychopathology, such as depression and anxiety severity[23]. Elhai et al[24] explored the concept of PSU (often referred to as smartphone addiction) and its relationships with psychopathology, specifically focusing on anxiety and depression. The systematic review highlighted a consistent association between PSU and psychopathological factors, with depression showing a particularly strong correlation.
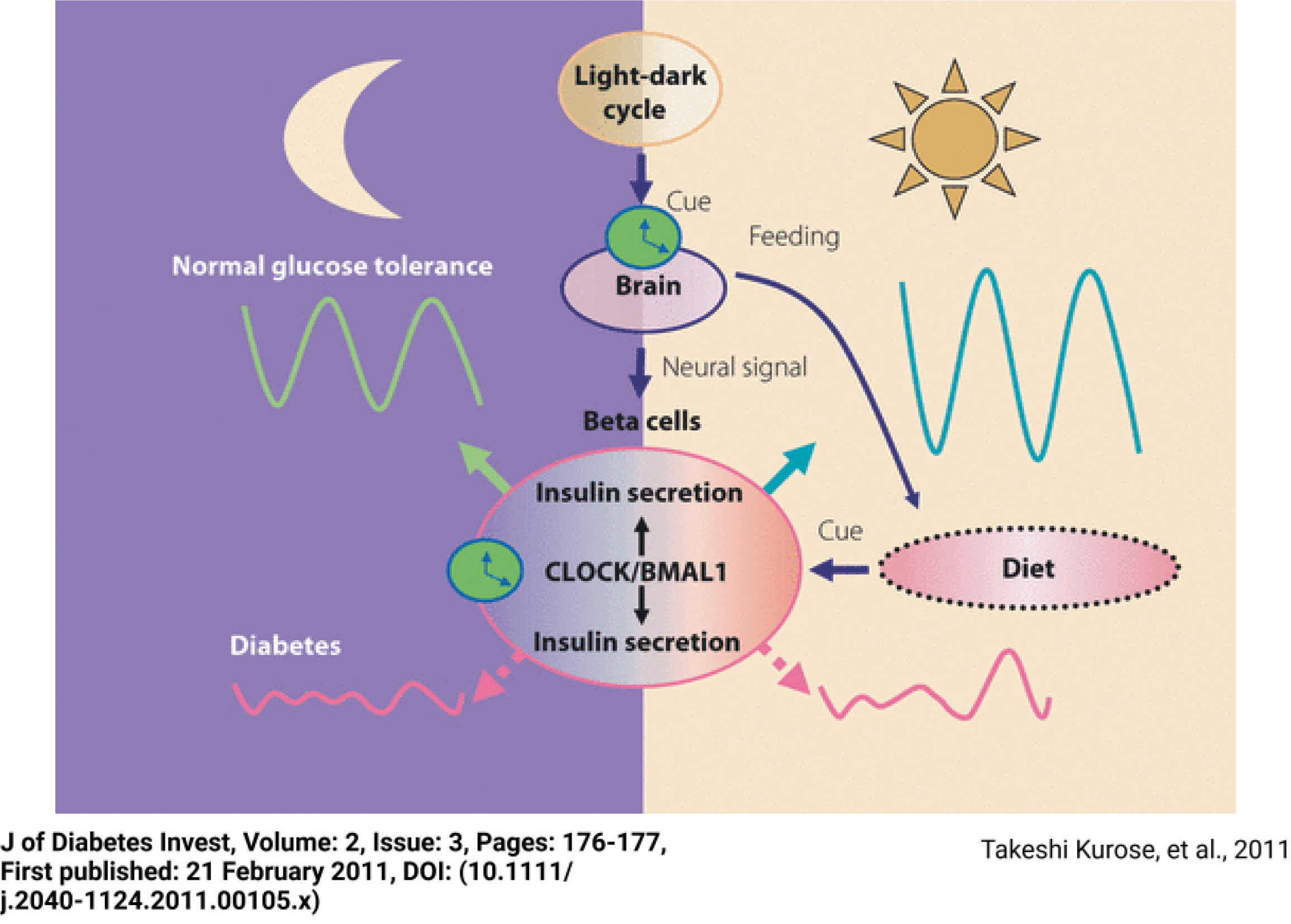
Skipped meals can be caused by an imbalanced time allocation between eating and using phones, which can encourage excessive snacking and eventually eating disorders[25,26]. Chronic snacking in the rest phase increased body weight gain and disrupted metabolic circadian rhythms in energy expenditure, body temperature, and locomotor activity[27]. CLOCK/BMAL1 regulates pancreatic insulin secretion in the day and night through insulin granule exocytosis. Disru
The findings of this narrative review emphasize the intricate relationship between mobile device use during meals and its potential impacts on metabolic health. Smartphone usage not only increases caloric intake and alters food composition but also disrupts postprandial metabolic responses, largely mediated by reduced meal awareness and psychological distractions. These disruptions may exacerbate metabolic dysfunction through mechanisms such as gut microbiota alteration and circadian rhythm dysregulation, including CLOCK/BMAL1 pathways. While the reviewed literature provides compelling evidence for these associations, significant variability in study designs and populations limits the generalizability of the findings. Moreover, the long-term effects of habitual device use during meals remain underexplored, necessitating further research with robust experimental and longitudinal designs. Addressing these gaps will be essential for developing targeted interventions and public health strategies aimed at mitigating the adverse effects of digital distractions on eating behaviors and metabolic health. The summary of key literature is presented in Table 2.
| Ref. | Study type | Sample size | Key findings | Relevance to study |
| Gonçalves et al[18] | Experimental study | 62 adults (26 males, 36 females) | Smartphone use during meals increases total caloric intake by approximately 15% compared to no distractions. Lipid intake is significantly higher during smartphone use, and sex differences in lipid consumption are observed, with women consuming more lipids than men across conditions | Provides direct evidence of how smartphone use during meals increases caloric and lipid intake, emphasizing the role of environmental distractions in food consumption behavior |
| Wu et al[25] | Cross-sectional | 4325 Chinese college students | Problematic smartphone use and psychological distress (anxiety and depression) mediate the relationship between poor sleep quality and disordered eating behaviors | Demonstrates the indirect role of smartphone use in shaping eating behaviors via psychological distress, providing a pathway for interventions targeting mealtime distractions |
| Rozgonjuk et al[23] | Empirical study | 101 undergraduate university students | Self-reported problematic smartphone use correlates with higher depression and anxiety symptoms, but objective smartphone use metrics (screen time, unlocks) over one week do not show this association | Highlights the discrepancy between self-reported PSU and actual smartphone use, emphasizing the role of psychological factors in perceived smartphone addiction |
In conclusion, our review showed a strong correlation between using a smartphone during meals and consuming more calories and fat, with differences seen according to the age and sex of young adults with full dentition (Figure 7). This finding emphasizes the possible influence of using digital devices on eating habits and nutritional results, underscoring a relevant field for additional study and public health consideration. Shifting our focus to the symbiotic relationship between gut microbes and the host, the existing literature presents compelling evidence for intricate communications between these entities. This cross-talk is finely regulated by mechanisms that promote the tolerance of commensals and the selection of presumed beneficial microbes. The gut microbiota, shaped by a combination of dietary habits and intrinsic host parameters, plays a pivotal role in influencing overall health. While certain factors, such as enterotypes, exhibit stability, others like microbial signatures demonstrate susceptibility to rapid changes, including metabolite production and specific taxa alterations. Recent preclinical interventions underscore the dynamic interplay involving intestinal epithelial cells and immunity, showcasing their role in modulating metabolic status based on ingested nutrients. Though understanding the inner workings of the interaction between humans and their gut microbes remains a challenging task, there is hope that we can impact this relationship in a good way. It becomes clear that one way to improve dietary practices is to focus on particular foods or nutrients, such probiotics, prebiotics, and polyphenols. By altering the gut microbiota, these therapies have the potential to improve overall health outcomes and optimize eating habits. The possibility for tailored dietary methods may present opportunities for improving individual well-being and encouraging healthier lifestyles as we navigate this rapidly developing field of research. Future investigations should focus on the long-term effects of specific device activities, individual behavioral patterns, and interventions designed to counteract these distractions. By addressing these gaps, researchers can contribute to a more comprehensive under
We would like to express our gratitude to Biorender and Flaticon for their valuable contributions to this research paper. Biorender provided a user-friendly platform for the creation of high-quality scientific illustrations, enhancing the visual representation of our findings. Additionally, Flaticon and Freepik contributed to the design elements, offering a diverse range of icons that complemented our visual content. The accessibility and quality of these resources significantly contributed to the overall presentation of our research. We acknowledge and appreciate the contributions of Biorender, Flaticon, Freepik in facilitating the creation of impactful visuals for this study.
| 1. | Akhtar S, Nasir JA, Ali A, Asghar M, Majeed R, Sarwar A. Prevalence of type-2 diabetes and prediabetes in Malaysia: A systematic review and meta-analysis. PLoS One. 2022;17:e0263139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 47] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 2. | Ranasinghe P, Jayawardena R, Gamage N, Sivanandam N, Misra A. Prevalence and trends of the diabetes epidemic in urban and rural India: A pooled systematic review and meta-analysis of 1.7 million adults. Ann Epidemiol. 2021;58:128-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 55] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 3. | Adnan M, Aasim M. Prevalence of Type 2 Diabetes Mellitus in Adult Population of Pakistan: A Meta-Analysis of Prospective Cross-Sectional Surveys. Ann Glob Health. 2020;86:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 4. | Mercado CI, McKeever Bullard K, Gregg EW, Ali MK, Saydah SH, Imperatore G. Differences in U.S. Rural-Urban Trends in Diabetes ABCS, 1999-2018. Diabetes Care. 2021;44:1766-1773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 5. | Simmons D, Glenister K, Magliano DJ, Bourke L. Changes in prevalence of diabetes over 15 years in a rural Australian population: The Crossroads Studies. Diabetes Res Clin Pract. 2020;170:108492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Hu H, Sawhney M, Shi L, Duan S, Yu Y, Wu Z, Qiu G, Dong H. A systematic review of the direct economic burden of type 2 diabetes in china. Diabetes Ther. 2015;6:7-16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 84] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 7. | Ganasegeran K, Hor CP, Jamil MFA, Loh HC, Noor JM, Hamid NA, Suppiah PD, Abdul Manaf MR, Ch'ng ASH, Looi I. A Systematic Review of the Economic Burden of Type 2 Diabetes in Malaysia. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 8. | Lo ZJ, Surendra NK, Saxena A, Car J. Clinical and economic burden of diabetic foot ulcers: A 5-year longitudinal multi-ethnic cohort study from the tropics. Int Wound J. 2021;18:375-386. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 56] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 9. | Oh SH, Ku H, Park KS. Prevalence and socioeconomic burden of diabetes mellitus in South Korean adults: a population-based study using administrative data. BMC Public Health. 2021;21:548. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 10. | Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, Abraham JP, Abu-Rmeileh NM, Achoki T, AlBuhairan FS, Alemu ZA, Alfonso R, Ali MK, Ali R, Guzman NA, Ammar W, Anwari P, Banerjee A, Barquera S, Basu S, Bennett DA, Bhutta Z, Blore J, Cabral N, Nonato IC, Chang JC, Chowdhury R, Courville KJ, Criqui MH, Cundiff DK, Dabhadkar KC, Dandona L, Davis A, Dayama A, Dharmaratne SD, Ding EL, Durrani AM, Esteghamati A, Farzadfar F, Fay DF, Feigin VL, Flaxman A, Forouzanfar MH, Goto A, Green MA, Gupta R, Hafezi-Nejad N, Hankey GJ, Harewood HC, Havmoeller R, Hay S, Hernandez L, Husseini A, Idrisov BT, Ikeda N, Islami F, Jahangir E, Jassal SK, Jee SH, Jeffreys M, Jonas JB, Kabagambe EK, Khalifa SE, Kengne AP, Khader YS, Khang YH, Kim D, Kimokoti RW, Kinge JM, Kokubo Y, Kosen S, Kwan G, Lai T, Leinsalu M, Li Y, Liang X, Liu S, Logroscino G, Lotufo PA, Lu Y, Ma J, Mainoo NK, Mensah GA, Merriman TR, Mokdad AH, Moschandreas J, Naghavi M, Naheed A, Nand D, Narayan KM, Nelson EL, Neuhouser ML, Nisar MI, Ohkubo T, Oti SO, Pedroza A, Prabhakaran D, Roy N, Sampson U, Seo H, Sepanlou SG, Shibuya K, Shiri R, Shiue I, Singh GM, Singh JA, Skirbekk V, Stapelberg NJ, Sturua L, Sykes BL, Tobias M, Tran BX, Trasande L, Toyoshima H, van de Vijver S, Vasankari TJ, Veerman JL, Velasquez-Melendez G, Vlassov VV, Vollset SE, Vos T, Wang C, Wang X, Weiderpass E, Werdecker A, Wright JL, Yang YC, Yatsuya H, Yoon J, Yoon SJ, Zhao Y, Zhou M, Zhu S, Lopez AD, Murray CJ, Gakidou E. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7951] [Cited by in RCA: 8005] [Article Influence: 727.7] [Reference Citation Analysis (0)] |
| 11. | Klein BE, Klein R, Moss SE, Cruickshanks KJ. Parental history of diabetes in a population-based study. Diabetes Care. 1996;19:827-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 79] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Sigal RJ, El-Hashimy M, Martin BC, Soeldner JS, Krolewski AS, Warram JH. Acute postchallenge hyperinsulinemia predicts weight gain: a prospective study. Diabetes. 1997;46:1025-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 99] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Nathan DM, Davidson MB, DeFronzo RA, Heine RJ, Henry RR, Pratley R, Zinman B; American Diabetes Association. Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care. 2007;30:753-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 931] [Cited by in RCA: 968] [Article Influence: 53.8] [Reference Citation Analysis (0)] |
| 14. | Melmer A, Laimer M. Treatment Goals in Diabetes. Endocr Dev. 2016;31:1-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 15. | Gill S. How Many People Own Smartphones in the World? (2024-2029). Priori Data. Available from: https://prioridata.com/data/smartphone-stats. |
| 16. | Moser C, Schoenebeck S, Reinecke K. Phones at the dinner table: U-M study explores attitudes. University of Michigan News. Available from: https://news.umich.edu/phones-at-the-dinner-table-u-m-study-explores-attitudes/. |
| 17. | Luckerson V. Everybody Hates When You Use Your Phone at Dinner. TIME. Available from: https://time.com/4010146/smartphones-dinner/. |
| 18. | Gonçalves RFDM, Barreto DA, Monteiro PI, Zangeronimo MG, Castelo PM, van der Bilt A, Pereira LJ. Smartphone use while eating increases caloric ingestion. Physiol Behav. 2019;204:93-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 19. | Petersen MC, Gallop MR, Flores Ramos S, Zarrinpar A, Broussard JL, Chondronikola M, Chaix A, Klein S. Complex physiology and clinical implications of time-restricted eating. Physiol Rev. 2022;102:1991-2034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 41] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 20. | Cani PD, Everard A. Talking microbes: When gut bacteria interact with diet and host organs. Mol Nutr Food Res. 2016;60:58-66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 109] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 21. | SayuriYamagata A, Brietzke E, Rosenblat JD, Kakar R, McIntyre RS. Medical comorbidity in bipolar disorder: The link with metabolic-inflammatory systems. J Affect Disord. 2017;211:99-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 89] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 22. | Faurholt-Jepsen M, Frost M, Busk J, Christensen EM, Bardram JE, Vinberg M, Kessing LV. Is smartphone-based mood instability associated with stress, quality of life, and functioning in bipolar disorder? Bipolar Disord. 2019;21:611-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 23. | Rozgonjuk D, Levine JC, Hall BJ, Elhai JD. The association between problematic smartphone use, depression and anxiety symptom severity, and objectively measured smartphone use over one week. Comput Hum Behav. 2018;87:10-17. [RCA] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 153] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 24. | Elhai JD, Dvorak RD, Levine JC, Hall BJ. Problematic smartphone use: A conceptual overview and systematic review of relations with anxiety and depression psychopathology. J Affect Disord. 2017;207:251-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 641] [Cited by in RCA: 684] [Article Influence: 85.5] [Reference Citation Analysis (0)] |
| 25. | Wu R, Guo L, Rong H, Shi J, Li W, Zhu M, He Y, Wang W, Lu C. The Role of Problematic Smartphone Uses and Psychological Distress in the Relationship Between Sleep Quality and Disordered Eating Behaviors Among Chinese College Students. Front Psychiatry. 2021;12:793506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 26. | Tayhan Kartal F, Yabancı Ayhan N. Relationship between eating disorders and internet and smartphone addiction in college students. Eat Weight Disord. 2021;26:1853-1862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 27. | Begemann K, Heyde I, Witt P, Inderhees J, Leinweber B, Koch CE, Jöhren O, Oelkrug R, Liskiewicz A, Müller TD, Oster H. Rest phase snacking increases energy resorption and weight gain in male mice. Mol Metab. 2023;69:101691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 28. | Kurose T, Yabe D, Inagaki N. Circadian rhythms and diabetes. J Diabetes Investig. 2011;2:176-177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |