Published online Jul 16, 2024. doi: 10.12998/wjcc.v12.i20.4217
Revised: May 10, 2024
Accepted: May 23, 2024
Published online: July 16, 2024
Processing time: 103 Days and 5.5 Hours
Pulmonary hypertension is a serious complication in the treatment of mainte
To investigate the intervention and control of pedal-powered bicycle in main
73 patients with maintenance hemadialysis combined with pulmonary arterial hypertension at a hemodialysis center in a certain hospital from May 2021 to May 2022 are selected. Patients are divided into two groups, 37 cases in the control group (group C) and 36 cases in the intervention group (group I). Patients are divided into two groups, group C is treated with oral administration of betaglan
After treatment, group I patients had higher muscle strength, 36-Item Short Form Health Survey scores, and Kidney Disease Targets Areas scores; The 6-minute walk distance test index level was higher and the Borg score was lower; The group I had lower systolic blood pressure, greater vital capacity, higher positive emotion, lower systolic pulmonary artery pressure index level, higher arterial partial oxygen pressure level, lower pulmonary vascular resistance index level, and higher blood oxygen saturation level [158.91 ± 11.89 vs 152.56 ± 12.81, 1795.01 ± 603.18 vs 1907.20 ± 574.15, 24.00 (22.00, 29.00) vs 24.00 (22.00, 28.00), P < 0.001].
Aerobic exercise combined with Western medicine treatment can effectively improve patients' pulmonary hypertension, alleviate their negative emotions, and enable them to achieve a higher level of quality of life.
Core Tip: This study investigates the effects of aerobic exercise, on the quality of life and pulmonary arterial hypertension (PAH) in patients undergoing hemodialysis. Employing a control design, the research divides patients into a control group receiving standard care and an intervention group undertaking power cycling in addition to standard care. The results demonstrate significant improvements in the intervention group, including enhanced muscle strength, better quality of life scores, reduced systolic blood pressure, and improved pulmonary function indicators. Incorporating aerobic exercise into the care regimen of hemodialysis patients with PAH can significantly improve their health outcomes and quality of life.
- Citation: Wang DD, Cheng M, Chen CY. Intervention control of aerobic exercise in maintaining quality of life and pulmonary hypertension in hemodialysis patients. World J Clin Cases 2024; 12(20): 4217-4229
- URL: https://www.wjgnet.com/2307-8960/full/v12/i20/4217.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i20.4217
The incidence rate of chronic kidney disease (CKD) in the world is increasing year by year, and its incidence rate in adults is 13.7%-17.3%. In China, the incidence rate of CKD is 10.8%. Due to the high incidence rate of CKD and irreversible course of disease development, the number of patients with end stage of renal disease (ESRD) is increasing year by year, and the number of patients is relatively large[1,2]. In China, the majority of ESRD patients undergo hemadialysis (HD) treatment, and under long-term treatment, their physical and mental health will be affected to varying degrees. They are prone to sleep disorder, which can lead to fatigue, anxiety, panic and other negative emotions. These emotions can be detrimental to the patient's treatment and seriously affect their quality of life. Moreover, compared to the general population, the incidence rate of pulmonary arterial hypertension (PAH) in maintenance HD (MHD) patients is higher. Among its main characteristics, pulmonary arteriole will have vasospasm, and intima will proliferate and reconstruct. Patients with PAH may experience progressive breathing difficulties, symptoms such as dizziness and chest pain, and their emotions may also be affected[3-5]. The current pathogenesis of this disease is not yet clear, and the treatment effect is poor, with poor prognosis and a high mortality rate. Therefore, to help MHD-PAH patients receive better treatment, auxiliary measures are used to alleviate their emotions and improve their symptoms. Research has shown that exercise therapy can help alleviate the physical and mental discomfort of HD patients and improve their quality of life[6,7]. Moreover, this therapy can also improve the endothelium-dependent vasodilation function and inhibit the formation of PAH under hypoxia. Considering the physical condition of patients with MHD and PAH, as well as the limitations of the venue, strength cycling exercise is chosen in aerobic exercise. It is easy to practice, relatively safe, and has good effects in improving patients' sleep quality, alleviating anxiety, and promoting blood flow[8,9]. In this regard, this paper applies power cycling exercise to the treatment of patients with MHD combined with PAH, with the aim of improving their quality of life and PAH.
From May 2021 to May 2022, 73 patients with MHD combined with PAH were selected as the study subjects at the HD center of a certain hospital. The patients were divided into a control group (group C) with 37 cases and an intervention group (group I) with 36 cases. This study has received the consent of the Medical Ethics Committee and the informed consent of the relevant patients and their families.
Inclusive: (1) Age ranges from 23 to 67 years old; (2) Meet the judgment criteria of the World Health Organization and the Chinese Medical Association for MHD merging with PAH; (3) The patient has a complete understanding of the research plan and is able to actively cooperate; (4) Patients are able to communicate without barriers; (5) After dialysis, the patient's weight meets the standard requirements; (6) The glomerular filtration rate is less than 15 mL/ (min × 1.73 m2); and (7) The patient has no severe anemia and hemoglobin is greater than or equal to 80 g/L.
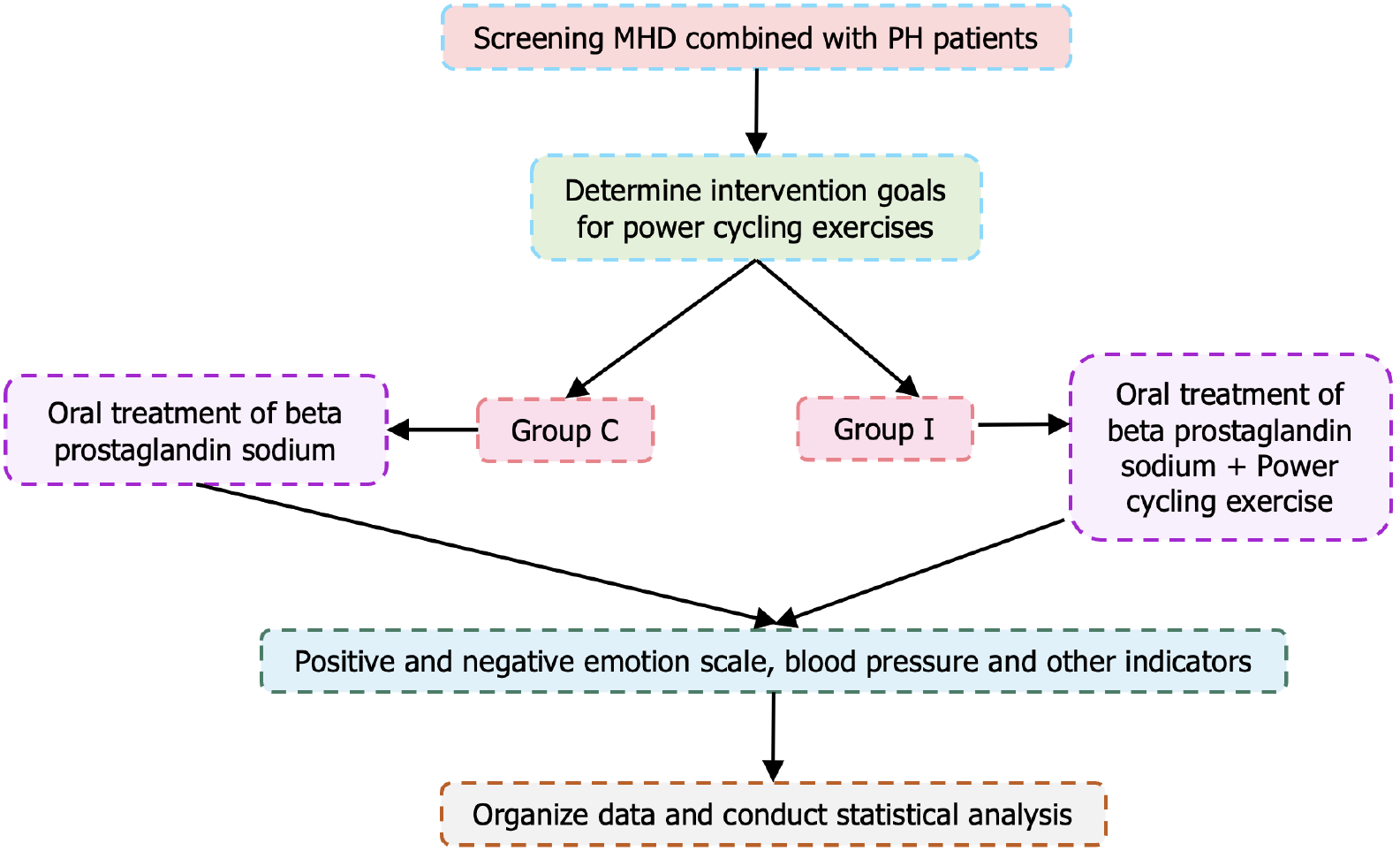
Exclusive: (1) Under 23 years old or over 67 years old; (2) Dialysis time is less than 3 months; (3) Patients who also suffer from heart disease and other diseases; (4) The patient is at risk of rheumatic or malignant tumors; (5) Having stubborn hypertension; (6) Acute kidney failure; (7) The presence of severe glaucoma; and (8) Not participating in the research process. Figure 1 shows the relevant research ideas.
In Figure 1, the first step is to preliminarily screen patients with MHD combined with PAH and obtain patients who meet the diagnostic requirements. According to the inclusion and exclusion criteria, MHD-PAH patients are further screened to obtain intervention targets for Laughter Yoga. According to the results in group C and group I, the group C patients receive routine treatment, while group I receives power cycling exercise on the basis of routine treatment. The correlation between the two groups of patients is tested using positive and negative emotion scales, blood pressure, and other indicators. The obtained results are organized and statistically analyzed.
Both group C and group I receive oral treatment with betaglandin sodium. On the basis of routine treatment, group I adopts power cycling exercise as the treatment plan. During the intervention period, it lasts for a total of 12 weeks, and the patient also undergoes power cycling exercise while undergoing dialysis. Under the guidance and guidance of professionals, appropriate strength circulation exercises should be carried out according to the patient's condition. Each practice lasts for 30 min and cannot be completed at once. Take a break midway, continue to accumulate time, and record the duration of the first and last runs. During the power cycling exercise, the patient's relevant data are recorded. In addition, during the practice period, patients with excellent performance can be given appropriate rewards to maintain their enthusiasm for practice and enable them to continue exercising every day.
After the patient has rested for 5 min, the patient's blood pressure are measured with a standard desk mercury sphygmomanometer for 3 times at an interval of 2 min. The average of the 3 measurements are taken to obtain systolic and diastolic blood pressure. The domestically produced WCS-100II electronic grip strength meter is selected to measure the arm strength on the non arteriovenous fistula side of the patient. The number of measurements is 3, with an interval of 15 s between each measurement. The value with the highest measurement value is selected as the measurement result of muscle strength. The patient's vital capacity is measured through the relevant vital capacity measuring instrument. When measuring, the patient needs to be in a quiet state, with 3 measurements taken and the average of the measurement results taken. The Positive and Negative Affect Scale is selected to measure the patient's emotions. The scale is segmented into two dimensions: positive and negative emotions. The number of entries in one dimension is 10, and a Likert 5-level score is used. The higher the score, the stronger the positive or negative emotions of the patient[10]. The Kidney Disease Quality of Life Short Forms is selected, which includes two scales: the MOS 36-Item Short Form Health Survey (SF-36) and the Kidney Disease Targets Areas (KDTA). Through these scales, the patient's health status, quality of life, and other factors are evaluated, including a total of 20 dimensions. Each dimension is scored using a percentage system, with a high score indicating a high quality of life for the individual; On the contrary, it is low[11,12]. Pulmonary vascular resistance (PVR), blood oxygen saturation (SaO2) and arterial partial oxygen pressure level (PaO2) of femoral artery are measured. The patient's breathing condition is evaluated using the Borg dyspnea score. The higher the score, the more difficult the patient's breathing is. The patient's motor function is evaluated and analyzed through the 6-minute walk distance test (6MWD)[13,14].
The data was analyzed using SPSS23.0 software. When P < 0.05, it indicates statistical significance. Researchers and another person alternated and mutually reviewed the input experimental results. The experimental results were described in the form of mean, sample rate, standard deviation, etc. Relevant statistical processing involved processing and analyzing relevant data through χ2-tests, t-tests, and other forms.
The experiment organizes relevant data of patients with group C and group I. There are 37 cases in group C and 36 cases in group I. Comparing these two groups, there is no statistically significant difference in gender, age, work status, per capita monthly household income, primary cause, dialysis time, and dialysis frequency (P > 0.05). Before treatment, the general information of group C and group I is shown in Table 1.
| Characteristic | Group I (n = 36) | Group C (n = 37) | P value |
| Gender | - | - | 0.859 |
| Male | 10 (27.78) | 11 (29.73) | - |
| Female | 26 (72.22) | 26 (70.27) | - |
| Age (yr) | 48.76 ± 9.05 | 47.84 ± 9.02 | 0.608 |
| Work situation | - | - | 0.675 |
| Be on the job | 3 (8.33) | 2 (5.41) | - |
| Depart | 4 (11.11) | 2 (5.41) | - |
| Retire | 6 (16.67) | 5 (13.51) | - |
| Farmer | 21 (58.33) | 24 (64.86) | - |
| Other | 2 (5.56) | 4 (10.81) | - |
| Per capita monthly income of households | - | - | 0.874 |
| < 1000 | 15 (41.67) | 18 (48.65) | - |
| 1001-2000 | 8 (22.22) | 10 (27.03) | - |
| 2001-3000 | 8 (22.22) | 3 (8.11) | - |
| > 3000 | 5 (5.56) | 6 (16.22) | - |
| Primary etiology | - | - | 0.963 |
| Nepahritis | 21 (56.76) | 19 (51.35) | - |
| Diabetes | 1 (2.70) | 2 (5.41) | - |
| Hypertensive nepahropathy | 8 (21.62) | 9 (24.32) | - |
| Other | 6 (16.22) | 9 (24.32) | - |
| Dialysis time (yr) | - | - | 0.481 |
| < 2 | 11 (30.56) | 14 (37.84) | - |
| 2-5 | 17 (47.22) | 13 (35.14) | - |
| > 5 | 8 (22.22) | 10 (27.03) | - |
| Dialysis frequency | - | - | 0.624 |
| Twice a week | 16 (44.44) | 14 (37.84) | - |
| 3 times a week | 10 (27.78) | 9 (24.32) | - |
| 5 times per 2 weeks | 8 (22.22) | 13 (35.14) | - |
| Other | 2 (5.56) | 1 (2.70) | - |
Table 2 shows the relevant physiological indicators of patients with group C and group I. Before treatment, there are differences in systolic blood pressure, muscle strength, and other indicators between group C and group I patients (P > 0.05). After treatment, group I patients have greater muscle strength (P < 0.05), lower systolic blood pressure, and greater vital capacity (P < 0.001) than group C. After treatment, the diastolic pressure, muscle strength and vital capacity of patients in group N are P > 0.05, and the systolic pressure is lower (P < 0.05). After treatment, group I has lower diastolic blood pressure, greater muscle strength (P < 0.05), lower systolic blood pressure (P < 0.01), and greater vital capacity (P < 0.001).
| Project | Group | Before treatment | After treatment | P value |
| Systolic pressure | Group I | 155.21 ± 10.45 | 147.95 ± 10.10 | 0.004 |
| Group C | 158.91 ± 11.89 | 152.56 ± 12.81 | 0.030 | |
| t | -1.423 | -3.545 | - | |
| P value | 0.160 | 0.001 | - | |
| Diastolic pressure | Group I | 86.30 ± 13.15 | 80.83 ± 8.33 | 0.039 |
| Group C | 86.78 ± 13.09 | 85.39 ± 10.88 | 0.621 | |
| t | -0.175 | -1.953 | - | |
| P value | 0.864 | 0.065 | - | |
| Myodynamia | Group I | 24.17 ± 6.53 | 28.41 ± 7.51 | 0.013 |
| Group C | 24.68 ± 9.19 | 25.50 ± 7.80 | 0.680 | |
| t | -0.281 | 1.623 | - | |
| P value | 0.780 | 0.033 | - | |
| Vital capacity | Group I | 1801.01 ± 568.86 | 2341.83 ± 569.82 | < 0.001 |
| Group C | 1795.01 ± 603.18 | 1907.20 ± 574.15 | 0.405 | |
| t | 0.045 | 4.210 | - | |
| P value | 0.967 | 0.000 | - |
Table 3 shows the positive emotional scores of group C and group I after treatment. After treatment, group I patients performs better in strong willed, inspired, and energetic emotions (P < 0.05), better in energetic, proud, enthusiastic, and energetic emotions (P < 0.01), and higher in positive emotions (P < 0.001); However, there is no difference in positive emotions among group C patients (P > 0.05). After treatment, group I performs better in strong willed emotions (P < 0.05), better in interested and encouraged emotions (P < 0.01). Overall, group I has higher positive emotions (P < 0.001).
| Project | Group | Before treatment | After treatment | P value |
| Interested | Group I | 3.00 (2.00, 3.00) | 3.00 (2.00, 4.00) | 0.077 |
| Group C | 2.00 (2.00, 3.00) | 2.00 (2.00, 3.00) | 0.986 | |
| Z | -0.828 | -2.972 | ||
| P value | 0.407 | 0.003 | ||
| Energetic | Group I | 3.00 (2.00, 3.00) | 3.00 (3.00, 4.00) | 0.003 |
| Group C | 2.00 (2.00, 3.00) | 2.00 (2.00, 3.00) | 0.633 | |
| Z | -1.160 | -4.868 | ||
| P value | 0.246 | 0.000 | ||
| Determined | Group I | 3.00 (2.25, 4.00) | 4.00 (3.00, 4.00) | 0.028 |
| Group C | 3.00 (2.00, 4.00) | 3.00 (2.00, 4.00) | 0.930 | |
| Z | -0.174 | -2.206 | ||
| P value | 0.862 | 0.027 | ||
| Highly alert | Group I | 3.00 (2.00, 3.00) | 3.00 (3.00, 3.75) | 0.019 |
| Group C | 2.00 (2.00, 3.00) | 3.00 (2.00, 3.00) | 0.718 | |
| Z | -0.251 | -1.961 | ||
| P value | 0.802 | 0.050 | ||
| Proud | Group I | 2.00 (1.00, 3.00) | 3.00 (2.00, 4.00) | 0.003 |
| Group C | 2.00 (1.00, 3.00) | 2.00 (1.00, 2.50) | 0.999 | |
| Z | -0.442 | -3.614 | ||
| P value | 0.659 | < 0.001 | ||
| Focused | Group I | 3.00 (2.00, 3.00) | 3.00 (3.00, 3.00) | 0.300 |
| Group C | 3.00 (2.00, 3.00) | 3.00 (2.00, 3.00) | 0.987 | |
| Z | -0.322 | -1.090 | ||
| P value | 0.747 | 0.276 | ||
| Encouraged | Group I | 3.00 (2.00, 3.00) | 2.00 (2.00, 3.00) | 0.031 |
| Group C | 2.00 (2.00, 3.00) | 2.00 (2.00, 3.00) | 0.610 | |
| Z | -1.080 | -3.037 | ||
| P value | 0.280 | 0.002 | ||
| Passionate | Group I | 3.00 (3.00, 4.00) | 4.00 (3.00, 4.00) | 0.009 |
| Group C | 3.00 (2.00, 4.00) | 3.00 (2.00, 4.00) | 0.926 | |
| Z | -1.532 | -3.825 | ||
| P value | 0.125 | < 0.001 | ||
| Highly energetic | Group I | 3.00 (2.00, 3.00) | 3.00 (3.00, 4.00) | 0.026 |
| Group C | 2.00 (2.00, 3.00) | 2.00 (2.00, 3.00) | 0.867 | |
| Z | -1.141 | -3.699 | ||
| P value | 0.254 | < 0.001 | ||
| Energetic | Group I | 3.00 (2.00, 3.00) | 3.00 (3.00, 4.00) | 0.004 |
| Group C | 2.00 (2.00, 3.00) | 2.00 (2.00, 3.00) | 0.831 | |
| Z | -0.606 | -3.817 | ||
| P value | 0.544 | < 0.001 | ||
| Positive emotions | Group I | 26.00 (24.00, 31.00) | 32.50 (29.25, 35.75) | < 0.001 |
| Group C | 24.00 (22.00, 29.00) | 24.00 (22.00, 28.00) | 0.987 | |
| Z | -1.350 | -5.218 | ||
| P value | 0.177 | < 0.001 |
Table 4 shows the negative emotional scores of group C and group I after treatment. After treatment, group I shows significant improvement in irritable, guilty, irritable, and fearful emotions (P < 0.05), while it shows significant improvement in tense emotions (P < 0.01). Overall, the negative emotions of group I improves significantly (P < 0.05). Compared to before treatment, there are no significant change in negative emotions in group C patients after treatment (P > 0.05).
| Project | Before treatment | After treatment | ||
| Group I | Group C | Group I | Group C | |
| Upset | 2.00 (2.00, 3.00) | 3.00 (2.00, 4.00) | 2.00 (2.00, 3.00) | 3.00 (2.00, 3.00) |
| P value | 0.272 | 0.023 | ||
| Hung up | 2.00 (2.00, 3.00) | 2.00 (2.00, 4.00) | 2.00 (2.00, 3.00) | 2.00 (2.00, 3.00) |
| P value | 0.552 | 0.231 | ||
| Guilty | 2.00 (2.00, 3.00) | 2.00 (2.00, 4.00) | 2.00 (1.25, 3.00) | 3.00 (2.00, 4.00) |
| P value | 0.890 | 0.047 | ||
| Fearful | 2.00 (1.25, 3.00) | 2.00 (1.00, 3.00) | 2.00 (1.00, 2.00) | 2.00 (1.00, 2.50) |
| P value | 0.652 | 0.279 | ||
| Hostile | 2.00 (1.00, 2.00) | 2.00 (1.00, 2.00) | 1.50 (1.00, 2.00) | 2.00 (1.00, 2.00) |
| P value | 0.456 | 0.782 | ||
| Irritable | 3.00 (2.00, 4.00) | 2.00 (2.00, 3.50) | 2.00 (2.00, 2.00) | 2.00 (2.00, 3.00) |
| P value | 0.372 | 0.035 | ||
| Shy | 3.00 (2.00, 3.00) | 2.00 (2.00, 3.00) | 2.00 (1.00, 2.75) | 2.00 (1.50, 3.00) |
| P value | 0.402 | 0.206 | ||
| Nervous | 2.00 (2.00, 4.00) | 2.00 (2.00, 4.00) | 2.00 (1.00, 3.00) | 3.00 (2.00, 4.00) |
| P value | 0.926 | 0.001 | ||
| Restless | 2.00 (2.00, 3.00) | 2.00 (2.00, 3.00) | 2.00 (1.00, 3.00) | 2.00 (1.50, 3.00) |
| P value | 0.991 | 0.884 | ||
| Fearful | 2.00 (2.00, 3.00) | 2.00 (1.50, 3.00) | 2.00 (1.00, 2.00) | 2.00 (1.50, 3.00) |
| P value | 0.768 | 0.019 | ||
| Negative emotions | 25.00 (19.25, 28.00) | 22.00 (18.50, 31.50) | 20.50 (16.00, 24.00) | 24.00 (19.00, 27.50) |
| P value | 0.770 | 0.028 | ||
Table 5 shows the SF-36 scores of group I and group C. In the pre-treatment, compared to group C, group I shows significant improvement in general health status (P < 0.05), as well as significant improvement in energy and mental health (P < 0.01). Overall, group I has a higher SF-36 score (P < 0.05). Compared to the pre-treatment, there are no significant change in negative emotions in group C patients after treatment (P > 0.05). Compared to before treatment, group I shows significant improvement in physiological function (P < 0.001); The physiological function of group C has significantly improved (P < 0.05).
| Project | Before treatment | After treatment | ||
| Group I | Group C | Group I | Group C | |
| General health status | 30.72 ± 24.91 | 28.50 ± 20.79 | 47.63 ± 22.37 | 34.21 ± 21.80 |
| P value | 0.691 | 0.011 | ||
| Pahysiology | 76.15 ± 13.97 | 72.43 ± 14.95 | 81.94 ± 9.65 | 79.77 ± 13.79 |
| P value | 0.279 | 0.068 | ||
| Pahysiological functions | 25.01 ± 36.83 | 23.64 ± 33.29 | 57.40 ± 37.92 | 33.07 ± 33.86* |
| P value | 0.868 | 0.005 | ||
| Body pain | 66.38 ± 22.63 | 62.98 ± 22.18 | 68.33 ± 19.21 | 67.57 ± 20.55 |
| P value | 0.518 | 0.868 | ||
| Emotional function | 35.23 ± 41.35 | 36.94 ± 39.89 | 62.96 ± 41.23 | 47.75 ± 38.12 |
| P value | 0.854 | 0.103 | ||
| Social function | 68.04 ± 23.06 | 60.75 ± 23.90 | 73.25 ± 20.97 | 64.88 ± 23.73 |
| P value | 0.189 | 0.115 | ||
| Energy | 51.53 ± 18.16 | 49.46 ± 24.46 | 64.18 ± 15.83 | 50.16 ± 17.41 |
| P value | 0.684 | 0.001 | ||
| Mental health | 67.18 ± 18.57 | 64.97 ± 16.80 | 76.11 ± 10.50 | 66.49 ± 14.98 |
| P value | 0.600 | 0.002 | ||
| Total score | 55.36 ± 15.48 | 52.66 ± 15.39 | 67.85 ± 13.02 | 57.53 ± 13.30 |
| P value | 0.460 | 0.001 | ||
In Table 6, in the time effect analysis, the P-values of SF-36 score, general health status, physiological function, etc. are all less than 0.05, indicating that the quality of life of MHD patients with PAH is affected by time. In the inter-group effect, the P-values of physiological function, social function, energy, mental health, and SF-36 scores are all less than 0.05, indicating that different intervention methods lead to differences in the quality of life between the two groups. Similarly, there is an interaction between the two groups of patients in terms of mental dimensions (P < 0.05).
| Project | Time effect | Intergroup effect | Interaction | |||
| F | P value | F | P value | F | P value | |
| General health status | 16.758 | < 0.001 | 3.613 | 0.058 | 2.958 | 0.065 |
| Pahysiology | 9.015 | < 0.001 | 2.678 | 0.108 | 0.171 | 0.814 |
| Pahysiological functions | 11.446 | < 0.001 | 4.231 | 0.041 | 3.143 | 0.051 |
| Pahysical pain | 3.196 | 0.045 | 0.429 | 0.516 | 0.168 | 0.842 |
| Emotional function | 8.673 | 0.001 | 0.765 | 0.387 | 1.512 | 0.226 |
| Social function | 2.770 | 0.076 | 4.688 | 0.032 | 0.325 | 0.695 |
| Energy | 7.597 | 0.003 | 5.329 | 0.026 | 4.574 | 0.019 |
| Mental health | 5.235 | 0.008 | 5.121 | 0.028 | 2.509 | 0.090 |
| Total score | 24.485 | < 0.001 | 5.869 | 0.021 | 4.028 | 0.029 |
In Table 7, after treatment, group I shows significant improvement in the burden of kidney disease on daily life, overall health assessment, and social support (P < 0.05), with better patient satisfaction and encouragement from medical staff (P < 0.01). Overall, group I has a higher KDTA score (P < 0.05). Compared to before treatment, there is no significant change in negative emotions in group C patients after treatment (P > 0.05); The group I shows significant improvement in the impact of kidney disease on daily life and overall health assessment (P < 0.05), while its other aspects are consistent with the former (P < 0.01); The overall health assessment of group C shows significant improvement (P < 0.05).
| Project | Before treatment | After treatment | ||
| Group I | Group C | Group I | Group C | |
| Cognitive | 69.79 ± 17.88 | 69.99 ± 22.27 | 71.15 ± 16.16 | 68.15 ± 20.98 |
| P value | 0.972 | 0.496 | ||
| Symptoms and discomforts | 67.36 ± 15.92 | 65.10 ± 19.43 | 72.86 ± 13.98 | 71.28 ± 13.92 |
| P value | 0.589 | 0.631 | ||
| The burden of kidney disease on life | 26.56 ± 22.82 | 24.66 ± 14.06 | 36.81 ± 23.94 | 24.49 ± 24.49 |
| P value | 0.671 | 0.013 | ||
| Social quality | 72.86 ± 16.61 | 71.70 ± 18.23 | 77.79 ± 12.56 | 71.68 ± 14.42 |
| P value | 0.781 | 0.058 | ||
| The impact of kidney disease on daily life | 48.10 ± 15.94 | 47.65 ± 15.47 | 56.69 ± 14.21 | 50.01 ± 17.57 |
| P value | 0.902 | 0.079 | ||
| Sexuality | 17.34 ± 29.75 | 18.23 ± 34.68 | 20.83 ± 29.43 | 18.24 ± 32.09 |
| P value | 0.908 | 0.721 | ||
| Sleep | 56.39 ± 18.08 | 55.47 ± 14.43 | 60.97 ± 13.70 | 58.24 ± 16.92 |
| P value | 0.811 | 0.452 | ||
| Social support | 66.20 ± 16.68 | 65.76 ± 11.76 | 73.60 ± 17.55 | 65.32 ± 12.66 |
| P value | 0.898 | 0.024 | ||
| Work situation | 26.51 ± 27.89 | 28.37 ± 25.10 | 33.34 ± 29.29 | 32.42 ± 24.19 |
| P value | 0.763 | 0.886 | ||
| Overall health assessment | 49.44 ± 18.18 | 46.49 ± 13.39 | 59.57 ± 15.00 | 53.02 ± 11.93 |
| P value | 0.430 | 0.042 | ||
| Patient satisfaction | 56.48 ± 17.52 | 57.18 ± 19.47 | 67.57 ± 17.75 | 54.01 ± 15.48 |
| P value | 0.866 | 0.001 | ||
| Encouragement from medical staff | 78.83 ± 16.05 | 78.37 ± 19.25 | 90.97 ± 15.98 | 78.72 ± 15.54 |
| P value | 0.916 | 0.001 | ||
| Total score | 55.43 ± 10.66 | 54.42 ± 10.26 | 61.96 ± 9.35 | 56.39 ± 8.91 |
| P value | 0.675 | 0.011 | ||
In Table 8, in the time effect analysis, the scores of KDTA, symptoms and discomfort, and the impact of kidney disease on daily life are found to be P < 0.05, indicating that the quality of life of MHD-PAH patients is influenced by time. In the inter-group effect, the burden of kidney disease on life, overall health assessment, patient satisfaction, encouragement from medical staff, and KDTA scores are all P < 0.05. This indicates different intervention methods led to differences in the quality of life between the two groups. Therefore, there is an interaction between the social support and patient satisfaction of the two groups of patients (P < 0.05).
| Project | Time effect | Intergroup effect | Interaction | |||
| F | P value | F | P value | F | P value | |
| The burden of kidney disease on life | 2.316 | 0.115 | 4.237 | 0.044 | 2.289 | 0.116 |
| Cognitive function | 0.343 | 0.686 | 0.218 | 0.645 | 0.502 | 0.585 |
| Social quality | 2.587 | 0.094 | 2.587 | 0.113 | 2.406 | 0.109 |
| Symptoms and discomforts | 10.124 | < 0.001 | 0.718 | 0.404 | 0.246 | 0.782 |
| The impact of kidney disease on daily life | 7.375 | 0.003 | 1.993 | 0.163 | 2.902 | 0.068 |
| Sexual function | 0.813 | 0.418 | 0.025 | 0.877 | 0.143 | 0.807 |
| Sleep | 2.587 | 0.083 | 0.197 | 0.658 | 0.320 | 0.706 |
| Social support | 7.588 | 0.002 | 1.558 | 0.215 | 9.658 | < 0.001 |
| Working conditions | 6.746 | 0.003 | 0.190 | 0.664 | 1.266 | 0.284 |
| Overall health assessment | 3.907 | 0.021 | 6.796 | 0.012 | 3.655 | 0.029 |
| Patient satisfaction | 2.531 | 0.083 | 4.214 | 0.045 | 7.403 | 0.001 |
| Encouragement from medical staff | 6.479 | 0.006 | 4.563 | 0.035 | 6.025 | 0.007 |
| Total score | 14.865 | < 0.001 | 3.995 | 0.048 | 3.860 | 0.029 |
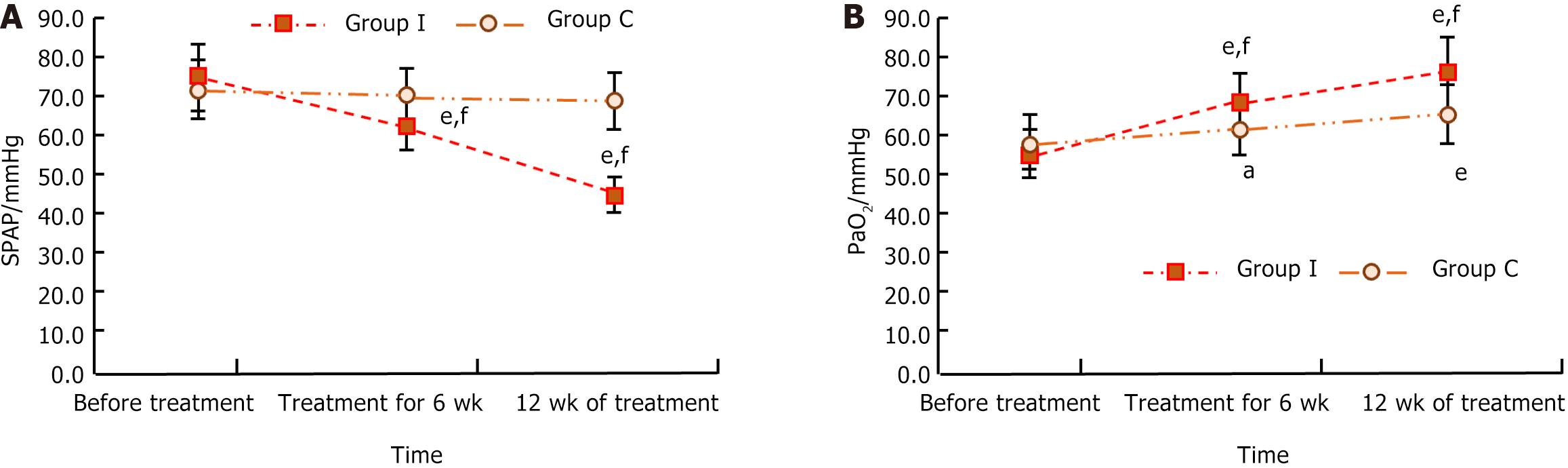
In Figure 2, after 6 wk of treatment, the systolic pulmonary artery pressure (SPAP) index level of group I is lower (P < 0.001) and the PaO2 level is higher (P < 0.01); The PaO2 level of group C is higher (P < 0.05). After 12 wk of treatment, the SPAP index levels of group I are lower (P < 0.001), and the PaO2 levels of both group I and group C are higher (P < 0.001).
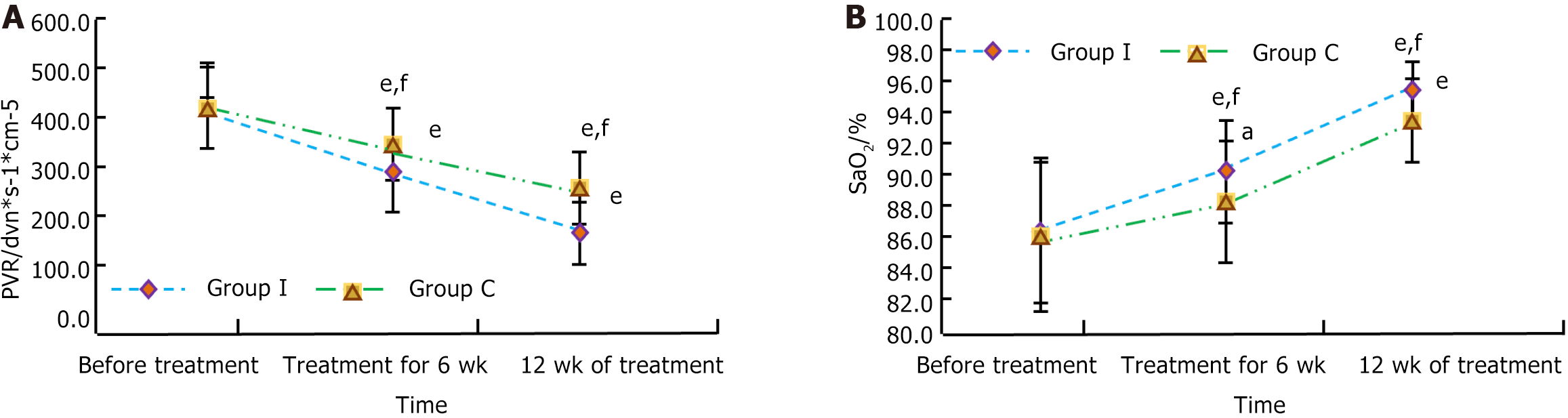
In Figure 3, after 6 wk of treatment, compared with group C, the level of group I’s PVR index is lower (P < 0.001) and its PaO2 level is higher (P < 0.05). After 12 wk of treatment, compared with group C, the group I’s PVR index level is lower and the SaO2 level is higher (P < 0.001). Compared to before treatment and after 6 wk of treatment, the group C’s PVR index level is lower (P < 0.001) and the SaO2 index level is higher (P < 0.05); After 12 wk of treatment, the group C PVR index level is lower and the SaO2 index level is higher (P < 0.001). Compared to before treatment, after 4 and 12 wk of treatment, the group I’s PVR index level is lower and the SaO2 index level is higher (P < 0.001).
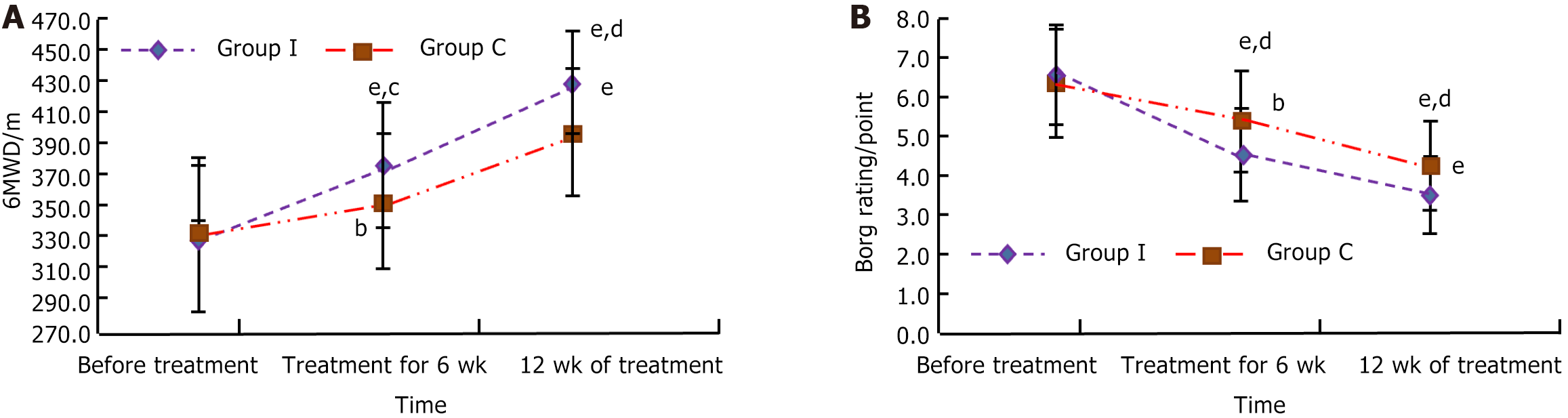
In Figure 4, after 6 wk of treatment, compared with group C, group I has a lower Borg score (P < 0.01) and a higher 6MWD indicator level (P < 0.05). After 12 wk of treatment, the 6MWD index level of group I is higher and the Borg score is lower (P < 0.01). Compared to before treatment and after 6 wk of treatment, the Borg score of group C is lower (P < 0.01); After 12 wk of treatment, the 6MWD index level of group C is higher and the Borg score is lower (P < 0.001). Compared to before treatment, after 12 wk of treatment, the 6MWD index level of group I is higher and the Borg score is lower (P < 0.001).
PAH is the most serious complication in the treatment of MHD patients, as they often experience metastatic calcification. This calcification will harden the patient's pulmonary capillaries, thus making the Pulmonary circulation more resistant, thus causing PAH[15-17]. Targeted interventions based on vasospasm and other conditions in PAH can delay the progression of PAH. Beprost sodium is a new type of anti-PAH drug, which can reduce pulmonary artery pressure and reduce heart load by inhibiting the proliferation of vascular smooth muscle cells and platelet aggregation, and relaxing smooth muscle. It is an ideal anti-pulmonary hypertension drug[18,19]. Some scholars, to effectively intervene in patients with autoimmune hemolytic anemia who contain PAH, choose drugs such as beta prostaglandin sodium for treatment. From the perspective of treatment effectiveness, the patient's functional state has been somewhat relieved and PAH has been improved[20]. Therefore, this drug will be applied in the treatment of MHD-PAH patients. Due to the tendency of patients to experience negative emotional issues during dialysis, their quality of life is greatly affected, which hinders their treatment. To improve the patient's mood and physical fitness, aerobic exercise is adopted, and considering the impact of the patient's body, venue, etc., power cycling practice is chosen[21-23]. This type of aerobic exercise is easy to operate and suitable for practice in patients with MHD and PAH. Therefore, it is used as an auxiliary treatment method to study its therapeutic effect.
Overall, compared to group C, group I achieved better therapeutic effects. After treatment, unlike group C, group I patients had greater muscle strength and stronger willpower. They showed significant improvement in their upset, guilty, irritable, and fearful emotions, with more improvement in negative emotions, and higher SF-36 and KDTA scores (P < 0.05); They performed better in emotions of interest and encouragement, had higher levels of 6MWD indicators, and had lower Borg scores (P < 0.01); Its systolic pressure was lower, its vital capacity was larger, and its performance was better in the energetic, proud, enthusiastic, energetic and energetic mood; They had higher positive emotions, lower levels of SPAP and PVR indicators, and higher levels of PaO2 and SaO2 (P < 0.001); Meanwhile, their SF-36 and KDTA scores were higher, and the time effect P-values of general health status, physiological function, etc. were less than 0.05, indicating that the quality of life of MHD-PAH patients was influenced by time.
The results of the treatment indicate that the combination of Western medicine treatment with conventional treatment, in conjunction with dynamic circulation exercise, may result in more favorable outcomes. It is beneficial for improving patient emotions, improving their quality of life, and alleviating their PAH symptoms. Some scholars take patients after cardiac surgery as research objects. To improve their functional ability, they use upper limb bicycle force meter. After relevant tests, they find this method is safe and effective[24]. Some scholars focus on hemodialysis patients and provide power cycling training to alleviate their functional impairments. From the results, the patient's related muscle strength has been significantly enhanced[25]. Some researchers choose prostaglandin sodium and record relevant experimental data when treating CKD. The results show that the treatment effect is better[26].
To sum up, bicycle riding exercise combined with Western medicine therapy has a good effect, which enables patients to gradually become more positive and better alleviate negative emotions. The PVR level is significantly reduced, and the patients' quality of life is significantly improved. Therefore, the research results validate the effectiveness of using aerobic exercise to promote the prognosis and rehabilitation of HD patients, and can further improve their quality of life while reducing their negative emotions. This has important value for the clinical treatment of HD patients. In future research, it is necessary to further expand the sample size and increase the follow-up period to further enhance the robustness of result analysis, which is beneficial for improving the quality of life of HD patients and obtaining longer-term benefits.
| 1. | House T, Wightman A, Rosenberg A. Pediatric Nephrologists’ Perspectives on Palliative Care for Children with Chronic Kidney Disease: A National Cross-Sectional Survey (S554). J Pain Symptom Manage. 2022;63:935-936. [DOI] [Full Text] |
| 2. | Yaribeygi H, Butler AE, Atkin SL, Katsiki N, Sahebkar A. Sodium-glucose cotransporter 2 inhibitors and inflammation in chronic kidney disease: Possible molecular pathways. J Cell Physiol. 2018;234:223-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 104] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 3. | Matsuda R, Ashikaga K, Sato Y, Kida K, Ishibashi Y, Akashi YJ. Pulmonary Artery Hypertension after Arteriovenous Fistula Creation Subsequently Resolved by Closure of the Fistula. J St Marianna Univ. 2019;10:109-114. [DOI] [Full Text] |
| 4. | Hogan J, Salomon R, Krid S, Bonnet D, Legendre A. Pulmonary hypertension in an adolescent with end-stage-renal disease-a diagnostic challenge: Questions. Pediatr Nephrol. 2019;34:71. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Edmonston DL, Rajagopal S, Wolf M. Echocardiography to Screen for Pulmonary Hypertension in CKD. Kidney Int Rep. 2020;5:2275-2283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Burger CD. In reply-Exercise-Based Cardiopulmonary Rehabilitation: A Suitable Addition to Pharmacological Therapy for Pulmonary Hypertension. Mayo Clin Proc. 2022;97:191-192. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Sharman JE, Smart NA, Coombes JS, Stowasser M. Exercise and sport science australia position stand update on exercise and hypertension. J Hum Hypertens. 2019;33:837-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 54] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 8. | Yano J, Kaida Y, Maeda T, Hashida R, Tonan T, Nagata S, Hazama T, Nakayama Y, Ito S, Kurokawa Y, Otome T, Shibata R, Tashiro K, Kakuma T, Matsuse H, Fukami K. l-carnitine supplementation vs cycle ergometer exercise for physical activity and muscle status in hemodialysis patients: A randomized clinical trial. Ther Apher Dial. 2021;25:304-313. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Parry-williams G, Obaid D, Moser J, Vlahos I, Bulleros P, Fanton Z, Basu J, Miles C, Maclachlan H, Moreira-accame M, Bakalakos A, Hisham IBI, Chis-ster I, O’driscoll J, Papadakis M, Tome Esteban MT, Sharma S. 183 Low-grade hypertension and coronary atherosclerosis in male master endurance athletes. Heart. 2021;107 (Suppl 1):A142-A143. [DOI] [Full Text] |
| 10. | Moreno-Küstner B, Fábrega-Ruz J, Gonzalez-Caballero JL, Reyes-Martin S, Ochoa S, Romero-Lopez-Alberca C, Cid J, Vila-Badia R, Frigola-Capell E, Salvador-Carulla L. Patient-reported impact of symptoms in schizophrenia scale (PRISS): Development and validation. Acta Psychiatr Scand. 2022;145:640-655. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Beska B, Coakley D, MacGowan G, Adams-Hall J, Wilkinson C, Kunadian V. Frailty and quality of life after invasive management for non-ST elevation acute coronary syndrome. Heart. 2022;108:203-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Silva G, Costa J, Simon J, Bichon L, Doan A, Oudin V, Prevost A, Nazeyrollas P, Metz D. SF-36 is a fast and easy way of assessing quality of life and correlates with exercise capacity in patients undergoing cardiac rehabilitation. Arch Cardiovasc Dis. 2021;13:118-119. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Retory Y, David P, Niedzialkowski P, de Picciotto C, Bonay M, Petitjean M. Gait Monitoring and Walk Distance Estimation With an Accelerometer During 6-Minute Walk Test. Respir Care. 2019;64:923-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Agarwala P, Salzman SH. Six-Minute Walk Test: Clinical Role, Technique, Coding, and Reimbursement. Chest. 2020;157:603-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 214] [Article Influence: 35.7] [Reference Citation Analysis (0)] |
| 15. | Hemnes A, Rothman AMK, Swift AJ, Zisman LS. Role of biomarkers in evaluation, treatment and clinical studies of pulmonary arterial hypertension. Pulm Circ. 2020;10:2045894020957234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 16. | Jeelani H, Sharma M, Parry MA, Doley P, Pegu G. Pulmonary hypertension in end stage kidney disease (ESKD) patients on maintenance hemodialysis (MHD) via surgically created arteriovenous fistula. IJMBS. 2019;3:88-94. [DOI] [Full Text] |
| 17. | Song L, Quan ZL, Zhao LY, Cui DM, Zhong M, Zhou LF, Sun CY, Chen YG, Mo YW, Feng Z, Tao Y, Ye Z, Chen Y, Liang H, Lin T, Liu S, Liang XL, Fu X. Impact of pulmonary hypertension on arteriovenous fistula failure of hemodialysis patients: A 10 years follow-up cohort study. J Vasc Access. 2023;24:261-270. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Kurumatani H, Okada K, Origasa H, Fujita T, Isono M, Nakamoto H. Prostacyclin analog beraprost sodium efficacy in primary glomerular disease or nephrosclerosis: Analysis of the Japanese subgroup in CASSIOPEIR study. Ther Apher Dial. 2021;25:551-564. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 19. | Nakamoto H, Yu XQ, Kim S, Origasa H, Zheng H, Chen J, Joo KW, Sritippayawan S, Chen Q, Chen HC, Tsubakihara Y, Tamai H, Song SH, Vaithilingam I, Lee KW, Shu KH, Hok-King Lo S, Isono M, Kurumatani H, Okada K, Kanoh H, Kiriyama T, Yamada S, Fujita T. Effects of Sustained-Release Beraprost in Patients With Primary Glomerular Disease or Nephrosclerosis: CASSIOPEIR Study Results. Ther Apher Dial. 2020;24:42-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Dzikrul Haq Karimullah M, Ardining H. Autoimmune Hemolytic Anemia Causing Group 5 Pulmonary Hypertension: A Rare Case. HSJ. 2020;1:32-35. [DOI] [Full Text] |
| 21. | Shattla SI, Mabrouk SM, Abed GA. Effectiveness of Laughter yoga Therapy on job Burnout Syndromes among Psychiatric Nurses. IJN. 2019;6. [DOI] [Full Text] |
| 22. | Brown A, Jeffrey C, Moyle D. Laughter Yoga therapy in haemodialysis: one unit’s experience. RSAJ. 2019;15:38-46. [DOI] [Full Text] |
| 23. | Burstein D, Shah M, Grasso JD, White R, Rossano J, O'connor M, Lin K, Mcbride M, Paridon S. Low Utility of Nuclear Perfusion Exercise Stress Tests for Detecting Graft Vasculopathy in Children after Heart Transplantation. J Heart Lung Transplant. 2019;38:S472-S473. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 24. | Gardenghi G, Kushida CL, Dias AF, Cruz JB, De Lima KR, De Souza AH. Pilot study of viability in the use of cycle ergometer for upper limbs in the immediate postoperative period of cardiac surgery. Rev Pesq Fisio. 2019;9:179-186. [DOI] [Full Text] |
| 25. | Abdo AL, Sens YADS, Miorin LA, Xavier VB, Fernandes ADO, Alves VLDS. Quadriceps muscle strength after training with a cycloergometer in patients on hemodialysis. Fisioter mov. 2019;32:e003237. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 26. | Shimamura M, Miyakawa J, Doi M, Okada K, Kurumatani H, Mori Y, Oshida K, Nakajo I, Oikawa K, Ushigome F, Miyashita A, Isono M, Miyamoto Y. The Pharmacokinetics of Beraprost Sodium Following Single Oral Administration to Subjects With Impaired Kidney Function. J Clin Pharmacol. 2017;57:524-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |