Published online Jul 26, 2024. doi: 10.12998/wjcc.v12.i21.4680
Revised: May 10, 2024
Accepted: June 11, 2024
Published online: July 26, 2024
Processing time: 119 Days and 5.7 Hours
Acute nonvariceal upper gastrointestinal bleeding (ANVUGIB) is a frequent life-threatening acute condition in gastroenterology associated with high morbidity and mortality. Over-the-scope-clip (OTSC) is a new endoscopic hemostasis tech
To summarize and analyze the effects of the OTSC in prevention of recurrent bleeding, clinical success rate, procedure time, hospital stay, and adverse events in the treatment of ANVUGIB, to evaluate whether OTSC can replace standard endoscopic therapy as a new generation of treatment for ANVUGIB.
The literature related to OTSC and standard therapy for ANVUGIB published before January 2023 was searched in PubMed, Web of Science, EMBASE, Cochra
This meta-analysis involved 11 studies with 1266 patients. Total risk of bias was moderate-to-high. For patients in the OTSC group, 7- and 30-days recurrent bleeding rates, as well as procedure time, hospital stay, and intensive care unit stay, were greatly inhibited. OTSC could significantly improve the clinical success rate of ANVUGIB. OTSC therapy did not cause serious adverse and was effective in reducing patient mortality.
OTSC may provide more rapid and sustained hemostasis, and thus, promote recovery and reduce mortality in patients with ANVUGIB. In addition, the safety of OTSC is assured.
Core Tip: Upper gastrointestinal bleeding, especially Acute nonvariceal upper gastrointestinal bleeding (ANVUGIB) is a common life-threatening acute condition with high morbidity and mortality in gastroenterology. With the advancements in medical technology, a new endoscopic hemostatic technique, called the over-the-scope-clip (OTSC), is being used for ANVUGIB treatment. We performed a meta-analysis to study the role of OTSC in ANVUGIB treatment in terms of pre
- Citation: Yang XZ, Yu DL, Wang Z, Gao ZL. Efficacy and safety of over-the-scope-clips in the therapy of acute nonvariceal upper gastrointestinal bleeding: Meta-analysis. World J Clin Cases 2024; 12(21): 4680-4690
- URL: https://www.wjgnet.com/2307-8960/full/v12/i21/4680.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i21.4680
Upper gastrointestinal bleeding, especially acute nonvariceal upper gastrointestinal bleeding (ANVUGIB), is a frequent life-threatening acute condition in gastroenterology associated with high morbidity and mortality[1]. In recent years, the number of people with gastrointestinal diseases, such as peptic ulcer, erosive esophagitis, and erosive gastritis, has increased yearly due to the influence of alcoholism, poor work habits, and high-intensity work[2]. According to statistics, the annual number of outpatient visits for gastrointestinal diseases in China was approximately 4 million in 2015[3]. Simultaneously, the incidence of the resulting ANVUGIB has increased. ANVUGIB is routinely treated endoscopically by thermal coagulation, hemostatic drug spray, and titanium clip hemostasis. However, approximately 26.3% suffer from recurrent bleeding in the early postoperative period due to excessive bleeding and decreased coagulation function[4], which has an essential role in increasing mortality in patients with ANVUGIB. Therefore, improving endoscopic hemostasis techniques to prevent rebleeding is the key to improving the cure rate of ANVUGIB.
With advances in medical technology, over-the-scope-clip (OTSC), a new endoscopic hemostasis technique, is being used in ANVUGIB therapy. OTSC was more effective than standard therapy for recurrent peptic ulcer bleeding, incre
However, OTSC has limitations in ANVUGIB therapy, such as delayed closure of OTSC in lesions with large caliber arterial injury and deep basal fibrosis, as well as misplacement or shallow placement of OTSC due to poor visualization or unstable endoscopic position[12,13]. Because OTSC has a large size and clamping area, it is not easily dislodged like conventional hemostatic clips, which can cause intestinal stenosis[14]. A literature analysis revealed many studies comparing the efficacy of OTSC with standard therapy in ANVUGIB; however, at a relatively small scale. In addition, the safety and related complications of OTSC during therapy were not reported, which to can limit the use of OTSC in the first-line therapy of ANVUGIB. Therefore, this meta-analysis aims to examine the efficacy and safety of OTSC in ANVUGIB therapy, to provide clinical guidance for the improvement of its first-line treatment regimens.
We searched PubMed, Web of Science, EMBASE, Cochrane, Wanfang, Weipu, and CNKI databases to obtain literature that met the requirements. The following keywords were used in the search: “upper gastrointestinal bleeding” or “upper gastrointestinal tumor” or “stress ulcer” or “peptic ulcer” or “gastric ulcer” or “bleeding” or “hemorrhage” and “acute” or “high-risk” or “refractory” and “over-the-scope clips” and “standard therapy” or “hemoclips” or “thermocoagulation” or “epinephrine” or “recurrent bleeding” or “recurrent hemorrhage” or “clinical success rate” or “procedure time” or “hospital stay” or “mortality” or “adverse events” or “surgery” or “safety”. The search was from January 2000 to January 2023 and was conducted by two researchers with three years of experience.
The literature included in this meta-analysis had to compound the following criteria: (1) Patients diagnosed with ANVUGIB; (2) studies containing the OTSC group, in which patients were treated with OTSC, and the standard therapy group, in which patients were treated with hemoclips, thermocoagulation, or epinephrine under endoscope; (3) contain relevant study indicators, such as recurrent bleeding, clinical success rate, procedure time, hospital stay, or safety (mortality, adverse events, or surgery); and (4) randomized controlled trial study.
(1) Case reports and reviews; (2) without detailed data; (3) < 10 people included in the study; (4) experiments were conducted on animals; and (5) relevant research indicators were not included.
We extracted key data from the included literature in detail, namely the author, year of publication, patient number, therapeutic method, recurrent bleeding, clinical success rate, procedure time, hospital stay, and safety. When necessary, we corresponded with the authors by e-mail to request detailed data.
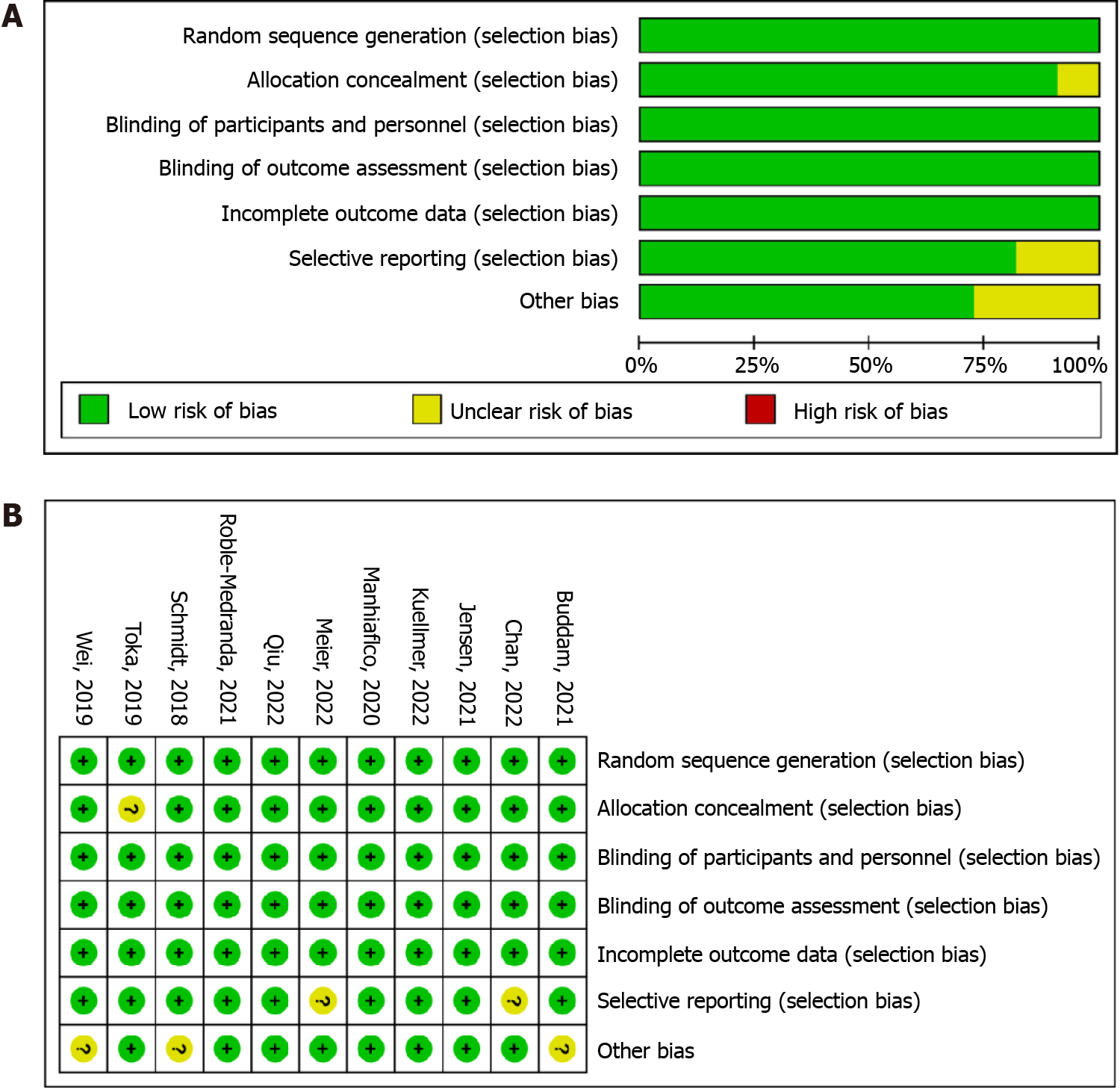
Two reviewers independently assessed the quality of the literature using the Cochrane risk of bias assessment tool, which contains seven domains: randomized sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. The methodological quality of prospective cohort studies and retrospective cohort studies was assessed using the Newcastle-Ottawa Scale. The risk of bias for each study was rated as low, medium, or high. The quality of evidence was assessed using the GRADEpro software and was categorized as high, moderate, low, and very low. A third reviewer arbitrated any disag
Revman 5.3 was used for meta-analysis. The continuous variables in-hospital stay and procedure time were expressed by MD and 95%CI. The dichotomous variables in recurrent bleeding, clinical success rate, and adverse events were expressed by OR and 95%CI. A forest plot was generated using a random-effects or fixed-effects model. For each meta-analysis, Cochran Q and I2 were used to evaluate study heterogeneity. If combined SMD or OR of 95%CI or in the meta-analysis did not overlap with 0, the effect of the outcome index was considered statistically significant. Funnel plots, Egger’s test, and Begg’s tests were used to examine publication bias data analysis was completed using STATA (version 15.0).
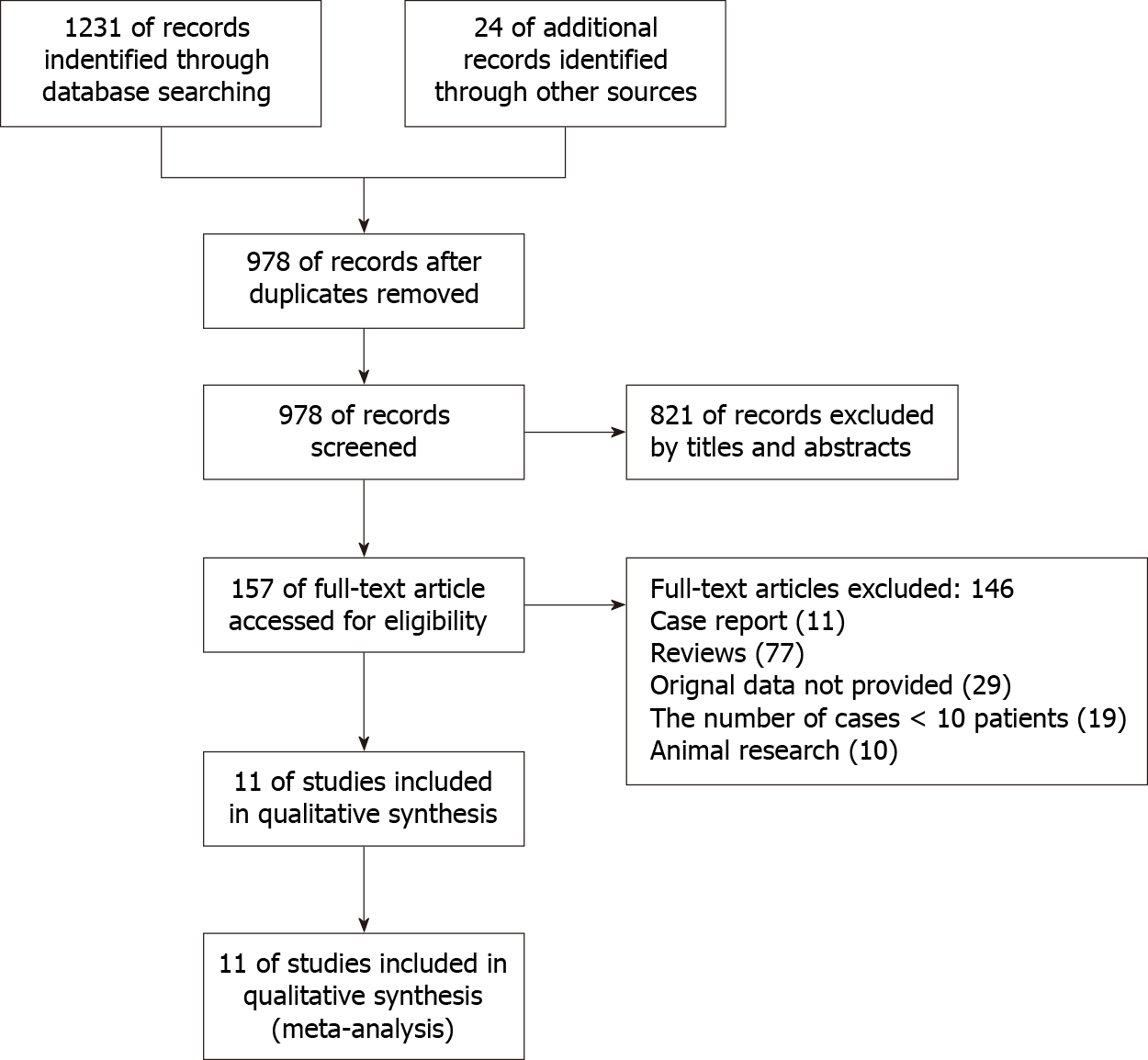
In this meta-analysis, we searched 1255 papers related to OTSC, of which 277 were duplicates. Subsequently, we read the titles and abstracts of the literature to exclude 821 papers with different scope of salvage and correction outcomes from this meta-analysis and retrieved the full-text of 157 papers. After reading the entire text, we excluded 146 papers: Case reports (31), reviews (130), no detailed data provided (59), < 10 people included in the study (29), and the study was conducted on animals (25); 11 studies with 1266 patients were finally included[4-7,11-17] (Figure 1). In the OTSC group, patients with ANVUGIB were treated with OTSC. In the standard therapy group, patients with ANVUGIB were treated with thermal coagulation, anticoagulant spraying, or hemostatic clips. Basic information about the patients included in the literature, the mode of treatment received, and relevant outcome indicators are summarized in Table 1.
| Ref. | Country | Number of patients | Therapeutic method | Recurrent bleeding | Clinical success rate | Procedure time (minute) | Therapy time | Safety | |||||||||||||||
| 7 days | 30 days | Hospital stay (day) | ICU stay (day) | Rate of surgery | In-hospital mortality | Adverse events | |||||||||||||||||
| OTSC | SET | OTSC | SET | OTSC | SET | OTSC | SET | OTSC | SET | OTSC | SET | OTSC | SET | OTSC | SET | OTSC | SET | OTSC | SET | OTSC | SET | ||
| Buddam et al[15], 2021 | United States of America | 21 | 47 | OTSC | Hemoclips, thermocoagulation, epinephrine | 2/21 | 10/47 | 20/21 | 39/47 | 17.08 ± 5.57 | 23 ± 13.77 | 5.72 ± 3.18 | 6.77 ± 5.35 | 0/21 | 2/47 | ||||||||
| Chan et al[7], 2023 | China, Thailand | 50 | 50 | OTSC | Hemoclips, thermocoagulation, epinephrine | 2/50 | 3/50 | 5/50 | 9/50 | 46/50 | 48/50 | 13.72 ± 24.33 | 13.27 ± 16.13 | 3/50 | 1/50 | 2/50 | 4/50 | ||||||
| Jensen et al[11], 2021 | the United States | 25 | 28 | OTSC | Hemoclips, thermocoagulation, epinephrine | 0/25 | 7/28 | 1/25 | 8/28 | 7.56 ± 8.17 | 10 ± 16.19 | 2.4 ± 3.48 | 11.11 ± 37.06 | 0/25 | 0/28 | 0/25 | 0/28 | 0/25 | 4/28 | ||||
| Kuellmer et al[13], 2023 | Germany | 66 | 37 | OTSC | Hemoclips | 10/66 | 5/37 | 49/66 | 31/37 | 15.2 ± 12.4 | 23.1 ± 18.4 | 4.7 ± 6.6 | 16.2 ± 18 | 6/66 | 13/37 | 3/66 | 26/37 | ||||||
| Mangiafico et al[14], 2020 | Italy | 112 | 215 | OTSC | Hemoclips, epinephrine | 13/112 | 32/215 | 15 ± 12 | 13 ± 19 | 8/112 | 20/215 | 0/112 | 1/215 | ||||||||||
| Meier et al[17], 2022 | Germany | 48 | 52 | OTSC | Hemoclips | 4/48 | 8/52 | 6/48 | 8/52 | 44/48 | 38/52 | 27 ± 15 | 28 ± 20 | ||||||||||
| Qiu et al[16], 2022 | China | 21 | 115 | OTSC | Hemoclips, thermocoagulation, epinephrine | 3/21 | 34/115 | 18/21 | 80/115 | ||||||||||||||
| Robles-Medranda et al[12], 2021 | Ecuador | 46 | 49 | OTSC | Hemoclips, epinephrine | 0/46 | 3/49 | 2/46 | 1/49 | 12.06 ± 3.83 | 25.31 ± 19.09 | 11.15 ± 20.66 | 11.43 ± 20.62 | ||||||||||
| Schmidt et al[8], 2020 | Germany | 33 | 33 | OTSC | Hemoclips, thermocoagulation, epinephrine | 3/33 | 5/33 | 5/33 | 19/33 | 31/33 | 19/33 | 29.27 ± 35.65 | 33.2 ± 44.17 | 1/33 | 1/33 | 4/33 | 2/33 | 5/33 | 1/33 | ||||
| Toka et al[4], 2019 | Turkey | 56 | 56 | OTSC | Hemoclips | 2/56 | 8/56 | 55/56 | 45/56 | 5 ± 1.46 | 9.47 ± 2.34 | 3.5 ± 1.04 | 4.37 ± 1.86 | ||||||||||
| Wei et al[6], 2019 | China | 26 | 80 | OTSC | Hemoclips, thermocoagulation, epinephrine | 26/26 | 46/80 | 8.86 ± 3.53 | 9.97 ± 3.59 | 0/26 | 24/80 | 0/26 | 11/80 | ||||||||||
After evaluation, the quality of included studies was moderate-to-high. All included literature was randomized and triple-blinded to the investigators, participants, and outcome analysis during the study, and the study data were complete. Two studies had “selective reporting” and one study did not mention “allocation consideration” (Figure 2).
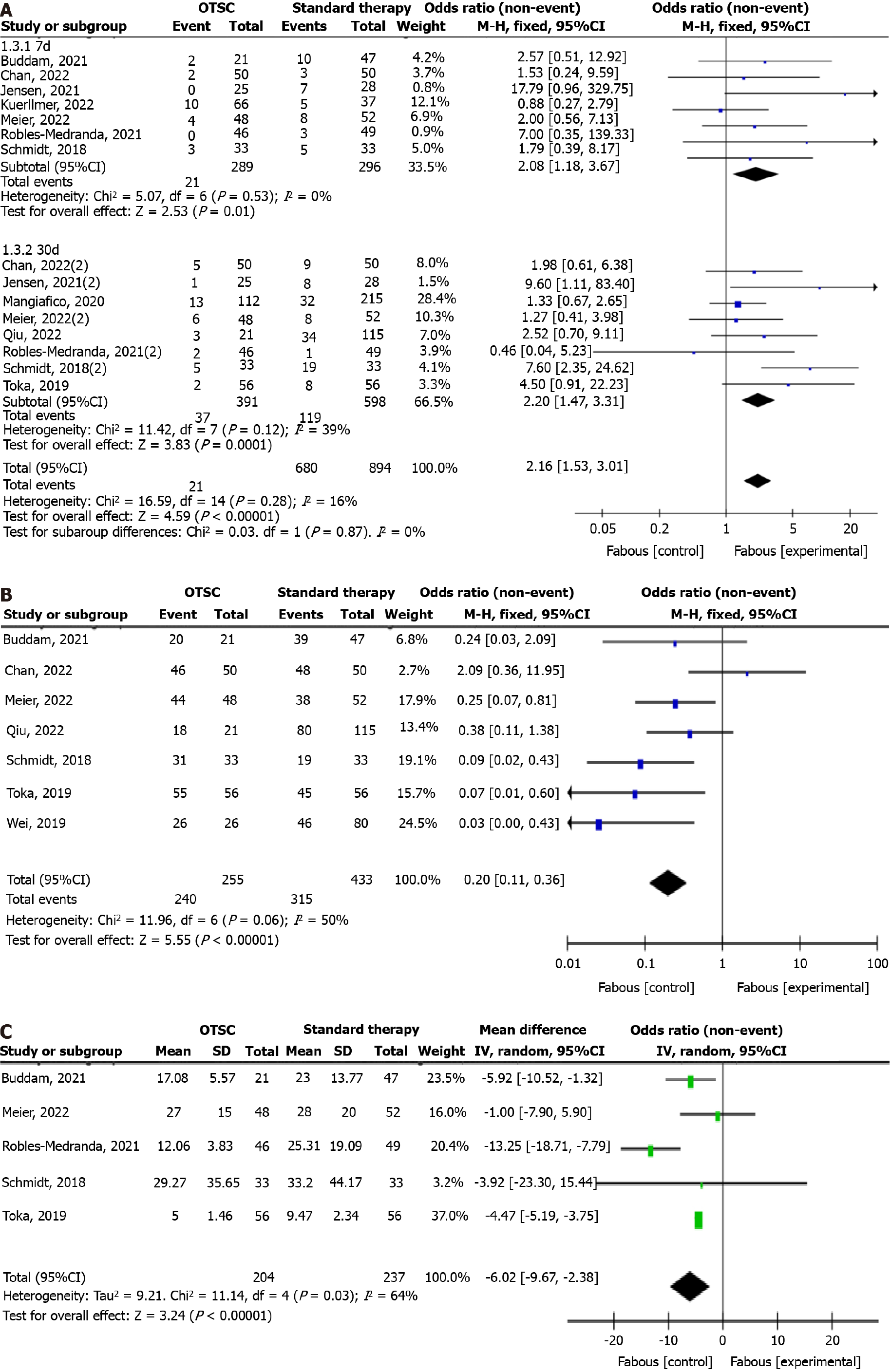
In the assessment of recurrent bleeding, we performed subgroup analyses according to recurrent bleeding at 7 and 30 days. Data from 15 groups of the 10 studies suggested that the incidence of 7-days recurrent bleeding in the OTSC group was significantly lower, as was the incidence of recurrent bleeding at 30 d, and combined OR values were 2.08 (95%CI: 1.18-3.67; P = 0.01) and 2.20 (95%CI: 1.47-3.31; P = 0.0001; Figure 3A). Therefore, OTSC could prevent the occurrence of rebleeding after ANVUGIB therapy and improve patient prognosis.
To assess the hemostatic efficacy of ANVUGIB, we analyzed data from 7 groups of 7 studies regarding hemostatic success rate. OTSC had a higher rate of hemostatic success, with a combined OR of 0.2 (95%CI: 0.11-0.36; P < 0.00001; Figure 3B). Therefore, the use of OTSC in ANVUGIB therapy can improve hemostasis, and thus, enhance the clinical success rate.
By analyzing 5 sets of data on hemostasis time from 5 studies, we found that OTSC took less time in ANVUGIB rescue, with a combined MD of -6.02 (95%CI: -9.67 to -2.38; P = 0.001; Figure 3C). This indicates that OTSC can achieve definitive hemostasis in a shorter time and improve clinical efficiency.
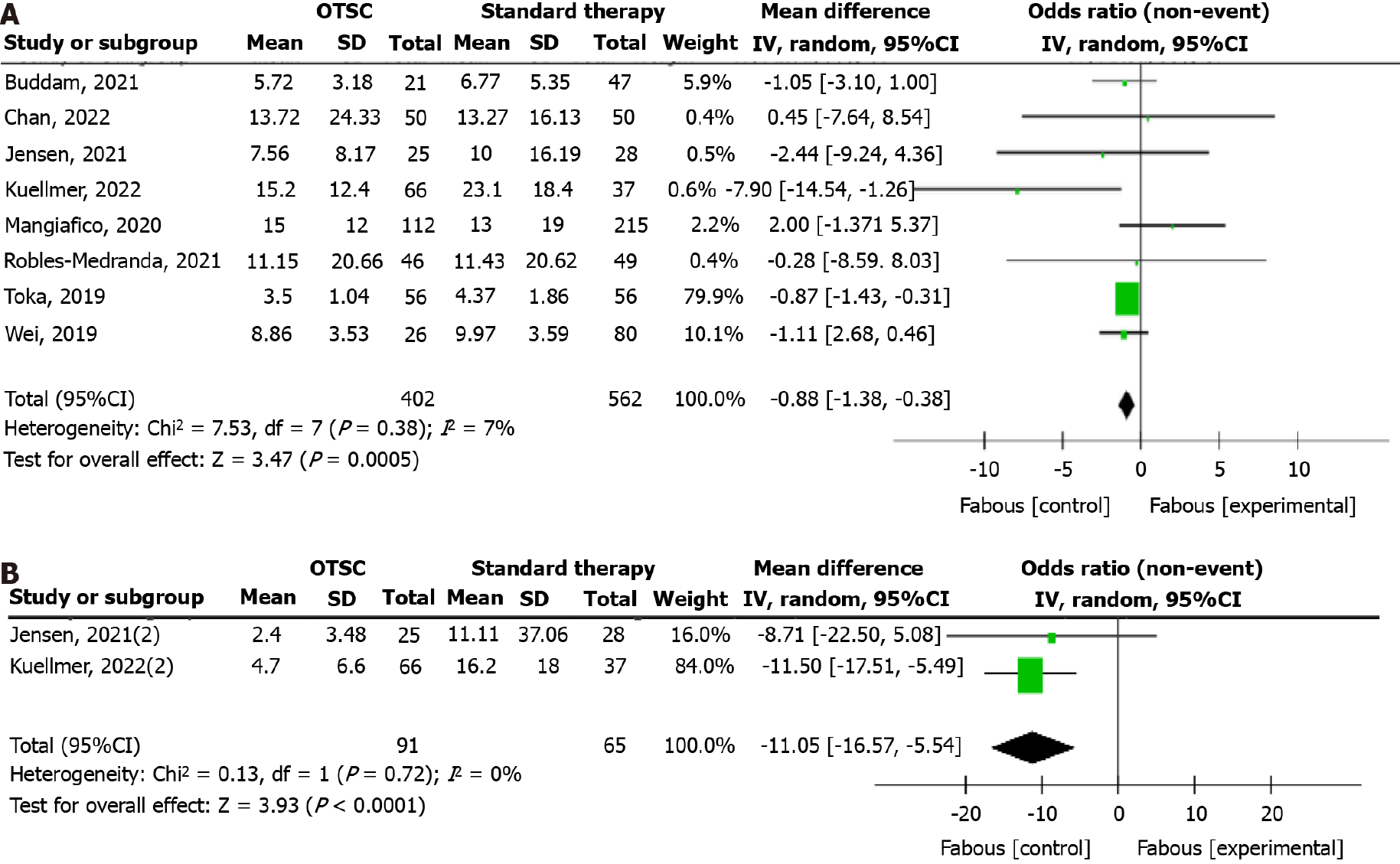
To better assess patient recovery, a comprehensive analysis of mean length of hospital stay and intensive care unit (ICU) stay was performed. In total, 8 sets of data from 8 studies showed that the OTSC system was effective in reducing mean length of stay in patients with ANVUGIB, with a combined MD of -0.88 (95%CI: -1.38 to -0.38; P = 0.0005; Figure 4A). The OTSC system could markedly reduce ICU length of stay, with a combined MD of -11.05 (95%CI: -16.57 to -5.54; P < 0.0001; Figure 4B). Therefore, patients with ANVUGIB have better recovery outcomes and shorter hospital stays after OTSC therapy.
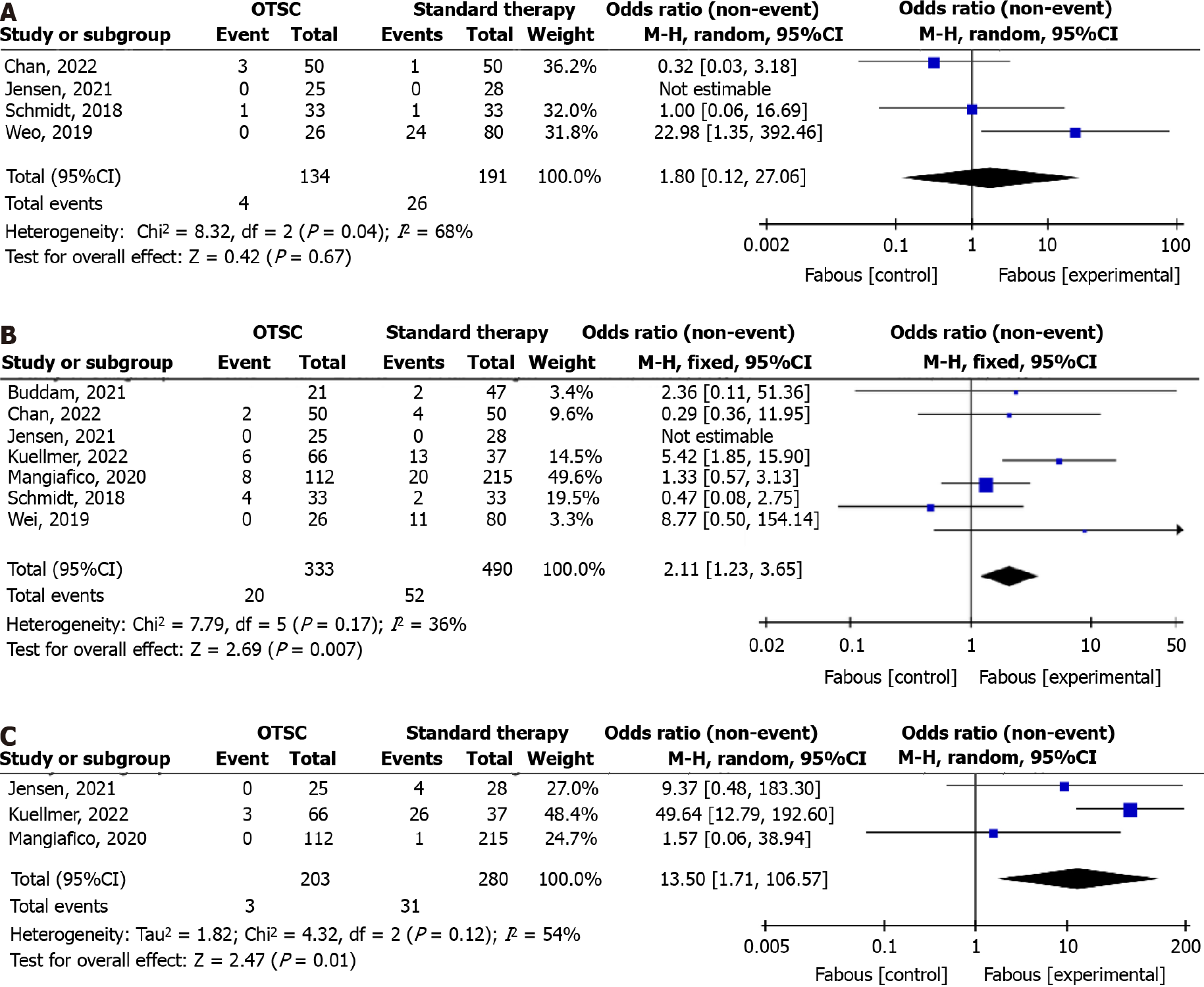
We evaluated the safety of the OTSC system in terms of operative rate, mortality, and complications. In total, 4 groups of data from 4 studies showed no obvious difference in patient number referred to surgical hemostasis after OTSC compared with standard therapy, with a combined OR of 1.80 (95%CI: 0.12 to 27.06; P = 0.67; Figure 5A). Analysis of data from 7 groups of 7 studies on in-hospital mortality revealed that OTSC was effective in reducing mortality, with a combined OR of 2.11 (95%CI: 1.23 to 3.65; P = 0.007; Figure 5B). Regarding occurrence of adverse events, such as luminal stenosis, gastroesophageal junction obstruction, and procedural deviations due to tissue fibrosis, data from 3 groups in 3 studies showed that OTSC was useful in minimizing the associated complications, with a combined OR of 13.5 (95%CI: 1.71 to 106.57; P = 0.01; Figure 5C). Therefore, the safety of the OTSC system for ANVUGIB is guaranteed.
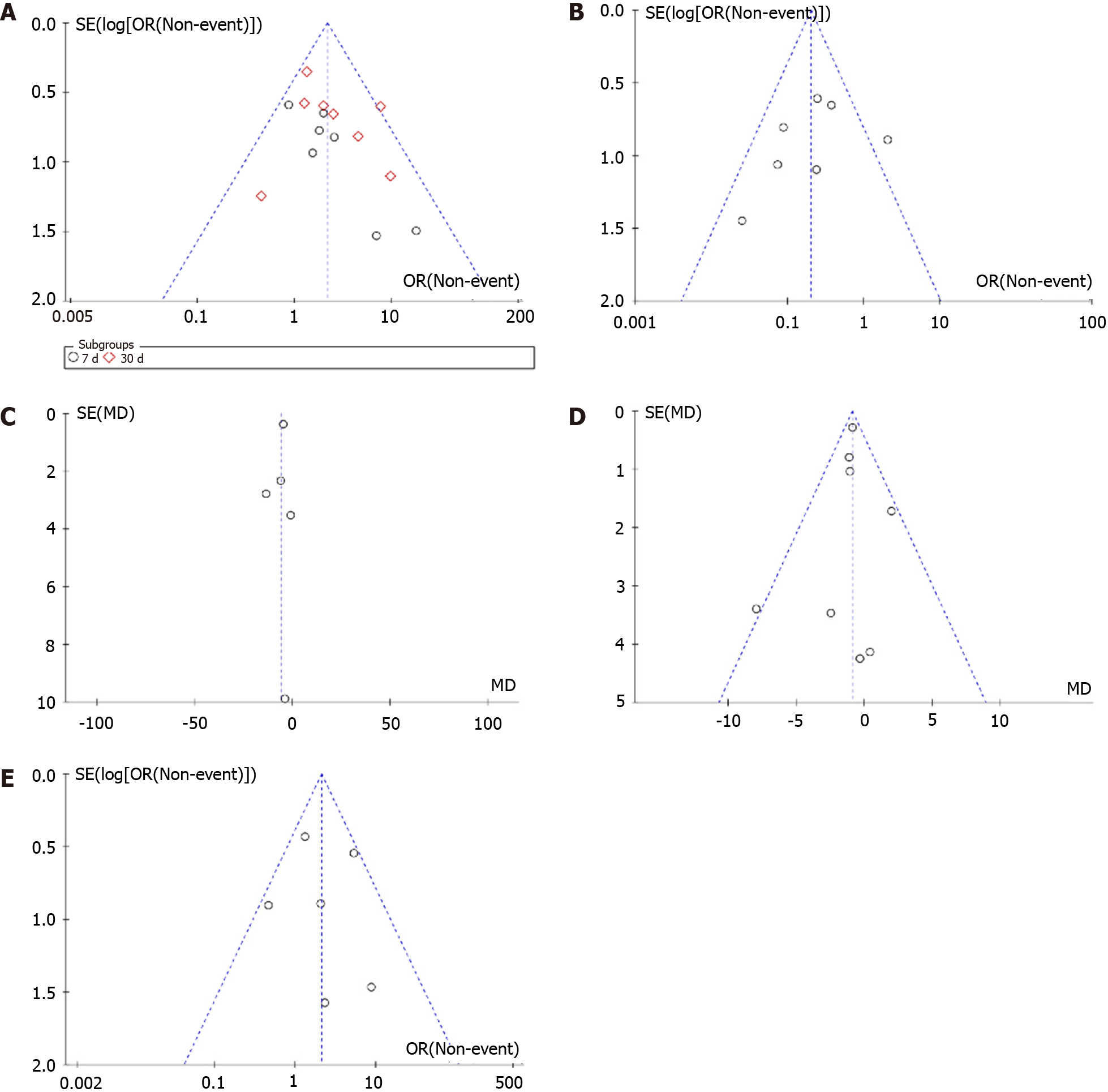
We selected the 5 main indicators for publication bias analysis: recurrent bleeding, hemostatic success, procedure time, length of stay, and mortality. The funnel plots for these indicators were generally symmetrical (Figure 6), indicating no significant publication bias.
To investigate whether OTSC can be the first-line therapy for ANVUGIB, we compared it with standard endoscopic hemostasis protocols through a meta-analysis, including topical spray coagulants, thermal coagulation, and titanium clip hemostasis, thus confirming the effectiveness and safety of OTSC in therapy. We compared two therapy regimens in terms of recurrent bleeding, hemostatic success rate, hospital stay, and safety. We found that OTSC prevented recurrent bleeding better and improved the hemostatic success rate, thus decreasing hospital stay and mortality in patients. In terms of safety, OTSC was useful in minimizing adverse events during treatment.
Recurrent bleeding during ANVUGIB therapy is an important indicator of patient prognosis and can be life-threatening in severe cases. Our analysis of data from 15 groups in 10 studies showed that the incidence of recurrent bleeding at 7 and 30 d was significantly lower in the OTSC group. This was because the hemostatic protocols in standard therapy are aimed at minor or small-vessel bleeding and will not be effective if the ulcer is large or has fibrous tissue proliferation at the base[15,18]. OTSC has a greater ability to clamp more tissue during treatment, thus providing effective compression of the tissue surrounding the ulcer. To achieve the same hemostatic effect often requires the use of multiple titanium clips, which tends to increase the risk of dislodging the hemostatic clip, and thus, cause bleeding from a torn vessel[16]. Furthermore, the OTSC is made of a new nickel-titanium alloy, which has good elasticity and thermal shape memory, facilitating better fit to soft tissue during clamping, and thus, achieving effective clamping. However, one study showed that the recurrent bleeding rate at 7 days after OTSC therapy was higher (15.15% vs 13.51%)[13], which may be related to the shallow placement of the OTSC due to its premature deployment and its misplacement due to poor visualization. Therefore, treatment with OTSC requires a learning curve and clinicians must familiarize with the OTSC system accessory to master hemostasis techniques, especially in emergency situations. Thanks to the better hemostatic effect of OTSC and its preventive effect on recurrent bleeding, the clinical therapy success rate is effectively improved. In total, 6/7 studies showed higher clinical efficiency in the OTSC group.
The time spent on hemostasis can laterally reflect the therapy effect of ANVUGIB and the complexity of the operation. We found that the hemostasis time used for OTSC was significantly lower. It is possible that OTSC can better fit soft tissue and has stronger clamping ability, thus treating bleeding caused by large ulcers with a single clamping, which can effectively avoid the therapy time consumed by placing multiple hemostatic clips and multiple sprays of epinephrine[17]. Through practice, clinicians can master the OTSC system and choose the appropriate diameter of OTSC, to shorten hemostasis time.
Because OTSC is mainly used for the therapy of perforation, fistula closure, and gastrointestinal anastomotic leakage in the early stage and is gradually applied to ANVUGIB therapy, its safety in therapy is a key concern. We evaluated the safety of OTSC mainly in terms of conversion rate to surgery, in-hospital mortality, and complications. The included literature showed that in-hospital mortality and adverse event rates were significantly reduced in the OTSC group, and conversion rate to surgery was not increased, which suggests that the therapeutic effect of OTSC is definite with gua
This meta-analysis has some limitations. First, our more stringent inclusion criteria allowed only 11 publications to be included in the study, which may have resulted in insufficient data on outcome indicators. In addition, we did not evaluate the etiology of NVUGIB and performed subgroup analysis, which can lead to heterogeneity and bias in the results. Moreover, we did not perform subgroup analyses for the doses of PPI drugs used in each paper to exclude the impact of high-dose PPI on recurrent bleeding outcome indicators, which may have biased results. In the future, we will collect literature related to OTSC and present a summary to better guide first-line therapy of ANVUGIB in clinical practice.
In summary, OTSC significantly reduced the rebleeding rate of ANVUGIB with a higher clinical success rate and rela
| 1. | Li Z, Zou D, Ma X, Chen J, Shi X, Gong Y, Man X, Gao L, Zhao Y, Wang R, Yan X, Dent J, Sung JJ, Wernersson B, Johansson S, Liu W, He J. Epidemiology of peptic ulcer disease: endoscopic results of the systematic investigation of gastrointestinal disease in China. Am J Gastroenterol. 2010;105:2570-2577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 100] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 2. | Dong WG, Cheng CS, Liu SP, Yu JP. Epidemiology of peptic ulcer disease in Wuhan area of China from 1997 to 2002. World J Gastroenterol. 2004;10:3377-3379. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 23] [Article Influence: 1.1] [Reference Citation Analysis (2)] |
| 3. | Zheng Y, Xue M, Cai Y, Liao S, Yang H, Wang Z, Wang X, Zhang X, Qian J, Wang L. Hospitalizations for peptic ulcer disease in China: Current features and outcomes. J Gastroenterol Hepatol. 2020;35:2122-2130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 4. | Toka B, Eminler AT, Karacaer C, Uslan MI, Koksal AS, Parlak E. Comparison of monopolar hemostatic forceps with soft coagulation versus hemoclip for peptic ulcer bleeding: a randomized trial (with video). Gastrointest Endosc. 2019;89:792-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Schmidt A, Gölder S, Goetz M, Meining A, Lau J, von Delius S, Escher M, Hoffmann A, Wiest R, Messmann H, Kratt T, Walter B, Bettinger D, Caca K. Over-the-Scope Clips Are More Effective Than Standard Endoscopic Therapy for Patients With Recurrent Bleeding of Peptic Ulcers. Gastroenterology. 2018;155:674-686.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 103] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 6. | Wei JJ, Xie XP, Lian TT, Yang ZY, Pan YF, Lin ZL, Zheng GW, Zhuang ZH. Over-the-scope-clip applications for perforated peptic ulcer. Surg Endosc. 2019;33:4122-4127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Chan S, Pittayanon R, Wang HP, Chen JH, Teoh AY, Kuo YT, Tang RS, Yip HC, Ng SKK, Wong S, Mak JWY, Chan H, Lau L, Lui RN, Wong M, Rerknimitr R, Ng EK, Chiu PWY. Use of over-the-scope clip (OTSC) versus standard therapy for the prevention of rebleeding in large peptic ulcers (size ≥1.5 cm): an open-labelled, multicentre international randomised controlled trial. Gut. 2023;72:638-643. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 8. | Schmidt AR, Glaser N, Kuellmer A, Caca K, Lau J. The Use of the Over the Scope Clip to Treat Upper Gastrointestinal Bleeding. Gastrointest Endosc Clin N Am. 2020;30:1-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Wedi E, von Renteln D, Gonzalez S, Tkachenko O, Jung C, Orkut S, Roth V, Tumay S, Hochberger J. Use of the over-the-scope-clip (OTSC) in non-variceal upper gastrointestinal bleeding in patients with severe cardiovascular comorbidities: a retrospective study. Endosc Int Open. 2017;5:E875-E882. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 10. | Ishak C, Ghazanfar H, Kandhi S, Alemam A, Abbas H, Patel H, Chilimuri S. Role of Transcatheter Arterial Embolization in Acute Refractory Non-variceal Upper Gastrointestinal Bleeding Not Controlled by Endoscopy: A Single-Center Experience and a Literature Review. Cureus. 2022;14:e29962. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Jensen DM, Kovacs T, Ghassemi KA, Kaneshiro M, Gornbein J. Randomized Controlled Trial of Over-the-Scope Clip as Initial Treatment of Severe Nonvariceal Upper Gastrointestinal Bleeding. Clin Gastroenterol Hepatol. 2021;19:2315-2323.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 12. | Robles-Medranda C, Oleas R, Alcívar-Vásquez J, Puga-Tejada M, Baquerizo-Burgos J, Pitanga-Lukashok H. Over-The-Scope Clip system as a first-line therapy for high-risk bleeding peptic ulcers: a retrospective study. Surg Endosc. 2021;35:2198-2205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Kuellmer A, Mangold T, Bettinger D, Schiemer M, Mueller J, Wannhoff A, Caca K, Wedi E, Kleemann T, Thimme R, Schmidt A. Reduced mortality for over-the-scope clips (OTSC) versus surgery for refractory peptic ulcer bleeding: a retrospective study. Surg Endosc. 2023;37:1854-1862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 14. | Mangiafico S, Pigò F, Bertani H, Caruso A, Grande G, Sgamato C, Manta R, Conigliaro R. Over-the-scope clip vs epinephrine with clip for first-line hemostasis in non-variceal upper gastrointestinal bleeding: a propensity score match analysis. Endosc Int Open. 2020;8:E50-E58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Buddam A, Rao S, Koppala J, Rangray R, Abdussalam A, Mukherjee S, Chandra S. Over-the-scope clip as first-line therapy for ulcers with high-risk bleeding stigmata is efficient compared to standard endoscopic therapy. Endosc Int Open. 2021;9:E1530-E1535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Qiu J, Xu J, Zhang Y, Liao F, Zhu Z, Shu X, Chen Y, Pan X. Over-the-Scope Clip Applications as First-Line Therapy in the Treatment of Upper Non-variceal Gastrointestinal Bleeding, Perforations, and Fistulas. Front Med (Lausanne). 2022;9:753956. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Meier B, Wannhoff A, Denzer U, Stathopoulos P, Schumacher B, Albers D, Hoffmeister A, Feisthammel J, Walter B, Meining A, Wedi E, Zachäus M, Pickartz T, Küllmer A, Schmidt A, Caca K. Over-the-scope-clips versus standard treatment in high-risk patients with acute non-variceal upper gastrointestinal bleeding: a randomised controlled trial (STING-2). Gut. 2022;71:1251-1258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 36] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 18. | Song JS, Kwak HS, Chung GH. Nonvariceal upper gastrointestinal bleeding: the usefulness of rotational angiography after endoscopic marking with a metallic clip. Korean J Radiol. 2011;12:473-480. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Lu Y, Loffroy R, Lau JY, Barkun A. Multidisciplinary management strategies for acute non-variceal upper gastrointestinal bleeding. Br J Surg. 2014;101:e34-e50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |