Published online Mar 6, 2024. doi: 10.12998/wjcc.v12.i7.1251
Peer-review started: November 26, 2023
First decision: December 29, 2023
Revised: January 9, 2024
Accepted: February 4, 2024
Article in press: February 4, 2024
Published online: March 6, 2024
Processing time: 95 Days and 18.7 Hours
Testicular torsion is the most common acute scrotum worldwide and mainly occurs in children and adolescents. Studies have demonstrated that the duration of symptoms and torsion grade lead to different outcomes in children diagnosed with testicular torsion.
To predict the possibility of testicular salvage (TS) in patients with testicular torsion in a tertiary center.
We reviewed the charts of 75 pediatric patients with acute testicular torsion during a 12-year period from November 2011 to July 2023 at the Suzhou Hospital of Anhui Medical University. Univariate and multivariate logistic regression analyses were used to determine independent predictors of testicular torsion. The data included clinical findings, physical examinations, laboratory data, color Doppler ultrasound findings, operating results, age, presenting institution status, and follow-up results.
Our study included 75 patients. TS was possible in 57.3% of all patients; testicular torsion occurred mostly in winter, and teenagers aged 11-15 years old accounted for 60%. Univariate logistic regression analyses revealed that younger age (P = 0.09), body mass index (P = 0.004), torsion angle (P = 0.013), red blood cell count (P = 0.03), neutrophil-to-lymphocyte ratio (P = 0.009), and initial presenting institution (P < 0.001) were associated with orchiectomy. In multivariate analysis, only the initial presenting institution predicted TS (P < 0.05).
The initial presenting institution has a predictive value for predicting TS in patients with testicular torsion. Children with scrotal pain should be admitted to a tertiary hospital as soon as possible.
Core Tip: We retrospectively collected cases of testicular torsion surgery in adolescents at a tertiary hospital and found that the initial visit to a non tertiary hospital may delay the patient's diagnosis and optimal surgical time.
- Citation: Gang XH, Duan YY, Zhang B, Jiang ZG, Zhang R, Chen J, Teng XY, Zhang DB. Clinical characteristics of testicular torsion and factors influencing testicular salvage in children: A 12-year study in tertiary center. World J Clin Cases 2024; 12(7): 1251-1259
- URL: https://www.wjgnet.com/2307-8960/full/v12/i7/1251.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i7.1251
Testicular torsion (TT) is the most common acute scrotum injury worldwide and mainly occurs in children and adolescents, which causes restricted blood flow to the affected testis, resulting in testicular atrophy and testicular loss in adolescents. According to public data, the incidence of TT is estimated to be 1 in 4000 males aged < 25 years and 1 in 160 males aged > 25 years[1,2], and TT accounts for 13%–54% of cases of acute scrotal disease[3]. The incidence was high at 21.76 per 100000 population in 2010 in the country of Ireland, which has cold weather[4]. Currently, no drugs are effective for treating TT in humans, and the most effective treatment for TT is surgical exploration. However, delays in the diagnosis of TT result in loss of testes, subfertility, or infertility in patients[5]. TT is related to a variety of factors, the most important of which is the duration from testicular ischemia to surgery and the torsion angle[6-8]. In the current study, we reviewed patients who underwent orchiopexy or orchiectomy and were diagnosed with TT from 2011–2023 to summarize the clinical characteristics of TT and identify predictors of testicular salvage (TS) in patients.
After receiving Institutional Review Board approval from the Ethics Committee of Anhui Medical University Suzhou Hospital (A2023006), we queried a maintained database of patients who underwent scrotal exploration at a tertiary referral medicine center from January 2011 to July 2023. In the current study, 75 patients were enrolled. Prior to study commencement, we obtained informed consent from patients who were preoperatively diagnosed with TT using Doppler ultrasonography (D-USG) (Supplementary Figure 1). Even young children with small testes, where testicular blood flow is difficult to detect, undergo D-USG to prevent misdiagnosis. The exclusion criteria for the retrospective study included: (1) Patients younger than one year old; (2) Patients who had severe hepatic or renal dysfunction or heart disease; and (3) Patients who underwent scrotal surgery before TT.
The patient was placed in the supine position, and after anesthesia was administered, the scrotum on the affected side was opened, and a warm, damp gauze was placed on the testis. If no blood supply was restored to the testicle after 15-20 min, an orchiectomy was performed. If the testicular blood supply was restored and bright red blood was observed on the needle prick, bilateral orchiopexy was performed.
According to type of surgery, patients were divided into two groups: TS and Orchiectomy groups.
Categorical data were presented as numbers and percentages. Means and standard deviations were calculated for the continuous variables. Statistical analysis was performed using SPSS (version 22.0; IBM, Armonk, NY, United States). A student’s t-test was used to perform parametric comparisons of normally distributed data. The Mann–Whitney U test was used to compare means between non-normally distributed groups. Fisher’s exact test and chi-square test were used to compare categorical data between the two groups. Two-sided test values of P < 0.05 were considered statistically significant. To identify the predictive factors of orchiectomy and develop a novel predictive model, univariable and multivariable binary logistic regression analyses were used.
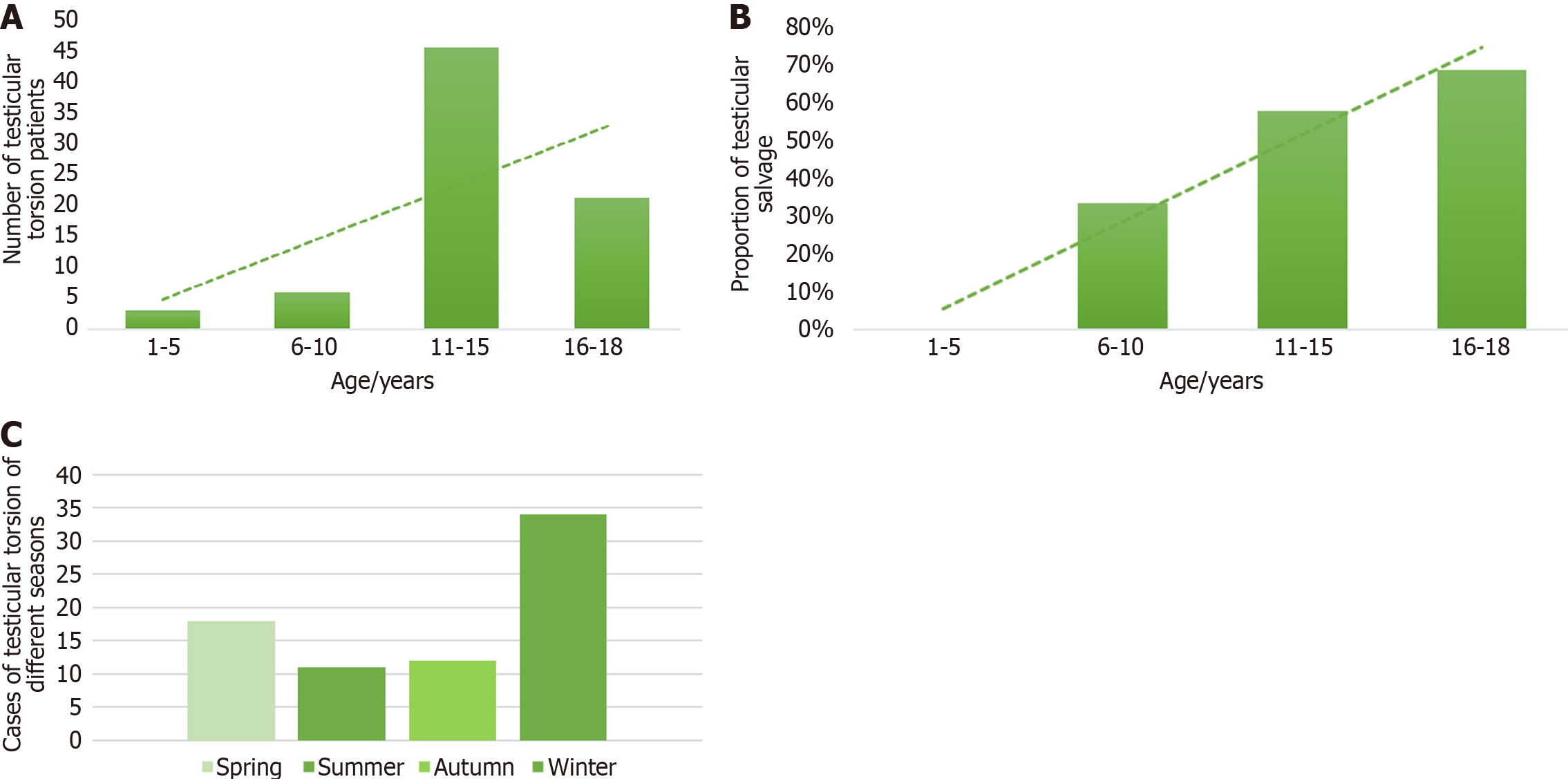
Patients with TT confirmed by Doppler ultrasound who were all minors aged 1–18 years were included in the study cohort, and we ultimately collected clinical information from 75 patients through the application of exclusion and inclusion criteria. Among them, 32 underwent orchiectomy, and TS occurred in 43 patients. The mean age of the Orchiectomy group was 12.53 ± 3.29 years younger than 14.42 ± 2.41 years in the TS group (Table 1). The peak TT rate was observed between 11–15 years old (Figure 1A). The probability of TS increased with age (Figure 1B). The incidence of TT was high in the winter (Figure 1C). Over 84% of the patients had testicular pain, and 10% had scrotal swelling. A previous history of TT occurred in only 5% of the patients. The time from the event to hospitalization ranged from 4–115 min. The twisted testicle side and location of the TT were comparable between the TS and Orchiectomy groups.
| Characteristic | Orchiectomy (n = 32) | Salvage (n = 43) | Total (n = 75) | P value |
| Age (yr), median (range) | 12.53 ± 3.29 (2-18) | 14.42 ± 2.41 (9-18) | 13.61 ± 2.97 (2-18) | 0.347 |
| BMI (kg/m2), mean ± SD | 18.75 ± 1.57 | 20.10 ± 1.97 | 19.53 ± 1.92 | P < 0.01 |
| Initial symptom | 0.662 | |||
| Testicular pain | 25 (78.13) | 38 (88.37) | 63 (84.00) | |
| Oscheocele | 5 (15.63) | 3 (6.97) | 8 (10.66) | |
| Nausea and vomiting | 1 (3.12) | 1 (2.33) | 2 (2.67) | |
| Others | 1 (3.12) | 1 (2.33) | 2 (2.67) | |
| Previous history of testicular torsion | 0.417 | |||
| No | 29 (90.63) | 41 (95.35) | 70 (93.33) | |
| Yes | 3 (9.37) | 2 (4.65) | 5 (6.67) | |
| Time from the event to the hospitalization (min), median (range) | 42 (4-115) | 37 (4-105) | 41 (4-115) | 0.791 |
| The side of the twisted testicle | 0.888 | |||
| Left | 25 (78.13) | 33 (76.74) | 58 (77.33) | |
| Right | 7 (21.87) | 10 (23.26) | 17 (22.67) | |
| Intratesticular blood flow | 0.657 | |||
| Invisible | 28 (87.50) | 39 (90.70) | 67 (89.33) | |
| Visible | 4 (12.50) | 4 (9.30) | 8 (10.66) | |
| Testicular parenchymal echotexture | 0.761 | |||
| Nonhomogeneous | 30 (93.75) | 41 (95.35) | 71 (94.67) | |
| Homogeneous | 2 (6.25) | 2 (4.65) | 4 (5.37) | |
| Location of testicular torsion | 0.739 | |||
| Intrathecal | 31 (96.88) | 41 (95.35) | 72 (96.00) | |
| Extrathecal | 1 (3.12) | 2 (4.65) | 3 (4.00) | |
| Torsion angle | 540 (90-1080) | 360 (45-720) | 540 (45-1080) | 0.49 |
| Testicular color of the affected testis | P < 0.01 | |||
| Black | 32 (100) | 30 (69.77) | 62 (82.67) | |
| Maroon | 0 | 7 (16.27) | 7 (9.33) | |
| Bright red | 0 | 5 (11.63) | 5 (6.67) | |
| Other | 0 | 1 (2.33) | 1 (1.33) | |
| Normal testicular fixation | 0.289 | |||
| No | 1 (3.12) | 4 (9.30) | 5 (6.67) | |
| Yes | 31 (96.88) | 39 (90.70) | 70 (93.33) | |
| Hospital stay time, median (range) | 4 (2-8) | 5 (1-9) | 5 (1-9) | 0.309 |
| Red blood cell count (109/L), mean ± SD | 4.58 ± 0.33 | 4.76 ± 0.35 | 4.69 ± 0.35 | 0.028 |
| White blood cell count (109/L), median (range) | 11.235 (5.16-19.31) | 11.06 (5.00-22.08) | 11.06 (5.00-22.08) | 0.894 |
| NLR, median (range) | 3.055 (0.96-8.90) | 5.28 (1.11-9.15) | 4.23 (0.96-9.15) | 0.014 |
| LMR, median (range) | 2.81 (0.49-6.14) | 2.89 (1.25-6.36) | 2.82 (0.49-6.36) | 0.894 |
When comparing the blood test results and testicular color of the affected testes, we found that all patients in the Orchiectomy group presented with a black color. The neutrophil-to-lymphocyte ratio (NLR) was higher in the Orchiectomy group than in the Salvage group.
We also compared differences between the Orchiectomy and Salvage groups. We find that the initial presenting institution accounts. More than 50% of the patients in the Orchiectomy group visited a primary hospital for the first time, while < 20% of the patients in the TS group visited a primary hospital (Table 2).
| Characteristic | Orchiectomy (n = 32) | Salvage (n = 43) | Total (n = 75) | P value |
| Season of events | 0.933 | |||
| Spring | 7 (21.87) | 11 (25.58) | 18 (24.00) | |
| Summer | 5 (15.63) | 6 (13.95) | 11 (14.67) | |
| Autumn | 6 (18.75) | 6 (13.95) | 12 (16.00) | |
| Winter | 14 (43.75) | 20 (46.52) | 34 (45.33) | |
| Patient's residence | 0.689 | |||
| Rural area | 9 (28.12) | 14 (32.56) | 23 (30.67) | |
| Urban area | 23 (71.88) | 29 (67.44) | 52 (69.33) | |
| Patient's guardian | 0.749 | |||
| Father | 13 (40.63) | 16 (37.21) | 29 (38.67) | |
| Mother | 10 (31.25) | 17 (39.53) | 27 (36.00) | |
| Other | 9 (28.12) | 10 (23.26) | 19 (25.33) | |
| Initial presenting institution | P < 0.01 | |||
| Primary hospital | 18 (56.25) | 8 (18.60) | 26 (34.67) | |
| Tertiary hospital | 14 (43.75) | 35 (81.49) | 49 (65.33) | |
| Median treatment cost [United States dollars, median (range)] | 764.085 (526.75-1266.32) | 726.19 (381.04-1363.83) | 736.79 (381.04-1363.83) | 0.739 |
Interestingly, we found that over 80% of the patients in the Salvage group were sent to tertiary hospitals, while only 65% of the patients in the Orchiectomy group were sent to tertiary hospitals. The guardian type (father or mother) and residence (urban or rural) of the children had no predictive effect on testicular salvage.
Univariate analysis showed that age, body mass index, torsion angle, red blood cell count, NLR, and the initial presenting institution were predictive of orchiectomy (Table 3). Univariate and subsequent multivariate logistic regression analyses showed that the initial presenting institution correlated with the risk of a salvageable testis (Table 3).
| Characteristic | Univariate analysis | Multivariate analysis | ||
| OR (95%CI) | P value | OR (95%CI) | P value | |
| Age (yr), median (range) | 1.16 (0.977-1.378) | 0.09 | ||
| BMI (kg/m2), mean ± SD | 1.54 (1.14-2.06) | < 0.01 | 1.24 (0.46-3.39) | 0.669 |
| Initial symptom | ||||
| Testicular pain | Ref | |||
| Scrotal swelling | 0.39 (0.09-1.80) | 0.230 | ||
| Nausea and vomiting | 0.66 (0.04-11.01) | 0.771 | ||
| Other | 0.66 (0.04-11.01) | 0.771 | ||
| Previous history of testicular torsion | ||||
| No | Ref | |||
| Yes | 0.72 (0.14-3.85) | 0.706 | ||
| Time from the event to the hospitalization (min), median (range) | 0.99 (0.97-1.01) | 0.423 | ||
| The side of the twisted testicle | ||||
| Left | Ref | |||
| Right | 1.08 (0.36-3.24) | 0.888 | ||
| Intratesticular blood flow | ||||
| Invisible | Ref | |||
| Visible | 0.72 (0.17-3.12) | 0.658 | ||
| Testicular parenchymal echotexture | ||||
| Nonhomogeneous | Ref | |||
| Homogeneous | 0.73 (0.10-5.49) | 0.761 | ||
| Operative time (min), median (range) | 0.98 (0.95-1.00) | 0.073 | ||
| Location of testicular torsion | ||||
| Intrathecal | Ref | |||
| Extrathecal | 1.51 (0.13-17.44) | 0.740 | ||
| Torsion angle | 1.00 (0.99-1.00) | < 0.05 | ||
| Testicular color of the affected testis | ||||
| Black | Ref | |||
| Maroon | 123358712.82 (0.00-Inf) | 0.994 | ||
| Bright red | 123358712.25 (0.00-Inf) | 0.995 | ||
| Other | 123358712.35 (0.00-Inf) | 0.998 | ||
| Normal testicular fixation | ||||
| No | Ref | |||
| Yes | 0.31 (0.03-2.96) | 0.312 | ||
| Hospital stay time, median (range) | 1.18 (0.96-1.44) | 0.112 | ||
| Red blood cell count (109/L), mean ± SD | 5.27 (1.18-23.57) | < 0.05 | 6.00 (0.10-348.34) | 0.387 |
| White blood cell count (109/L), median (range) | 0.98 (0.86-1.13) | 0.811 | ||
| NLR, median (range) | 1.34 (1.08-1.67) | < 0.01 | 3.78 (0.96-14.91) | 0.057 |
| LMR, median (range) | 1.21 (0.85-1.73) | 0.285 | ||
| Season of events | ||||
| Spring | Ref | |||
| Summer | 0.76 (0.17-3.49) | 0.728 | ||
| Autumn | 0.64 (0.15-2.78) | 0.548 | ||
| Winter | 0.91 (0.28-2.92) | 0.873 | ||
| Patient's residence | ||||
| Rural area | Ref | |||
| Urban area | 0.81 (0.30-2.20) | 0.681 | ||
| Patient's guardian | ||||
| Father | Ref | |||
| Mather | 1.38 (0.47-4.03) | 0.554 | ||
| Other | 0.90 (0.28-2.88) | 0.863 | ||
| Initial diagnosis institution | ||||
| Primary hospital | Ref | Ref | ||
| Tertiary hospital | 5.62 (1.99-15.88) | < 0.01 | 12.58 (1.12-141.05) | < 0.05 |
| Median treatment cost [United States dollars, median (range)] | 1.00 (1.00-1.00) | 0.650 | ||
TT is a common urological emergency in adolescents that often results in testicular loss, decreased fertility, and even loss of fertility if the diagnosis and management of TT are delayed. It has been reported that the overall incidence is approximately 4 in 100000 people worldwide, with a higher incidence of TT in Ireland, between 16.8 and 26.3[4]. At present, the initial causes of TT remain unknown, and mouse models have been used to study the causes of TT and protective factors of TT[9]. Some researchers have reported that TT causes dysfunction in mitochondrial oxidative phosphorylation[10] and that Insl3 could be a protective factor against TT[11]. Which clinical characteristics predict a higher risk for testicular orchiectomy? In the Orchiectomy group in our study, the testicular color was black, and the NLR was higher than that in the TS group. Multiple studies have also reported that torsion grade is associated with testicular vitality[12-14]. In this study, the degree of torsion was associated with TS. The median torsion grade was 568.12 ± 195.501 in the Orchiectomy group compared to 425.93 ± 235.747 in the TS group. Recently, Delgado-Miguel et al[15] confirmed that laboratory tests of the NLR should be considered a predictor of pediatric TT in cases with clinical and ultrasound suspicion, which may help anticipate the urgent surgical treatment required in these patients[15]. Therefore, testicular color, torsion grade, and laboratory tests will help urologists judge the severity of TT.
TT is a urological emergency; therefore, social factors may delay the diagnosis and treatment of patients with TT. Accurate and prompt diagnosis and surgical treatment are important for TS. TT can occur at any age, but teenagers are the main victims, especially children who are 12–16 years old[16]. Similarly, we found that patients aged 11–15 account for 60% of the cohort (Figure 1A). We found a correlation between age and TS, with younger children being more likely to undergo orchiectomy. This may be because younger children are unable to judge the severity of pain and accurately describe pain symptoms in words[17]. Similarly, Bayne et al[18] reported that misdiagnosed patients tended to be younger and more likely to have developmental, cognitive, or social disorders than those in an acute setting[18].
In addition to young age and atypical symptoms, what factors could lead to a delay in TT and failure of TS? In our study, we found that the initial presenting institution was important. TT is a urology emergency; therefore, sociological characteristics, such as tertiary hospital location, were also considered. Univariate and multivariate logistic regression analyses in the current study showed that only patients who visited the tertiary facility shortly after symptom onset had a higher salvage rate, which was similar to research in Brazil[19]. Tertiary hospitals often have better Doppler ultrasound equipment, more experienced ultrasound diagnosticians, and urologists at higher levels, which results in lower rates of misdiagnosis. In 2016, Douglas pointed out the inclination to refer adolescent patients with TT away from regional hospitals to a tertiary pediatric center and experienced urologists[20]. However, in northern and central China, many children live in rural areas far from tertiary hospitals in cities, which often causes delays in TT treatment.
In addition to preventing delays in diagnosis, we must avoid long durations before surgery. If patients with TT are diagnosed and treated promptly, the probability of testicular loss will decrease significantly. The “golden six-hour” window for TT treatment signifies that if patients reach the hospital within six hours of symptom onset, the salvage incidence can reach 90%[21]. Dias Filho et al[19] reported that presentation delay was a significant predictor of orchiectomy[19]. If surgical exploration is delayed, the TS rate decreases to 50% when symptoms last beyond 12 h. When symptoms last for over 24 h, the TS rate is reduced to less than 10%[22].
TT often occurs in cold weather at low temperatures. In cold zone countries, such as Ireland and Canada, the incidence rate of TT is relatively higher than that in other countries[4,23,24]. Even in tropical countries, TT follows a seasonal pattern and is more frequent in the colder months of the year[25]. Why do low temperatures cause TT? Researchers have suggested that contraction of the cremasteric muscle at low temperatures increases the risk of TT[26]. In Japan, researchers found that over 70% of TT cases occurred in winter[27], and in Brazil, the TT incidence was higher in the southern area than in the northern area (the cold zone in the south)[24]. According to a report in Taiwan, 73.7% of the patients had TT when the diurnal temperature change was ≥ 6°C. Compared to the torsion rate for diurnal temperature changes < 6°C, the relative risk of TT at ≥ 6 °C was 1.8 (P < 0.05)[28]. This finding is similar to the results of the present study. We found that TT occurred more frequently in winter than in the other seasons, and winter was the season with the most severe temperature changes in northern and central China.
From the perspective of disease characteristics, the degree of TT and laboratory indicators of blood tests affect the success rate of TS in TT. However, it should be noted that TT is a urologic emergency, and the delay in diagnosis due to sociological characteristics leads to the loss of testes. In rural areas or small towns, the lack of tertiary hospitals causes delays in diagnosis. Therefore, for better treatment, we should popularize emergency knowledge among parents and children[29], and provide corresponding diagnosis and treatment training for doctors in rural areas to avoid misdiagnosis of TT.
This study has several limitations. First, it is a retrospective study, which is subject to selection bias. Secondly, the study is single-centered with a limited number of cases included. In the future, larger-scale multicenter studies will be needed to identify factors that influence the outcomes of TT.
The initial presenting institution has a predictive value for predicting outcomes in children with acute TT. Children with scrotal pain should be referred to a tertiary hospital as soon as possible for an accurate diagnosis and timely surgery.
Testicular torsion (TT) is currently the leading cause of testicular removal in adolescents, with an incidence rate of 1 in 4000 among males under the age of 25. Delayed medical consultation for TT and misdiagnosis could lead to orchiectomy. Therefore, we aim to analyze the factors influencing orchiectomy or testicular salvage by reviewing the data of patients who presented at our center.
Various factors, such as delayed presentation to the healthcare facility and excessive degree of torsion, can lead to orchiectomy in adolescents with TT. Hence, we conducted a retrospective analysis of data from our center to identify the factors affecting the prognosis of TT.
Factors to predict the possibility of testicular salvage (TS) in patients with TT in our tertiary center.
By collecting clinical data from patients with TT treated at our center, we performed univariate and multivariate regression analyses to compare between the TS and the orchiectomy group.
Our study has identified that younger age, body mass index, torsion angle, red blood cell count and neutrophil-to-lymphocyte ratio have predictive value for TS. And we found a new factor that the type of institution where patients first presented as a predictive factor for the outcome of TT; patients who initially presented to a tertiary-care hospital were more likely to have testicular preservation.
The initial presenting institution is a new predictive factor for outcome of TT. Patients with scrotal pain should be presented to a tertiary hospital as soon as possible.
Future research will focus on enhancing public health education regarding scrotal emergencies to prevent delays in the presentation of patients with conditions such as TT.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Arslan M, Turkey; Govindarajan KK, India S-Editor: Li L L-Editor: A P-Editor: Zhao S
| 1. | Mansbach JM, Forbes P, Peters C. Testicular torsion and risk factors for orchiectomy. Arch Pediatr Adolesc Med. 2005;159:1167-1171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 121] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 2. | Barada JH, Weingarten JL, Cromie WJ. Testicular salvage and age-related delay in the presentation of testicular torsion. J Urol. 1989;142:746-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 128] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | McAndrew HF, Pemberton R, Kikiros CS, Gollow I. The incidence and investigation of acute scrotal problems in children. Pediatr Surg Int. 2002;18:435-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 76] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Sugrue DD, O'Connor E, Davis N. Testicular torsion in Ireland: a 10-year analysis of incidence and risk of orchidectomy. Ir J Med Sci. 2022;191:2267-2274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Henning J, Waxman S. Legal aspects of men's genitourinary health. Int J Impot Res. 2009;21:165-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Sessions AE, Rabinowitz R, Hulbert WC, Goldstein MM, Mevorach RA. Testicular torsion: direction, degree, duration and disinformation. J Urol. 2003;169:663-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 24] [Reference Citation Analysis (0)] |
| 7. | Zvizdic Z, Aganovic A, Milisic E, Jonuzi A, Zvizdic D, Vranic S. Duration of symptoms is the only predictor of testicular salvage following testicular torsion in children: A case-control study. Am J Emerg Med. 2021;41:197-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 8. | Turner TT, Bang HJ, Lysiak JL. The molecular pathology of experimental testicular torsion suggests adjunct therapy to surgical repair. J Urol. 2004;172:2574-2578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 97] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 9. | Minas A, Mahmoudabadi S, Gamchi NS, Antoniassi MP, Alizadeh A, Bertolla RP. Testicular torsion in vivo models: Mechanisms and treatments. Andrology. 2023;11:1267-1285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 18] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 10. | Shih HJ, Chang CY, Huang IT, Tsai PS, Han CL, Huang CJ. Testicular torsion-detorsion causes dysfunction of mitochondrial oxidative phosphorylation. Andrology. 2021;9:1902-1910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Sozubir S, Barber T, Wang Y, Ahn C, Zhang S, Verma S, Lonergan D, Lorenzo AJ, Nef S, Baker LA. Loss of Insl3: a potential predisposing factor for testicular torsion. J Urol. 2010;183:2373-2379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Feng S, Yang H, Lou Y, Ru W, Wang A, Liu W. Clinical Characteristics of Testicular Torsion and Identification of Predictors of Testicular Salvage in Children: A Retrospective Study in a Single Institution. Urol Int. 2020;104:878-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Visser AJ, Heyns CF. Testicular function after torsion of the spermatic cord. BJU Int. 2003;92:200-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 173] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 14. | Paltiel HJ, Estrada CR Jr, Alomari AI, Stamoulis C, Passerotti CC, Meral FC, Lee RS, Clement GT. Multi-planar dynamic contrast-enhanced ultrasound assessment of blood flow in a rabbit model of testicular torsion. Ultrasound Med Biol. 2014;40:361-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Delgado-Miguel C, García A, Muñoz-Serrano AJ, López-Pereira P, Martínez-Urrutia MJ, Martínez L. The role of neutrophil-to-lymphocyte ratio as a predictor of testicular torsion in children. J Pediatr Urol. 2022;18:697.e1-697.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 16. | Srinivasan A, Cinman N, Feber KM, Gitlin J, Palmer LS. History and physical examination findings predictive of testicular torsion: an attempt to promote clinical diagnosis by house staff. J Pediatr Urol. 2011;7:470-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 17. | Yu C, Zhao J, Lu J, Wei Y, Jiang L, Zhao T, Lin T, He D, Wen S, Wu S, Wei G. Demographic, clinical, and socioeconomic factors associated with delayed diagnosis and management of pediatric testicular torsion in West China: a retrospective study of 301 cases in a single tertiary children's hospital. BMC Pediatr. 2021;21:553. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Bayne CE, Villanueva J, Davis TD, Pohl HG, Rushton HG. Factors Associated with Delayed Presentation and Misdiagnosis of Testicular Torsion: A Case-Control Study. J Pediatr. 2017;186:200-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 19. | Dias Filho AC, Maroccolo MVO, Ribeiro HP, Riccetto CLZ. Presentation delay, misdiagnosis, inter-hospital transfer times and surgical outcomes in testicular torsion: analysis of statewide case series from central Brazil. Int Braz J Urol. 2020;46:972-981. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Husmann DA. Who Should be Taking Care of Adolescent Testicular Torsion? J Urol. 2017;197:282-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Mäkelä E, Lahdes-Vasama T, Rajakorpi H, Wikström S. A 19-year review of paediatric patients with acute scrotum. Scand J Surg. 2007;96:62-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 84] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 22. | Günther P, Rübben I. The acute scrotum in childhood and adolescence. Dtsch Arztebl Int. 2012;109:449-57; quiz 458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 23. | Preshaw RM. Seasonal frequency of testicular torsion. Can J Surg. 1984;27:404-405. [PubMed] |
| 24. | Korkes F, Cabral PR, Alves CD, Savioli ML, Pompeo AC. Testicular torsion and weather conditions: analysis of 21,289 cases in Brazil. Int Braz J Urol. 2012;38:222-8; discussion 228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 25. | Gomes Dde O, Vidal RR, Foeppel BF, Faria DF, Saito M. Cold weather is a predisposing factor for testicular torsion in a tropical country. A retrospective study. Sao Paulo Med J. 2015;133:187-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 26. | Shukla RB, Kelly DG, Daly L, Guiney EJ. Association of cold weather with testicular torsion. Br Med J (Clin Res Ed). 1982;285:1459-1460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Hoshino H, Abe T, Watanabe H, Katsuoka Y, Kawamura N. [Correlation between atmospheric temperature and testicular torsion]. Hinyokika Kiyo. 1993;39:1031-3; discussion 1033. [PubMed] |
| 28. | Chen JS, Lin YM, Yang WH. Diurnal temperature change is associated with testicular torsion: a nationwide, population based study in Taiwan. J Urol. 2013;190:228-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 29. | Yap LC, Keenan R, Khan J, Cozman C, Dowling C, Cullen I, Darcy F. Parental awareness of testicular torsion amongst Irish parents. World J Urol. 2018;36:1485-1488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |