Published online Sep 16, 2024. doi: 10.12998/wjcc.v12.i26.5885
Revised: June 7, 2024
Accepted: June 25, 2024
Published online: September 16, 2024
Processing time: 126 Days and 18.3 Hours
Adjacent segment disease (ASD) after fusion surgery is frequently manifests as a cranial segment instability, disc herniation, spinal canal stenosis, spondylo
To investigate the risk factors and clinical significance of retrograde movement of the proximal vertebral body after lower lumbar fusion.
This was a retrospective analysis of the clinical data of patients who underwent transforaminal lumbar interbody fusion surgery between September 2015 and July 2021 and who were followed up for more than 2 years. Ninety-one patients with degenerative lumbar diseases were included (22 males and 69 females), with an average age of 52.3 years (40-73 years). According to whether there was retrograde movement of the adjacent vertebral body on postoperative X-rays, the patients were divided into retrograde and nonretrograde groups. The sagittal parameters of the spine and pelvis were evaluated before surgery, after surgery, and at the final follow-up. At the same time, the Oswestry Disability Index (ODI) and Visual Analogue Scale (VAS) were used to evaluate the patients’ quality of life.
Nineteen patients (20.9%) who experienced retrograde movement of proximal adjacent segments were included in this study. The pelvic incidence (PI) of the patients in the retrograde group were significantly higher than those of the patients in the nonretrograde group before surgery, after surgery and at the final follow-up (P < 0.05). There was no significant difference in lumbar lordosis (LL) between the two groups before the operation, but LL in the retrograde group was significantly greater than that in the nonretrograde group postoperatively and at the final follow-up. No significant differences were detected in terms of the |PI–LL|, and there was no significant difference in the preoperative lordosis distribution index (LDI) between the two groups. The LDIs of the retrograde group were 68.1% ± 11.5% and 67.2% ± 11.9%, respectively, which were significantly lower than those of the nonretrograde group (75.7% ± 10.4% and 74.3% ± 9.4%, respectively) (P < 0.05). Moreover, the patients in the retrograde group had a greater incidence of a LDI < 50% than those in the nonretrograde group (P < 0.05). There were no significant differences in the ODI or VAS scores between the two groups before the operation, but the ODI and VAS scores in the retrograde group were significantly worse than those in the nonretrograde group after the operation and at the last follow-up, (P < 0.05).
The incidence of posterior slippage after lower lumbar fusion was approximately 20.9%. The risk factors are related to a higher PI and distribution of lumbar lordosis. When a patient has a high PI and insufficient reconstruction of the lower lumbar spine, adjacent segment compensation via posterior vertebral body slippage is one of the factors that significantly affects surgical outcomes.
Core Tip: Sagittal alignment of the spine and pelvis was assessed for patients with or without retrograde of the adjacent vertebra body on postoperative X-rays. We concluded that the risk factors of the posterior slip of the proximal vertebra body after lower lumbar fusion are related to a higher pelvic incidence (PI) and distribution of lumbar lordosis. When a patient has a high PI and insufficient reconstruction of the lower lumbar spine, adjacent segment compensation via posterior vertebra body slippage is one of the factors that significantly affects surgical outcomes.
- Citation: Zhu JJ, Wang Y, Zheng J, Du SY, Cao L, Yang YM, Zhang QX, Xie DD. Risk factors and clinical significance of posterior slip of the proximal vertebral body after lower lumbar fusion. World J Clin Cases 2024; 12(26): 5885-5892
- URL: https://www.wjgnet.com/2307-8960/full/v12/i26/5885.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i26.5885
Adjacent segment disease (ASD) has become a highly concerning complication following low lumbar fusion surgery. Okuda et al[1] reported that incidence of radiologically ASD after posterior lumbar interbody fusion with pedicle screw fixation reached 19%, 49%, and 75% at 2, 5 and 10 years, respectively. In addition, ASD is an important factor affecting clinical outcomes[1]. Owing to the different definitions of ASD, its radiographic features differ presenting as adjacent segment instability, disc herniation, spinal canal stenosis, spondylolisthesis or retrolisthesis of the adjacent vertebra[2,3]. The clinical characteristics of ASD differ on different imaging modalities appearing as adjacent segment instability, spondylolisthesis or retrolisthesis appear at the short-term follow-up, or disc herniation and spinal canal stenosis of the adjacent segment at the long-term follow-up. Different pathogeneses can thus result in different imaging results[1,2]. Retrograde movement of cranial adjacent segments is common after transforaminal lumbar interbody fusion (TLIF). Although the risk factors for ASD have been previously investigated, no study has focus on the retrograde movement of cranial adjacent segments. However, to the best of our knowledge, there has been no study of the risk factors or clinical value of retrolisthesis of cranial adjacent segments. The present study was designed to quantitatively evaluate the radiographic and clinical data of patients who underwent TLIF, to identify the incidence, risk factors and clinical value of retrolisthesis of cranial adjacent segments.
The study was approved by the Institutional Review Board, and the clinical data of all patients who were diagnosed with degenerative lumbar disease and who underwent TLIF at our department between September 2015 and July 2021 were retrospectively reviewed. Inclusion criteria: (1) A diagnosis of degenerative lumbar disease, including lumbar disc herniation, lumbar spinal stenosis, lumbar spondylolisthesis; (2) Followed up for more than 2 years; and (3) Complete preoperative, postoperative and follow-up X-rays. Patients who previously underwent lumbar surgery or had a congenital spine deformity were excluded. In total, 91 patients, including 22 males and 69 females with an average age of 52.3 years (40-73 years), were ultimately enrolled. The mean duration of follow-up were 27.3 months (range 24-51 months). According to whether there was retrograde movement of the adjacent vertebral body on postoperative X-rays, the patients were divided into retrograde and nonretrograde groups.
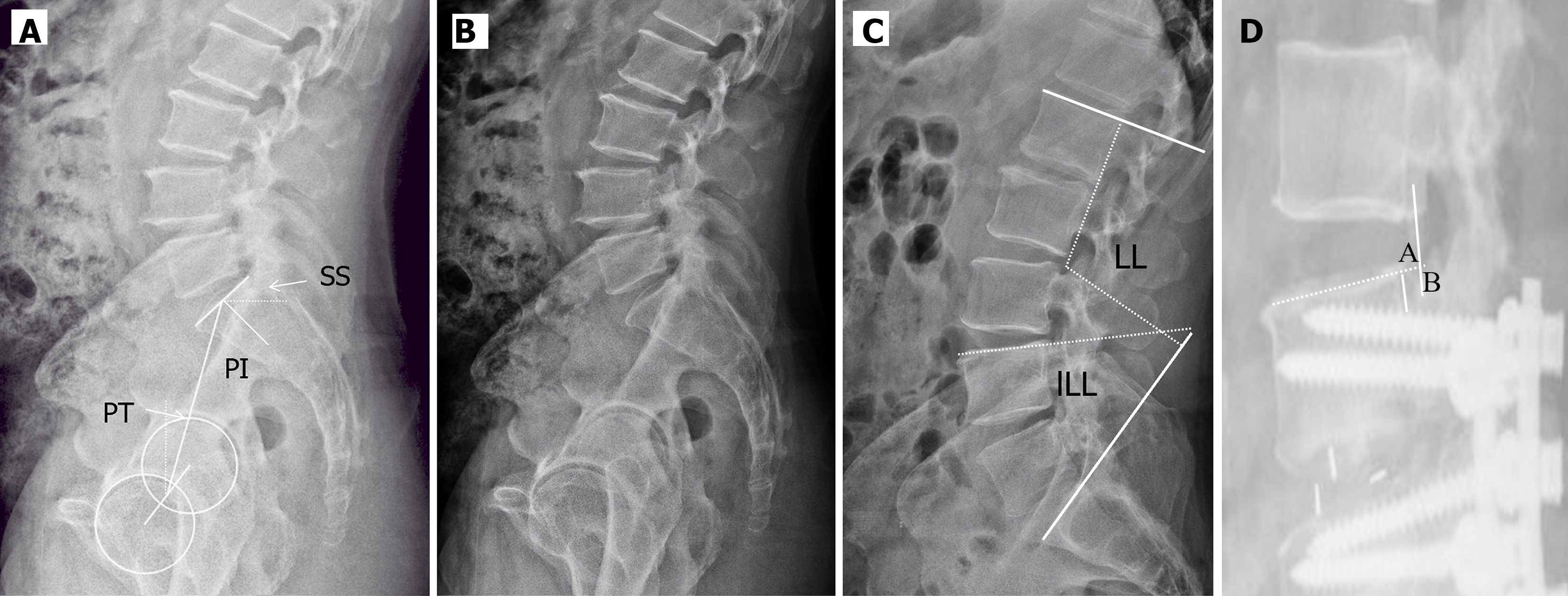
Sagittal alignment of the spine and pelvis was assessed with Surgimap Spine software (Nemaris, Inc., New York, NY, United States). In line with previously described methods[4-7], three pelvic and three spinal parameters were measured on upright standing lateral radiographs of the lumbar spine: (1) Pelvic incidence (PI): The angle between the line perpendicular to the sacral plate at its midpoint and the line connecting this point to the axis of the femoral heads; (2) Pelvic tilt (PT): The angle between the line connecting the midpoint of the sacral plate to the femoral head axis and the vertical axis; (3) Sacral slope (SS): The angle between the superior plate of S1 and a horizontal line[8-11]; (4) Lumbar lordosis (LL): The angle between the superior endplate of the L1 vertebra and the superior endplate of the S1 vertebra; (5) Lower LL (lLL): The angle between the superior endplate of the L4 vertebra and the superior endplate of the S1 vertebra; and (6) Upper LL (uLL): The angle of LL minus lLL (Figure 1A and B). A positive angle was defined as lordosis and a negative angle was defined as kyphosis.
Retrograde distance of cranial adjacent segments: Distance between point A and point B (Figure 1C); point A: The dorsal edges of the cranial endplate of the inferior vertebra, point B: The intersection point between the line crossing the dorsal edges of the caudal endplate of the superior vertebra and the line perpendicular to the cranial endplate of the inferior vertebra. A distance > 3 mm was defined as unstable vertebral body slip.
|PI-LL| > 10° was defined as PT and LL mismatch. The lordosis distribution index (LDI) was defined as lLL/LL × 100%. A normal LDI was defined as 50%-80%. A LDI < 50% indicates insufficient lLL, and a LDI > 80% indicates excessive lLL[3,8,9].
The Oswestry Disability Index (ODI) and Visual Analogue Scale (VAS) were used for preoperative, postoperative and final follow-up evaluations. The questionnaire results were recorded and statistically analyzed by two independent orthopedic surgeons, and inconclusive results were statistically analyzed again.
Data analysis was performed with SPSS 17.0 software (SPSS, Chicago, IL, United States). Continuous data are described as the mean ± SD (range). Paired t test was used to compare continuous variables between the two groups. Comparisons of categorical variables were analyzed with the χ2 test. A P-value < 0.05 indicated statistical significance.
Ninety-one patients with degenerative lumbar diseases were included (22 males and 69 females), with an average age of 52.3 years (40-73 years). Retrograde movement of cranial adjacent segments was observed in 19 (20.9%) patients at the last follow-up (Figure 2). Table 1 summarizes the demographic data of the patients in the two groups. Age and the sex ratio were similar between the two groups. No significant differences were noted between the two groups in terms of the operation time, blood loss volume, follow-up time, fixed segment, fusion segment, or fixation of S1.
| Nonretrograde group | Retrograde group | t value | P value | |
| Age (year) | 51.7 ± 10.6 | 52.4 ± 11.3 | 0.258 | 0.797 |
| Sex (male/female) | 18/54 | 4/15 | 0.128 | 0.721 |
| Operation time (minute) | 257.3 ± 46.9 | 264.7 ± 43.8 | 0.619 | 0.540 |
| Blood loss (mL) | 219.6 ± 49.3 | 207.7± 56.5 | 0.907 | 0.367 |
| Follow-up time (month) | 27.4 ± 6.3 | 26.9 ± 7.0 | ||
| Fixed segment | 2.4 ±0.69 | 2.5 ± 0.74 | 0.554 | 0.581 |
| Fusion segment | ||||
| 1 | 59 | 14 | 0.646 | 0.421 |
| 2 | 13 | 5 | ||
| Fixation of S1 | ||||
| Yes | 12 | 5 | 0.921 | 0.337 |
| No | 60 | 14 | ||
The surgery was successful in all patients. In the nonretrograde group, two patients experienced fat liquefaction, which healed after debridement. One patient experienced cerebrospinal fluid leakage but showed good recovery 9 days after endorhachis repair. In the retrograde group, one patient developed an infection and was cured after anti-inflammatory therapy. One patient presented with nerve root irritation, which disappeared on the seventh day after treatment with methylprednisolone and mecobalamin. There was no cage shifting, screw fracture or internal fixation loosening during the follow-up period in the nonretrograde group. One patient underwent revision surgery due to internal fixation failure. At the final follow-up, 4 patients in the nonretrograde group and 7 patients in the retrograde group were diagnosed with ASD.
Comparisons of the pelvic parameters and sagittal lumbar parameters between the two groups are presented in Table 2. The PI, SS and uLL were significantly greater in the retrograde group preoperatively, postoperatively and at the final follow-up (P < 0.05). Compared with those in the nonretrograde group, LL was significantly greater postoperatively and at the final follow-up (P < 0.05), but did not significantly differ before the operation (P > 0.05). In addition, the PT and lLL did not significantly differ between the two groups preoperatively, postoperatively or at the final follow-up (P > 0.05).
| Nonretrograde group | Retrograde group | t value | P value | |
| PI (°) | ||||
| Preoperative | 47.9 ± 9.2 | 57.8 ± 10.6 | 4.041 | < 0.001 |
| Postoperative | 49.2 ± 9.6 | 58.1 ± 11.4 | 3.454 | 0.008 |
| Final follow-up | 49.6 ± 10.3 | 57.2 ± 11.9 | 2.768 | < 0.001 |
| PT (°) | ||||
| Preoperative | 20.5 ± 6.2 | 21.5 ± 6.4 | 0.621 | 0.536 |
| Postoperative | 15.6 ± 4.4 | 14.8 ± 5.6 | 0.665 | 0.508 |
| Final follow-up | 14.9 ± 3.9 | 15.3 ± 5.0 | 0.374 | 0.709 |
| SS (°) | ||||
| Preoperative | 27.9 ± 8.3 | 35.1 ± 8.2 | 3.371 | < 0.001 |
| Postoperative | 35.8 ± 7.9 | 42.7 ± 10.8 | 3.123 | 0.002 |
| Final follow-up | 37.1 ± 9.4 | 41.9 ± 7.7 | 2.049 | 0.043 |
| LL (°) | ||||
| Preoperative | 34.1 ± 10.2 | 38.9 ± 14.8 | 1.649 | 0.103 |
| Postoperative | 48.7 ± 12.6 | 57.1 ± 10.6 | 2.664 | 0.009 |
| Final follow-up | 48.9 ± 9.7 | 56.3 ± 9.2 | 2.988 | 0.003 |
| lLL (°) | ||||
| Preoperative | 24.9 ± 4.8 | 27.0 ± 6.8 | 1.546 | 0.126 |
| Postoperative | 38.1 ± 8.9 | 38.7 ± 9.9 | 0.255 | 0.799 |
| Final follow-up | 37.4 ± 9.6 | 38.9 ± 8.5 | 0.619 | 0.537 |
| uLL (°) | ||||
| Preoperative | 8.1 ± 3.4 | 10.9 ± 4.7 | 2.934 | 0.004 |
| Postoperative | 12.5 ± 4.3 | 18.2 ± 6.4 | 4.605 | < 0.001 |
| Final follow-up | 12.7 ± 5.6 | 17.6 ± 5.4 | 3.417 | < 0.001 |
The sagittal morphology of the lumbar spine was also compared between the two groups (Table 3). No significant differences were detected in terms of |PI-LL| preoperatively, postoperatively or at the final follow-up (P > 0.05). There was no significant difference in the preoperative LDI between the two groups. The LDIs of the retrograde group were 68.1% ± 11.5% and 67.2% ± 11.9%, respectively, which were significantly lower than those of the nonretrograde group (75.7% ± 10.4% and 74.3% ± 9.4%, respectively) (P < 0.05). Moreover, patients in the retrograde group were noted had a higher incidence of insufficient lLL than those in the nonretrograde group (P < 0.05).
| Nonretrograde group | Retrograde group | t value | P value | |
| |PI-LL| (°) | ||||
| Preoperative | 13.9 ± 5.2 | 15.3 ± 5.8 | 1.019 | 0.311 |
| Postoperative | 1.9 ± 4.3 | 1.4 ± 3.6 | 0.465 | 0.643 |
| Final follow-up | 0.9 ± 2.1 | 1.2 ± 3.0 | 0.671 | 0.504 |
| PI-LL matching | ||||
| Yes | 63 | 16 | 0.142 | 0.706 |
| No | 9 | 3 | ||
| LDI (%) | ||||
| Preoperative | 75.9 ± 14.9 | 71.1 ± 16.7 | 1.217 | 0.226 |
| Postoperative | 75.7 ± 10.4 | 68.1 ± 11.5 | 2.772 | 0.006 |
| Final follow-up | 74.3 ± 9.4 | 67.2 ± 11.9 | 2.764 | 0.006 |
| Distribution of LL | ||||
| LDI < 50% | 6 | 7 | 49.937 | < 0.001 |
| 50% ≤ LDI < 80% | 64 | 12 | ||
| 80 ≤ LDI | 2 | 0 | ||
The ODI and VAS scores were significantly better in nonretrograde group postoperatively and at the final follow-up (P < 0.05), but did not significantly differ before the operation between the two groups (P > 0.05) (Table 4).
| Nonretrograde group | Retrograde group | t value | P value | |
| ODI score | ||||
| Preoperative | 41.4 ± 11.9 | 40.8 ± 10.3 | 0.201 | 0.841 |
| Postoperative | 21.1 ± 7.2 | 26.1 ± 7.4 | 2.677 | < 0.001 |
| Final follow-up | 18.0 ± 6.3 | 24.2 ± 4.6 | 4.009 | < 0.001 |
| VAS score | ||||
| Preoperative | 7.0 ± 2.2 | 7.4 ± 2.5 | 0.685 | 0.495 |
| Postoperative | 2.2 ± 1.2 | 3.1 ± 1.6 | 2.703 | 0.008 |
| Final follow-up | 1.8 ± 1.1 | 2.9 ± 1.4 | 3.654 | < 0.001 |
Lumbar retrolisthesis is a common occurrence, and its incidence and mechanism have been described in several studies. However, all of the studies concentrated on patients who did not undergo surgery. In a retrospective study by Zhu et al[5], the sagittal spinopelvic parameters of 105 patients (60 patients with retrolisthesis and 45 patients with anterolisthesis) and 40 healthy age-matched adults were measured and analyzed. They reported that the sagittal vertical axis, PI, SS, and LL in the retrolisthesis group were significantly lower than those in the anterolisthesis group and in the control group, whereas the thoracolumbar kyphosis (TLK) in the retrolisthesis group was significantly greater than that in the other 2 groups. They concluded that a low PI may contribute to the occurrence and progression of retrolisthesis. In contrast, another similar study reported that lumbar retrolisthesis could also occur under in patients with a high PI[10]. They concluded that lumbar retrolisthesis in patients with a high PI might be primarily associated with increased backward sliding forces at the hyper tilted vertebra in the large TLK segment and lumbar instability caused by disc degeneration and facet arthritis[10]. Currently, the mechanism underlying the backward displacement of the vertebra is unclear, and cannot provided a reliable theoretical reference for lumbar retrolisthesis following TLIF.
In our study, the patients in the retrograde group had a high PI preoperatively, postoperatively and at the final follow-up. The LL and uLL were significantly greater in the retrograde group postoperatively and at the final follow-up; however, the LL preoperatively and the lLL preoperatively, postoperatively and at the final follow-up did not significantly differ between the two groups. In the healthy adult population, the loss of lLL is the most important factor. Reconstruction of the lLL is the key point for ideal sagittal spine resconstruction[6]. For patients who underwent lLL short-segment spina fusion surgery, insufficient reestablishment of the lLL was compensated for hyperextension of the unfused uLL, which resulted in excessive cranial adjacent intervertebral space expansion to compensate for insufficient LL. According to a finite element analysis of biomechanics, Senteler et al[7] concluded that insufficient reestablishment of the lLL results in increased segmental joint loads in the unfused and fused lumbar spine, and predisposes patients to ASD after lumbar spinal fusion[7]. Our study also revealed that backward displacement of the cranial adjacent vertebra following low spinal fusion was correlated with insufficient reestablishment of the lLL for patients with a high PI. Patients with a high PI and who experience lLL reconstruction deficiency can cause forward progression the trunk. The uLL increases to maintain gravity balance, which results in an increase in adjacent segment backward shear force, and thus leads to backward sliding of the adjacent segment of the vertebra.
To determine the mechanical of properties cranial adjacent vertebra retrolisthesis following lumbar fusion surgery, PI-LL matching and sagittal lumbar morphology data were collected. There was no significant difference between the two groups with respect to PI-LL matching. However, in term of the distribution of LL, the LDI of the retrograde group was significantly lower postoperatively and at the final follow-up. Moreover, the proportion of patients with a LDI < 50% was significantly greater in the retrograde group than in the nonretrograde group. The results support the theoretical foundation of the mechanism of retrolisthesis in patients with a high PI. Based on these results, we believe that the distribution of LL should be considered as important as PI-LL matching in patients who undergo lumbar fusion surgery. Yilgor et al[11] evaluated the sagittal spinal parameters of patients following long-segment spine fusion surgery and reported that the PI-LL may be insufficient for predicting the proximal junction mechanics and internal fixation complications postoperatively. A low LDI should be considered; moreover, a lower LDI indicates significantly higher risks of mechanical and internal fixation complications. This study revealed that all of the following factors should be considered prior to reconstruction of LL through lumbar spinal surgery: The segments responsible for preoperative lordosis loss, the PI, and the distribution of LL. A full intervertebral bone graft and larger cage were selected and placed as front as possible in the intervertebral space to obtain satisfactory intervertebral lordosis and LL.
The ODI and VAS scores were significantly lower in the retrograde group postoperatively and at the final follow-up, which might be related to the local stress concentration and the nonideal distribution of LL. Adjacent segment shear forces and the burden on the functional units of the spine increase because the proximal adjacent intervertebral space expands and cranial adjacent vertebra retrolisthesis occurs, which leads to back pain[7]. At the same time, the long-term inability of the spine to perform compensatory function decreases the effect of surgery and lead to a lower quality of life[8]. Yilgor et al[11] confirmed that the distribution of LL is closely associated with long-term surgical effects and that the ideal distribution of LL could maintain long-term satisfactory quality of life.
Limitations of our study include its retrospective design, short follow-up duration and lack of systematic evaluation of the relationship between vertebral retrolisthesis and ASD. Vertebra retrolisthesis is a time-dependent complication, and a longer follow-up duration is needed to observe its incidence and clinical outcome. Theoretically, vertebral retrolisthesis is a form of ASD. Seven patients in the retrograde group and 4 patients in the nonretrograde group were diagnosed with ASD. Whether intraoperative facet joint damage could affect the posterior displacement of the vertebra was not mentioned in this study.
The incidence of proximal adjacent vertebra retrolisthesis after lower lumbar fusion is 20.9%, and a high PI and inappropriate LDI are risk factors. Backward sliding of the cranial adjacent vertebra to compensate for insufficient restoration of LL in patients with a high PI significantly affects surgical outcomes.
I would like to express my gratitude to all those who helped me during the writing of this paper. My deepest gratitude goes first and foremost to my team members for their contribution to this paper, including research designed and performed, data collected and analyzed, manuscript wrote. Secondly, I would like to express my heartfelt gratitude to Professor Pei-An Lou, who helped me a lot about data analyzed. Finally, I am indebted to the editor and the reviewers for the time and effort on our paper.
| 1. | Okuda S, Nagamoto Y, Matsumoto T, Sugiura T, Takahashi Y, Iwasaki M. Adjacent Segment Disease After Single Segment Posterior Lumbar Interbody Fusion for Degenerative Spondylolisthesis: Minimum 10 Years Follow-up. Spine (Phila Pa 1976). 2018;43:E1384-E1388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 101] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 2. | Jeong TS, Son S, Lee SG, Ahn Y, Jung JM, Yoo BR. Comparison of adjacent segment disease after minimally invasive versus open lumbar fusion: a minimum 10-year follow-up. J Neurosurg Spine. 2022;36:525-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 3. | Bae JS, Lee SH, Kim JS, Jung B, Choi G. Adjacent segment degeneration after lumbar interbody fusion with percutaneous pedicle screw fixation for adult low-grade isthmic spondylolisthesis: minimum 3 years of follow-up. Neurosurgery. 2010;67:1600-7; discussion 1607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Scemama C, Magrino B, Gillet P, Guigui P. Risk of adjacent-segment disease requiring surgery after short lumbar fusion: results of the French Spine Surgery Society Series. J Neurosurg Spine. 2016;25:46-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 5. | Zhu F, Bao H, Liu Z, Zhu Z, He S, Qiu Y. Lumbar Retrolisthesis in Aging Spine: What are the Associated Factors? Clin Spine Surg. 2017;30:E677-E682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Kim SI, Min HK, Ha KY, Park HY, Cho CH, Cho RK, Kim YH. Effects of Restoration of Sagittal Alignment on Adjacent Segment Degeneration in Instrumented Lumbar Fusions. Spine (Phila Pa 1976). 2020;45:E1588-E1595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 7. | Senteler M, Weisse B, Snedeker JG, Rothenfluh DA. Pelvic incidence-lumbar lordosis mismatch results in increased segmental joint loads in the unfused and fused lumbar spine. Eur Spine J. 2014;23:1384-1393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 87] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 8. | Yilgor C, Sogunmez N, Boissiere L, Yavuz Y, Obeid I, Kleinstück F, Pérez-Grueso FJS, Acaroglu E, Haddad S, Mannion AF, Pellise F, Alanay A; European Spine Study Group (ESSG). Global Alignment and Proportion (GAP) Score: Development and Validation of a New Method of Analyzing Spinopelvic Alignment to Predict Mechanical Complications After Adult Spinal Deformity Surgery. J Bone Joint Surg Am. 2017;99:1661-1672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 413] [Article Influence: 51.6] [Reference Citation Analysis (0)] |
| 9. | Rothenfluh DA, Mueller DA, Rothenfluh E, Min K. Pelvic incidence-lumbar lordosis mismatch predisposes to adjacent segment disease after lumbar spinal fusion. Eur Spine J. 2015;24:1251-1258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 219] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 10. | Zhu W, Kong C, Zhang S, Wang P, Sun X, Lu S. The radiographic characteristics and developmental mechanism of the lumbar degenerative retrolisthesis under a high-grade PI. J Orthop Sci. 2021;26:103-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Yilgor C, Sogunmez N, Yavuz Y, Abul K, Boissiére L, Haddad S, Obeid I, Kleinstück F, Sánchez Pérez-Grueso FJ, Acaroğlu E, Mannion AF, Pellise F, Alanay A; European Spine Study Group. Relative lumbar lordosis and lordosis distribution index: individualized pelvic incidence-based proportional parameters that quantify lumbar lordosis more precisely than the concept of pelvic incidence minus lumbar lordosis. Neurosurg Focus. 2017;43:E5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 79] [Article Influence: 9.9] [Reference Citation Analysis (0)] |