Published online Sep 26, 2024. doi: 10.12998/wjcc.v12.i27.6105
Revised: June 21, 2024
Accepted: July 10, 2024
Published online: September 26, 2024
Processing time: 185 Days and 13.4 Hours
The coexistence of esophageal variceal bleeding and superficial esophageal cancer (SEC) is relatively rare in clinical practice. Moreover, there have been few reports of SEC overlying esophageal varices (EVs). Herein, we report our successful use of endoscopic submucosal dissection (ESD), esophageal solitary venous dilatation (ESVD), and endoscopic injection sclerotherapy (EIS) to treat a 75-year-old man who was diagnosed with SEC coexisting with esophageal variceal bleeding.
A 75-year-old man was admitted to the hospital due to black stool for 4 days. The patient had a history of liver cancer, cirrhosis, and portal hypertension. Endosco
The sequential treatment of ESVD, EIS, and ESD is an effective method for trea
Core Tip: Esophageal varices (EVs) with bleeding and superficial esophageal cancer (SEC) are two different diseases. Their coexistence is rare in clinical practice. Endoscopic submucosal dissection (ESD) for SEC with EVs is one of the most challenging endoscopic procedures due to the high risk of bleeding and fibrosis caused by prior treatment. We report on a 75-year-old man with “black stool”. He had a history of cirrhosis and portal hypertension. After esophageal solitary venous dilatation and endoscopic injection sclerotherapy, ESD was successfully performed without significant complications, and the SEC was treated by R0 resection. This method may become the mainstream treatment for EVs with SEC.
- Citation: Xu L, Chen SS, Yang C, Cao HJ. Successful endoscopic treatment of superficial esophageal cancer in a patient with esophageal variceal bleeding: A case report. World J Clin Cases 2024; 12(27): 6105-6110
- URL: https://www.wjgnet.com/2307-8960/full/v12/i27/6105.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i27.6105
Esophageal variceal bleeding and superficial esophageal cancer (SEC) are two different diseases whose coexistence is relatively rare in clinical practice. The Japanese Esophageal Society defines SEC as a tumor limited to the mucosal layer (T1a) and submucosal layer (T1b), regardless of the presence of lymph node or distant organ metastasis[1]. Middle-to-late-stage esophageal cancer is often treated by surgery, radiotherapy, or combination therapy. For SECs staged clinically as cT1N0M0, the traditional treatment option is esophagectomy, but this causes significant surgical trauma. During the last few years, immunotherapy has emerged. Although the antitumor efficacy of immune checkpoint inhibitors is significant, it is also associated with a higher risk of all-grade and grades 3-4 hypertransaminasemia[2-4]. In recent years, endoscopic resection has gradually become the preferred treatment for some SECs due to its safety, effectiveness, and minimal invasiveness, especially its preservation of the esophagus and being more physiologically aligned[5-8]. Eso
A 75-year-old man was admitted to the hospital due to black stool for 4 d.
The patient had been diagnosed with liver cirrhosis 6 years earlier and mixed left liver cancer (hepatocellular carcinoma and hepatobiliary cell carcinoma) 3 years earlier.
The patient’s surgical history included surgery for left liver cancer before admission and transcatheter arterial chemoembolization after the operation. The patient was followed up regularly for 3 years. There was no recurrence of the tumor during that period.
The patient had a history of smoking and drinking but had quit smoking for 6 years. The patient’s family history was unremarkable.
At admission, the vital signs were as follows: Body temperature, 36.3 °C; pulse, 108/min; respiratory rate, 76 per minute; and blood pressure, 102/58 mmHg. The abdomen was distended with prominent abdominal varicose veins. On pal
Blood parameters were: Hemoglobin, 102 g/L; platelet count, 99 × 109/L. The fecal occult blood test was positive.
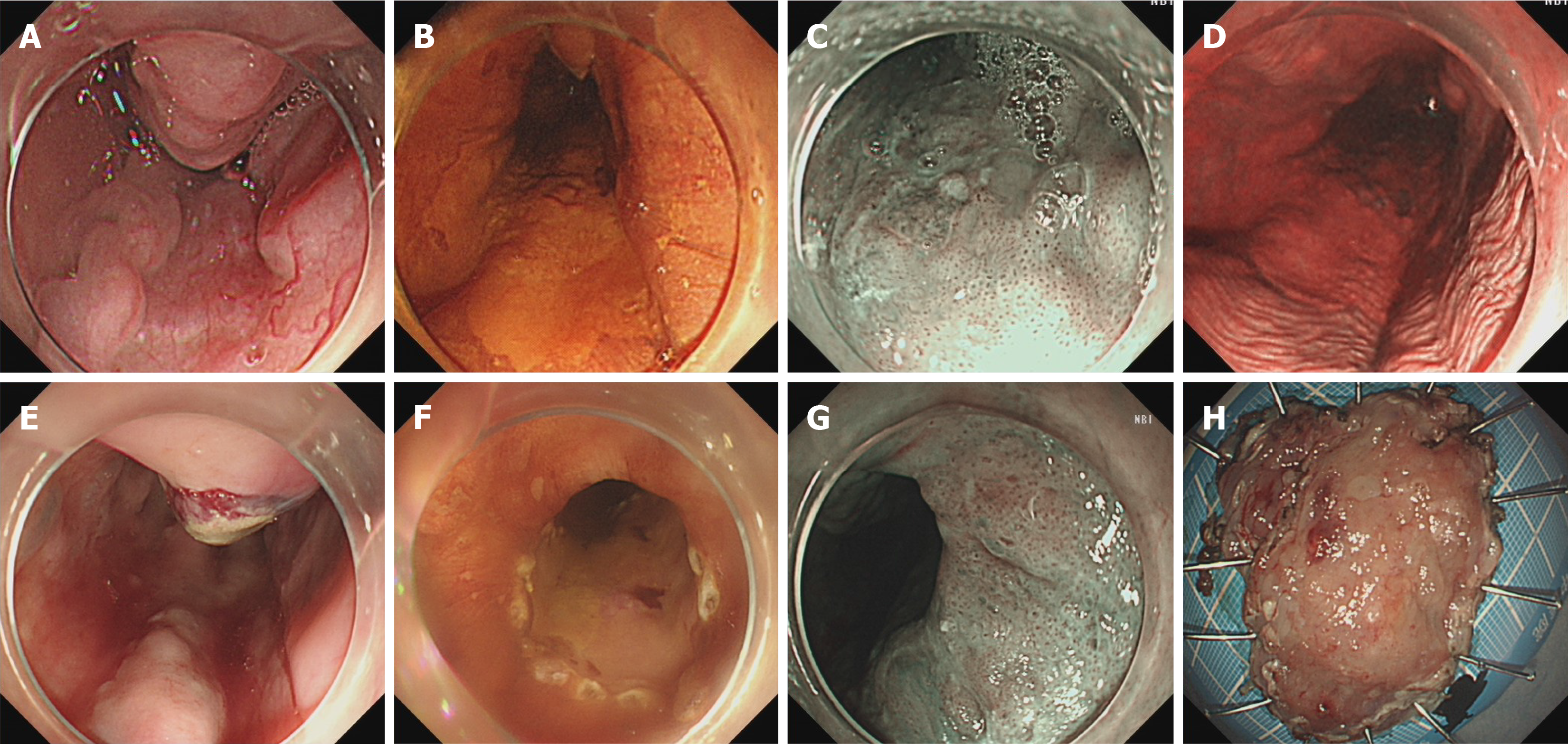
Endoscopy revealed three EVs with a diameter of approximately 0.6 cm, with a red color sign, and the patient was diagnosed with LemigfD1Rf1. Narrow-band imaging with magnifying endoscopy (NBI-ME) revealed that a type IIb lesion was located in the inferior region of the esophagus, was pink in color, and could not be stained with iodine (Figure 1A-D).
Bleeding of SEC coexisting with EVs.
We performed ESVD and EIS to deal with the bleeding of the EVs and performed a biopsy on the lesion, which we co
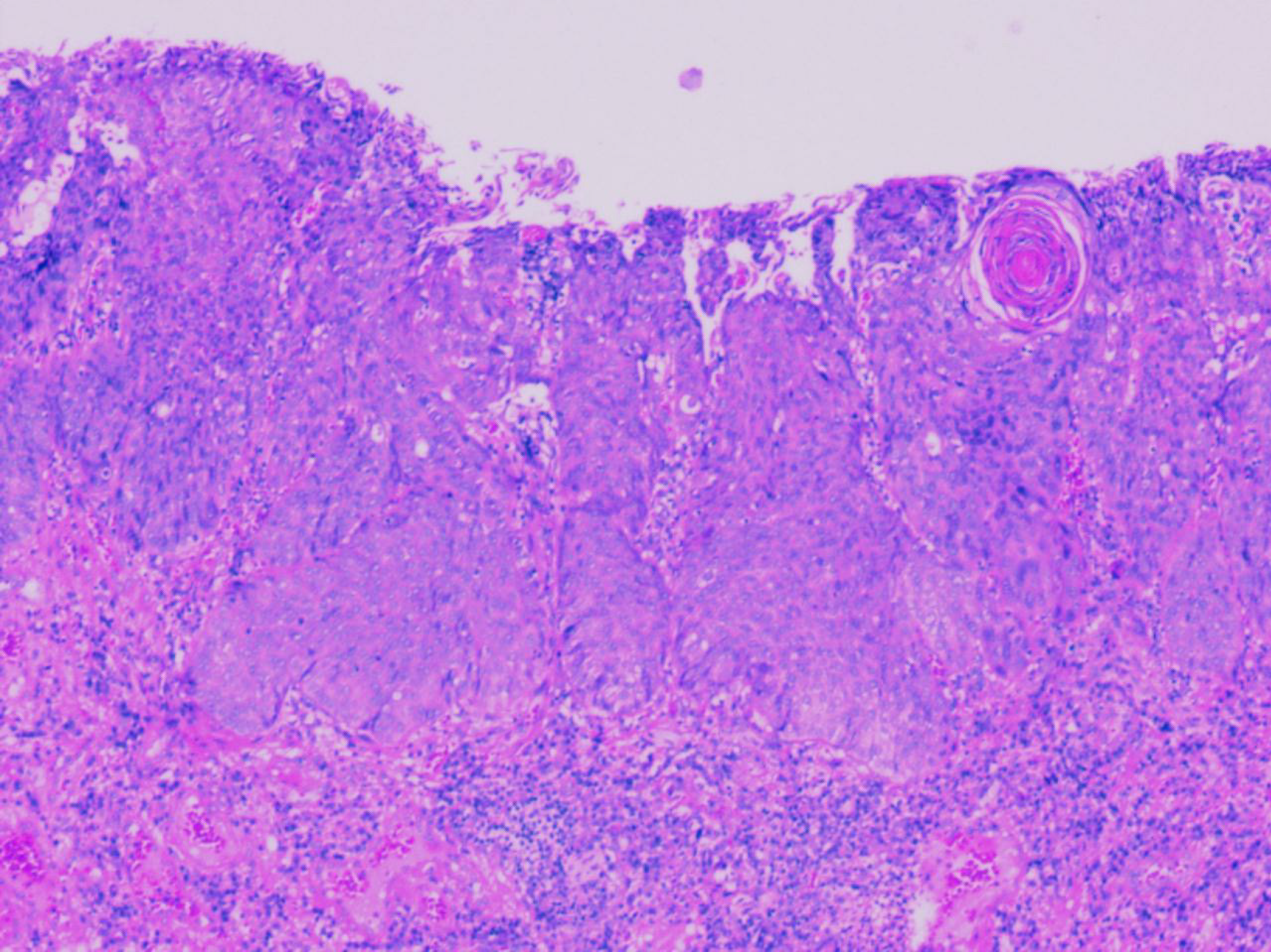
After 7 d of conservative treatment, the patient had no obvious hemorrhage, pain, emesis, or any other clinical symptoms. The final pathological results were as follows (Figure 2): (1) Histological type: 0-IIa + IIb type squamous cell carcinoma with moderate differentiation; (2) Specimen size: 4.2 cm × 1.8 cm; (3) Depth of infiltration: Mucous membrane (MM); (4) Scar and vascular infiltration: (-); (5) Cutting margin: Horizontal (-) and vertical (-); and (6) Immunohistochemical staining: Desmin (smooth muscle +), CD31 (vascular endothelium, +), Ki-67 (30%, +), p53 (80%, +), P63 (+), and CK34βE12 (+).
After 3 mo of postoperative follow-up, the wound was repaired well by gastroscopy, and there was no bleeding during the one-year follow-up (Figure 3).
The coexistence of EVs bleeding and SEC is relatively rare in clinical practice, and most cases of esophageal cancer are in the late stage at diagnosis. Therefore, in the process of endoscopy, patients whose esophageal varicose veins are located still need to be carefully scanned. Erosive lesions and protrusive lesions of the esophagus may constitute the early stage of esophageal cancer. The risk of surgical treatment for patients with cirrhosis and esophageal cancer is extremely high. Serious complications, such as anastomotic fistula, chylothorax, and liver function failure, occur frequently[9], result in a very high death rate. In recent years, there have been some case reports of cirrhosis combined with bleeding of EVs in SEC patients, indicating that minimally invasive endoscopic treatments, such as ESD and EMR, are associated with better results with fewer complications[10]. Although the treatment steps may seem clear, many issues still need to be explored. Bleeding and fibrotic adhesions are the most common problems encountered during the ESD procedure[11]. One of the reasons for the observed bleeding may be related to the patient’s concurrent presence of gastric varicose veins, which were not treated properly. For this patient, we used ESVD to treat the gastric varicose veins, resulting in less bleeding during ESD. The liver function status of patients is also worthy of attention. Esophagectomy in patients with cirrhosis has been reported to result in a higher rate of complications and mortality than surgery in patients without cirrhosis[12]. Liver cirrhosis patients with Child-Pugh class A liver function may be more suitable for ESD. Fibrotic adhesions may cause the piecemeal resection, which is thought to be due to the fibrosis caused by EIS[11]. Tahara et al[13] reported that APC may be an option for treating ESCC that is evaluated endoscopically within the mucosa and is difficult to safely treat with ESD. However, APC differs from ESD and surgical esophagectomy because it does not allow histopathological evaluation of ESCC, and careful follow-up is necessary. TIPS may also be effective as an EV treatment that does not affect the ESD in patients with SESCC[14]. ESD can be used to pathologically evaluate the depth of lesions, and it is the first choice for ESCC treatment. There are still many issues that need further attention: What is the best time interval between EIS and ESD? How can the risk of postoperative bleeding be assessed for such patients? Will there be a higher risk of bleeding from recurrent variceal rupture in the ESD resection area? How can esophageal stenosis after ESD combined with varicose veins be treated?
Esophageal variceal bleeding is a common complication of liver cirrhosis, but its coexistence with esophageal cancer is relatively rare. Varices are prone to bleeding, and patients with liver cirrhosis have poor coagulation function, making it difficult to tolerate surgical intervention. Therefore, for patients with early-stage esophageal cancer, endoscopic treatment after ESVD and EIS of varicose veins is a feasible method.
We would like to thank Mr. Zhang Shuo for his support and help with the care of the patient.
| 1. | Japan Esophageal Society. Japanese Classification of Esophageal Cancer, 11th Edition: part I. Esophagus. 2017;14:1-36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 479] [Cited by in RCA: 708] [Article Influence: 88.5] [Reference Citation Analysis (1)] |
| 2. | Dall'Olio FG, Rizzo A, Mollica V, Massucci M, Maggio I, Massari F. Immortal time bias in the association between toxicity and response for immune checkpoint inhibitors: a meta-analysis. Immunotherapy. 2021;13:257-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 104] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 3. | Rizzo A, Mollica V, Tateo V, Tassinari E, Marchetti A, Rosellini M, De Luca R, Santoni M, Massari F. Hypertransaminasemia in cancer patients receiving immunotherapy and immune-based combinations: the MOUSEION-05 study. Cancer Immunol Immunother. 2023;72:1381-1394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 120] [Reference Citation Analysis (0)] |
| 4. | Guven DC, Sahin TK, Erul E, Rizzo A, Ricci AD, Aksoy S, Yalcin S. The association between albumin levels and survival in patients treated with immune checkpoint inhibitors: A systematic review and meta-analysis. Front Mol Biosci. 2022;9:1039121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 144] [Article Influence: 48.0] [Reference Citation Analysis (0)] |
| 5. | Ishihara R, Arima M, Iizuka T, Oyama T, Katada C, Kato M, Goda K, Goto O, Tanaka K, Yano T, Yoshinaga S, Muto M, Kawakubo H, Fujishiro M, Yoshida M, Fujimoto K, Tajiri H, Inoue H; Japan Gastroenterological Endoscopy Society Guidelines Committee of ESD/EMR for Esophageal Cancer. Endoscopic submucosal dissection/endoscopic mucosal resection guidelines for esophageal cancer. Dig Endosc. 2020;32:452-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 262] [Article Influence: 52.4] [Reference Citation Analysis (0)] |
| 6. | Sgourakis G, Gockel I, Lang H. Endoscopic and surgical resection of T1a/T1b esophageal neoplasms: a systematic review. World J Gastroenterol. 2013;19:1424-1437. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 90] [Cited by in RCA: 101] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 7. | Tsujii Y, Nishida T, Nishiyama O, Yamamoto K, Kawai N, Yamaguchi S, Yamada T, Yoshio T, Kitamura S, Nakamura T, Nishihara A, Ogiyama H, Nakahara M, Komori M, Kato M, Hayashi Y, Shinzaki S, Iijima H, Michida T, Tsujii M, Takehara T. Clinical outcomes of endoscopic submucosal dissection for superficial esophageal neoplasms: a multicenter retrospective cohort study. Endoscopy. 2015;47:775-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 157] [Article Influence: 15.7] [Reference Citation Analysis (1)] |
| 8. | McCarty JC, Parker RK, Vidri RJ, Robinson KA, Lipsitz S, Gangadharan SP, Iyer PG. A retrospective cohort study of endoscopic therapy and esophagectomy for stage 1 esophageal cancer: less is more. Gastrointest Endosc. 2020;92:23-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Lu MS, Liu YH, Wu YC, Kao CL, Liu HP, Hsieh MJ. Is it safe to perform esophagectomy in esophageal cancer patients combined with liver cirrhosis? Interact Cardiovasc Thorac Surg. 2005;4:423-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Ciocîrlan M, Chemali M, Lapalus MG, Lefort C, Souquet JC, Napoléon B, Ponchon T. Esophageal varices and early esophageal cancer: can we perform endoscopic mucosal resection (EMR)? Endoscopy. 2008;40 Suppl 2:E91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Toya Y, Hatta W, Shimada T, Matsuhashi T, Shiroki T, Sasaki Y, Tatsuta T, Nakamura J, Hanabata N, Horikawa Y, Nagino K, Koike T, Masamune A, Harada Y, Ohira T, Iijima K, Abe Y, Hikichi T, Igarashi S, Fushimi S, Takeda H, Fukuda S, Matsumoto T; Tohoku GI Endoscopy Group. Clinical outcomes of endoscopic submucosal dissection for esophageal squamous cell carcinoma with esophageal varices: Multicenter retrospective study. Dig Endosc. 2024;36:314-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Valmasoni M, Pierobon ES, De Pasqual CA, Zanchettin G, Moletta L, Salvador R, Costantini M, Ruol A, Merigliano S. Esophageal Cancer Surgery for Patients with Concomitant Liver Cirrhosis: A Single-Center Matched-Cohort Study. Ann Surg Oncol. 2017;24:763-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Tahara K, Tanabe S, Ishido K, Higuchi K, Sasaki T, Katada C, Azuma M, Nakatani K, Naruke A, Kim M, Koizumi W. Argon plasma coagulation for superficial esophageal squamous-cell carcinoma in high-risk patients. World J Gastroenterol. 2012;18:5412-5417. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Xu ZG, Zhao YB, Yu J, Bai JY, Liu E, Tang B, Yang SM. Novel endoscopic treatment strategy for early esophageal cancer in cirrhotic patients with esophageal varices. Oncol Lett. 2019;18:2560-2567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |