Published online Aug 6, 2024. doi: 10.12998/wjcc.v12.i22.5217
Revised: May 21, 2024
Accepted: May 30, 2024
Published online: August 6, 2024
Processing time: 81 Days and 22.4 Hours
Goblet cell carcinoid (GCC) of the appendix is a rare tumor characterized by neuroendocrine and adenocarcinoma features. Accurate preoperative diagnosis is very difficult, with most patients complaining mainly of abdominal pain. Com
Between 2017 and 2022, 6 patients with GCC were treated in our hospital. The presenting complaint for 5 of these 6 patients was abdominal pain. All 5 patients underwent appendectomy, including 4 for a preoperative diagnosis of appen
As preoperative diagnosis of GCC is difficult, this possibility must be considered during surgical treatments for presumptive appendicitis.
Core Tip: Diagnosing goblet cell carcinoid (GCC) of the appendix preoperatively is very difficult, because most patients with a chief complaint of acute abdomen undergo appendectomy based on a preoperative diagnosis of appendicitis. Even if colonoscopy is performed, accurate endoscopic diagnosis is very difficult because GCCs show a submucosal growth pattern with invasion of the appendiceal wall. The possibility of GCC must always be kept in mind during surgical treatment for presumptive appendicitis. This report includes an extremely rare example of correct preoperative diagnosis of appendiceal GCC.
- Citation: Toshima T, Inada R, Sakamoto S, Takeda E, Yoshioka T, Kumon K, Mimura N, Takata N, Tabuchi M, Oishi K, Sato T, Sui K, Okabayashi T, Ozaki K, Nakamura T, Shibuya Y, Matsumoto M, Iwata J. Goblet cell carcinoid of the appendix: Six case reports. World J Clin Cases 2024; 12(22): 5217-5224
- URL: https://www.wjgnet.com/2307-8960/full/v12/i22/5217.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i22.5217
Goblet cell carcinoid (GCC; recently referred to as goblet cell adenocarcinoma) is a rare tumor of the appendix that is diagnosed in less than 1% of appendectomy specimens[1]. GCC was first described by Gagné et al[2] in 1969. Histologically, GCCs show both neuroendocrine tumor (NET) and adenocarcinoma morphology. GCCs have more malignant features than NETs, and are thus classified and staged as appendiceal carcinoma[3]. GCC diagnosed histologically before surgery is extremely rare[4]. The frequency of regional nodal metastases with GCCs is about 20%[5]. Colectomy with regional lymph node dissection is therefore recommended as surgical treatment for patients with localized GCC by the American Society of Colon and Rectal Surgeons (ASCRS)[6], the North American Neuroendocrine Tumor Society (NANETS)[7], and the European Neuroendocrine Tumor Society (ENTS)[8].
This report describes 6 cases of GCC treated by ileocecal resection (ICR) in our hospital and presents a review of the literature on GCC cases.
Five of the six patients complained of abdominal pain and the remaining patient presented with vomiting (Table 1).
| Feature | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 |
| Sex | Male | Female | Female | Male | Male | Male |
| Age in year | 44 | 50 | 50 | 72 | 47 | 69 |
| BMI in kg/m2 | 22.8 | 32 | 22.1 | 25 | 27.1 | 23.2 |
| Chief complaint | Vomiting | Abdominal pain | Abdominal pain | Abdominal pain | Abdominal pain | Abdominal pain |
| Laboratory data at 1st visit | ||||||
| WBC as /mm3 | 5190 | 17060 | 8100 | 12510 | 19480 | 15830 |
| CRP in mg/dL | 1.01 | 0.21 | 0.01 | 14.2 | 12.2 | 5.9 |
| CEA in ng/mL | 2.2 | 2.1 | 2.2 | 4 | 1.2 | 5.7 |
| CA19-9 in U/mL | 5.2 | 5.7 | 7.6 | < 0.4 | 5.6 | 3.9 |
| Colonoscopy before operation (biopsy) | Edematous mucosa of cecum (+) | - | - | - | - | - |
| Maximum minor diameter of appendix on CT in mm | 9 | 8 | 9 | 20 | 19 | 17 |
| Initial diagnosis | GCC | Appendicitis | Appendix tumor | Appendicitis | Appendicitis | Appendicitis |
| 1st operation | ICR (open) | Appendectomy | Appendectomy | Appendectomy | Appendectomy | Appendectomy |
| Colonoscopy before 2nd operation (biopsy) | - | Wnl (-) | - | Wnl (-) | Wnl (-) | - |
| 2nd operation | - | ICR (lap) | ICR (lap) | ICR (open) | ICR (lap) | ICR (lap) |
| Lymph node dissection | D3 | D3 | D3 | D3 | D3 | D3 |
| T factor | 4a | 3 | 3 | 3 | 3 | 3 |
| N factor | 1b | 0 | 1a | 0 | 0 | 0 |
| Stage by AJCC | IIIB | IIA | IIIB | IIA | IIA | IIA |
| Tumor size in mm | 70 | 15 | 22 | 50 | 12 | 27 |
| Adjuvant chemotherapy | FOLFOX | - | CAPOX | - | - | - |
| Outcomes (follow-up in mo) | RFS (56) | RFS (30) | RFS (18) | RFS (12) | RFS (6) | RFS (2) |
Characteristics of the 6 patients are shown in Table 1, comprising 4 men and 2 women ranging in age from 44 years to 72 years. Diagnoses of GCC in our hospital were made pre- and postoperatively.
Case 3 had a history of hypertension. Case 4 had Parkinson’s disease and had undergone coronary artery bypass grafting for acute myocardial infarction 15 years earlier. This patient was receiving oral levodopa and aspirin. Case 6 had hy
All 6 patients had no notable personal or family history.
All patients except Case 1 displayed abdominal tenderness and rebound tenderness. Case 1 presented with abdominal distention, but no abdominal tenderness.
With the exception of Cases 1 and 4, inflammatory markers were elevated. In Case 6, carcinoembryonic antigen (CEA) was slightly elevated.
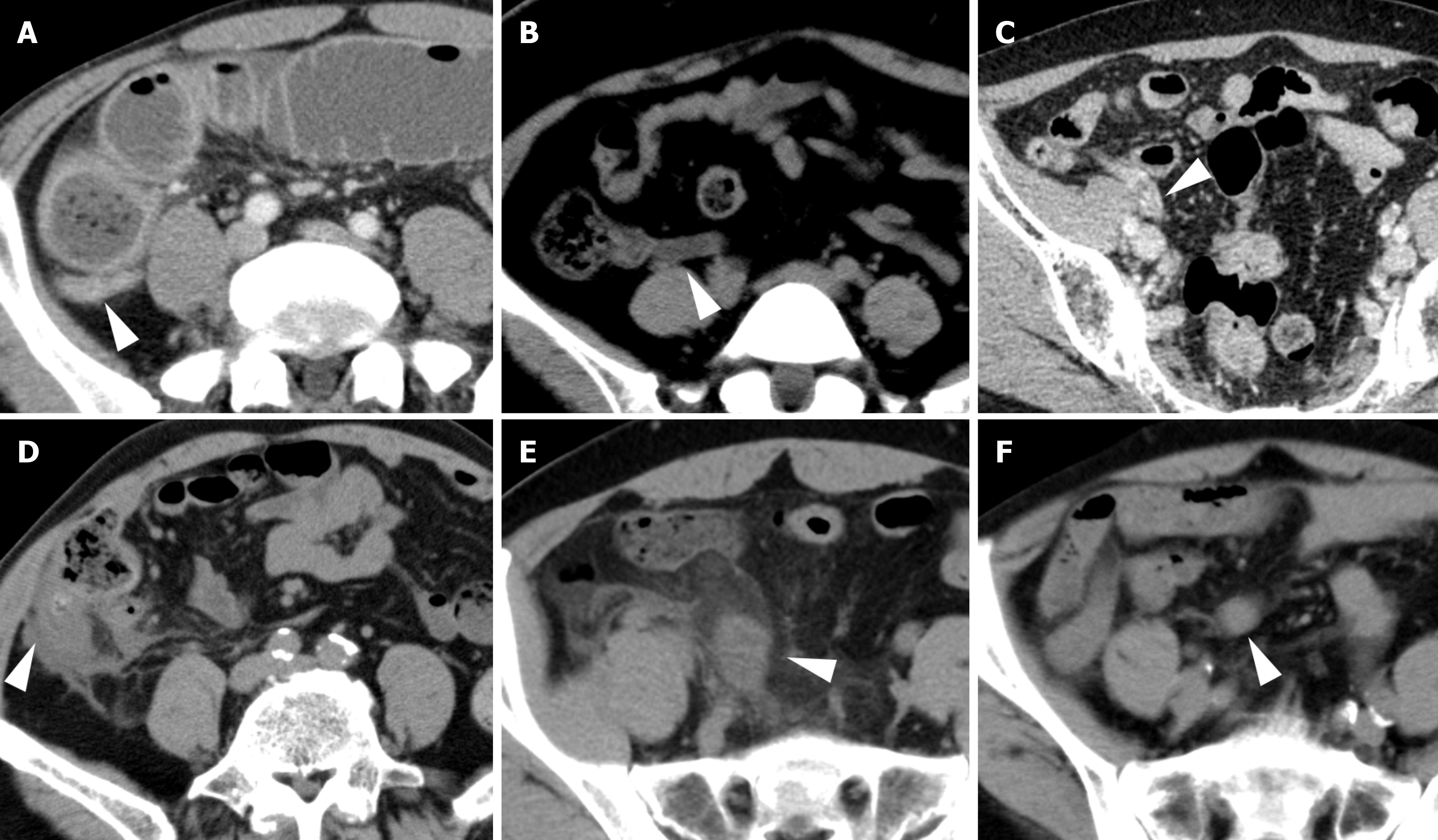
Contrast-enhanced computed tomography: Median maximum minor diameter of the appendix was 13 mm (range, 8-20 mm) (Figure 1).
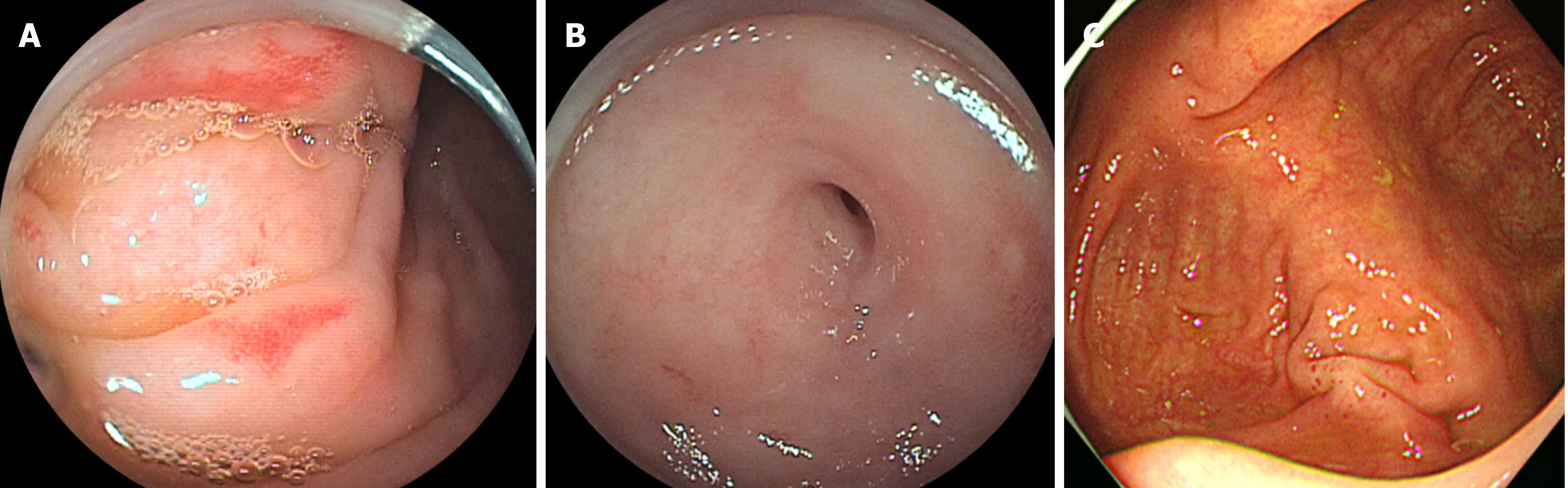
Colonoscopy before first and second operations: Only Case 1 underwent colonoscopy before the first operation for detailed examination of edema of an ileocecal lesion. Although no neoplastic changes were found at the cecum and appendiceal orifice, cecal and appendiceal orifice biopsies showed GCC (Figure 2A and B). Case 4 underwent colono
Case 1 was diagnosed as having GCC of the appendix by biopsy of the cecal wall. Cases 2, 4, 5, and 6 were diagnosed as having acute appendicitis, and Case 3 was diagnosed as an appendiceal tumor.
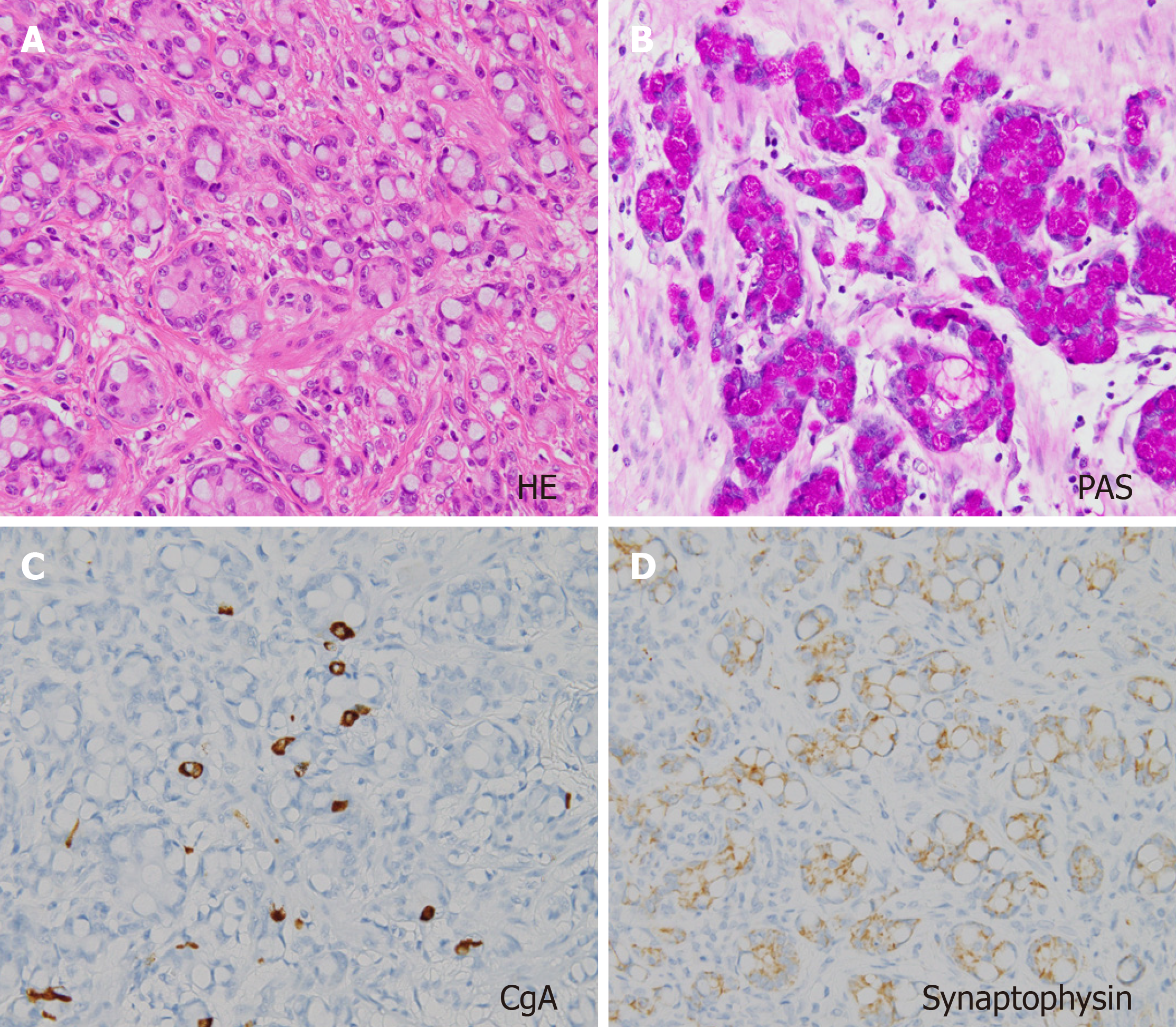
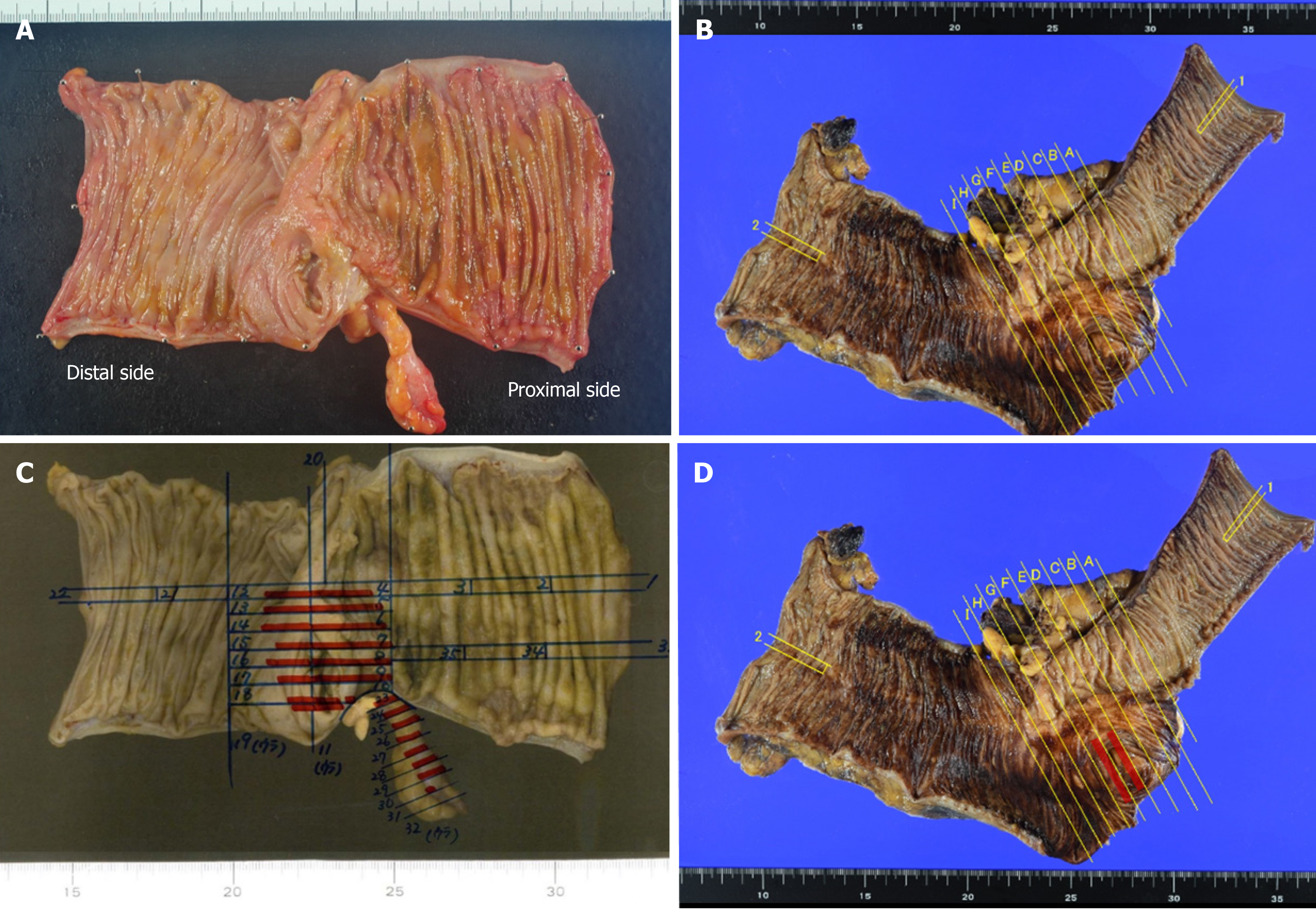
All cases were diagnosed with GCC of the appendix. Pathological examination revealed a tumor cell mixed pattern composed of large goblet cells mimicking signet-ring cells, with mucus in the cytoplasm, positive on periodic acid-Schiff (PAS) staining for mucin, and immunohistostaining positive for chromogranin A (CgA), synaptophysin, CD56, cyto
Case 1 underwent elective ICR with regional lymph node dissection, and the others underwent appendectomy. In Case 4, the first operation was performed for diagnosis and treatment.
Second operations were performed for 5 cases (excluding Case 1). All but Case 1 underwent ICR with regional lymph node dissection. Four of the five cases underwent laparoscopic surgery, and the remaining one underwent open surgery. All cases received curative resection.
Adjuvant chemotherapy was provided for 2 cases with lymph node metastasis (Cases 1 and 3) for 6 mo. At a median follow-up of 15 mo (range: 2-56 mo), all cases were alive without recurrence after treatment.
Appendiceal GCCs have an incidence of approximately 0.01 to 0.05 per 100000 persons per year, and they are very rare tumors[9]. Appendiceal carcinomas are often found incidentally after surgery for a preoperative diagnosis of appen
Appendiceal cancer presents with significant histopathological variety and is further classified into adenocarcinoma, NET, mucinous cystadenocarcinoma, GCC, and signet ring cell tumor[11]. GCCs have features of both adenocarcinomas and NETs. All GCCs stain positive on PAS staining. Immunohistochemical staining reveals pronounced expression of CgA and synaptophysin, and CEA is the key marker. CK staining for CK20, CK19, and CD56 may assist the diagnosis. Ki-67 immunostaining as a marker of proliferation is widely used for NET grading and staging[12]; Ki-67 has been reported to show a positive correlation with prognosis in gastrointestinal NETs. However, GCCs comprise a heterogeneous set of tumors, which makes the Ki-67 index unreliable for GCC[13]. Therefore, Ki-67 was not investigated in the present cases.
In general, the prognosis is worse for GCCs than for NETs; therefore, GCCs are classified and staged as appendiceal carcinomas, not as NETs[3]. The optimal surgical procedure for localized GCCs is often debated. Some suggest appen
Although only a few retrospective series support a specific benefit from adjuvant chemotherapy, those studies suggest adjuvant chemotherapy in the setting of node-positive disease (Stage III), similar to recommendations for appendiceal adenocarcinomas[17,18].
A literature review of GCCs was conducted using PubMed, revealing a constant increase in the number of GCC case reports in the past decade. This is because of the establishment of a definition of GCCs and increasing the awareness of this pathology among pathologists. Therefore, the review was narrowed down to case reports including over 50 cases (Table 2)[4,15,19]. In summary, GCCs occur most frequently from the age of 50 years, and there are no sex differences. Overall, 37% (172/462) of the total patients had stage IV disease, and 5-year overall survival rates were 40%-60%. Of the above, only Tang et al[4] mentioned preoperative diagnosis of appendiceal GCC in less than 1%.
| Ref. | Cases | Median age in yr (range) | Sex as male/female | Stage I/II/III/IV by AJCC | Colectomy, % | 5-yr OS, % | MST in mo |
| Pham et al[15] | 57 | 55 (mean) | 21/36 | 8/20/6/23 | NA | 45 | 47 |
| Tang et al[4] | 63 | 49 (29-80) | 20/43 | 2/18/3/40 | 57 (75) | 58 | 43 |
| Olsen et al[19] | 83 | 59 (31-77) | 56/27 | 12/35/3/27 | 69 (83) | 58 | 83 |
| Lamarca et al[20] | 74 | 56 (26-83) | 34/40 | 2/29/12/28 | 42 (57) | 48 | 52 |
| Nonaka et al[21] | 105 | 54 (25-79) | 54/51 | 5/52/13/35 | 45 (43) | NA | 67 |
| Tsang et al[22] | 86 | 54 (25-91) | 42/44 | 67 (I-III)/19 | 51 (76) | 68 | NA |
In summary, preoperative diagnosis of GCCs is very difficult. At the time of surgical treatment for presumptive appendicitis, the possibility of GCC must always be kept in mind.
| 1. | Rossi RE, Luong TV, Caplin ME, Thirlwell C, Meyer T, Garcia-Hernandez J, Baneke A, Conte D, Toumpanakis C. Goblet cell appendiceal tumors--management dilemmas and long-term outcomes. Surg Oncol. 2015;24:47-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Gagné F, Fortin P, Dufour V, Delage C. [Tumors of the appendix associating histologic features of carcinoid and adenocarcinoma]. Ann Anat Pathol (Paris). 1969;14:393-406. [PubMed] |
| 3. | Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17:1471-1474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5537] [Cited by in RCA: 6461] [Article Influence: 430.7] [Reference Citation Analysis (0)] |
| 4. | Tang LH, Shia J, Soslow RA, Dhall D, Wong WD, O'Reilly E, Qin J, Paty P, Weiser MR, Guillem J, Temple L, Sobin LH, Klimstra DS. Pathologic classification and clinical behavior of the spectrum of goblet cell carcinoid tumors of the appendix. Am J Surg Pathol. 2008;32:1429-1443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 211] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 5. | Turaga KK, Pappas SG, Gamblin T. Importance of histologic subtype in the staging of appendiceal tumors. Ann Surg Oncol. 2012;19:1379-1385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 152] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 6. | Glasgow SC, Gaertner W, Stewart D, Davids J, Alavi K, Paquette IM, Steele SR, Feingold DL. The American Society of Colon and Rectal Surgeons, Clinical Practice Guidelines for the Management of Appendiceal Neoplasms. Dis Colon Rectum. 2019;62:1425-1438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 92] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 7. | Boudreaux JP, Klimstra DS, Hassan MM, Woltering EA, Jensen RT, Goldsmith SJ, Nutting C, Bushnell DL, Caplin ME, Yao JC; North American Neuroendocrine Tumor Society (NANETS). The NANETS consensus guideline for the diagnosis and management of neuroendocrine tumors: well-differentiated neuroendocrine tumors of the Jejunum, Ileum, Appendix, and Cecum. Pancreas. 2010;39:753-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 426] [Cited by in RCA: 376] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 8. | Pape UF, Perren A, Niederle B, Gross D, Gress T, Costa F, Arnold R, Denecke T, Plöckinger U, Salazar R, Grossman A; Barcelona Consensus Conference participants. ENETS Consensus Guidelines for the management of patients with neuroendocrine neoplasms from the jejuno-ileum and the appendix including goblet cell carcinomas. Neuroendocrinology. 2012;95:135-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 300] [Article Influence: 23.1] [Reference Citation Analysis (0)] |
| 9. | McGory ML, Maggard MA, Kang H, O'Connell JB, Ko CY. Malignancies of the appendix: beyond case series reports. Dis Colon Rectum. 2005;48:2264-2271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 175] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 10. | Falk V, Ballantyne M, Zepeda-Gómez S, Kohansal-Vajargah A. Endoscopic diagnosis of a goblet cell carcinoid tumour of the appendix. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | McCusker ME, Coté TR, Clegg LX, Sobin LH. Primary malignant neoplasms of the appendix: a population-based study from the surveillance, epidemiology and end-results program, 1973-1998. Cancer. 2002;94:3307-3312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 386] [Cited by in RCA: 404] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 12. | Jamali M, Chetty R. Predicting prognosis in gastroentero-pancreatic neuroendocrine tumors: an overview and the value of Ki-67 immunostaining. Endocr Pathol. 2008;19:282-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 78] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 13. | Oberg K, Modlin IM, De Herder W, Pavel M, Klimstra D, Frilling A, Metz DC, Heaney A, Kwekkeboom D, Strosberg J, Meyer T, Moss SF, Washington K, Wolin E, Liu E, Goldenring J. Consensus on biomarkers for neuroendocrine tumour disease. Lancet Oncol. 2015;16:e435-e446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 214] [Article Influence: 21.4] [Reference Citation Analysis (1)] |
| 14. | Varisco B, McAlvin B, Dias J, Franga D. Adenocarcinoid of the appendix: is right hemicolectomy necessary? A meta-analysis of retrospective chart reviews. Am Surg. 2004;70:593-599. [PubMed] |
| 15. | Pham TH, Wolff B, Abraham SC, Drelichman E. Surgical and chemotherapy treatment outcomes of goblet cell carcinoid: a tertiary cancer center experience. Ann Surg Oncol. 2006;13:370-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 77] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 16. | Japanese Society for Cancer of the Colon and Rectum. Japanese Classification of Colorectal, Appendiceal, and Anal Carcinoma: the 3d English Edition [Secondary Publication]. J Anus Rectum Colon. 2019;3:175-195. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 289] [Cited by in RCA: 436] [Article Influence: 72.7] [Reference Citation Analysis (0)] |
| 17. | Fields AC, Lu P, Enzinger A, Goldberg J, Irani J, Bleday R, Nash G, Melnitchouk N. Treatment patterns and outcomes in goblet cell carcinoid tumors of the appendix. J Surg Oncol. 2019;120:1096-1101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | AlMasri S, Nassour I, Kowalsky SJ, Hrebinko K, Singhi AD, Lee KK, Choudry HA, Bartlett D, Zureikat A, Paniccia A. The Role of Adjuvant Chemotherapy in Non-Metastatic Goblet Cell Carcinoid of the Appendix: An 11-Year Experience from the National Cancer Database. Ann Surg Oncol. 2021;28:3873-3881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Olsen IH, Holt N, Langer SW, Hasselby JP, Grønbæk H, Hillingsø J, Mahmoud M, Ladekarl M, Iversen LH, Kjær A, Federspiel BH, Knigge U. Goblet cell carcinoids: characteristics of a Danish cohort of 83 patients. PLoS One. 2015;10:e0117627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Lamarca A, Nonaka D, Lopez Escola C, Hubner RA, O'Dwyer S, Chakrabarty B, Fulford P, Valle JW. Appendiceal Goblet Cell Carcinoids: Management Considerations from a Reference Peritoneal Tumour Service Centre and ENETS Centre of Excellence. Neuroendocrinology. 2016;103:500-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 21. | Nonaka D, Papaxoinis G, Lamarca A, Fulford P, Valle J, Chakrabarty B. A study of appendiceal crypt cell adenocarcinoma (so-called goblet cell carcinoid and its related adenocarcinoma). Hum Pathol. 2018;72:18-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Tsang ES, McConnell YJ, Schaeffer DF, Lee L, Yin Y, Zerhouni S, Schaff K, Speers C, Kennecke HF. Outcomes of Surgical and Chemotherapeutic Treatments of Goblet Cell Carcinoid Tumors of the Appendix. Ann Surg Oncol. 2018;25:2391-2399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |