Published online Sep 16, 2024. doi: 10.12998/wjcc.v12.i26.5868
Revised: May 6, 2024
Accepted: May 24, 2024
Published online: September 16, 2024
Processing time: 134 Days and 3.5 Hours
Orthodontic treatment can easily cause local soft tissue reactions in the oral cavity of patients under mechanical stress, leading to oral mucosal ulcers and affecting their quality of life. At present, only limited literature has explored the factors leading to oral ulcers in orthodontic treatment, and these research results are still controversial.
To investigate the current status and related factors of oral mucosal ulcers during orthodontic treatment, aiming to provide a valuable reference for preventing this disease in clinical practice.
A total of 587 patients who underwent orthodontic treatment at the Peking Uni
A logistic regression model with oral ulcers as the dependent variable was esta
Age ≥ 60 years, smoking history, hard toothbrush, hot diet, treatment course for > 1 year, tooth brushing frequency of ≤ 1 time per day, and mental anxiety are independent risk factors for oral mucosal ulcers. Therefore, these factors should receive clinical attention and be incorporated into the development and optimization of preventive stra
Core Tip: Currently, there is limited literature exploring the factors leading to oral ulcers during orthodontic treatment, with considerable controversy. Therefore, this study uses retrospective data to explore and analyze the current situation and related factors of oral mucosal ulcers during orthodontic treatment in our hospital, providing a reference for the clinical prevention of this disease.
- Citation: Chang J, Li X. Multivariate analysis of oral mucosal ulcers during orthodontic treatment. World J Clin Cases 2024; 12(26): 5868-5876
- URL: https://www.wjgnet.com/2307-8960/full/v12/i26/5868.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i26.5868
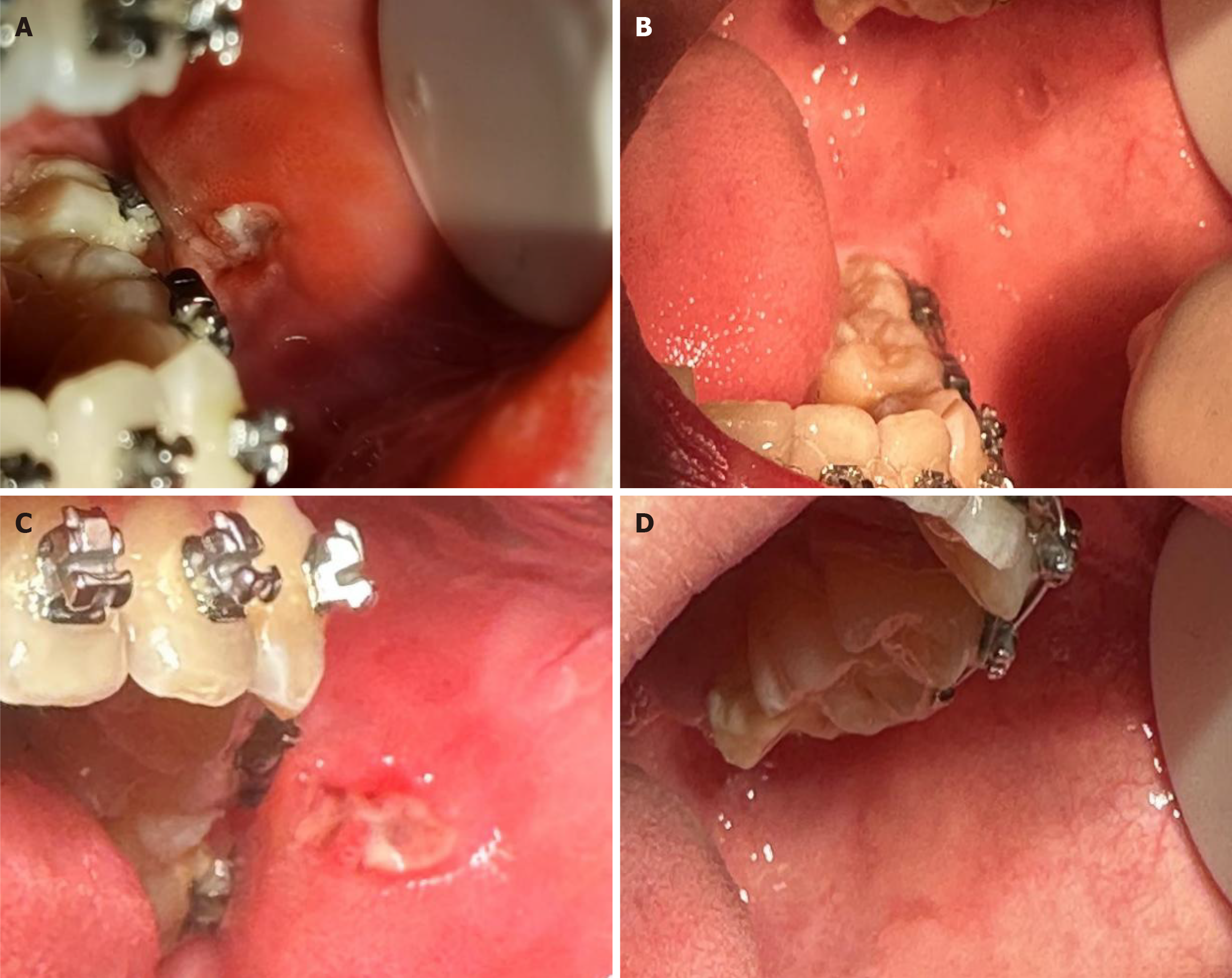
Orthodontic treatment traditionally refers to the correction of teeth and the removal of malocclusion and deformed teeth, with the diagnosis and treatment procedures primarily involving determining the etiology and mechanism of the malocclusion to achieve an aesthetic modification of the affected teeth. Although this treatment can effectively ameliorate dental and skeletal problems, utilizing orthodontic appliances to adjust the coordination between facial bones, teeth, nerves, and muscles in the maxillofacial region can easily cause the reaction of the local soft tissues in the patient's oral cavity following mechanical stress and ultimately result in the accumulation of oral bacteria[1]. In the initial treatment stage, oral mucosal ulcers can sometimes occur due to the contact of the mucosa with orthodontic brackets[2-4]. Oral mucosal ulcers are a prevalent adverse reaction in patients undergoing orthodontic treatment, often presenting on the surface of the mouth and tongue margin and triggering a burning sensation and pain (Figure 1). Thus, the speech and diet of the patients are affected to a certain degree by these ulcers, which generally heal spontaneously within 1–2 week. However, oral mucosal ulcers tend to occur as repeated attacks, with some patients experiencing multiple infections over a short period that affect their quality of life. Currently, only limited literature has explored the factors leading to oral ulcers during orthodontic treatment, and those study results remain debated. Therefore, this study utilized retrospective data to investigate the current status and factors linked to oral mucosal ulcers during orthodontic treatment in our hospital, aiming to provide a reliable reference for improving the clinical prevention of this disease.
A total of 587 patients who underwent orthodontic treatment at the Peking University School and Hospital of Sto
The patients were included if they met the following criteria: (1) Underwent orthodontics in our hospital; (2) Age of ≥ 18 years; and (3) No history of other dental diseases or abnormal dental morphology.
The patients were excluded if they met any of the following criteria: (1) Severe systemic diseases (hypertension, diabetes, or cardiovascular diseases); (2) Communication difficulties that hindered the ability to independently complete the questionnaire; (3) Mental health disorders; or (4) Pregnant or breast-feeding women or other patients deemed not suitable to participate in this research.
All enrolled patients were informed of the research purpose, and signed informed consent was obtained from each patient.
A unified questionnaire was administered to the included patients via telephone interviews to collect the following information: basic information (age, sex, and smoking and drinking history), lifestyle and eating habits (tooth brushing frequency, toothbrush hardness, dietary preference for meat, and dietary temperature), treatment details (treatment course, tooth position, disease type, and orthodontic appliance type), mental factors (anxiety and depression), and trace element levels (zinc, copper, and iron concentrations). Oral mucosal ulcers refer to persistent defects or destruction of the oral epithelium integrity, accompanied by surface necrosis and detachment that result in the formation of a depression. These ulcers can be classified as primary (recurrent aphthous ulcers) and secondary ulcers. The diagnostic criteria for oral mucosal ulcers were according to the criteria specified in the Diseases of Oral Mucosa, 4th edition, People's Medical Publishing House[5]. Additionally, the recurrence of the symptoms in the patients with oral ulcers was recorded. Recurrence was defined as an increase in the area and number of ulcers (i.e. > 1 attack per month) that recurred 3 months following successful treatment.
The study data were entered by trained professionals using EpiData3.1 software via double entry of the collected data and verification of consistency. Finally, the data were logically reviewed and quality-controlled to ensure authenticity, accuracy, and reliability.
Detection of trace elements: After obtaining consent from the patients, 20 μL of peripheral blood was collected from each patient by the senior chief doctor of our hospital. Subsequently, the quantitative measurement of the trace elements, such as zinc, copper, and iron, in the blood samples was conducted utilizing an atomic absorption spectrometer. Quantitative analysis of the trace elements by an atomic absorption spectrometer is based on the principle of light radiation absorption by gaseous atoms, with the wavelength of absorbed light corresponding to the specific emission spectrum of the stimu
Anxiety and depression scores: The Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS) were used to assess the anxiety and depression levels of the patients. The two scales comprise 20 items each, and both scales have a 1–4 scoring system for rating the respondents’ feelings during the most recent week. The cumulative scores of each item are weighted to obtain the total SAS or SDS scores, with higher total scores suggesting greater levels of anxiety or depression, respectively. The current cut-off value for the standard deviation is 50 points, with scores of 50–59, 60–69, and > 69 indicating mild, moderate, and severe anxiety/depression, respectively.
All data were analyzed using SPSS 22.0 statistical software. Measurement data were expressed as mean ± standard deviation or median (interquartile range), while count data were presented as numbers (percentage). Furthermore, the measurement data were tested for normality. Normally distributed data were compared between groups via t-test, whereas the Wilcoxon rank sum test was employed for non-normally distributed data. Intergroup comparisons of count data were performed utilizing the χ2 test. After conducting a univariate analysis with oral ulcer occurrence (with/without) as the dependent variable, variables with P < 0.1 were selected for subsequent modeling. A binary logistic regression model was then used to identify the independent risk factors for oral ulcers. Similarly, a binary logistic regression model with recurrence as a dependent variable was applied to detect the independent risk factors for oral ulcer recurrence.
The test level was set at α = 0.05 (two-tailed test), and P < 0.05 was considered statistically significant.
As demonstrated in Table 1, the basic data of all 587 patients were analyzed after grouping them based on the incidence and recurrence of oral ulcers. Patients with oral ulcers had a mean age of 52.53 ± 11.10 years, and those without oral ulcers exhibited a mean age of 52.98 ± 11.94 years, with no significant difference in age between these two groups (P > 0.05). Among the patients who developed oral ulcers, 153 (26.06%) presented with recurrent symptoms. Except for drinking history, disease type, tooth position, and orthodontic appliance type, all other factors were significantly different between the two groups. Therefore, these factors were included in the models constructed for further comparison analyses.
| Categories | Indicators | Oral ulcer group, n = 297 | Non-oral ulcer group, n = 290 | P value | Recurrence group, n = 144 | Non-recurrence group, n = 153 | P value |
| Sex | Male | 113 (38.05) | 236 (81.38) | < 0.001 | 51 (35.42) | 62 (40.52) | 0.365 |
| Female | 184 (61.95) | 54 (18.62) | 93 (64.58) | 91 (59.48) | |||
| Smoking | No | 178 (59.93) | 258 (88.9) | < 0.001 | 93 (64.58) | 85 (55.56) | 0.113 |
| Yes | 119 (40.07) | 32 (11.03) | 51 (35.42) | 68 (44.44) | |||
| Drinking history | No | 97 (32.66) | 109 (37.59) | 0.211 | 44 (30.56) | 53 (34.64) | 0.453 |
| Yes | 200 (67.34) | 181 (62.41) | 100 (69.44) | 100 (65.36) | |||
| Disease type | Dental caries | 152 (51.18) | 149 (51.38) | 0.484 | 69 (47.92) | 83 (54.25) | 0.253 |
| Dentofacial deformity | 72 (24.24) | 60 (20.69) | 41 (28.47) | 31 (20.26) | |||
| Periodontal disease | 73 (24.58) | 81 (27.93) | 34 (23.61) | 39 (25.49) | |||
| Toothbrush hardness | Soft | 151 (50.84) | 199 (68.62) | < 0.001 | 95 (65.97) | 56 (36.60) | < 0.001 |
| Hard | 146 (49.16) | 91 (31.38) | 49 (34.03) | 97 (63.40) | |||
| Dietary preference for meat | No | 218 (73.40) | 243 (83.79) | 0.002 | 108 (75.00) | 110 (71.90) | 0.545 |
| Yes | 79 (26.60) | 47 (16.21) | 36 (25.00) | 43 (28.10) | |||
| Dietary temperature | Warm | 76 (25.59) | 105 (36.21) | 0.005 | 39 (27.08) | 37 (24.18) | 0.567 |
| Hot | 221 (74.41) | 185 (63.79) | 105 (72.92) | 116 (75.82) | |||
| Treatment course | ≤ 1 year | 84 (28.28) | 157 (54.14) | < 0.001 | 47 (32.64) | 37 (24.18) | 0.106 |
| > 1 year | 213 (71.72) | 133 (45.86) | 97 (67.36) | 116 (75.82) | |||
| Tooth position | Non-anterior tooth region | 158 (53.20) | 136 (46.90) | 0.127 | 89 (61.81) | 69 (45.10) | 0.004 |
| Anterior tooth region | 139 (46.80) | 154 (53.10) | 55 (38.19) | 84 (54.90) | |||
| Orthodontic appliance type | Straight-wire bracket | 138 (46.46) | 120 (41.38) | 0.215 | 67 (46.53) | 71 (46.41) | 0.983 |
| Conventional straight wire | 159 (53.54) | 170 (58.62) | 77 (53.47) | 82 (53.59) | |||
| Age | < 60 years | 179 (60.27%) | 226 (77.93%) | < 0.001 | 95 (65.97) | 84 (54.90) | 0.051 |
| ≥ 60 years | 118 (39.73%) | 64 (22.07%) | 49 (34.03) | 69 (45.10) | |||
| SAS score | 44.66 (5.58) | 37.31 (5.54) | < 0.001 | 44.69 (5.67) | 44.64 (5.51) | 0.940 | |
| SDS score | 47.04 (7.51) | 37.16 (5.15) | < 0.001 | 47.13 (7.12) | 46.96 (7.88) | 0.849 | |
| Zn | 97.95 (20.53) | 127.88 (26.83) | < 0.001 | 98.91 (21.36) | 97.05 (19.74) | 0.434 | |
| Cu | 17.04 (6.40) | 17.70 (6.03) | 0.201 | 17.15 (6.48) | 16.93 (6.35) | 0.773 | |
| Fe | 9.14 (1.50) | 9.31 (1.52) | 0.158 | 9.16 (1.49) | 9.12 (1.51) | 0.830 |
Variables were assigned values as outlined in Table 2, and the independent variables with significant differences (P < 0.1) were included in the univariate analysis to establish the model with oral ulcers as the dependent variable. Age (60 years: odds ratio [OR]: 6.820; 95% confidence interval [CI]: 2.226–20.893), smoking history (smoking: OR: 4.434; 95%CI: 2.527–7.782), toothbrush hardness (hard: OR: 2.804; 95%CI: 1.746–4.505), dietary temperature (hot diet: OR: 1.399; 95%CI: 1.220–1.722), treatment course (> 1 year, OR: 3.830; 95%CI: 2.203–6.659), and tooth brushing frequency (> 1 time per day: OR: 0.228; 95%CI: 0.138–0.377) were found to be independent factors for oral mucosal ulcers (P < 0.05). Furthermore, the level of the trace element Zn (OR: 0.945; 95%CI: 0.927–0.964) was a protective factor against oral ulcers, while the SAS (OR: 1.284; 95%CI: 1.197–1.378) and SDS (OR: 1.322; 95%CI: 1.231–1.419) scores were demonstrated to be risk factors. Table 3 provides the complete details of the analysis.
| Variable | Assigned values |
| Sex | Male = 1; female = 2 |
| Smoking history | No = 0; yes = 1 |
| Drinking history | No = 0; yes = 1 |
| Tooth brushing frequency | ≤ 1 time per day = 0; > 1 time per day = 1 |
| Toothbrush hardness | Soft = 0; hard = 1 |
| Dietary preference for meat | No = 0; yes =1 |
| Dietary temperature | Warm = 0; hot =1 |
| Treatment course | ≤ 1 year = 0; > 1 year = 1 |
| Tooth position | Non-anterior tooth region = 0; anterior tooth region = 1 |
| Disease type | Dental caries = 1; dentofacial deformity = 2; periodontal disease =3 |
| Orthodontic appliance type | Straight-wire bracket = 1; conventional straight-wire = 2 |
| Recurrence | Without = 0; with = 1 |
| Parameters | Univariate model | Multivariate model | ||||
| OR | 95%CI | P value | OR | 95%CI | P value | |
| Age | ||||||
| < 60 years | 1.000 | 1.000 | ||||
| ≥ 60 years | 7.116 | 4.880–10.377 | < 0.001 | 6.820 | 2.226–20.893 | < 0.001 |
| Smoking history | ||||||
| No | 1.000 | 1.000 | ||||
| Yes | 5.390 | 3.491–8.323 | < 0.001 | 4.434 | 2.527–7.782 | < 0.001 |
| Toothbrush hardness | ||||||
| Soft | 1.000 | 1.000 | ||||
| Hard | 2.114 | 1.510–2.960 | < 0.001 | 2.804 | 1.746–4.505 | < 0.001 |
| Dietary preference for meat | ||||||
| No | 1.000 | 1.000 | ||||
| Yes | 1.874 | 1.250–2.808 | 0.002 | 1.719 | 0.994–2.973 | 0.053 |
| Dietary temperature | ||||||
| Warm | 1.000 | 1.000 | ||||
| Hot | 1.650 | 1.158–2.351 | 0.006 | 1.399 | 1.220–1.722 | 0.002 |
| Treatment course | ||||||
| ≤ 1 year | 1.000 | 1.000 | ||||
| > 1 year | 2.993 | 2.126–4.215 | < 0.001 | 3.830 | 2.203–6.659 | < 0.001 |
| Sex | ||||||
| Male | 1.000 | 1.000 | ||||
| Female | 2.328 | 1.621–3.343 | < 0.001 | 1.610 | 0.933–2.780 | 0.087 |
| Tooth brushing frequency | ||||||
| ≤ 1 time per day | 1.000 | 1.000 | ||||
| > 1 time per day | 0.309 | 0.218–0.437 | < 0.001 | 0.228 | 0.138–0.377 | < 0.001 |
| Zn level | 0.947 | 0.938–0.957 | < 0.001 | 0.945 | 0.927–0.964 | < 0.001 |
| SAS score | 1.262 | 1.213–1.314 | < 0.001 | 1.284 | 1.197–1.378 | < 0.001 |
| SDS score | 1.278 | 1.228–1.331 | < 0.001 | 1.322 | 1.231–1.419 | < 0.001 |
We further analyzed the recurrence of oral ulcers by modeling, with disease recurrence as the dependent variable and in
| Indicators | B | SE | Wald | P value | OR | 95%CI |
| Smoking history | 1.278 | 0.344 | 13.806 | < 0.001 | 3.588 | 1.829–7.040 |
| Tooth brushing frequency ≤ 1 time per day | 1.063 | 0.352 | 9.111 | 0.003 | 2.894 | 1.452–5.770 |
| Dentofacial deformity | −0.927 | 0.350 | 7.008 | 0.008 | 0.396 | 0.199–0.786 |
| Hard toothbrush | 2.067 | 0.342 | 36.555 | < 0.001 | 7.905 | 4.044–15.451 |
| Non-dietary preference for meat | −0.659 | 0.345 | 3.639 | 0.046 | 0.517 | 0.263–0.984 |
| Disease in anterior tooth region | 0.841 | 0.334 | 6.354 | 0.012 | 2.319 | 1.206–4.462 |
In recent years, the proportion of people paying attention to the beauty and alignment of their teeth has been increasing due to the expanding and evolving social relationships and aesthetic needs[6]. Related research has shown that the number of individuals receiving orthodontic treatment in China has been growing at present, with an emerging trend in the younger population[7,8]. Although orthodontic treatment provides a good diagnostic effect and can improve facial beauty, it can also lead to numerous complications, such as enamel demineralization and oral mucosal ulcers, owing to the use of external appliances. Oral ulcers usually present within 2 week after commencing orthodontic treatment. At the initial treatment stage, the mucosa can become ulcerated following contact with orthodontic brackets. Ulcers may also appear during treatment because of the irritation at the end of the ligature or archwire. In this study, 153 patients (26.06%) experienced the symptoms of recurrent oral ulcers, similar to the recurrence rate of 22.24% (117 of 526 patients) in an investigation by Liu et al[9]. Oral ulcers are a multifactorial disease, with the risk factors varying across studies. Moreover, the research findings may exhibit deviations in populations from different regions and ethnicities. Therefore, this study explored the current status of oral ulcers during orthodontic treatment and the related factors in 587 patients, providing useful reference and evidence for the clinical prevention of this disease.
According to this study results, age < 60 years, smoking history, hard toothbrush, hot diet, treatment course for > 1 year, and tooth brushing frequency of > 1 time per day were associated with oral ulcer occurrence. Additionally, Zn level (OR: 0.945; 95%CI: 0.927–0.964) served as a protective factor for oral ulcers, while the SAS (OR: 1.284; 95%CI: 1.197–1.378) and SDS (OR: 1.322; 95%CI: 1.231–1.419) scores were risk factors. Age ≥60 years was identified as an independent risk factor for oral ulcer development, potentially because older patients were more likely to develop oral mucosal ulcers and experience more severe symptoms than those who were younger due to the aging-related effects of decreased meta
Previous studies have also suggested that high dietary temperature is an independent risk factor for oral ulcers[12]. The consumption of food that is excessively hot or at a high temperature can lead to the destruction of oral mucosal cells. Such extremely hot dietary temperatures can result in the scalding of the oral mucosa and traumatic ulcer development, even in the absence of orthodontic treatment. A longer treatment course (i.e. > 1 year) and tooth brushing frequency of ≤ 1 time per day were also found to be risk factors for oral mucosal ulcers in this study. Good brushing habits are known to have a positive impact on oral cleanliness and bacterial elimination in the oral cavity. Conversely, an inadequate fre
Finally, the influence of mental factors on oral ulcers during orthodontic treatment was examined. Our results found that the SAS (OR: 1.284; 95%CI: 1.197–1.378) and SDS (OR: 1.322; 95%CI: 1.231–1.419) scores were risk factors for oral ulcers. Correspondingly, long-term anxiety and depression have been suggested to cause neurological dysfunction in patients[14,15]. A possible explanation for these observations may be that the increased nervousness during orthodontic treatment may activate sympathetic adrenal hormones and induce emotional tension, ultimately reducing patient immunity and causing oral ulcer disease.
In addition to identifying the risk factors for oral ulcers, we further determined the factors linked to oral ulcer recurrence. Our analysis demonstrated that disease type (dentofacial deformity: OR: 0.396; 95%CI: 0.199–0.786) and disease location (anterior tooth region: OR: 2.319; 95%CI: 1.206–4.462) were associated with recurrent oral ulcers. Compared to the other disease types (i.e. dental caries and periodontal disease), dentofacial deformities were not prone to oral ulcer recurrence after orthodontic treatment. This result implied that dentofacial deformities have a specific protective effect against recurrent mouth ulcers. Considering that the anterior tooth region is an area of oral exposure and a frequently used area of the oral cavity, this region may be more prone to recurrent oral mucosal ulcers[16].
In summary, age ≥ 60 years, smoking history, hard toothbrush, hot diet, treatment course for > 1 year, tooth brushing frequency of ≤ 1 time per day, and mental anxiety are independent risk factors for oral mucosal ulcers during orthodontic treatment. Therefore, the incidence of oral ulcers during orthodontic treatment can be reduced by enhancing the protective measures for older patients. Moreover, efforts should be made to promote oral health-related knowledge and encourage patients to maintain good lifestyle habits after orthodontic treatment, including adopting a healthy diet with more vegetables and fruits, supplementing with trace elements and vitamins, employing correct tooth brushing methods, adjusting mentality, and alleviating anxiety and depression. All these strategies will contribute to improving immunity and preventing oral mucosal ulcers in patients during orthodontic treatment.
| 1. | Jiang WX, Xia CL, Ding X, Liu MX, Liu GR. Effects of Periodontal-Orthodontic Combined Treatment on Periodontal Function, Gingival Crevicular Fluid TSLP and IL-33 and its Influence Factors Study of Prognosis in Patients with Invasive Periodontitis. Xiandai Shengwu Yixue Jinzhan. 2022;22:3972-3976+3981. [DOI] [Full Text] |
| 2. | Brancher JA, Spada PP, Meger MN, Fatturri AL, Dalledone M, de Paiva Bertoli FM, Deeley K, Scariot R, Vieira AR, Küchler EC, de Souza JF. The association of genetic polymorphisms in serotonin transporter and catechol-O-methyltransferase on temporomandibular disorders and anxiety in adolescents. J Oral Rehabil. 2019;46:597-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Kretschmer WB, Baciuţ G, Baciuţ M, Sader R. Effect of bimaxillary orthognathic surgery on dysfunction of the temporomandibular joint: a retrospective study of 500 consecutive cases. Br J Oral Maxillofac Surg. 2019;57:734-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Lin L, Duan N, Wang X, Song YF, Wang WM. Study on the correlation between common diseases of oral mucosa and psychological factors. Kouqiang Jibing Fangzhi. 2019;27:236-240. [DOI] [Full Text] |
| 5. | Chen QM. Oral Mucosal Diseases. 4th Edition. People's Health Publishing House, 2012. |
| 6. | Richter GM, Kruppa J, Munz M, Wiehe R, Häsler R, Franke A, Martins O, Jockel-Schneider Y, Bruckmann C, Dommisch H, Schaefer AS. A combined epigenome- and transcriptome-wide association study of the oral masticatory mucosa assigns CYP1B1 a central role for epithelial health in smokers. Clin Epigenetics. 2019;11:105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 7. | Gong F, Wang QQ, Ma L. The effect of fluoxetine in adjuvant treatment of erosive ulcer oral mucosal disease and its influence on patients’ anxiety,depression and quality of life. Guoji Jingshenbingxue Zazhi. 2021;48:703-706. [DOI] [Full Text] |
| 8. | Lv L. Effect of systematic nursing intervention on the occurrence and quality of life of oral mucosal ulcers in patients with nasopharyngeal carcinoma undergoing intensity-modulated radiotherapy. Xiandai Zhenduan Yu Zhiliao. 2018;29:3009-3010. [DOI] [Full Text] |
| 9. | Liu J, Xu H, Tang G, Liu H, Sun Z, Zhou G, Cheng B, Wang W, He H, Guo B, Meng W, Liu Q, Wang J, Luo X, Zhou Y, Jiang L, Zeng X, Dan H, Chen Q. A multi-center cross-sectional study of 1495 Chinese oral lichen planus patients. Oral Dis. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 10. | Lv XD, Wu MM, Zhang LR, Shi YH. Er: Clinical observation of YAG Laser-assisted Ultrasound Therapy in the Treatment of Severe Periodontitis. Linchuang Kouqiang Yixue Zazhi. 202;38:356-359. [DOI] [Full Text] |
| 11. | Zhao Y, Yin Y, Tao L, Nie P, Tang Y, Zhu M. Er:YAG laser vs scaling and root planing as alternative or adjuvant for chronic periodontitis treatment: a systematic review. J Clin Periodontol. 2014;41:1069-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 12. | Fitzpatrick SG, Cohen DM, Clark AN. Ulcerated Lesions of the Oral Mucosa: Clinical and Histologic Review. Head Neck Pathol. 2019;13:91-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 91] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 13. | Hu SL, Qin F, Zheng JH. Dai M. A study on the correlation between polymorphisms of IL-4, IL-6, and IL-13 genes and chronic periodontitis. Hainan Yixue. 2016;27:3455-3457. [DOI] [Full Text] |
| 14. | Tang Y, Liu YP, Li YC. Analysis of the relationship between anxiety-depression and TCM syndrome types in patients with oral lichen planus. Zhongguo Yiyao Kexue. 2020;10:6-9+22. [DOI] [Full Text] |
| 15. | Mainville GN, Marsh WL, Allen CM. Oral ulceration associated with concurrent herpes simplex virus, cytomegalovirus, and Epstein-Barr virus infection in an immunocompromised patient. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119:e306-e314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Diwan B, Shirbhate U, Bajaj P, Reche A, Pahade A. Conventional Scalpel and Diode Laser Approach for the Management of Traumatic Fibroma. Cureus. 2023;15:e47810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |