Published online Sep 16, 2024. doi: 10.12998/wjcc.v12.i26.5990
Revised: June 8, 2024
Accepted: July 3, 2024
Published online: September 16, 2024
Processing time: 95 Days and 16.6 Hours
Extragastrointestinal stromal tumors (EGIST) and gastrointestinal stromal tumors are of similar pathological type and form. Here we report a rare case of EGIST diffusely distributed in membranous tissue in abdominal cavity, the feature of which included diffuse tumors at membranous tissue in entire abdominal cavity and spontaneous bleeding of the tumors.
The patient was a 71-year man and hospitalized due to continuous pain at lower abdomen for more than 10 days. Upon physical examination, the patient had flat and tough abdomen with mild pressing pain at lower abdomen, no obvious abdominal mass was touchable, and shifting dullness was positive. Positron emission tomography-computed tomography (CT) showed that in his peritoneal cavity, there were multiple nodules of various sizes, seroperitoneum, multiple enlarged lymph nodes in abdominal/pelvic cavity and right external ilium as well as pulmonary nodules. Plain CT scanning at epigastrium/hypogastrium/pelvic cavity + enhanced three-dimensional reconstruction revealed multiple soft tissue nodules in abdominal/pelvic cavity, peritoneum and right groin. Tumor marker of carbohydrate antigen 125 was 808 U/mL, diffuse tuberous tumor was seen in abdominal/pelvic cavity during operation with hematocelia, and postoperative pathological examination confirmed EGIST. Imatinib was administered with better therapeutic effect.
Gene testing showed breast cancer susceptibility gene 1 interacting protein C-terminal helicase 1 and KIT genovariation, and the patient was treated with imatinib follow-up visit found that his clinical symptoms disappeared and the tumor load alleviated obviously via imageological examination.
Core Tip: Extragastrointestinal stromal tumors (EGIST) are less common in comparison with gastrointestinal stromal tumors. EGIST tumors in the membranous tissue are rare and tumors independently developing in membrane tissues such as greater omentum, mesentery or peritoneum are occasionally reported. Diffuse membranous tumor in entire abdominal cavity is extremely rare worldwide. We report a case of EGIST with the tumors like cobblestone being diffusely distributed in entire abdominal cavity accompanied by spontaneous bleeding. The tumors may not be fully resected by surgery, hence we made biopsy, pathological examination and gene detection to determine the therapy. Treatment with imatinib achieved better outcome.
- Citation: Xu JD, Wang Z, Zhou Q, Meng N, Zhang SM, Liu N. Extragastrointestinal stromal tumors with diffuse membranous distribution with bleeding: A case report. World J Clin Cases 2024; 12(26): 5990-5997
- URL: https://www.wjgnet.com/2307-8960/full/v12/i26/5990.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i26.5990
Extragastrointestinal stromal tumors (EGIST) are less common compared with gastrointestinal stromal tumors (GIST). The tumor developing in membranous tissue is rare and independently developing in membrane tissues such as greater omentum, mesentery or peritoneum has been occasionally reported. Diffuse membranous tumor in entire abdominal cavity is extremely rare worldwide. We here report a case of EGIST with the tumors like cobblestone being diffusely distributed in entire abdominal cavity accompanied by spontaneous bleeding. The tumors may not be fully resected by surgery, hence we made biopsy, pathological examination and gene detection to determine the treatment strategy. The patient was treated with imatinib, and achieved better outcome.
The patient was a 71-year man, with hypertensive disease for 6 months, the highest pressure being 200/110 mmHg, and he has been taking felodipine orally to control blood pressure.
The patient had continuous mild pain at lower abdomen about 10 days prior to hospitalization, with regular bowel movement, and loss of appetite and weight for 5 kg.
He had a history of smoking for 50 years, 60 cigarettes/day, without drinking or exposing to radioactive substance.
His family history was unremarkable.
Upon physical examination, the patient had normal abdominal appearance, tough abdomen with mild pressing pain at lower abdomen, no rebound tenderness or muscular tension, no obvious abdominal mass was touchable, shifting dullness was positive, with normal bowel sound.
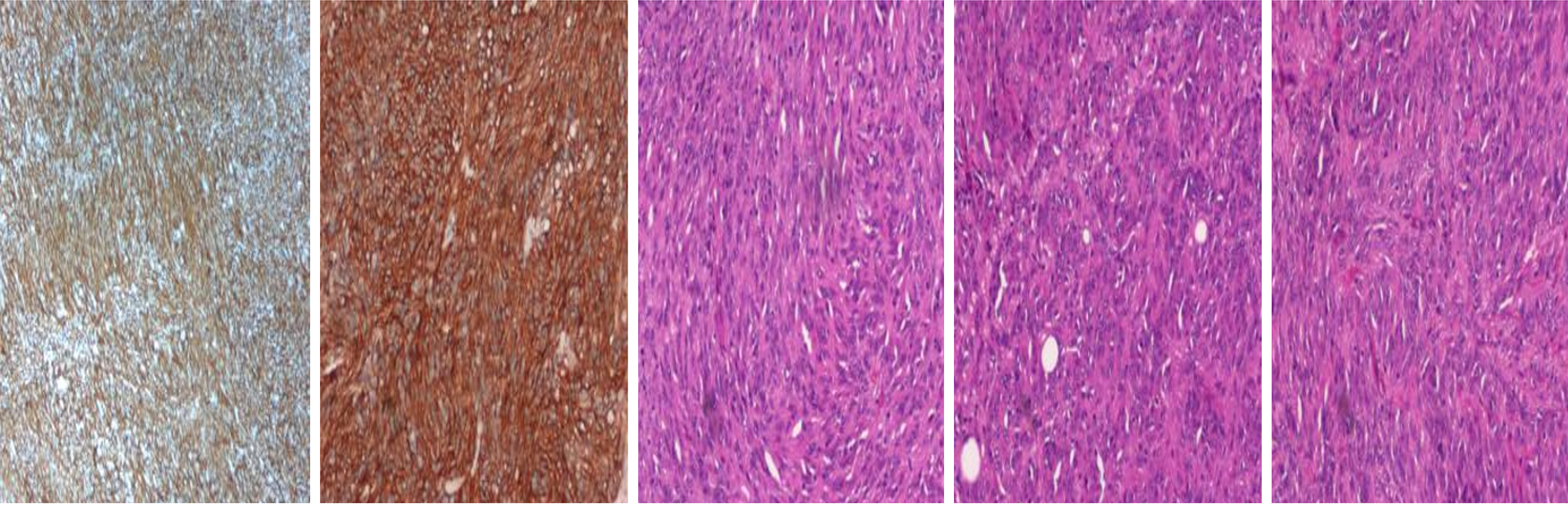
Tumor marker of carbohydrate antigen 125 was 808 U/mL. Gene detection showed breast cancer susceptibility gene 1 interacting protein C-terminal helicase 1 (BRIP1) and KIT genovariation, and the patient was thus sensitive to imatinib. Immunohistochemical analysis resulted in the following results: Calretinin (-), D2-40 (-), CK5/6 (-), WT-1 (+), CD117 (+), Dog-1 (+), SHA (diffused weakly +), Desmin (-), S-100 (-), SOX-10 (-), P16 (-), CD34 (-), and Ki-67 (30% approximately).
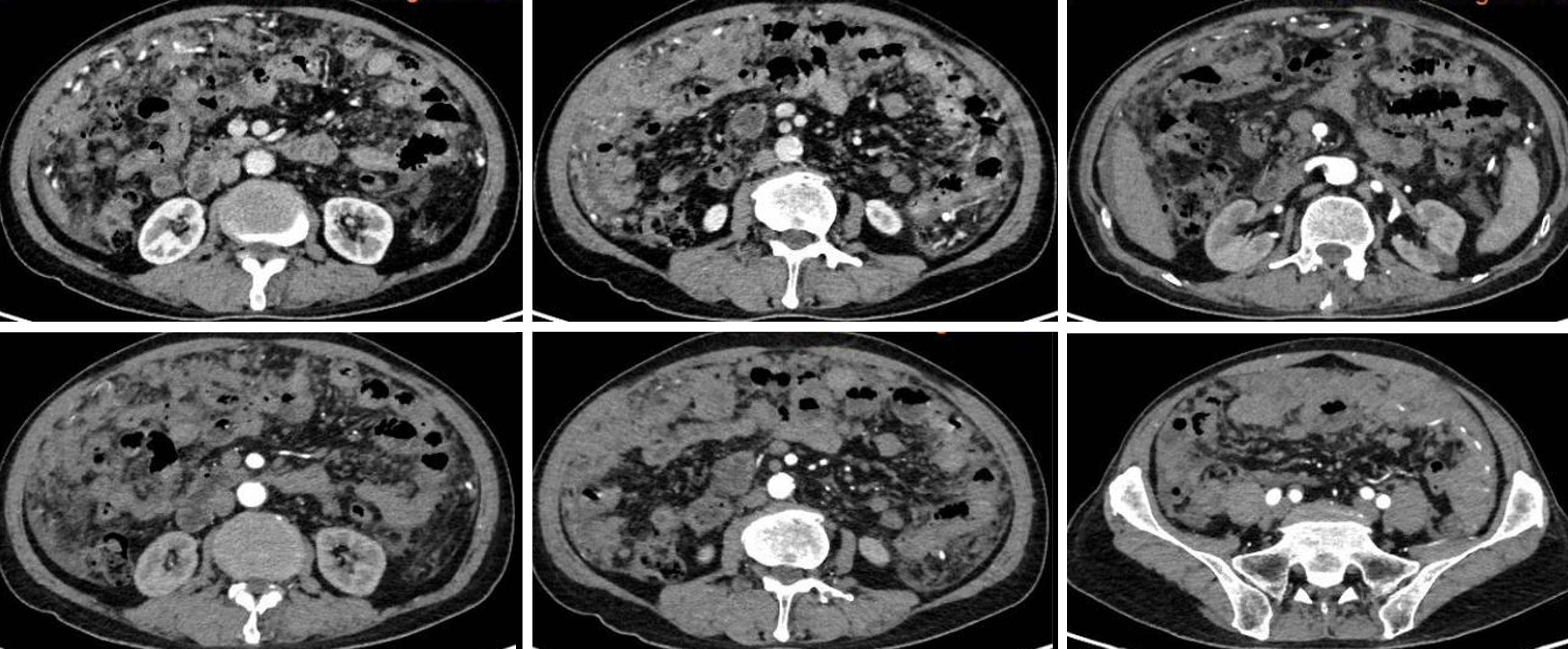
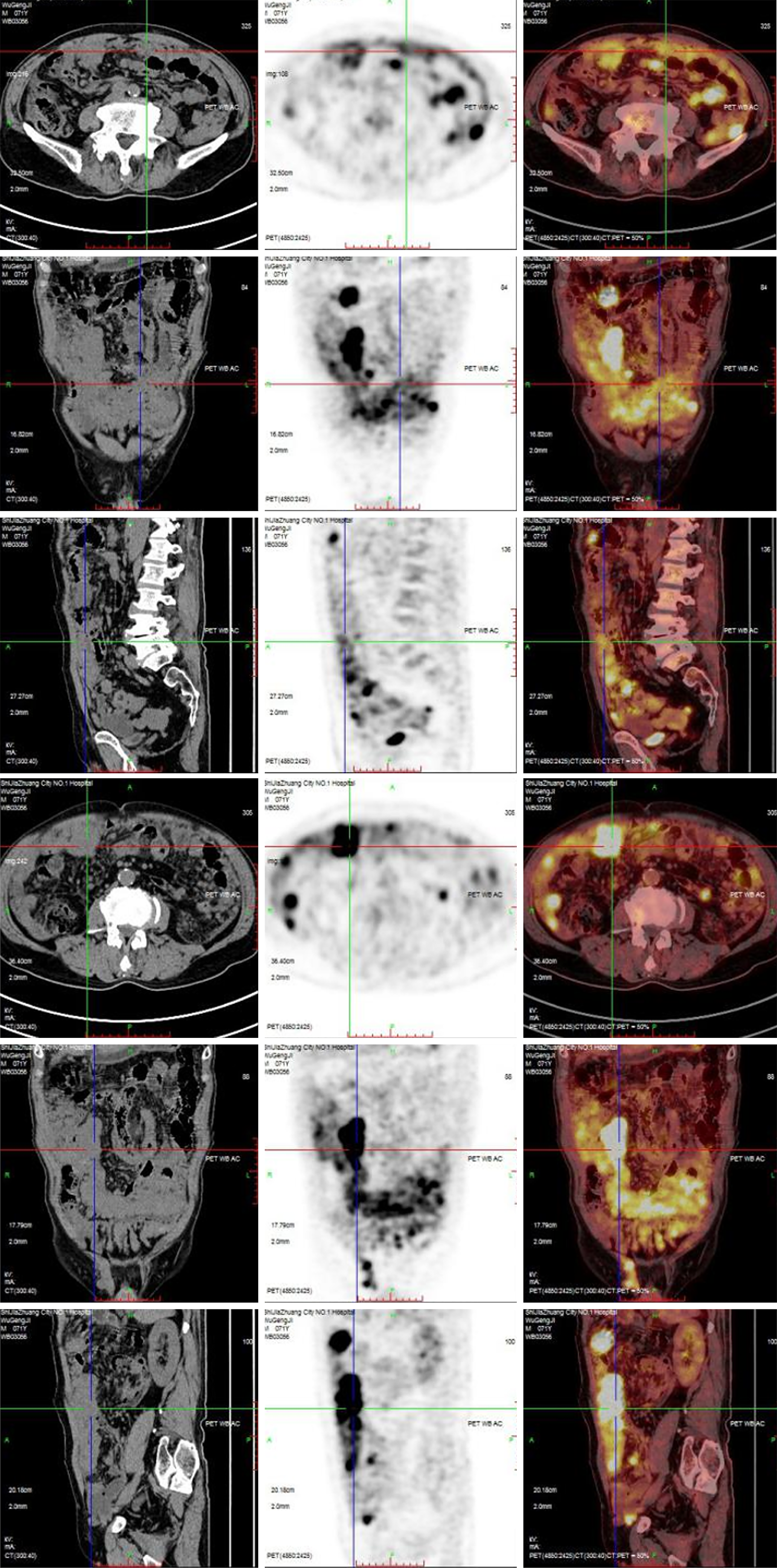
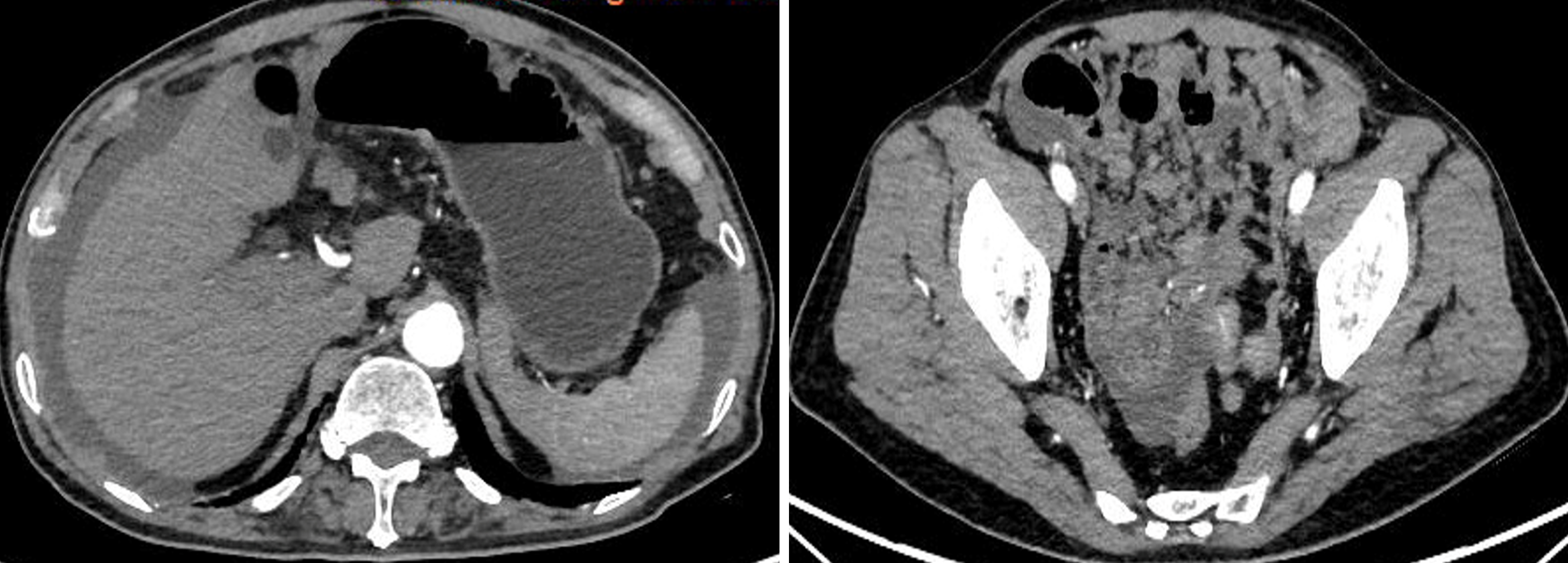
Plain CT scanning at epigastrium/hypogastrium/pelvic cavity + enhanced three-dimensional reconstruction revealed multiple soft tissue nodules in abdominal/pelvic cavity, peritoneum and right groin (Figure 1). Positron emission tomography-computed tomography showed thickened peritoneum with abnormal hypermetabolism, multiple mass or nodular soft tissue density images in abdominal/pelvic cavity and peritoneum (Figure 2). On enhanced scanning, the lesion was enhanced at a mild to moderate level; multiple hypermetabolic lymph nodes in abdominal/pelvic cavity and right external ilium; and seroperitoneum were observed.
Based on pathological examination, a diagnosis of EGIST was considered (Figure 3).
Based on gene detection results, the patient was treated with imatinib.
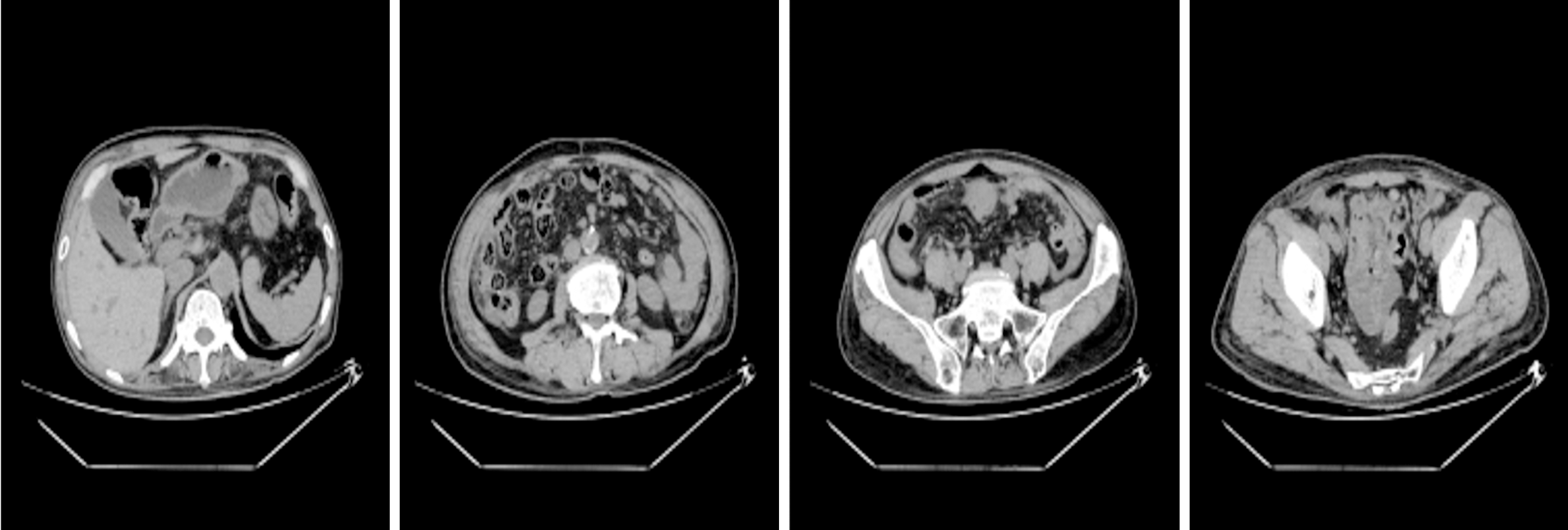
Follow-up visit found that his clinical symptoms disappeared and the tumor load alleviated obviously via imageological examination (Figure 4).
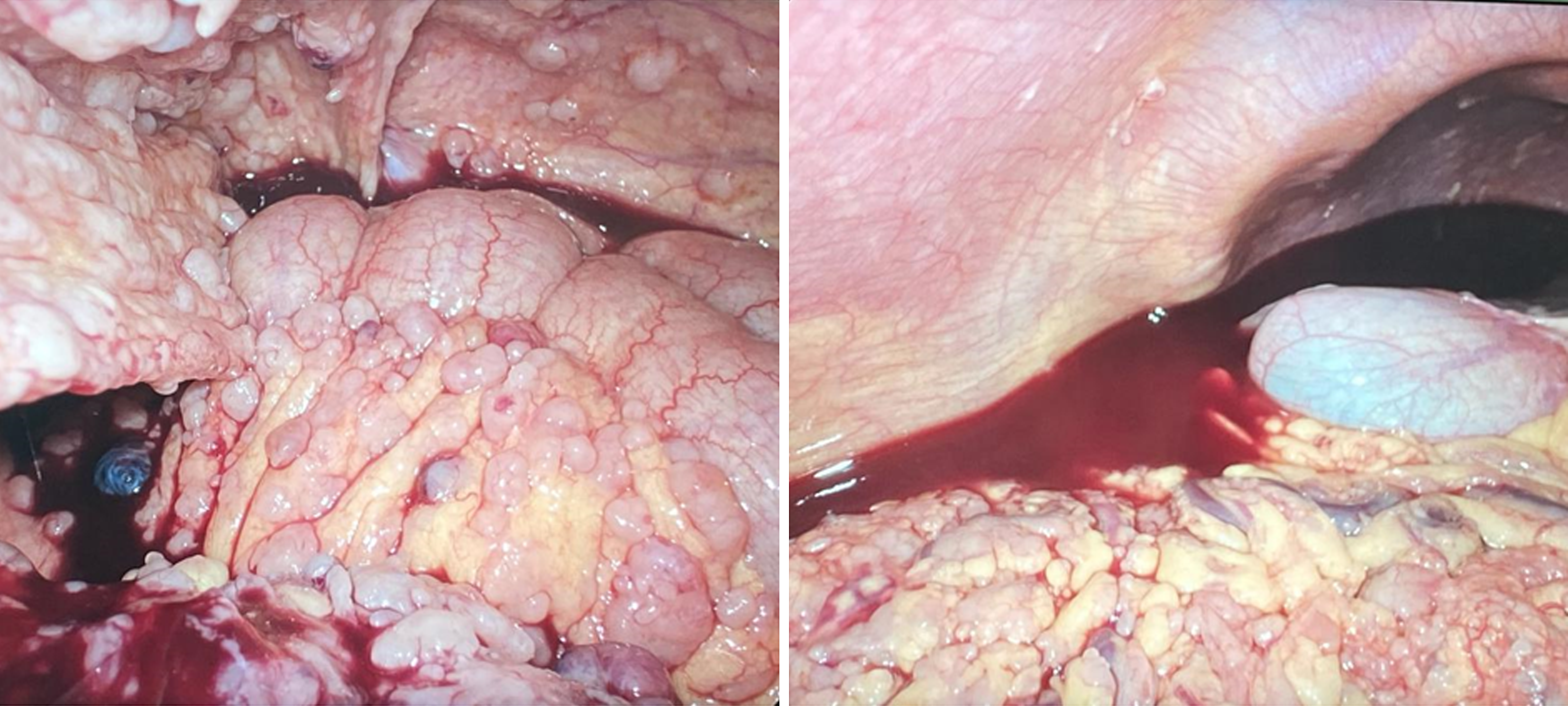
EGIST is rarer in comparison with GIST. GIST is diagnosed due to bleeding and obstruction while EGIST usually presents pain and palpable lump. In this case, the patient was hospitalized due to abdominal pain; upon physical examination, the entire abdomen was tough without solitary lump, but accompanied with spontaneous bleeding in abdominal cavity (Figure 5). The patient had symptoms of both GIST and EGIST. EGIST is commonly seen at vulva[1,2], vagina[3,4], retroperitoneum[5], ovary, posterior gastric, testis[6], greater omentum[7,8], pancreas[9,10], prostate[11-13], bladder[14], mesentery[15,16], liver[17], rectum[18,19], rectosacral space[20], esophagus[21], etc. But this case is rare where diffuse membranous tissue tumors existed in abdominal cavity. In addition, EGIST may have spontaneous rupture[22], just as this case, as shown in Figure 6 for tumor rupture and bleeding. Some EGIST cases are characterized by strong invasion and have unfavorable prognosis[23]. Uzunoglu and Tosun[24] have reported 135 EGIST cases between 2007 and 2020 and showed that elderly or female patients had worse prognosis. In our case, the patient was an old man with strong tumor invasiveness; however, conservative medicating treatment showed a better treatment effect.
Compared with GIST, EGIST has negative c-KIT mutation and positive PDGFRA in histopathological examination and immunohistochemical analysis. Whatever the tumor location is, DOG1 remains a preferred biomarker and CN34 and CD117 are deemed as auxiliary examination[25]. The gene detection for this case showed BRIP1 and KIT genovariation, BRIP1 (point mutation, exon11; nucleotide variation c.1567A > G; amino acid variation p.T523A; abundance 34.45%), KIT (insertion/deletion variation, exon11; nucleotide variation c.1672_1677del; amino acid variation p.K558_V559del; abundance 34.94%). The detection showed that the patient was sensitive to imatinib. After treatment with imatinib, his clinical symptoms disappeared gradually and the abdominal CT reexamination showed that the imageological indexes had obviously improved. This case is different from previous ones in clinical symptoms, imageological manifestations and gene detection results, which have indicated that EGIST has various manifestations, thus comprehensive diagnostics should be performed.
This case of EGIST is rarely seen in clinical practice. The patient was a 71-year man with continuous hypogastralgia. During laparoscopic surgery, several botryoid nodules of various sizes were found in the abdominal cavity. Surgical treatment was impossible. The patient underwent tumor biopsy, and histopathological examination, which showed positive CD117, and gene detection showed BRIP1 and KIT genovariation. After treatment with imatinib, his clinical symptoms disappeared and the abdominal CT reexamination showed that the imageological indexes had obviously improved. In this case, we made an overall evaluation on tumor characteristics in the aspects of imageological examination, gene detection, immunohistochemical analysis and pathological feature, and clinical manifestation difference, which verifies that imatinib treatment for EGIST with diffuse membranous distribution has better therapeutic effect than surgical treatment.
| 1. | Mohamed N, Khan M, Hosler G, Tumminello K. Primary vulvar extragastrointestinal stromal tumor in a 77-year-old woman. J Cutan Pathol. 2023;50:723-729. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Asada Y, Kuroda K, Shirasaka D, Era Y, Ikegawa T, Arai Y, Nakahara A, Kawano M, Kadowaki Y, Okino T. [A case of rectovaginal metastasis 6 years after initial resection of extra-gastrointestinal stromal tumor of vulvar origin]. Nihon Shokakibyo Gakkai Zasshi. 2022;119:946-953. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Liu S, Pan P, Han B, Wang J, Sun M, Sun Y. Extragastrointestinal Stromal Tumor Presenting as a Recurrent Vaginal Mass: Case Report. Onco Targets Ther. 2021;14:959-965. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Addley S, Alazzam M, Johnson C, Soleymani Majd H. Rectovaginal extragastrointestinal stromal tumour (EGIST): an additional entity to be considered in the differential diagnosis of tumours of the rectovaginal septum. BMJ Case Rep. 2021;14:e237669. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Lin J, Liao W, Wang J, Li W, Tang X, Li H, Yi X, Lu X, Chen Z, Zhu B, Feng X, Diao D. Primary extra-gastrointestinal stromal tumor of retroperitoneum: Clinicopathologic characteristics and prognosis of six cases. Front Oncol. 2023;13:1033598. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | El Charif MH, Amro S, Boulos F, Khalife M, Shamseddine A, Assi H, Sbaity E. Extra-gastrointestinal stromal tumors (EGISTs): A case report for a mischief entity. Medicine (Baltimore). 2023;102:e33394. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Almeida M, Sousa F, Resende F, Devesa V, Ferrão A, Carneiro S, Canão P, Barbosa E, Barbosa J. Primary EGIST of the greater omentum - a rare presentation. Acta Chir Belg. 2024;124:137-142. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Kataoka M, Saitoh T, Kawashima K, Yazaki T, Sonoyama H, Okimoto E, Oka A, Mishima Y, Mishiro T, Oshima N, Shibagaki K, Tobita H, Moriyama I, Ishimura N, Nagase M, Hirahara N, Tajima Y, Ishihara S. Primary Extragastrointestinal Stromal Tumor of Greater Omentum with Intraperitoneal Bleeding. Intern Med. 2021;60:3413-3419. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Zackria R, Jayaraman V. The Gastrointestinal Stromal Tumor (GIST) of a Pancreatic Cyst. Cureus. 2022;14:e26197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 10. | Ene D, Florescu LM, Ene R, Popescu B, Gheonea IA. An extremely uncommon case of pancreatic extragastrointestinal stromal tumor in a 53-year-old female patient. Rom J Morphol Embryol. 2021;62:569-573. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Yang Y, Sun D, Tang K. Primary extragastrointestinal stromal tumors of the prostate: A case report and literature review. Front Oncol. 2022;12:1038853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Lu L, Qu H, Wang J, Yao B, Ma B, Qiu JG, Wang ZY, Ren DL. Whole-exome sequencing for high-risk primary prostatic extra-gastrointestinal stromal tumor: A case report. Mol Clin Oncol. 2021;15:249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 13. | Li L, Hu ZQ, Yang CG, Gan JH, Tian JH, Ke CJ, Zeng X. Current knowledge of primary prostatic extra-gastrointestinal stromal tumor: a case report and review of the literature. J Int Med Res. 2021;49:3000605211013172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Tripathy S, Arun Raj ST, Prakash S, Thanaignathan T, Shamim SA. Response Assessment of Recurrent Extragastrointestinal Stromal Tumor of the Urinary Bladder to Imatinib: Findings on Serial (18)F-Fluorodeoxyglucose Positron Emission Tomography-Computed Tomography Scans. Indian J Nucl Med. 2020;35:350-352. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 15. | Sajjanar AB, Katole NT, Vagha SJ. KIT (CD117) Positive Huge Primary Malignant Extra Gastrointestinal Stromal Tumors (EGISTs) Arising From Jejunal Mesentery: A Rare Case Report. Cureus. 2022;14:e33168. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Kadel D, Bhuju S, Thapa BR, Chalise S, Kumar Sah S. Curative intent treatment of late presented extragastrointestinal stromal tumor: two identical case reports with literature review. J Surg Case Rep. 2021;2021:rjab220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Lian J, Feng M, Zhang S, Lu H. Case report: 10-year survival of a patient with a primary hepatic gastrointestinal stromal tumor. Front Oncol. 2022;12:1035824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 18. | Harouachi A, Harhar M, Mhand M, Atmani A, Elamrani A, Kharkhach A, Bouhout T, Serji B, Harroudi TE. Extra gastrointestinal stromal tumor EGIST in the recto-vesical pouch: A case report and literature review. Ann Med Surg (Lond). 2022;74:103283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 19. | Elagami MM, Khalid A, Kumar V, Singhal M, Grossman MA. Perirectal Extragastrointestinal Stromal Tumor: An Unusual Presentation. Cureus. 2021;13:e15529. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | El-Helou E, Chamma L, Mazraani HB, Sebaaly D, Chamma OG, Naccour J, Haddad MM, Lichaa D, Alam H. Extra-Gastrointestinal Stromal Tumor (EGIST) in the Pelvis Mimicking Retroperitoneal Sarcoma. Surg J (N Y). 2022;8:e266-e269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 21. | Fujiwara N, Sato H, Miyawaki Y, Ito M, Aoyama J, Ito S, Oya S, Watanabe K, Sugita H, Yasuda M, Sakuramoto S. The hybrid procedure of thoracoscopic and hand-assisted laparoscopic resection of an esophageal gastrointestinal stromal tumor: A case report. Asian J Endosc Surg. 2021;14:286-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 22. | Murata T, Ishimori T, Naitou W, Igrashi Y, Suno Y, Kawachi J. Laparoscopic resection for spontaneously ruptured primary extragastrointestinal stromal tumor of the greater omentum: A case report. Int J Surg Case Rep. 2022;99:107567. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 23. | Abidoye O, Johnson A. Extremely Aggressive Mesenteric Extragastrointestinal Stromal Tumor: A Case Report and Literature Review. Cureus. 2022;14:e23108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 24. | Uzunoglu H, Tosun Y. Primary extra gastrointestinal stromal tumors of the abdomen. North Clin Istanb. 2021;8:464-471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Moldovan VT, Pătraşcu OM, Ali L, Costache M, Sajin M. Morphological and immunohistochemical diagnostic of extragastrointestinal stromal tumors - a 51 case series analysis. Rom J Morphol Embryol. 2021;62:1011-1016. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |