Published online Aug 6, 2024. doi: 10.12998/wjcc.v12.i22.5140
Revised: May 19, 2024
Accepted: June 5, 2024
Published online: August 6, 2024
Processing time: 130 Days and 22.7 Hours
Heterotopic pancreas (HP) refers to pancreatic tissue located in areas with no vascular or anatomical connection to the pancreas. HP occurs mostly in the stomach, duodenum, and colon, and rarely in the gallbladder.
A 57-year-old woman was referred to our hospital complaining of right upper quadrant discomfort for 3 years. An abdominal computed tomography scan revealed adenomyomatosis with a thickened fundus of the gallbladder. The patient underwent a laparoscopic cholecystectomy, and pathological examination unexpectedly showed heterotopic pancreatic tissue in the gallbladder. The patient had a favorable recovery and was discharged on postoperative day 3. She did not report any symptoms or complications at the 6-mo postoperative follow-up. Pathologists should pay close attention to such pancreatic tissue and carefully examine it for dysplasia or malignancy.
This case provides more information about HP in the gallbladder, a rare occur
Core Tip: In this study, we report a rare case of heterotopic pancreatic tissue in the gallbladder. The patient was initially diagnosed with adenomyomatosis through a computed tomography scan. She underwent a laparoscopic cholecystectomy, and pathological examination revealed heterotopic pancreatic tissue in the gallbladder. Although the malignant transformation of heterotopic pancreatic tissue is rare, pathologists should be aware of this condition and carefully examine the tissue for dysplasia or malignancy.
- Citation: Wang T, Jiang J, Guo LL, Chen X, Chen EB. Heterotopic pancreas in the gallbladder: A case report. World J Clin Cases 2024; 12(22): 5140-5144
- URL: https://www.wjgnet.com/2307-8960/full/v12/i22/5140.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i22.5140
Heterotopic pancreas (HP) refers to the presence of pancreatic tissue outside its normal location, without vascular or anatomical connection to the pancreas[1]. HP is most commonly found in the stomach and duodenum[1], and rarely in the lungs, liver, spleen, and gallbladder[2]. As this condition is often asymptomatic, it is usually diagnosed during pathological examination after cholecystectomy[3]. The prevalence of HP has been reported to vary between 0.55% and 13.7% in autopsy studies and is reported to be 0.2% in surgical cases[4]. HP in the gallbladder is extremely rare, with only 40 cases described in the literature[5]. In this study, we present a case of a 57-year-old woman who underwent laparoscopic cholecystectomy, and histopathological examination revealed HP in the gallbladder. Despite the rarity of malignant transformation in HP, pathologists must pay attention to this entity and ensure the absence of any dysplasia or malignancy.
A 57-year-old woman was admitted to our hospital complaining of right upper quadrant discomfort for 3 years.
The patient presented with a history of right upper quadrant discomfort for 3 years.
The patient denied any history of past illness.
The patient’s mother had died from gallbladder cancer.
Physical examination revealed no pain or tenderness in the right upper abdomen, with a negative Murphy’s sign.
Blood tests, liver function tests, kidney function tests, and serum electrolytes were all within normal limits.
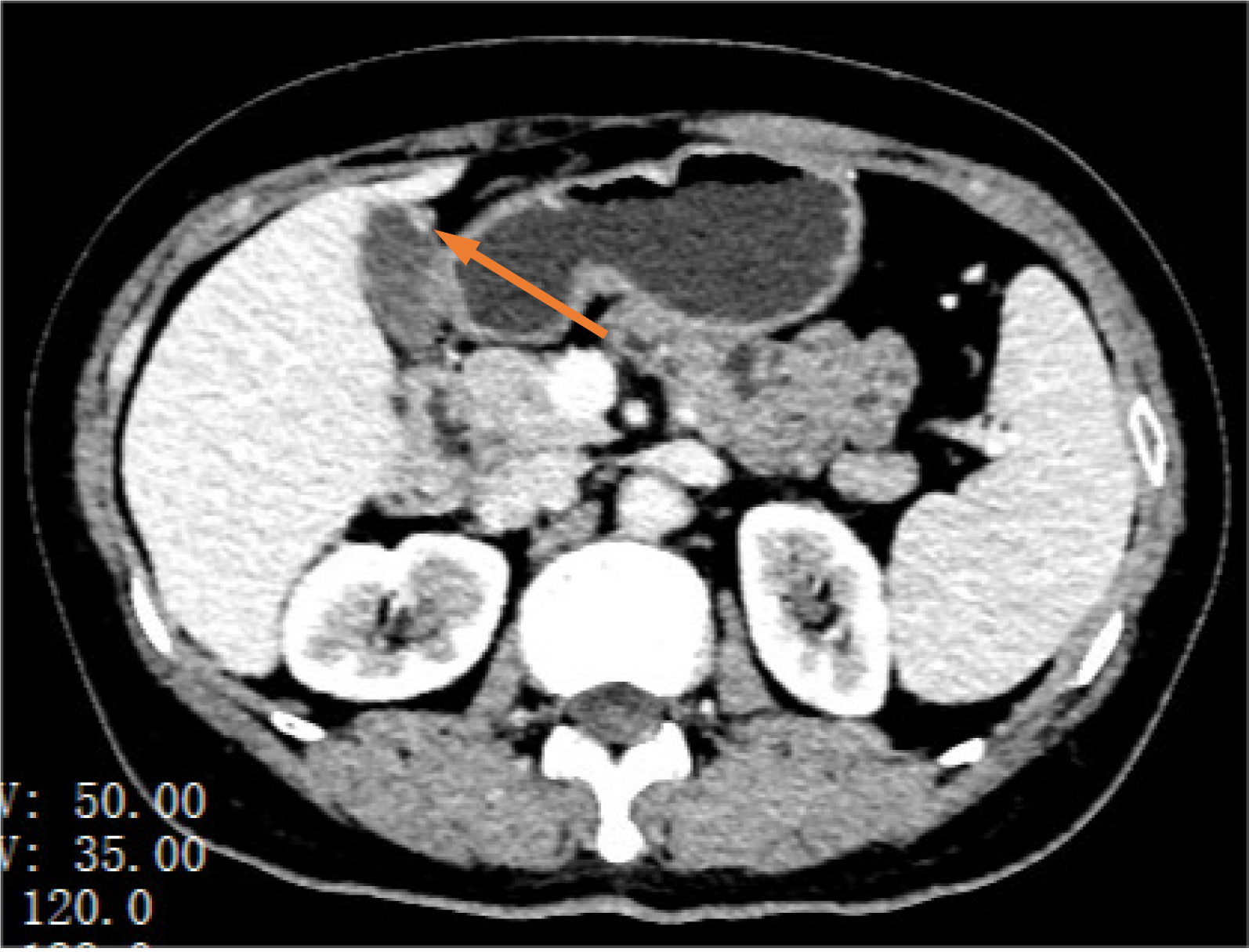
An abdominal computed tomography (CT) scan revealed adenomyomatosis with a thickened fundus of the gallbladder (Figure 1).
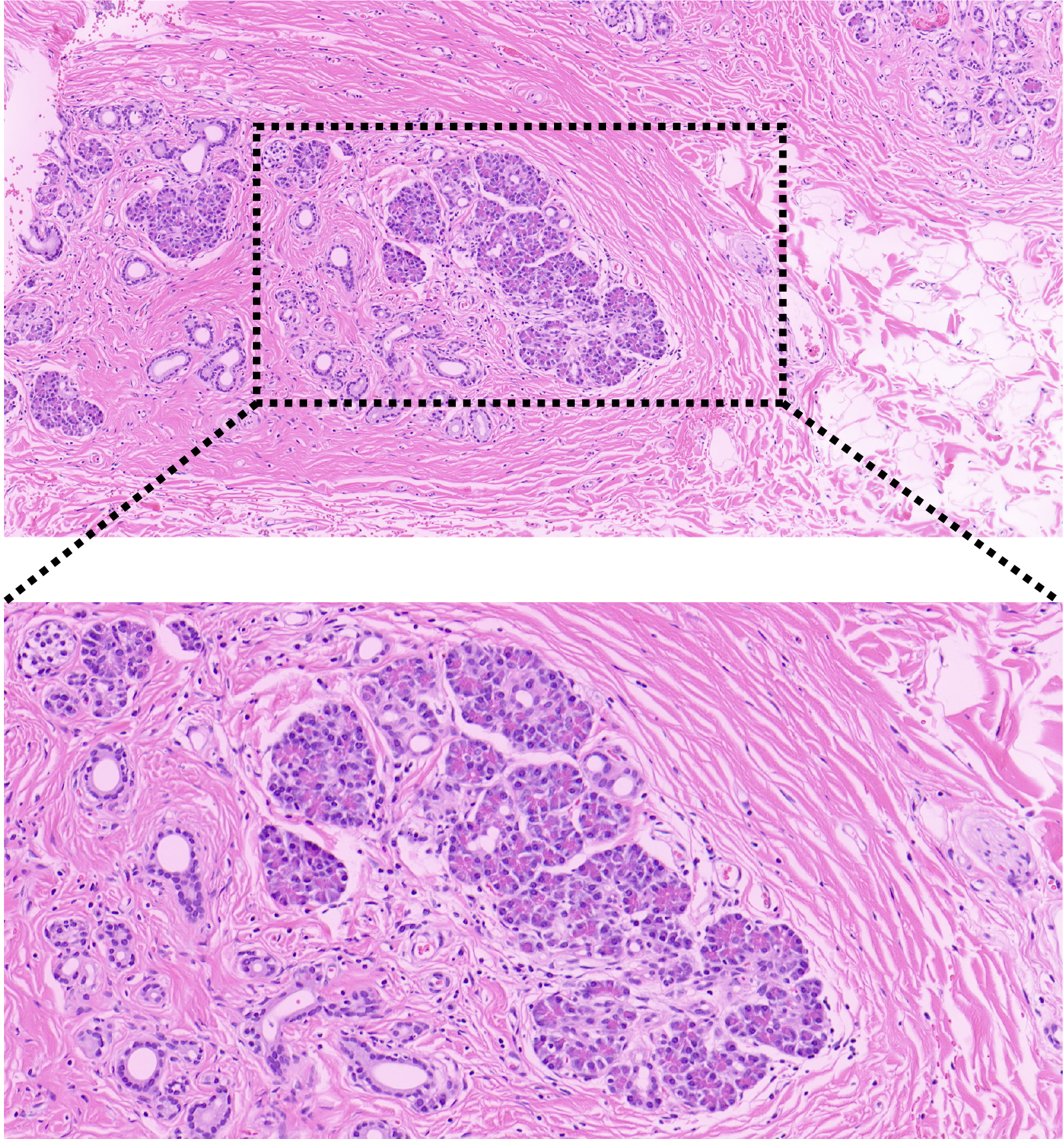
During histopathological examination, gross examination revealed a gallbladder measuring 5.5 cm × 3 cm × 1.5 cm. No polyps or stones were found. Microscopic examination demonstrated characteristics indicative of chronic cholecystitis. In addition, heterotopic pancreatic tissue, consisting of numerous pancreatic acini and a few ducts outside the islets of Langerhans, was found beneath the serosa in the fundus of the gallbladder (Figure 2). No signs of dysplasia or malignancy were observed.
Based on the histopathological findings, the patient was diagnosed with HP in the gallbladder.
Under the initial diagnosis of adenomyomatosis, the patient underwent a laparoscopic cholecystectomy. During the surgery, she was found to have a thickened gallbladder with severe adhesion to the abdominal wall.
The patient had a favorable recovery and was discharged on postoperative day 3. She did not report any complications or symptoms at the 6-mo postoperative follow-up.
We describe a case of HP in the gallbladder, initially diagnosed as adenomyomatosis. Our patient underwent a laparoscopic cholecystectomy, and histopathological examination revealed HP tissue in the gallbladder. HP in the gallbladder is rare, with only 40 cases reported previously[5]. The origin of this abnormal tissue remains unclear. It is widely accepted that HP separates from the normal pancreas during the rotation of the gastrointestinal tract in the embryonic period[6].
The literature demonstrates that HP in the gallbladder has a female predominance, with a female-to-male ratio of approximately 2:1, which may be related to the higher number of cholecystectomies among female patients[5]. The age of patients within reported cases varies between 8 years and 80 years, with a median age of 46 years, and most patients are aged over 40 years. Despite being asymptomatic and usually detected incidentally during histological examination, most cases of HP present with biliary colic or acute/chronic cholecystitis. One patient even developed peritonitis due to the perforation of an inflamed gallbladder[7].
Our case involves a 57-year-old woman who experienced right upper quadrant discomfort for 3 years, consistent with most cases. Preoperative imaging examinations, including CT and ultrasound scans, are typically unable to detect the presence of HP; consequently, the diagnosis of this condition depends on pathological examination after cholecystectomy. Macroscopically, the HP tissue may appear as a nodule or polyp, measuring between a few millimeters and four centimeters[1]. In our case, the thickened fundus of the gallbladder wall revealed by preoperative CT may have been the HP tissue.
HP was first described by Jean Schultz in 1727. In 1909, Heinrich et al[8] classified HP into three types based on its pathological characteristics; this classification was modified by Fuentes in 1973 to include four types[9]. In our case, pathological examination revealed HP composed of acini and ducts, without endocrine islets; hence, it was classified as Type III according to Fuentes’ classification.
Carcinoma arising in HP is very rare, accounting for 0.7% to 1.8% of reported HP cases, and there have been no reports of malignancy of HP in the gallbladder[10-12]. Nevertheless, it is important for pathologists to carefully check for evidence of malignancy in HP, especially in cases of polypoid formation and isolated wall thickening.
The strength of our study is that it adds another reported case initially diagnosed as adenomyomatosis, but ultimately diagnosed as HP in the gallbladder. A limitation of this case is the absence of novel or unique clinical symptoms. Nevertheless, this case report helps increase our understanding of HP in the gallbladder.
HP in the gallbladder is an extremely rare finding, and its diagnosis depends on the pathological examination after cholecystectomy. Our case was initially misdiagnosed as adenomyomatosis because of the thickened fundus of the gallbladder, as indicated by the CT scan. Although the malignant transformation of HP is rare, pathologists need to pay attention to this tissue and perform careful examinations for dysplasia or malignancy. More case reports are needed to reveal its clinical significance.
We sincerely thank the pathologist Jiang Jing for her work in guiding the hematoxylin-eosin reading.
| 1. | Al-Shraim M, Rabie ME, Elhakeem H, Kandeel A, Shah MT, Jamil S. Pancreatic heterotopia in the gallbladder associated with chronic cholecystitis: a rare combination. JOP. 2010;11:464-466. [PubMed] |
| 2. | Filip R, Walczak E, Huk J, Radzki RP, Bieńko M. Heterotopic pancreatic tissue in the gastric cardia: a case report and literature review. World J Gastroenterol. 2014;20:16779-16781. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Sanchiz Cárdenas EM, Soler Humanes R, Lavado Fernández AI, Díaz Nieto R, Suárez Muñoz MA. Ectopic pancreas in gallbladder. Clinical significance, diagnostic and therapeutic implications. Rev Esp Enferm Dig. 2015;107:701-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Kung JW, Brown A, Kruskal JB, Goldsmith JD, Pedrosa I. Heterotopic pancreas: typical and atypical imaging findings. Clin Radiol. 2010;65:403-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Aborajooh E, Ghayada IKK, Lafi YMI. Heterotopic Pancreas in the Gallbladder: Case Report and Literature Review. Case Rep Med. 2021;2021:6611291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Jansen van Rensburg A, Raufian K. A case report of ectopic pancreatic tissue in the gallbladder. J Surg Case Rep. 2022;2022:rjac098. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 7. | Elpek GO, Bozova S, Küpesiz GY, Oğüş M. An unusual cause of cholecystitis: heterotopic pancreatic tissue in the gallbladder. World J Gastroenterol. 2007;13:313-315. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Heinrich H. Ein Beitrag zur Histologie des sogen. akzessorischen Pankreas. Virchows Arch path Anat. 1909;198:392-401. [RCA] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 84] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Trifan A, Târcoveanu E, Danciu M, Huţanaşu C, Cojocariu C, Stanciu C. Gastric heterotopic pancreas: an unusual case and review of the literature. J Gastrointestin Liver Dis. 2012;21:209-212. [PubMed] |
| 10. | Fukino N, Oida T, Mimatsu K, Kuboi Y, Kida K. Adenocarcinoma arising from heterotopic pancreas at the third portion of the duodenum. World J Gastroenterol. 2015;21:4082-4088. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Kaneko T, Ohara M, Okamura K, Fujiwara-Kuroda A, Miyasaka D, Yamabuki T, Takahashi R, Komuro K, Suzuoki M, Iwashiro N, Kato M, Kimura N, Kijima H, Nakamura T, Hirano S. Adenocarcinoma arising from an ectopic pancreas in the duodenum: a case report. Surg Case Rep. 2019;5:126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Cazacu IM, Luzuriaga Chavez AA, Nogueras Gonzalez GM, Saftoiu A, Bhutani MS. Malignant Transformation of Ectopic Pancreas. Dig Dis Sci. 2019;64:655-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |