INTRODUCTION
This case report aimed to present the case of a 63-year-old Han Chinese male, admitted on July 7, 2023, with a 5-day history of memory loss as the chief complaint.
CASE PRESENTATION
Chief complaints
The patient had a 5-day history of memory loss.
History of present illness
The patient presented with sudden-onset memory impairment without symptoms such as nausea, vomiting, cough, limb weakness, convulsions, speech impairment, dizziness, headache, or other discomforts. Bowel and urinary functions were normal, with no weight change.
History of past illness
His medical history included hypertension, diabetes, and cerebral infarction.
Personal and family history
The patient reported no personal and family history.
Physical examination
Upon admission, physical examination revealed decreased memory and calculation ability (93-7), accompanied by preserved comprehension and orientation. Likewise, the pupillary light reflex was unremarkable, with no nystagmus, smooth eye movement, and stable gaze. Tongue was central, with limb muscle strength at grade 5 and normal muscle tone. Additionally, bilateral tendon reflexes were symmetrical, with no pathological signs and no evidence of deep or superficial sensation abnormalities. Auxiliary examinations were pending. Thus, a preliminary diagnosis of acute cerebral infarction was made.
Laboratory examinations
Laboratory examinations were not performed.
Imaging examinations
Following admission, the patient received treatment aimed at for enhancing cerebral circulation, nourishing cerebral neuronal function nerves, preventing platelet aggregation, and regulating lipid levels. On the second day, besides previous memory decline, the patient had developed new symptoms of pain sensory loss in the right limb. Post-admission, the patient, in addition to the pre-existing memory decline, exhibited new symptoms, including pain loss in the right limb. Indeed, this clinical scenario presentation significantly raises concerns about potential underlying neurological conditions like such as stroke or acute limb ischemia, as given that they can manifest with similar symptoms[1]. As is well documented, the symptom overlaps between stroke and other conditions (e.g., acute limb ischemia) requires thorough investigation to prevent mitigate the risk of misdiagnosis[2]. Magnetic resonance imaging (MRI) is a crucial diagnostic tool here, as considering that it offers detailed brain structure images and can assist in identifying ischemic, infarcted, or other abnormal areas that might explain account for the patient’s symptoms[3]. Moreover, MRI can assess the functional connectivity and structural changes in the brain, which may be altered in cases of sudden neurological deficits[4]. On the same day, a brain MRI plain scan and diffusion-weighted imaging were performed, revealing brain MRI (plain scan and diffusion-weighted imaging) showed displayed acute infarction in the bilateral anterior medial thalamus, suggestive of Percheron artery embolism.
FINAL DIAGNOSIS
Notably, calculation impairment, severe memory loss, personality changes, diminished inhibition, and initiative, as well as disorientation in time and place, can potentially be induced by the disruption of fibers projecting from this region to the orbitofrontal cortex and cingulate gyrus as a result of ischemic injury[5-8]. Additionally, damage to the papillary thalamic tract adjacent to the dorso-medial nucleus and disruptions in the connection between the thalamic nucleus and the hippocampus can also lead to memory impairment[9]. However, acute occlusion of the Percheron artery may involve the medial and anterior thalamic nuclei[10-12]. Consequently, in this particular case, head MRI delineated acute occlusion in the Percheron artery[13-15], resulting in acute cerebral infarction. Of note, this neuroanatomical localization accounted for the fundamental cause of the patient’s memory decline[16,17]. Subsequently, the pain subsided on the second day, which might have been elicited by the disruption of connecting fibers from the medial thalamus to the cortical sensory area due to acute cerebrovascular ischemia and associated with the unique vascular orientation of the Percheron artery[18,19]. Finally, based on the aforementioned clinical findings and neurological localization, the patient was diagnosed with Percheron artery syndrome.
TREATMENT
At present, the main treatment principles for Percheron syndrome are as follows: (1) Conservative treatment: Given the challenges in the diagnosis of artery of Percheron infarction, early conservative treatment can assist in minimizing disability and mortality rates[20]; and (2) Neurorehabilitation: For patients who have experienced Percheron syndrome, neurorehabilitation plays an important role. Rehabilitation programs should include physical therapy, occupational therapy, and language therapy to aid patients in restoring restore function and improving their quality of life[17]. Besides, administered antiplatelet therapy, lipid-lowering drugs agents, measures to enhance cerebral circulation and neurotrophic support were implemented cerebral nerves. To begin, anti-platelet therapy prevents thrombosis and vascular blockage. In cases of acute cerebral infarction caused by thrombotic-blocked occlusion, it improves cerebral blood flow and minimizes the risk of ischemic injury by inhibiting platelet function[21]. Secondly, lipid-regulating therapy aims to lowers blood cholesterol and triglyceride levels and, therefore, decreases the risk of atherosclerosis, a key factor for cerebral infarction. Statins can effectively reduce low-density lipoprotein cholesterol levels, improve vascular endothelial function, and maintain vascular health[22]. The pharmacotherapy for improving cerebrovascular circulation improvement includes vasodilators and microcirculation-improving drugs. They enhance cerebral blood supply and mitigate ischemic nerve damage by dilating vessels and increasing flow, thereby promoting nerve cell survival and functional recovery[23]. Finally, nutritional neurotherapy focuses on providing nutrients to promote neuroprotection and nerve regeneration. For instance, using the administration of some antioxidants and neurotrophic factors can alleviate oxidative stress and inflammatory responses, thus protecting nerve cells from injury. Additionally, nutritional therapy can improve patients’ overall health and enhance their resilience[24,25].
OUTCOME AND FOLLOW-UP
After 5 days of treatment, the patient’s recent memory improved, and he was discharged with significant symptom relief. Following discharge, the patient regularly attended follow-ups for reexamination[26]. Noteworthily, no limb movement, language, or cognitive disorders were recorded during the subsequent six-month follow-up.
DISCUSSION
This case, presents a case of Percheron’s artery syndrome, a rare form of acute cerebral infarction in a rare type of acute cerebral infarction in neurology, is Percheron’s artery syndrome. The Percheron artery is an anatomical variation of the brain’s posterior circulation artery of the brain, and Its occlusion causes bilateral para-thalamic artery infarcts, with or without mesencephalic involvement[27-29]. This type of specific type of acute ischemic stroke manifests as vertical gaze palsy, altered level of consciousness, and memory impairment. However, it is rarely associated with pyramidal signs or cranial nerve injury. Standard brain scans or low-resolution MRI generally fail to accurately reveal identify the lesion, often frequently leading to misdiagnosis[18,30]. We report a case of acute Percheron artery occlusion involving the Percheron artery. Interestingly, this case presented only manifested memory impairment and lacked the typical “triad” manifestations. The injuries of the medial thalamic nucleus, and the anterior nucleus, along with the damage and the fibers connecting the medial thalamus to the cortical sensory area, were identified as the crucial factors contributing to this particular clinical manifestation. These findings were in accordance with the specific vascular innervation area of the Percheron artery in this case[31]. Bilateral para-thalamic cerebral infarctions are rarely encountered, suggesting a link possible association with Percheron artery occlusion. To understand elucidate the symptoms and their neurological localization, one must consider the thalamic vascular anatomy must be considered. Specifically, Thalamic blood vessel types can be classified into three categories[32,33]. The first category is type involves normal paravenous anatomy, where the left and right collateral arteries originate from their respective posterior cerebral arteries[34,35]. The second type is divided into two subtypes. Subtype 1 involves both accessory arteries originating from either the left or right posterior cerebral artery, whereas, while subtype 2 features the Percheron artery (a congenital variant of the posterior cerebral artery branch) supplying both sides of the thalamus. a congenital variant of the posterior cerebral artery branch, specifically the Percheron artery, which supplies both sides of the thalamus[11]. Lastly, the third type is a variation in collateral vein anatomy, where with two veins originate from a single arterial branch that simultaneously connects connecting the posterior cerebral arteries on both sides[36]. This patient exhibited the second type, subtype 2 (Percheron artery), of vascular anatomical variation. The thalamus regulates is responsible for regulating the sleep-wake cycle. Therefore, thalamic infarction can lead to cause abnormal sensation or numbness, language or cognitive impairment, and memory impairment. It is worthwhile emphasizing that the Percheron artery variation occurs in 4% to 11% of the global population, and its with the artery infarction accounting accounts for 4% to 18% of all thalamic infarctions and 0.1% to 2% of all strokes[32,37]. Herein, the patient exclusively presented with cognitive impairment and paresthesia, without vertical gaze palsy, likely attributable to the intact the due to an intact superior mesencephalon nucleus responsible for pupillary innervation. Consequently, careful rigorous clinical examination is warranted to identify aids in identifying the location of the damage location. Occipital infarction was ruled out by based on the findings of head MRI (Figure 1), which suggested indicated basilar artery occlusion with symmetrical ischemic lesions in both the thalamus and premesencephalic region. Further cranial vascular enhanced computed tomography revealed a variant vascular branch of the right posterior cerebral artery, the Percheron artery (Figure 2). A significant filling defect in the Percheron artery, not involving the occipital lobe, aligned with clinical findings. The Percheron artery caused damage to both the medial thalamic nucleus and the anterior thalamic nucleus[38]. Furthermore, computed tomography angiography demonstrated that the right vertebral artery was slender, with an anastomotic variation, consistent with the Percheron artery’s anatomical features.
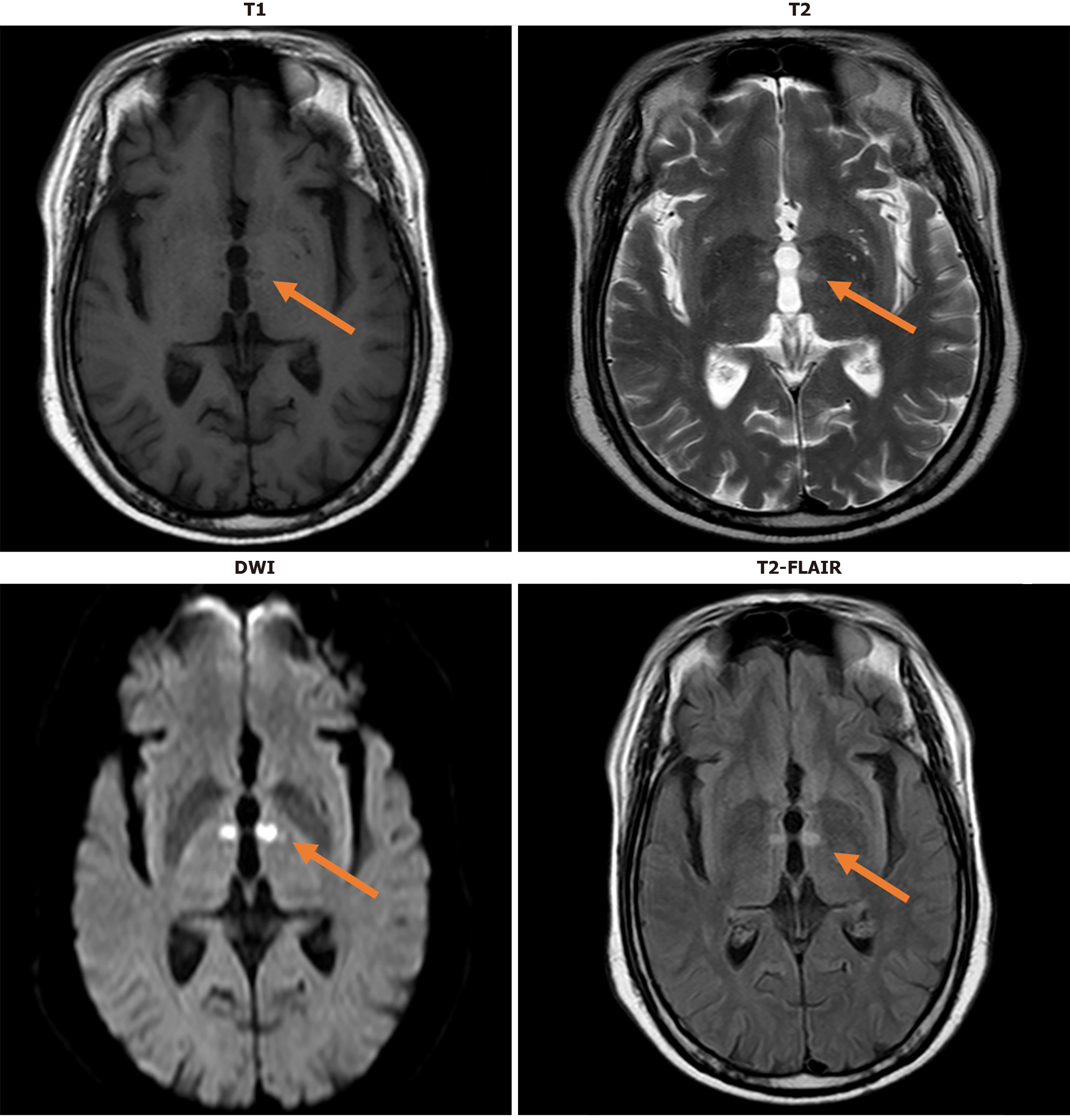
Figure 1 Magnetic resonance imaging.
This figure clearly reflects the imaging manifestations of acute cerebral infarction closely associated with Percheron artery occlusion on various magnetic resonance imaging sequences, including but not limited to T1-weighted imaging, T2-weighted imaging, diffusion-weighted imaging, and fluid-attenuated inversion-recovery sequences. Each sequence provides unique information regarding the location, extent, and characteristics of the infarcted area within the brain. DWI: Diffusion-weighted imaging; FLAIR: Fluid-attenuated inversion-recovery.
Figure 2 Computed tomography angiography examination.
This figure illustrates the location of the Percheron artery and its acute occlusion on computed tomography angiography examination.
CONCLUSION
Treatment of Percheron artery infarction should be tailored to the pathological process and its potential effects. Though rare, its treatment protocol is similar to that of other strokes. Continuous follow-up is vital for monitoring the patient’s progress and adjusting treatment plans, which relies on patient compliance. Follow-up is crucial for preventing recurrent strokes and other cardiovascular events. According to earlier studies, patients with acute cerebral infarction have a higher risk of subsequent strokes. Thus, the management of risk factors, including hypertension, diabetes, and dyslipidemia, is of paramount significance[39]. Moreover, follow-up care can assist in addressing psychological requirements since numerous stroke survivors experience emotional distress and express uncertainty regarding their recovery process[40]. Thus, for patients with Percheron artery occlusion, attending physicians must establish detailed patient records, ensure timely communication, and conduct regular follow-up evaluations to facilitate prompt treatment and support effective rehabilitation.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade D
Novelty: Grade B
Creativity or Innovation: Grade C
Scientific Significance: Grade C
P-Reviewer: Masoumi S S-Editor: Wei YF L-Editor: A P-Editor: Li X