Published online Jan 16, 2024. doi: 10.12998/wjcc.v12.i2.412
Peer-review started: October 9, 2023
First decision: November 13, 2023
Revised: November 27, 2023
Accepted: December 22, 2023
Article in press: December 22, 2023
Published online: January 16, 2024
Processing time: 94 Days and 4.9 Hours
Cervical cancer is a rare primary tumor resulting in metastases to the breast with few cases reported in literature. Breast metastases are associated with poor prognosis. The following case highlights the diagnostic challenges associated with metastatic cervical cancer to the breast along with individualized treatment.
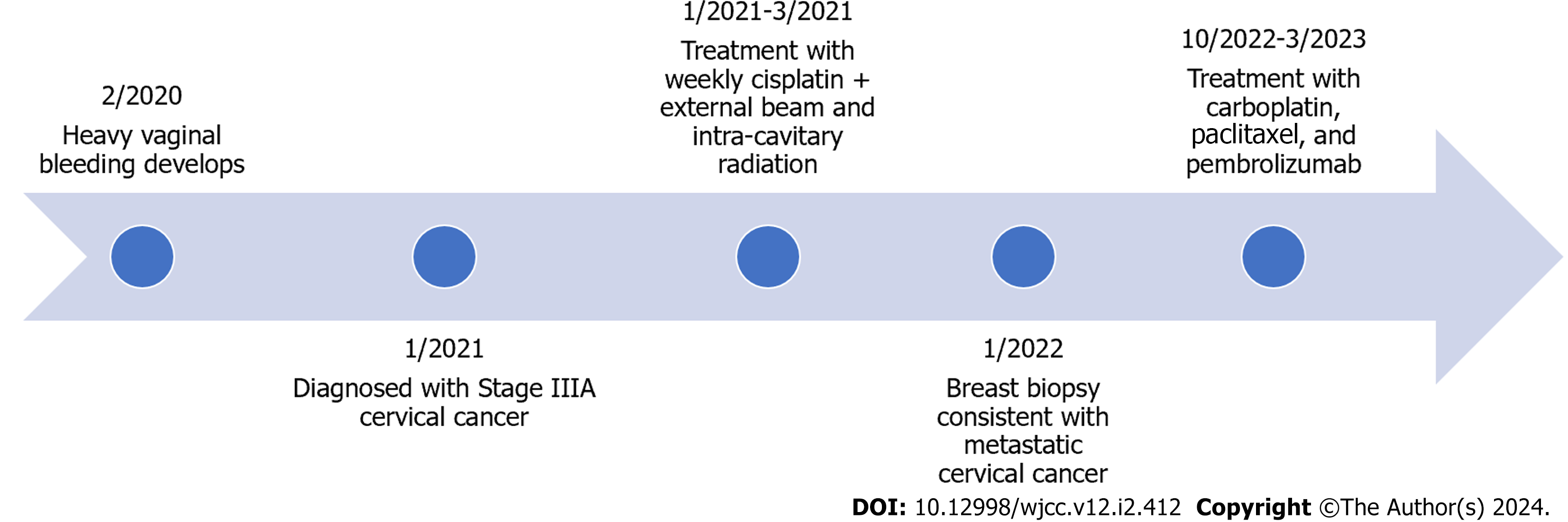
A 44-year-old G7P5025 with no significant past medical or surgical history presented with heavy vaginal to an outside emergency department where an exam and a pelvic magnetic resonance imaging showed a 4.5 cm heterogenous lobulated cervical mass involving upper two thirds of vagina, parametria and lymph node metastases. Cervical biopsies confirmed high grade adenocarcinoma with mucinous features. A positron emission tomography/computed tomography (PET/CT) did not show evidence of metastatic disease. She received concurrent cisplatin with external beam radiation therapy. Follow up PET/CT scan three months later showed no suspicious fluorodeoxyglucose uptake in the cervix and no evidence of metastatic disease. Patient was lost to follow up for six months. She was re-imaged on re-presentation and found to have widely metastatic disease including breast disease. Breast biopsy confirmed programmed death-ligand 1 positive metastatic cervical cancer. The patient received six cycles of carboplatin and paclitaxel with pembrolizumab. Restaging imaging demonstrated response. Patient continued on pembrolizumab with disease control.
Metastatic cervical cancer to the breast is uncommon with nonspecific clinical findings that can make diagnosis challenging. Clinical history and immunohistochemical evaluation of breast lesion, and comparison to primary tumor can support diagnosis of metastatic cervical cancer to the breast. Overall, the prognosis is poor, but immunotherapy can be considered in select patients and may result in good disease response.
Core Tip: Metastatic cervical cancer to the breast is rare with nonspecific clinical findings that can make diagnosis challenging. Clinical history, histology and immunohistochemical evaluation of the breast lesion, and comparison to the primary tumor can support the diagnosis of metastatic cervical cancer rather than a primary breast malignancy. Overall, the prognosis is poor, but immunotherapy can be considered in select patients and may result in good disease response.
- Citation: Akers A, Read S, Feldman J, Gooden C, English DP. Diagnostic challenges and individualized treatment of cervical adenocarcinoma metastases to the breast: A case report. World J Clin Cases 2024; 12(2): 412-417
- URL: https://www.wjgnet.com/2307-8960/full/v12/i2/412.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i2.412
Metastases to the breast are uncommon, accounting for approximately 2% of all malignant breast tumors[1,2]. Breast metastases most commonly arise from the contralateral breast or a hematologic malignancy but have also been reported to develop from melanoma, lung, gastric, ovarian, and neuroendocrine cancers[1-3]. Cervical cancer is a rare primary tumor resulting in metastases to the breast with few cases reported in literature. Cervical cancer typically metastasizes through direct invasion of local structures, hematogenous dissemination, or dissemination through the lymphatic system, but the exact mechanism in which it metastasizes to the breast is unknown[1,4]. Breast metastases are associated with poor prognosis as they represent widely disseminated disease burden at the time of diagnosis[5,6]. The following case highlights the diagnostic challenges associated with metastatic cervical cancer to the breast along with individualized therapy for treatment.
A 44-year-old G7P5025 presented with heavy vaginal bleeding, pelvic pressure, and constipation.
She initially presented to an outside emergency department for vaginal bleeding where an exam and pelvic magnetic resonance imaging (MRI) showed a 4.5 cm heterogenous lobulated cervical mass confined to the upper two thirds of the vagina. MRI pelvis also showed possible bilateral iliac lymphadenopathy.
Her gynecologic history was significant for menarche at age 13 with regular monthly periods. She denied a history of abnormal Pap smears however her most recent Pap smear was approximately ten years prior. The patient was not up to date with general screening recommendations including mammogram imaging.
She had no significant past medical, family or surgical history.
On presentation to our clinic, physical exam demonstrated a 5 cm cervical mass impinging on the rectum with no normal cervical tissue identified. The mass was noted to involve the upper and posterior lower vagina and parametrium, consistent with clinical stage IIIa cervical cancer.
Cervical biopsies confirmed high grade adenocarcinoma with mucinous features (Figure 1A).
A positron emission tomography/computed tomography (PET/CT) scan at the time of diagnosis did not show evidence of metastatic disease.
She was initially diagnosed with clinical stage IIIa cervical cancer. She received six weeks of concurrent cisplatin with external beam radiation therapy with 50.4 Gy in 28 fractions followed by Ir-192 high dose rate brachytherapy. Follow up PET/CT scan three months later showed no suspicious fluorodeoxyglucose uptake in the cervix or uterus and no evidence of metastatic disease. The patient declined repeat PET/CT three months after that for further evaluation of treatment response.
She was then lost to follow up for six months. On re-presentation, she reported firmness along the right nipple over the last few months. Physical exam was significant for dimpling of skin and firmness around the right nipple and peau d’orange-like appearance of the right breast concerning for new inflammatory breast cancer. Interestingly, she had no evidence of residual disease on pelvic exam, and Pap smear collected at this time was negative for intraepithelial lesions or malignancy. The patient underwent diagnostic mammography and right breast biopsies with initial pathology concerning for high grade invasive lobular carcinoma. Breast MRI was significant for multi-centric right breast carcinoma with invasion to the right pectoralis muscle and enlarged right internal mammary lymph nodes concerning for metastatic disease. Additional immunohistochemical staining of the breast biopsy showed the carcinoma cells to be positive for p16 and PAX-8 and human papillomavirus 16/18 positive. Review of prior cervical biopsies for comparison confirmed that the new breast mass was most consistent with metastatic cervical cancer (Figures 1B and 2).
She received at the time of initial diagnosis six weeks of concurrent cisplatin with external beam radiation therapy. For her recurrent metastatic disease including metastases to the breast, she received six cycles of carboplatin and paclitaxel with pembrolizumab. Bevacizumab was not given with this regimen as there was a concern for increased risk of rectovaginal fistula given her initial perirectal disease and the amount of radiation delivered to that area at the time of initial treatment (Figure 2).
Restaging imaging demonstrated partial response to carboplatin and paclitaxel with pembrolizumab (Figure 3). The patient continued on pembrolizumab with disease control.
Distant metastases in cervical cancer are most commonly reported to the liver, lung, and bone with breast metastases rarely reported in the literature[3]. The infrequency of breast metastases and even rarer occurrence of metastatic cervical cancer to the breast presents diagnostic challenges for clinicians. Most patients present with a palpable breast mass, and clinical exam alone is often insufficient in differentiating between a primary breast malignancy and metastatic disease[3,7]. Among reported cases in the literature describing metastatic cervical cancer to the breast, there are only two documented cases of metastatic cervical adenocarcinoma presenting as a new inflammatory breast cancer[4,8]. However, both of the aforementioned patients had other symptoms or evidence of non-skeletal disease on presentation. Ward et al[8] describes a case of metastatic cervical adenocarcinoma presenting as inflammatory breast cancer with simultaneous wide-spread venous thrombosis. In a more recent case described by Cholmondeley et al[4], the patient’s inflammatory breast lesion occurred during brachytherapy for known cervical adenocarcinoma. To our knowledge, this is the only documented case of metastatic cervical adenocarcinoma in which an inflammatory breast lesion is the only evidence of non-skeletal disease on presentation. Cervical pap smear was negative with no evidence of disease on pelvic exam when this patient presented with the new breast changes. The exam findings limited to the breast in this patient further exacerbated existing diagnostic challenges.
As previously stated, clinical exam alone is insufficient, and histologic and immunohistochemical evaluation are often necessary to confirm metastatic disease to the breast[5,7]. High grade cytologic features, lack of elastosis, or histology abnormal for a primary mammary malignancy should raise suspicion of a metastatic lesion[6]. Histologic comparison to the primary tumor is particularly helpful in establishing a diagnosis. Immunohistochemical evaluation can further support the diagnosis of metastatic disease, although no marker is 100% sensitive or specific[6]. In the case of metastatic cervical cancer, positive p16 reactivity with negative reactivity for estrogen receptor, progesterone receptor, HER2 and mammoglobin support the diagnosis of metastatic disease with the right clinical history[4]. Review of our patient’s original cervical biopsies in addition to immunohistochemical staining of the breast showing p16 and PAX-8 reactivity and negative reactivity for mammoglobin ultimately lead to the diagnosis of metastatic cervical adenocarcinoma.
Historically, the prognosis for patients with extramammary metastases to the breast is overall poor, with a median survival time of 10 mo after breast metastases diagnosis[5]. In patients with an extramammary primary in which metastatic disease is limited to the breast or with minimal overall disease burden, conservative surgical treatment can be offered[5,9]. However, treatment should be individualized, and often systemic or palliative treatment is most appropriate[6]. In a literature review of patients with metastatic cervical cancer to the breast, the majority of patients were treated with chemotherapy, radiation, or both[3]. Only one case utilizing monoclonal antibody treatment is documented in the literature. Cholmondeley et al[4] described treatment of metastatic cervical adenocarcinoma to the breast with carboplatin and paclitaxel with bevacizumab. However, immunotherapy has never been described in the treatment of these patients. Our case is the only documented use of immunotherapy in patients with metastatic cervical cancer to the breast and the only case describing maintenance therapy with pembrolizumab. Pembrolizumab is an anti-programmed death 1 (PD-1) monoclonal antibody that has shown promising results in patients with persistent, recurrent, or metastatic cervical cancer[10]. Somatic tumor testing showed that our patient is programmed death-ligand 1 positive and she had good a response to chemotherapy and pembrolizumab. Nivolumab, another anti-PD-1 antibody was not utilized in treating this patient as pembrolizumab is the National Comprehensive Cancer Network preferred anti-PD-1 agent for patients with persistent, recurrent or metastatic cervical cancer following from the data of the KEYNOTE-826 trial in this patient population.
Our case was limited in some ways by the patient’s poor follow up and presentation to outside hospital systems. However, this case demonstrates the role of individualized therapy with consideration of immunotherapy in metastatic cervical cancer to the breast depending on biomarker status.
Metastatic cervical cancer to the breast is rare with nonspecific clinical findings that can make diagnosis challenging. Clinical history, histology and immunohistochemical evaluation of the breast lesion, and comparison to the primary tumor can support the diagnosis of metastatic cervical cancer rather than a primary breast malignancy. Overall, the prognosis is poor, but immunotherapy can be considered in select patients and may result in good disease response. Therefore, individualized therapy should be offered to patients with metastatic cervical cancer to the breast.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Safarzadeh Kozani P, Iran S-Editor: Wang JJ L-Editor: A P-Editor: Cai YX
| 1. | DeLair DF, Corben AD, Catalano JP, Vallejo CE, Brogi E, Tan LK. Non-mammary metastases to the breast and axilla: a study of 85 cases. Mod Pathol. 2013;26:343-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 114] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 2. | Wan X, Zhang H, Zhang Y, Peng Y. Metastases to the Breast from Extramammary Nonhematological Malignancies: Case Series. Int J Gen Med. 2020;13:1105-1114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Kumar L, Pokharel YH, Dawar R, Thulkar S. Cervical Cancer Metastatic to the Breast: A Case Report and Review of the Literature. Clin Oncol. 1999;11:414-416. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Cholmondeley K, Callan L, Sangle N, D'Souza D. Metastatic cervical adenocarcinoma to the breast: A case report and literature review. Gynecol Oncol Rep. 2019;28:33-36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Williams SA, Ehlers RA 2nd, Hunt KK, Yi M, Kuerer HM, Singletary SE, Ross MI, Feig BW, Symmans WF, Meric-Bernstam F. Metastases to the breast from nonbreast solid neoplasms: presentation and determinants of survival. Cancer. 2007;110:731-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 116] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 6. | Lee AH. The histological diagnosis of metastases to the breast from extramammary malignancies. J Clin Pathol. 2007;60:1333-1341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 116] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 7. | Mangla A, Agarwal N, Saei Hamedani F, Liu J, Gupta S, Mullane MR. Metastasis of cervical cancer to breast: A case report and review of literature. Gynecol Oncol Rep. 2017;21:48-52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Ward R, Conner G, Delprado W, Dalley D. Metastatic adenocarcinoma of the cervix presenting as an inflammatory breast lesion. Gynecol Oncol. 1989;35:399-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Klingen TA, Klaasen H, Aas H, Chen Y, Akslen LA. Secondary breast cancer: a 5-year population-based study with review of the literature. APMIS. 2009;117:762-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Colombo N, Dubot C, Lorusso D, Caceres MV, Hasegawa K, Shapira-Frommer R, Tewari KS, Salman P, Hoyos Usta E, Yañez E, Gümüş M, Olivera Hurtado de Mendoza M, Samouëlian V, Castonguay V, Arkhipov A, Toker S, Li K, Keefe SM, Monk BJ; KEYNOTE-826 Investigators. Pembrolizumab for Persistent, Recurrent, or Metastatic Cervical Cancer. N Engl J Med. 2021;385:1856-1867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 597] [Article Influence: 149.3] [Reference Citation Analysis (0)] |