Published online Aug 6, 2024. doi: 10.12998/wjcc.v12.i22.5184
Revised: May 14, 2024
Accepted: June 11, 2024
Published online: August 6, 2024
Processing time: 99 Days and 23.7 Hours
Autoimmune pancreatitis (AIP) is a chronic form of pancreatitis characterized by diffused enlargement of the pancreas and irregular stenosis of the main pancreatic duct. Some studies have reported that AIP can cause hemorrhage of gastric varices (GV) related to portal hypertension (PH). However, such cases are rare. In addition, the association of PH with AIP is unclear. At the same time, the efficacy and duration of glucocorticoid therapy is also controversial.
In this case, we reported a case of GV in pancreatic PH associated with AIP. Enhanced abdominal computed tomography (CT) suggested splenic vein (SV) and superior mesenteric vein (SMV) thromboses. The patient received a long-term glucocorticoid therapy, that the initial dose of 40 mg is reduced weekly by 5 mg, and then reduced to 5 mg for long-term maintenance. CT and gastroscopic examination after 8 mo of treatment indicated that SV and SMV were recanalized, pancreatic stiffness and swelling were ameliorated, and the GV almost completely disappeared.
Long-term glucocorticoid therapy can alleviate the development of GV in patients with AIP and has potential reversibility.
Core Tip: Few studies have reported pancreatic portal hypertension (PPH) related to autoimmune pancreatitis (AIP). In our case, the complications of superior mesenteric vein and splenic vein thromboses, splenomegaly, and gastric varicose veins were observed with AIP. After 4 mo and 8 mo of glucocorticoid therapy, thrombus recanalization, disappearance of gastric varices (GV), and spleen shrinkage were observed. Glucocorticoid therapy may reduce the development and potential reversibility of GV in patients with AIP, and patients with PPH associated with AIP will benefit more from active steroid therapy. There remains controversy about the duration of hormone therapy, and long-term follow-up is required.
- Citation: Zhang Y, Li ZD, He YJ, Peng W, Luo YJ, Li XA. Glucocorticoid therapy in pancreatic portal hypertension associated with autoimmune pancreatitis: A case report. World J Clin Cases 2024; 12(22): 5184-5188
- URL: https://www.wjgnet.com/2307-8960/full/v12/i22/5184.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i22.5184
Yoshida described the steroid-reactive mass pancreatitis syndrome with elevated autoantibody titers in detail in 1995[1]. Autoimmune pancreatitis (AIP) is divided into types 1 and 2. Type 1 AIP is an autoimmune disease mediated by immunoglobulin G4 (IgG4) involving all organs, whereas type 2 AIP is a specific pancreatic disease, occasionally accompanied by inflammatory bowel disease[2,3]. However, portal hypertension (PH) associated with AIP is uncommon. This case suggested that clinicians should be aware of the possibility of complicated regional PH in patients with AIP. Moreover, continuous glucocorticoid therapy is effective for such cases, and some patients can respond well.
Abdominal pain for 10 d.
The patient experienced progressive aggravation of abdominal pain with no obvious cause 10 d before. The pain was under the xiphoid process; additionally, he experienced insomnia and poor appetite but no fever, jaundice, or vomiting.
The patient used to be in excellent health and had no history of viral hepatitis.
The patient had no history of long-term alcohol consumption or medication, and there were no similar cases in the family.
Physical examination revealed subxiphoid tenderness without rebound tenderness.
Laboratory tests revealed that the test for serum IgG4 was positive. At the same time, the liver function was normal (including aspartate aminotransferase, alanine aminotransferase and total bilirubin), while amylase and lipase were negative. In addition, Hepatitis B virus surface antigen positive, but hepatitis B virus DNA negative.
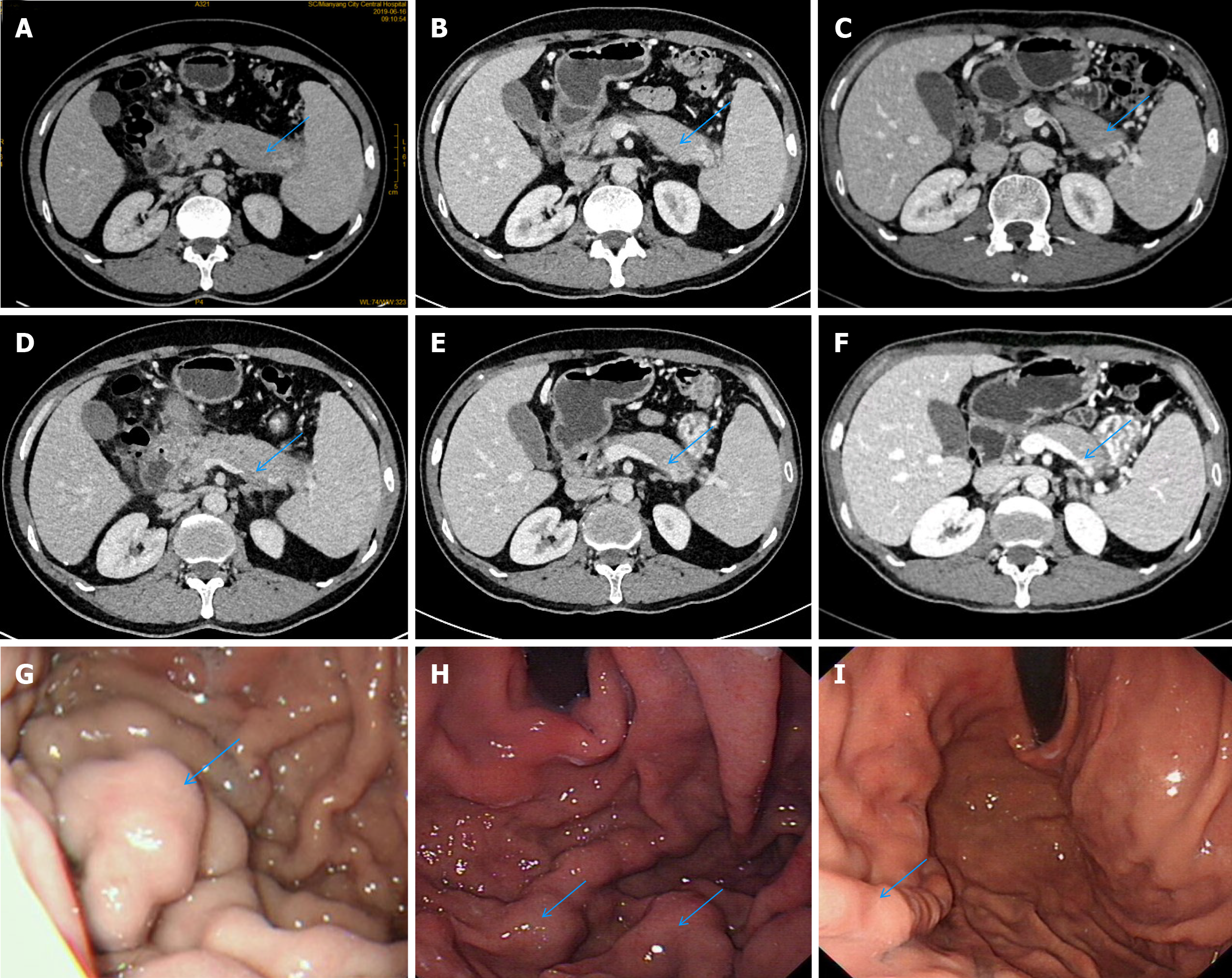
The computed tomography (CT) scan revealed the pancreas with sausage-like changes and stiffness, splenic vein (SV) and superior mesenteric vein (SMV) thromboses, PH, and gastric varicose veins. The results of gastroscopy were severe varicose veins in the fundus, and consistent with those of CT (Figure 1A, D and G).
AIP
We administered long-term glucocorticoid therapy, that the initial dose of 40 mg is reduced weekly by 5 mg, and then reduced to 5 mg for long-term maintenance.
CT and gastroscopic examination after 4 mo (Figure 1B, E and H) and 8 mo (Figure 1C, F and I) of treatment indicated that SV and SMV were recanalized, pancreatic stiffness and swelling were ameliorated, and the GV almost completely disappeared.
AIP is a rare form of chronic pancreatitis that was originally described as “primary inflammatory sclerosis” by Sarles et al[4]. The term “autoimmune pancreatitis” was proposed in 1995[4]. The exact incidence and prevalence are unknown; however, the incidence rate is approximately 2.2 per 100000 people in Japan[5]. AIP is commonly characterized by obstructive jaundice, epigastrium pain, and weight loss. CT and MRI are the critical factors in the diagnosis. In this disease, the pancreas exhibits diffused or local swelling, irregular stenosis of the main pancreatic duct, and enlargement of the proximal pancreas[6]. The pathological manifestations were infiltration of lymphocytes and plasma cells, IgG4-positive cells, pancreatic fibrosis, and phlebitis obliterans[7]. Pancreatic histopathology is not specific, but it helps in distinguishing from pancreatic cancer. In addition, elevated serum IgG4 levels, extrapancreatic organ involvement (type 1 AIP), and response to steroids are common diagnostic criteria for AIP[3]. Steroid-induced remission has been shown to rapidly improve clinical symptoms in up to 99% of cases, improve long-term outcomes, and reduce recurrence rates[8]. It is consistent with the therapeutic effect of the case.
Few studies have reported pancreatic PH (PPH) related to AIP; however, the mechanism is not completely clear. Cheng et al[6] reported a case of PPH associated with AIP, speculating that the swollen pancreas oppresses the SV, obstructs the venous return, and increases the gastrosplenic vein pressure. Splenomegaly and formation of collateral circulation (often involving gastro-omental and short gastric veins) eventually form RPH. The complication of SV obstruction is reported in approximately 7%–20% of AIP cases[9], of which 50%–75% cases exhibit the complication of GV[10]. Juarez et al[11] suggested that SV occlusion and thrombosis were associated with pancreatic inflammation and fibrosis. In our case, the complications of SMV and SV thromboses, splenomegaly, and gastric varicose veins were observed with AIP. However, no evidence of cirrhosis or extrahepatic portal vein obstruction was observed, conforming to the PPH. Combined with the appeal inference, PPH in this patient was considered to be due to a combination of mechanical factors caused by the pressure of the enlarged pancreas, pancreatic inflammation, and phlebitis obliterans.
As per the patient’s wish, we did not perform surgery; however, we administered long-term glucocorticoid therapy and performed close follow-up. Comparing the observations after 4 mo and 8 mo of treatment, thrombus recanalization, disappearance of GV, and spleen shrinkage were observed. Goto et al[12] believed that the blocked SV needs to be reperfused before splenomegaly, otherwise the obstruction will be irreversible. The importance of corticosteroids in PPH is confirmed. In addition, glucocorticoids may prevent AIP from progressing to chronic pancreatitis[13]. However, the use of glucocorticoids is controversial in the long-term prognosis of AIP; therefore, a close follow-up is needed to evaluate its side effects.
In this case, the thrombus recanalization was observed after glucocorticoid therapy, and the GV improved significantly. Therefore, we believe that glucocorticoid therapy can reduce the development and potential reversibility of GV in patients with AIP, and the patients with PPH associated with AIP will benefit more from active steroid therapy. In addition, with the process of long-term hormone therapy, the symptoms improved without hormone-related side effects, which leads to a guiding role for the current use of hormone therapy in AIP. However, there is still controversy about the duration of hormone therapy and long-term follow-up of patients is required. Therefore, a large number of data studies are needed in the future to provide more evidence-based outcomes for clinical practice.
Long-term glucocorticoid therapy can reduce the development and potential reversibility of GV in patients with AIP, and the patients with PPH associated with AIP will benefit more from active steroid therapy.
| 1. | Yoshida K, Toki F, Takeuchi T, Watanabe S, Shiratori K, Hayashi N. Chronic pancreatitis caused by an autoimmune abnormality. Proposal of the concept of autoimmune pancreatitis. Dig Dis Sci. 1995;40:1561-1568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1044] [Cited by in RCA: 925] [Article Influence: 30.8] [Reference Citation Analysis (0)] |
| 2. | Lian MJ, Liu S, Wu GY, Liu SY. Serum IgG4 and IgG for the diagnosis of autoimmune pancreatitis: A systematic review with meta-analysis. Clin Res Hepatol Gastroenterol. 2016;40:99-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Shimosegawa T, Chari ST, Frulloni L, Kamisawa T, Kawa S, Mino-Kenudson M, Kim MH, Klöppel G, Lerch MM, Löhr M, Notohara K, Okazaki K, Schneider A, Zhang L; International Association of Pancreatology. International consensus diagnostic criteria for autoimmune pancreatitis: guidelines of the International Association of Pancreatology. Pancreas. 2011;40:352-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1050] [Cited by in RCA: 1058] [Article Influence: 75.6] [Reference Citation Analysis (0)] |
| 4. | SARLES H, SARLES JC, MURATORE R, GUIEN C. Chronic inflammatory sclerosis of the pancreas--an autonomous pancreatic disease? Am J Dig Dis. 1961;6:688-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 536] [Cited by in RCA: 496] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 5. | Kanno A, Nishimori I, Masamune A, Kikuta K, Hirota M, Kuriyama S, Tsuji I, Shimosegawa T; Research Committee on Intractable Diseases of Pancreas. Nationwide epidemiological survey of autoimmune pancreatitis in Japan. Pancreas. 2012;41:835-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 107] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 6. | Cheng X, Zhou D, Wei J, Zheng S. Regional portal hypertension, systemic lymphadenopathy, and splenomegaly associated with autoimmune pancreatitis. Clin Res Hepatol Gastroenterol. 2013;37:e75-e80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Notohara K, Kamisawa T, Fukushima N, Furukawa T, Tajiri T, Yamaguchi H, Aishima S, Fukumura Y, Hirabayashi K, Iwasaki E, Kanno A, Kasashima S, Kawashima A, Kojima M, Kubota K, Kuraishi Y, Mitsuhashi T, Naito Y, Naitoh I, Nakase H, Nishino T, Ohike N, Sakagami J, Shimizu K, Shiokawa M, Uehara T, Ikeura T, Kawa S, Okazaki K. Guidance for diagnosing autoimmune pancreatitis with biopsy tissues. Pathol Int. 2020;70:699-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 8. | Takuma K, Kamisawa T, Tabata T, Inaba Y, Egawa N, Igarashi Y. Short-term and long-term outcomes of autoimmune pancreatitis. Eur J Gastroenterol Hepatol. 2011;23:146-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 9. | Heider TR, Azeem S, Galanko JA, Behrns KE. The natural history of pancreatitis-induced splenic vein thrombosis. Ann Surg. 2004;239:876-80; discussion 880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 115] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 10. | Butler JR, Eckert GJ, Zyromski NJ, Leonardi MJ, Lillemoe KD, Howard TJ. Natural history of pancreatitis-induced splenic vein thrombosis: a systematic review and meta-analysis of its incidence and rate of gastrointestinal bleeding. HPB (Oxford). 2011;13:839-845. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 164] [Cited by in RCA: 150] [Article Influence: 10.7] [Reference Citation Analysis (1)] |
| 11. | Juarez LA, Gupta RR, Ruhnke GW. Gastric varices and splenic vein obstruction during steroid treatment for autoimmune pancreatitis: A case report and literature review. Medicine (Baltimore). 2018;97:e11940. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Goto N, Mimura J, Itani T, Hayashi M, Shimada Y, Matsumori T. Autoimmune pancreatitis complicated by gastric varices: a report of 3 cases. World J Gastroenterol. 2012;18:4228-4232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Kuraishi Y, Uehara T, Watanabe T, Ashihara N, Ozawa M, Kanai K, Kawa S. Corticosteroids prevent the progression of autoimmune pancreatitis to chronic pancreatitis. Pancreatology. 2020;20:1062-1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |