Published online Jul 6, 2024. doi: 10.12998/wjcc.v12.i19.3854
Revised: May 11, 2024
Accepted: May 20, 2024
Published online: July 6, 2024
Processing time: 81 Days and 21.4 Hours
Cold-dampness-type knee osteoarthritis is a common middle-aged and elderly disease, but its pathogenesis is not fully understood, and its clinical treatment has limitations. Glucosamine sulfate capsules are commonly used for treating arthritis, and San Bi Tang is a classic formula of traditional Chinese medicine (TCM) that has the effects of warming yang, dispelling dampness, relaxing muscles, and activating collaterals. This research hypothesized that the combination of modified San Bi Tang and glucosamine sulfate capsules could enhance the clinical efficacy of treating cold-dampness-type knee osteoarthritis through complementary effects.
To analyze the clinical efficacy of San Bi Tang combined with glucosamine sulfate capsules when treating cold-dampness-type knee osteoarthritis.
A total of 110 patients with cold-dampness-type knee osteoarthritis were selected as research subjects and randomly divided into a control group and an experimental group of 55 cases each. The control group received only treatment with glucosamine sulfate capsules, while the experimental group received additional treatment with modified San Bi Tang for a duration of 5 wk. The patients’ knee joint functions, liver and kidney function indicators, adverse reactions, and vital signs were evaluated and analyzed using SPSS 26.0 software.
Before treatment, the two groups’ genders, ages, and scores were not significantly different, indicating comparability. Both groups’ scores improved after treatment, which could indicate pain and knee joint function improvement, but the test group had better scores. The TCM-specific symptoms and the clinical efficacy of the treatment in the test group were higher. Before and after treatment, there were no abnormalities in the patients’ liver and kidney function indicators.
The combination of modified San Bi Tang and glucosamine sulfate capsules is superior to treatment with sulfated glucosamine alone and has high safety.
Core Tip: This study evaluates the effectiveness and safety of modified San Bi Tang combined with glucosamine sulfate capsules in treating cold dampness type knee osteoarthritis (KO). It reveals that this combination therapy significantly improves pain, knee joint function, and traditional Chinese medicine (TCM)-specific symptoms compared to glucosamine sulfate alone. Utilizing visual simulation scores, osteoarthritis index scores, and functional tests, the research highlights the superior clinical efficacy of the combined treatment. Safety assessments indicate no adverse impacts on liver and kidney functions, suggesting a high safety profile. These findings advocate for the integration of TCM with conventional treatments in KO management, offering a promising alternative for patients seeking relief from osteoarthritis symptoms.
- Citation: Ni HY, Zhang YP, Zhang XF. Therapeutic effect of San Bi Tang combined with glucosamine sulfate capsules in cold-dampness-type knee osteoarthritis. World J Clin Cases 2024; 12(19): 3854-3865
- URL: https://www.wjgnet.com/2307-8960/full/v12/i19/3854.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i19.3854
Knee osteoarthritis (KO) is a common inflammatory disease of the joints, which is characterized by joint pain, swelling, stiffness, and functional impairment. The incidence rate of this disease gradually increases with age, which has a serious impact on the quality of life and health of patients[1,2]. At present, western medicine mainly uses non-steroidal anti-inflammatory drugs, glucocorticoids, and other drugs to treat KO. Although they can alleviate pain and inflammation, long-term use can lead to gastrointestinal reactions, liver and kidney damage, and other side effects. In addition, although surgical treatments such as joint replacement have significant therapeutic effects, the surgical risks and expensive medical costs deter many patients. Therefore, seeking a safe, effective, and less likely to cause side effects treatment method is a focus of clinical research. Traditional Chinese medicine (TCM) has significant advantages in treating arthritis. Firstly, TCM treatment can regulate the etiology and pathogenesis, thereby achieving the goal of treating both the symptoms and the root cause. Secondly, TCM treatment has individualized characteristics, which can be differentiated and treated based on the patient's condition, constitution, and symptoms to improve treatment effectiveness. In addition, TCM treatment has lower side effects, which can reduce patients’ pain while ensuring efficacy. The middle-aged and elderly, as well as postmenopausal women, are a high incidence group of KO, with an aging population trend. The number of patients with this disease is increasing, which has attracted widespread attention from society. Related investigations show that the incidence rate of osteoarthritis is about 15%. People over 60 years old are about 50%, and people over 75 years old are about 80%, of which KO accounts for the majority[3]. Local chronic aseptic inflammation is considered to be the cause of KO. Under the action of chronic inflammation, joint cartilage and other tissues will be correspondingly damaged. TCM experts have an early understanding of KO, as recorded in "Su Wen": the three qi of wind, cold, and dampness are mixed together to form Bi. TCM categorizes KO as knee joint obstruction and believes it is related to the invasion of wind, cold, and dampness[4]. Common oral medications in western medicine include non-steroidal anti-inflammatory drugs and cartilage protectors. The surgical treatment methods include arthroscopic surgery, osteotomy, etc. The effectiveness of western medicine treatment is fast, while the risk and cost of treatment are high[5]. TCM treatment for KO includes oral administration of TCM decoction, external application of TCM and acupuncture and moxibustion. The oral administration of TCM decoction is a commonly used method, which has obvious effects and minimal adverse reactions[6]. For the combination of modified San Bi Tang and glucosamine sulfate capsules (GSC) in the treatment of KO patients, its clinical efficacy and safety are explored by using visual analysis scale (VAS) and clinical observations. The research hypothesis is that the clinical efficacy and safety of the combination of modified San Bi Tang and GSC in the treatment of cold dampness type KO are better than those of GSC alone. The research objective is to compare the clinical efficacy, TCM symptom efficacy, and adverse reactions of two treatment methods, providing reference for the rational selection of treatment plans.
This study was conducted in the outpatient clinic of Fuyang Traditional Chinese Medicine Bone Trauma Hospital in Hangzhou. The cold and wet KO patients from April 2020 to April 2023 were selected, and the selection process should strictly comply with ethical standards[7]. All study subjects met the early and mid-term inclusion criteria for KO patients, and 110 study subjects were ultimately obtained. The inclusion criteria are as follows: (1) Meet the diagnostic criteria of TCM and Western medicine; (2) Unilateral onset of knee joint, clinically manifested as early and mid-stage patients; (3) The age range is [50, 70] years old, without gender restrictions; (4) No relevant treatment was given two weeks before the experiment; (5) VAS is less than or equal to 6; and (6) Subjects signed an informed consent form. Exclusion items are: (1) Patients with rheumatoid arthritis and other diseases; (2) Breastfeeding and pregnant women; (3) Patients with coagulation disorders; (4) Patients who are intolerant of TCM; and (5) Patients who received hormone therapy nearly 60 d before the experiment. 110 study subjects who met the criteria were classified into two groups. The control group (CG) and test group (TG) have 55 patients, respectively.
The study lasted for 5 wk, and CG patients received GSC treatment, taking 0.5 g three times a day. TG was treated with modified San Bi Tang based on CG. The dosage and composition of San Bi Tang include Heracleum hemsleyanum Diels (6 g), Saposhnikovia divaricata (6 g), Cinnamomum cassia Presl (6 g), Radix Codonopsis Pilosulae (12 g), Gentianae Macrophyllae Radix (6 g), Angelica sinensis (6 g), Poria cocos (6 g), Moxibustion of licorice (6 g), Asarum (3 g), Rehmannia glutinosa (12 g), Eucommia ulmoides (12 g), Astragalus membranaceus (15 g), Chuanxiong (6 g), Paeonia lactiflora (12 g), Achyranthes bidentata (12 g), Dipsacus asperus (12 g). The efficacy of San Bi Tang is to dissipate cold and remove dampness, dispel wind and relieve pain. Meanwhile, it needs to be adjusted according to the patient's concurrent symptoms. Patients with wet weight need to add Rhizoma Atractylodis. Patients with severe cold need to join Rhizoma Zingiberis. All drugs are decocted in a TCM room, with each bag of 200 mL. Patients take warm medication twice a day in the morning and evening. All research subjects should avoid getting cold on their knees during treatment, pay attention to keeping warm, and avoid prolonged squatting and physical labor. The patient needs to carry out leg lifting and quadriceps femoris muscle exercise under guidance, straighten the thigh and lower leg, raise the heel about 25 cm from the bed surface, and then keep it for 5 s and slowly put it down, which is a movement standard. The patient should do at least 22 exercises at a time and practice four times a day.
The study uses VAS for pain evaluation, with a VAS value interval of [0, 10]. The [0, 2] interval represents comfort, the [3, 4] interval represents mild discomfort, the [5, 6] interval represents moderate discomfort, the [7, 8] interval represents severe discomfort, and the [9, 10] interval represents extreme discomfort. The osteoarthritis index score (WOMAC) evaluates patients' pain, stiffness, and activity. The WOMAC score includes 5 cases of pain, 2 cases of stiffness, and 17 cases of difficulty in daily activities. A score of 0 means no difficulty, 1 is mild difficulty, 2 indicates moderate difficulty, 3 means very difficult, and 4 represents extreme difficulty. The higher the VAS score and WOMAC exponential integral, the more serious the osteoarthritis. The patient’s knee joint function is evaluated by sitting up for 30 s. The more time it is completed within 30 s, the knee joint is better. In the experiment, patients should be encouraged to complete as many times as possible within 30 s.
Clinical efficacy evaluation criteria: Efficacy observation is calculated from the sixth week after the start of treatment. The improvement rate before and after treatment is calculated using the efficacy evaluation calculation formula. The efficacy evaluation is divided into four levels. Invalid: WOMAC score reduction is less than 30%. Effective: WOMAC score decreases by more than 30% and less than 70%. Significant effect: WOMAC score decreases by more than 70% and less than 95%. Clinical control: WOMAC score decreases by more than 95%.
The study combines the TCM Symptom Score Table to determine the efficacy of TCM. The study uses the symbolic efficacy (SE) judgment standard to determine TCM SE, and the efficacy included four levels: ineffective, effective, significant, and clinical recovery. The criteria for determining SE in TCM include five main symptoms: joint pain, joint tenderness, joint stiffness, joint swelling and pain, and joint activity. The points are divided into four levels: 0, 2, 4, and 6. Five sub-symptoms are included: fear of wind and cold, joint chills, lukewarm hands and feet, limb difficulties, and tongue and pulse disorders. The points are divided into four levels: 0, 1, 2, and 3. TCM SE assessment includes four levels. Invalid: TCM symptom score reduction is less than 30%. Effective: The reduction of TCM syndrome points is greater than 30% and less than 70%. Significant effect: The reduction in TCM syndrome points is greater than 70% and less than 95%. Clinical recovery: TCM symptom scores decrease by more than 95%.
The safety evaluation includes liver and kidney function indicators, adverse reactions, and vital signs of patients before and after treatment. In the experiment, the incidence and severity of adverse reactions are evaluated, and doctors judge whether they are related to treatment. Liver and kidney function indexes include alanine transaminase (ALT), and its normal range is 7 to 40 U/L. The normal range of aspartate transaminase (AST) is 13 to 35 U/L. The normal range of alkaline phosphatase (ALK) is 35 to 100 U/L. The normal range of glutamyltranspeptidase (GGT) is 7 to 45 U/L. The direct bilirubin (DBil) is from 0 to 6.0 μmol/L. The total bilirubin (TBil) is from 1.7 to 17.1 μmol/L. The normal range of total protein (TP) is 65 to 80 g/L. The normal range of albumin (ALB) is 40 to 50 g/L. The normal range of globulin (GLOB) is 20 to 40 g/L. Renal function examination indicators include endogenous creatinine clearance rate (Ccr), which is within the normal range of 80 to 120 mL/min. The normal range of blood urea nitrogen (BUN) is 2.9 to 7.5 mmol/L. The normal range of uric acid (UA) is 90 to 420 μmol/L.
The research data are analyzed by SPSS26.0. Chi square distribution is applied to test counting data. mean ± SD is the data description, which is consistent with normal distribution and tested by t test. The median and upper and lower quartile expressions are tested and ranked by rank sum test. If P < 0.05, it indicates statistical significance[8].
The study divided 110 study subjects who met the criteria into two groups, with 55 patients in CG and 55 patients in TG. General information includes age, gender, disease course, disease stage, and disease location, and they are not significant (P > 0.05). Table 1 shows the comparison results.
| Baseline information | CG | TG | Statistical value | P value |
| Gender (male/female) | 18/37 | 19/36 | 0.0407 | 0.8401 |
| Age (yr) | 59.63 ± 4.36 | 59.73 ± 5.01 | 0.1117 | 0.9113 |
| Disease course (wk) | 49.82 ± 17.95 | 50.62 ± 16.53 | 0.2431 | 0.8084 |
| Stage (early/mid) | 37/18 | 35/20 | 0.1608 | 0.6884 |
| Location (left/right) | 30/25 | 25/30 | 0.9091 | 0.3404 |
The average age of patients in CG and TG was (59.63 ± 4.36) years and (59.73 ± 5.01) years, respectively. The average course of disease was (49.82 ± 17.95) wk and (50.62 ± 16.53) wk, respectively. In the study cases, women accounted for about one third and women accounted for about two thirds, basically consistent with the epidemiological sex ratio of KO. The main reason why female patients are greater than men is that estrogen can inhibit bone resorption. Most of the female patients in the study have already menopaused, and their levels of estrogen are relatively low.
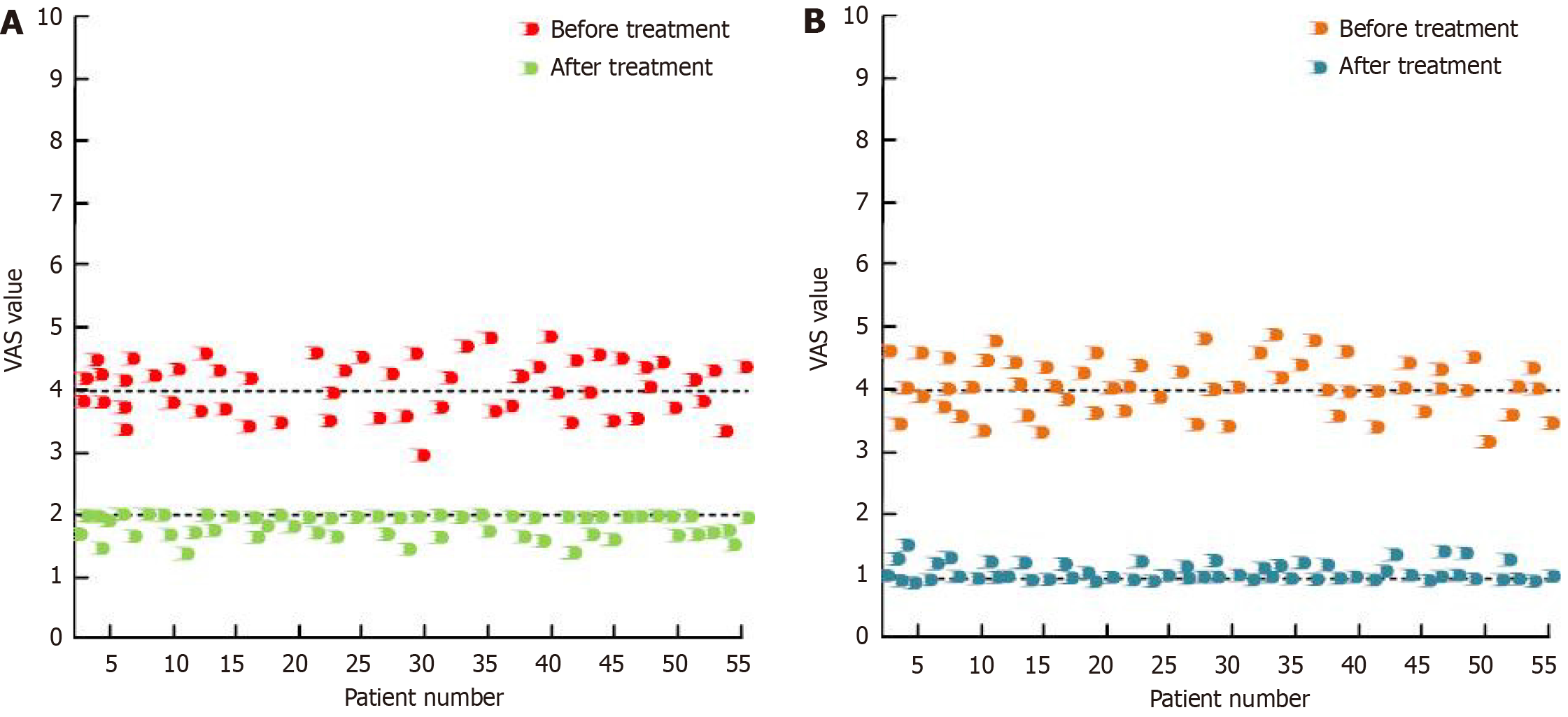
The pain evaluation of patients was evaluated using VAS in Figure 1. Figure 1A shows the VAS results in CG and they are within [3, 5] interval before treatment, while they are within [1.25, 2] interval after treatment. Figure 1B shows the VAS results in CG and they are within [3, 5] interval before treatment, while they are within [1, 2] interval after treatment. Table 2 shows two groups’ VAS results [M (P25, P75)].
| Group | Before treatment | After treatment | Z | P value |
| CG | 4 (3, 5) | 2 (1.25, 2) | 3.273 | 0.002 |
| TG | 4 (3, 5) | 1 (1, 2) | 1.736 | 0.003 |
| Z | 1.959 | 0.000 | - | - |
| P value | 1.001 | 0.002 | - | - |
In Table 2, two groups’ VAS results were compared, and they were not significant before treatment (P > 0.05). After treatment, two groups’ VAS results were significant (P < 0.05). After treatment, the VAS results decreased, indicating that both treatment regimens can alleviate pain in KO patients. Among them, TG decreased by 1 [1, 2] and CG decreased by 2 [1.25, 2]. The significant decrease in TG indicates that the pain relief effect of TG treatment is superior to CG.
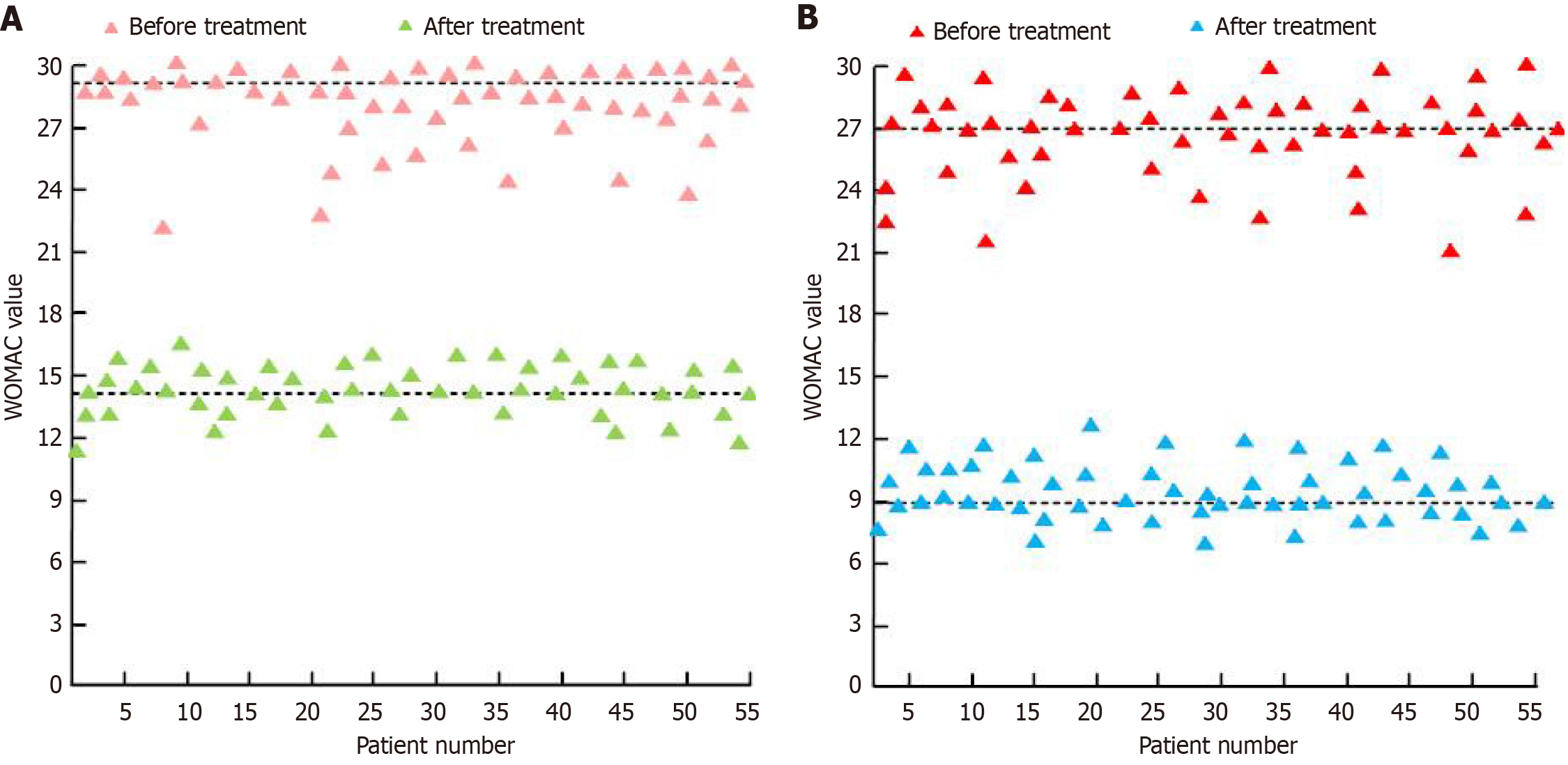
The patient's osteoarthritis index was estimated using the WOMAC score. Figure 2 shows the distribution of WOMAC scores. Figure 2A shows the comparison of WOMAC results in CG. The distribution of WOMAC results were within [21, 30] interval before treatment, while the distribution of WOMAC results were within [9, 18] interval after treatment. Figure 2B shows the comparison of WOMAC results in TG. The distribution of WOMAC results were within [21, 30] interval results before treatment, while the distribution of WOMAC results were within [6, 13] interval after treatment. Table 3 shows the comparison of WOMAC results.
| Group | Before treatment | After treatment | Z | P value |
| CG | 29.13 ± 8.40 | 14.05 ± 3.52 | 12.267 | 0.000 |
| TG | 27.72 ± 7.26 | 9.75 ± 3.52 | 16.518 | 0.000 |
| t | 0.9418 | 6.4061 | - | - |
| P value | 0.3484 | 0.000 | - | - |
In Table 3, two groups’ WOMAC results showed that P > 0.05 before treatment, meaning comparability. The intra-group and inter-group WOMAC results were P < 0.05 after treatment. After both treatment regimens, the WOMAC score decreased, indicating that both treatment regimens can improve joint function. After TG treatment, it was 9.75 ± 3.52. After CG treatment, it was 14.05 ± 3.52. The decrease in TG was greater than CG, indicating that the joint improvement effect of TG's treatment plan was better than CG.
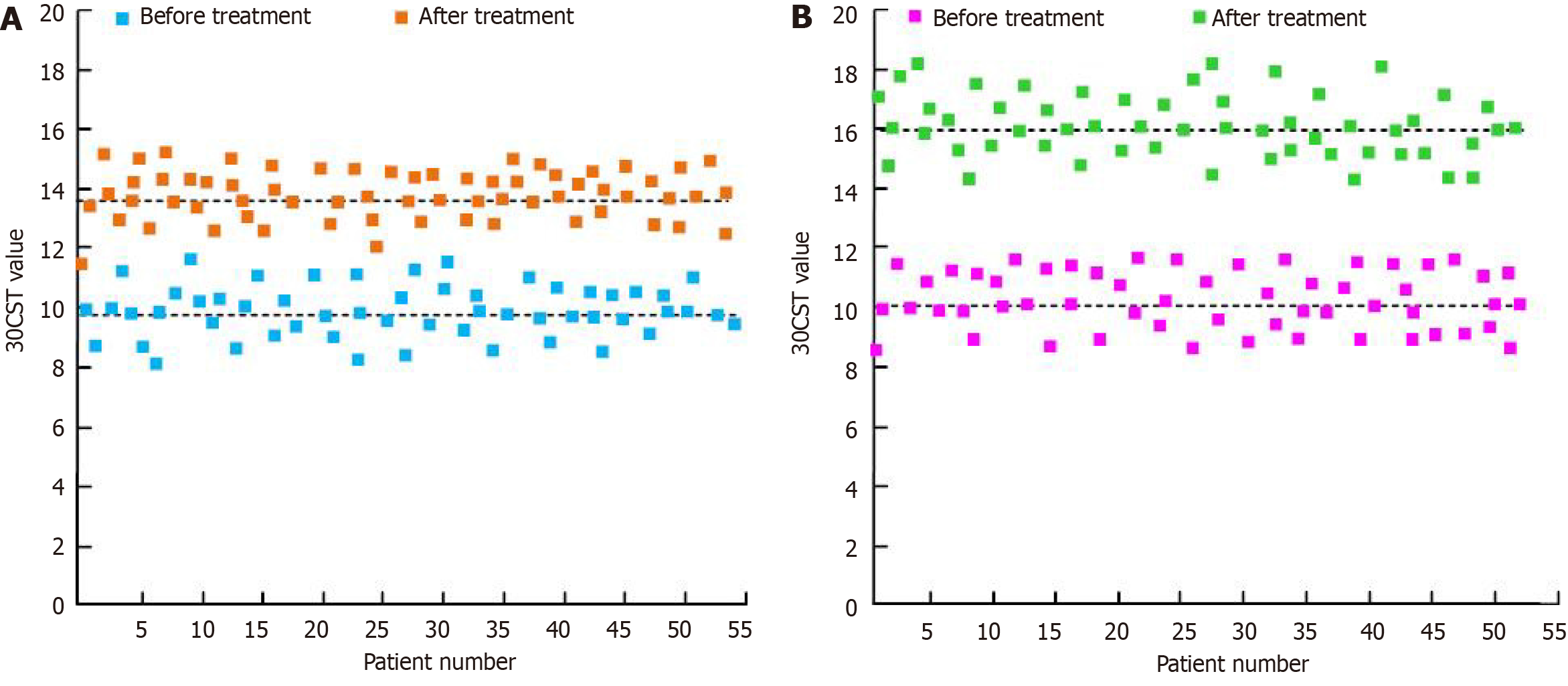
The study used a 30 s Chair Stand Test (30CST) test to evaluate knee joint function in patients. Figure 3 shows the 30CST results. Figure 3A shows the 30CST results in CG. The distribution of pre-treatment 30CST results was within the [8, 12] interval, and the post treatment 30CST score was within the [11, 16] interval. Figure 3B shows the comparison of 30CST scores before and after TG treatment. The distribution of the pre-treatment 30CST score was within the [8, 12] interval, and the post treatment 30CST score was within the [14, 19] interval. Table 4 shows the 30CST results.
| Group | Before treatment | After treatment | Z | P value |
| CG | 10.89 ± 2.01 | 12.01 ± 2.21 | 2.7804 | 0.003 |
| TG | 11.12 ± 2.03 | 16.01 ± 2.22 | 12.005 | 0.000 |
| t | 0.597 | 9.470 | - | - |
| P value | 0.275 | 0.000 | - | - |
In Table 4, two groups’ 30CST results showed that P > 0.05 before treatment, indicating comparability. After treatment, the intra-group and inter-group 30CST results were P < 0.05. After both treatment regimens, the 30CST score increased, indicating that both treatment regimens can improve knee joint performance. The average value after TG treatment was 16.01, and the average value after CG treatment was 13.01. The significant change in the 30 CST score after TG treatment indicated that the knee joint performance improvement effect of TG treatment was better than that of CG.
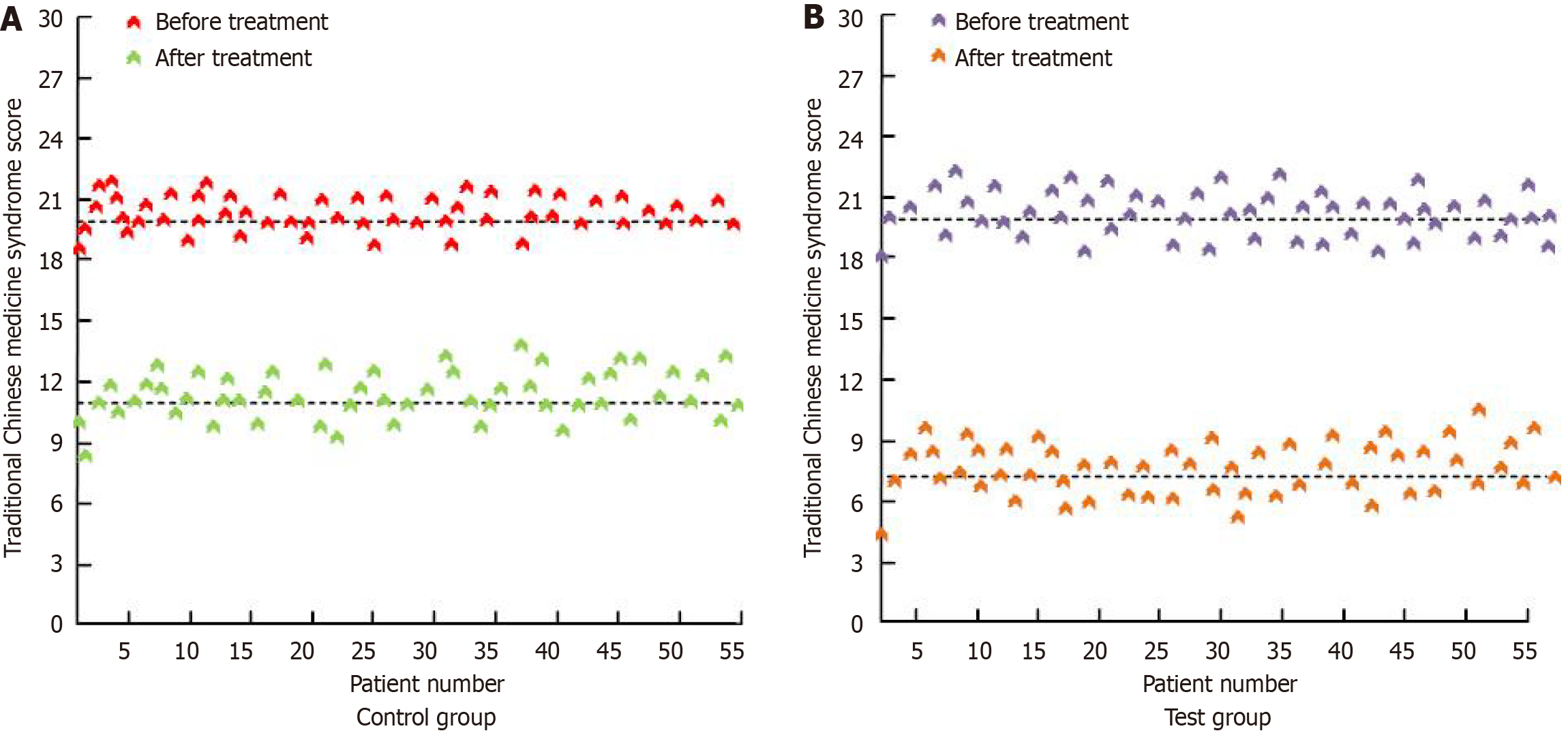
This study evaluated the symptoms like pain and worsening of cold in the treatment method using TCM syndrome scores. Figure 4 shows the distribution of TCM syndrome results. Figure 4A shows the TCM syndrome results in CG. The TCM syndrome results were within [18, 22] interval before treatment, while the TCM syndrome results were within [8, 15] interval after treatment. Figure 4B shows the TCM syndrome results in TG. The TCM syndrome results were within [18, 23] interval before treatment, while the TCM syndrome results were within [4, 11] interval after treatment. Table 5 shows the TCM syndrome results.
| Group | Before treatment | After treatment | Z | P value |
| CG | 10.89 ± 2.01 | 12.36 ± 2.21 | 3.6493 | 0.000 |
| TG | 10.76 ± 2.03 | 16.01 ± 2.22 | 12.943 | 0.000 |
| t | 0.3375 | 8.6414 | - | - |
| P value | 0.7364 | 0.000 | - | - |
In Table 5, the comparison of TCM symptom scores between the two groups of patients showed that P > 0.05 before treatment, meaning comparability. After treatment, two groups’ TCM symptom results were P < 0.05. After both treatment regimens, the TCM symptom scores were decreased, indicating that both treatment regimens improved symptoms such as pain and worsening of cold. After TG treatment, it was 16.01 ± 2.22. After CG treatment, it was 13.01 ± 2.21. The significant change in TCM symptom scores after TG treatment indicated that the treatment plan for TG could improve symptoms such as pain and worsening of cold compared to CG.
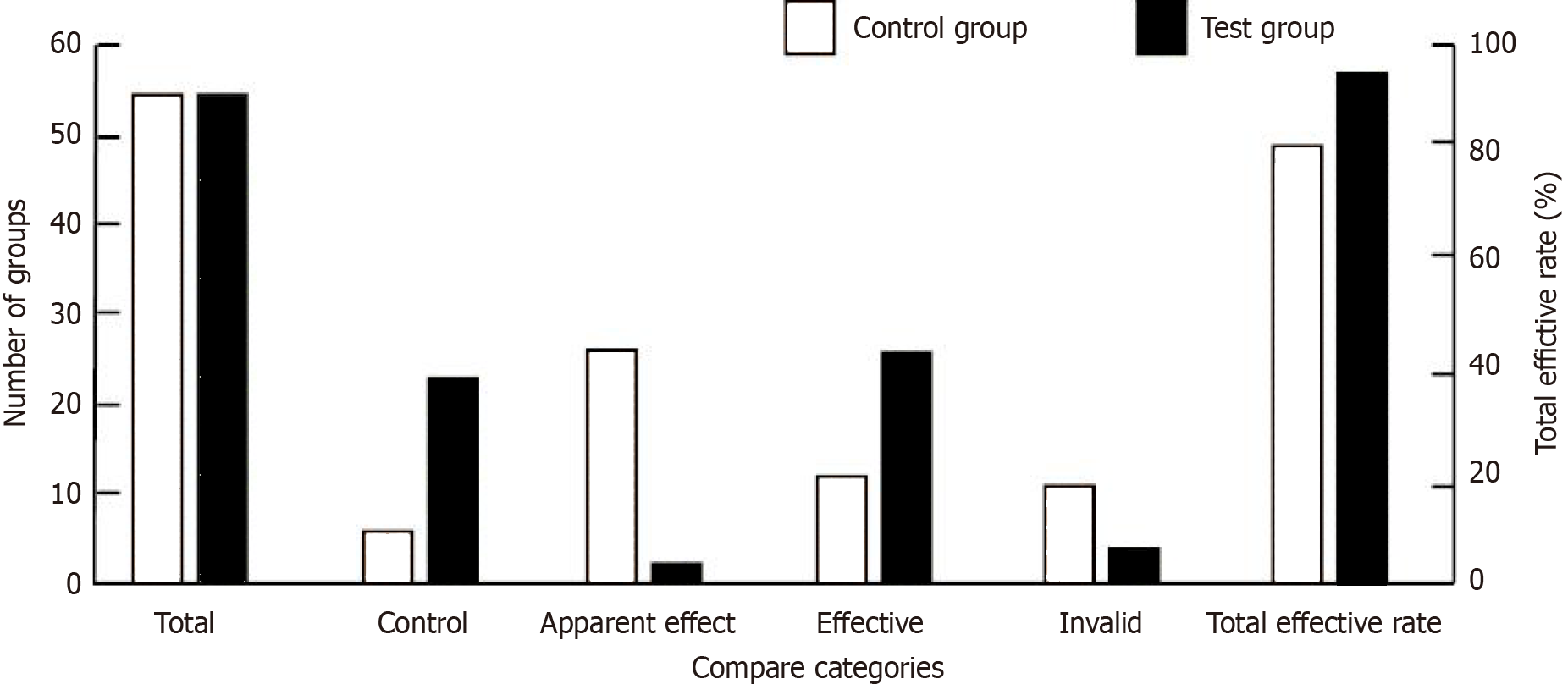
Figure 5 shows the clinical efficacy comparison of the 2 patients groups. In Figure 5, there was a significant gap in clinical efficacy between the two groups (P < 0.05). In Figure 5, the patients of CG were 55. Among them, there were 6 cases with controlled clinical efficacy, 26 cases with significant clinical efficacy, 12 cases with effective clinical efficacy, and 11 cases with ineffective clinical efficacy. The total effective rate of clinical efficacy was 80%. The patients of TG were 55. Among them, there were 23 cases with controlled clinical efficacy, 2 cases with significant clinical efficacy, 26 cases with effective clinical efficacy, and 4 cases with ineffective clinical efficacy. The effective rate of TG was significantly higher than that of CG, indicating that the combination of modified San Bi Tang and GSC treatment scheme had a better effect on improving the pain and joint performance of cold dampness type KO than the single treatment of GSC.
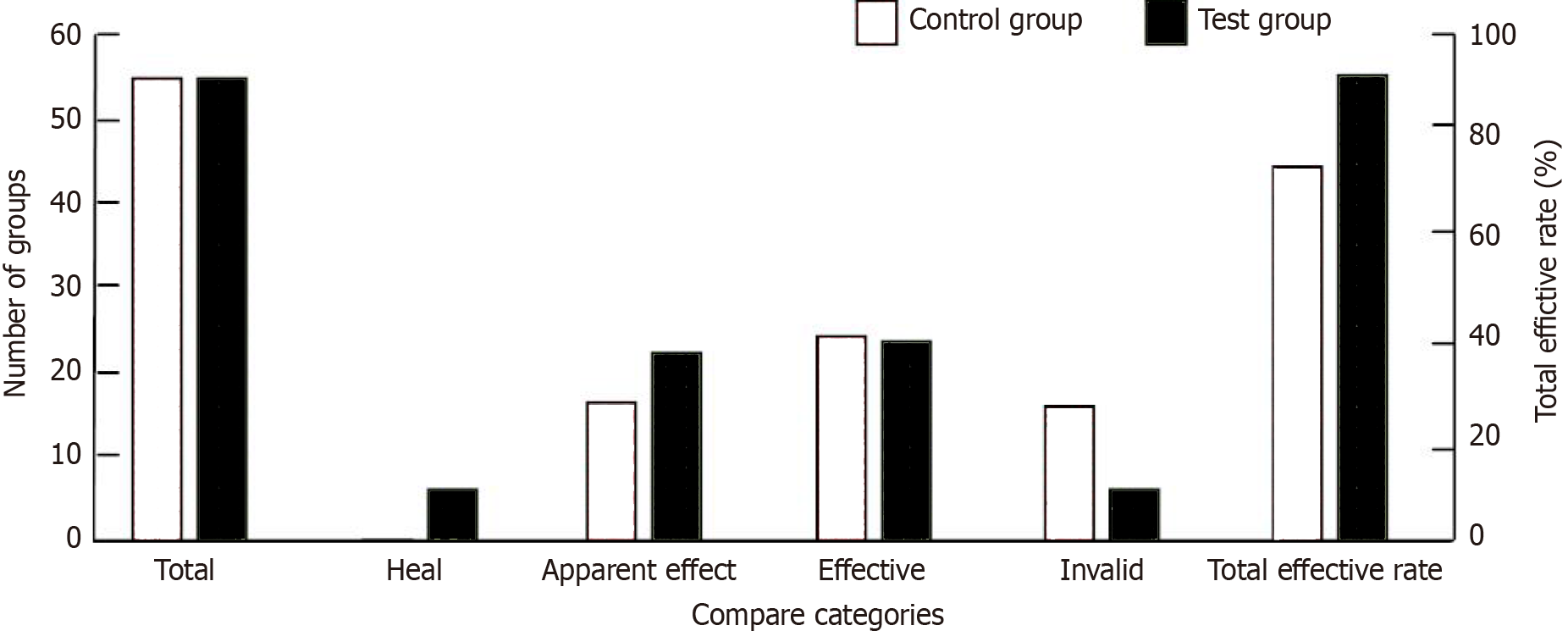
Figure 6 shows the TCM SE of patients. Two groups’ TCM SE had a significant difference (P < 0.05). In Figure 6, the patients of CG were 55. Among them, there were 0 cases with TCM SE being controlled, 16 cases with TCM SE being significantly effective, 24 cases with TCM SE being effective, and 15 cases with TCM SE being ineffective. The total effective rate of TCM SE was 72.73%. The patients of TG were 55. Among them, 5 cases were controlled by TCM SE, 22 were significantly effective, 23 effective, and 5 ineffective. The total effective rate of TCM SE was 90.91%. The effective rate of TG treatment was significantly higher than CG, indicating that the combination of San Bi Tang and GSC treatment scheme had a better improvement effect on the pain, joint performance, and worsening symptoms of cold dampness type KO than the use of GSC alone.
The vital signs of both groups in any stage of medication were normal. Table 6 manifests the average changes in liver-kidney functional indicator of patients. In Table 6, sequence number 1 represents pre-treatment indicator data, and sequence number 2 represents post treatment indicator data. Liver functional indicators have: AST, ALT, GGT, ALK, DBil, TP, ALB, TBil, and GLOB. Renal function examination indicators include BUN, Ccr, and UA. The various indicators of both groups of patients were basically within the normal range. No significant change found in liver-kidney function before and after treatment. It indicates that neither treatment regimen will have an impact on liver and kidney function, nor will it produce adverse reactions.
| Liver and kidney function indicators | Control group | Test group | ||||
| Before treatment | After treatment | P value | Before treatment | After treatment | P value | |
| ALT (U/L) | 32.23 ± 0.92 | 32.25 ± 1.03 | 0.9144 | 32.23 ± 3.62 | 33.36 ± 3.25 | 0.0849 |
| AST (U/L) | 29.36 ± 3.26 | 30.12 ± 2.36 | 0.1614 | 23.56 ± 2.35 | 24.02 ± 2.23 | 0.2923 |
| ALK (U/L) | 85.26 ± 9.23 | 88.24 ± 8.26 | 0.2358 | 86.24 ± 3.56 | 86.35 ± 2.51 | 0.8514 |
| GGT (U/L) | 36.25 ± 2.34 | 35.42 ± 2.45 | 0.069 | 35.16 ± 3.25 | 34.32 ± 3.12 | 0.1667 |
| DBil (μmol/L) | 3.26 ± 1.23 | 3.32 ± 0.25 | 0.7229 | 3.36 ± 2.01 | 3.02 ± 1.03 | 0.2642 |
| TBil (μmol/L) | 5.26 ± 3.25 | 6.23 ± 2.01 | 0.0059 | 6.34 ± 6.12 | 7.12 ± 5.21 | 0.4716 |
| TP (g/L) | 71.12 ± 1.22 | 71.23 ± 1.23 | 0.6377 | 71.36 ± 2.35 | 71.86 ± 1.02 | 0.1492 |
| ALB (g/L) | 42.36 ± 1.21 | 42.53 ± 1.02 | 0.4256 | 44.36 ± 2.31 | 45.26 ± 3.25 | 0.0942 |
| GLOB (mL/min) | 25.46 ± 3.26 | 26.34 ± 2.12 | 0.0933 | 26.34 ± 3.25 | 27.01 ± 3.21 | 0.2767 |
| Ccr (mmol/L) | 92.36 ± 5.24 | 93.14 ± 3.24 | 0.3478 | 91.02 ± 3.02 | 92.09 ± 3.26 | 0.0742 |
| BUN (μmol/L) | 6.35 ± 1.02 | 6.12 ± 1.11 | 0.2578 | 7.45 ± 1.85 | 7.03 ± 1.03 | 0.1413 |
| UA (μmol/L) | 263.26 ± 11.23 | 271.09 ± 31.02 | 0.0754 | 270.01 ± 9.26 | 272.89 ± 8.12 | 0.0828 |
The clinical features of cold dampness type KO mainly include joint cartilage damage, deformation, and detachment, accompanied by bone hyperplasia. It can cause degradation of knee joint movement. Among them, middle-aged women have a higher probability of developing the disease[9]. The secondary causes of KO include metabolic and endocrine factors, joint trauma and instability, and coagulation dysfunction. The primary causes include race, gender, age, weight, lifestyle, etc.[10]. Existing research shows that the incidence rate of KO in Europe is lower than that in Africa, and the incidence rate of KO in white people is lower than that in yellow people. It shows that there are differences in the incidence rate of KO among different races[11]. Some scholars found that the incidence rate of KO was related to gender. The incidence rate of females is higher than that of males. The main reason is that female estrogen can inhibit the influence of osteoclast[12]. A research team found that the KO incidence rate was positively correlated with age. The main reason is that the balance ability of muscles and bones decreases with age, and the imbalance of internal and external stress in the knee joint leads to joint cartilage degeneration and arthritis[13]. Relevant research showed that the higher the BMI index of the human body, the higher the KO incidence rate. The increase in body weight can increase the load on the knees, leading to accelerated cartilage degradation[14,15]. Modern medicine believes that genetic factors will affect the incidence rate of KO. Among twins, the inheritance of cartilage volume is 73%. In addition, researchers found that living environment, occupational habits, smoking, and drinking were also risky for KO.
The theory of articular cartilage degeneration was proposed in 1968. Pauwels believed that degenerative changes in articular cartilage were the fundamental cause of KO. The main reason is the metabolic imbalance between cartilage and subchondral bone. The synthesis and decomposition of articular cartilage are dynamically balanced under normal circumstances[16]. If the balance of factors is disrupted, the decomposition or synthesis of cartilage matrix increases or decreases. Cracking and degradation can lead to cartilage detachment, leading to KO. The theory of intraosseous hypertension suggests that subchondral intraosseous hypertension can cause bone marrow circulation to regress, reduce intraosseous blood flow and blood oxygen partial pressure, and result in insufficient nutrient supply to bone cells. Slow metabolism of bone cells leads to degenerative changes in the knee joint[17]. The theory of free radicals holds that oxygen free radicals are the foundation of cellular redox balance, ensuring the metabolic balance of osteoarticular chondrocytes. The repair of chondrocytes and tissues in KO patients is influenced by oxygen free radicals, which can also affect chondrocyte apoptosis and genetic material expression[18].
Pain reducing, disease progress delay, deformities correcting, and joint function enhancing are the main directions of KO treatment[19,20]. The current KO treatment is divided into phased and individualized treatment methods. Early treatment focuses on health promotion and exercise. In the mid-term, anti-inflammatory-drugs and articular cartilage-nutrition drugs are the main treatment drugs. Patients with advanced functional impairments mainly use surgical treatment to improve their joint status. Early treatment methods mainly include exercise therapy and physical assisted therapy. Studies have shown that health education and other guidance can help improve patients' daily life, knee joint, and life quality. In the development of KO, the role of the quadriceps femoris muscle is to stabilize the structure of the knee joint and the knee extension device. The straight leg lifting exercise of quadriceps femoris muscle contributes to the improvement of knee joint function. Proper exercise with mobility aids can reduce the weight bearing capacity of the knee joint. Direct stimulation of the body can accelerate blood circulation and reduce knee joint pain in patients. Physical therapy typically includes ultrasound, hydrotherapy, and hyperthermia. Research has shown that the pain and physical function of KO patients can be improved through hydrotherapy.
Oral and injectable western medicine treatments can alleviate pain in KO patients. Joint cartilage nutrients is a common oral medication. Anti-inflammatory drugs can have anti-inflammatory and analgesic effects, effectively relieving pain in KO patients. However, its adverse reactions to the digestive tract are not suitable for the treatment of gastritis patients. The representative of joint cartilage nutrients is GSC, which improves the supply of cartilage nutrients and alleviates the progression of KO. However, the analgesic effect is not significant, and the combination of anti-inflammatory drugs and nutrients can alleviate symptoms. Sodium hyaluronate and platelet rich plasma are common injectable drugs. A study has shown that one month of sodium hyaluronate treatment is the optimal treatment time, and the treatment effect can be maintained for 3 years. Platelet rich plasma helps patients with exercise rehabilitation. In early KO patients such as athletes, platelet rich plasma treatment has a better effect. The final treatment for KO is surgery. When it is difficult to achieve pain relief or joint correction in conservative treatment, surgery can be chosen for treatment. Surgical treatment can be divided into arthroscopic debridement, osteotomy, and artificial joint replacement. Mid to late stage patients usually undergo arthroscopic debridement surgery. Its advantages include minimal trauma, fast recovery, and fewer complications. Osteotomy can correct lower limb deformities and lower limb force lines to reduce patient pain. The final treatment method for advanced KO patients is artificial joint replacement surgery, which has a high risk index and high cost.
Joint cartilage injury is the main pathological feature of KO. The protection of articular cartilage is crucial for treatment and prevention. GSC is usually extracted from the cartilage of deep-sea sharks or natural shrimp and crab shells. Generally, it is a polymer glycan belonging to cartilage proteins, containing polysaccharides and collagen fibers. It is an important substance for repairing and generating cartilage matrix, which can promote the formation of joint synovial fluid and has a certain anti-inflammatory effect. It can absorb and maintain moisture in cartilage, lubricate joints, and remove debris from joints. It can effectively alleviate knee pain, swelling, and stiffness. It is called joint soft butter and can also effectively treat and prevent osteoarthritis. The human body absorbs glucosamine sulfate better than hydrochloric acid-based glucosamine, and the repair effect will be stronger.
The principle of TCM treatment for knee joint syndrome is nourishing the kidney-liver internally and disperse wind, cold, and dampness pathogenic factors externally. Modern Chinese medicine is mainly treated by taking medicine orally, supplemented by acupuncture and moxibustion, massage and other exercises, and combined with a variety of treatment methods to build a comprehensive treatment system. The most common treatment method in TCM is oral administration of TCM decoction. Dialectical treatment with drugs for promoting blood circulation and resolving stasis, as well as tonifying qi and blood, can be used according to different clinical manifestations. The medicinal properties of Heracleum hemsleyanum Diels in San Bi Tang are pungent, bitter, and dry, commonly used in rheumatism and pain treatment. Related studies have shown that the main component of Heracleum hemsleyanum Diels, volatile oil, can be anti-inflammatory and analgesic. Various drugs of San Bi Tang can help improve bone cell proliferation, inhibit joint inflammation, and alleviate pain. It is mainly used for the treatment of orthopedic arthritis and shoulder periarthritis.
In this study, 110 KO patients underwent 5 wk of treatment and were evaluated for pain using VAS score. WOMAC score evaluates the pain, stiffness, and activity of the patients. Knee joint function was evaluated by sitting up times within 30 s, and the efficacy of TCM was evaluated based on the TCM symptom score table. The research results showed that under both treatment regimens, the VAS and WOMAC scores of patients decreased, while the 30CST score improved. It indicates that the combination of modified San Bi Tang and GSC treatment has a better effect. The clinical efficacy and TCM symptoms of both groups of patients are relatively obvious. The effective rate of TG is higher CG. It indicates that the combination of modified San Bi Tang and GSC treatment has a better effect on improving pain, joint function, and exacerbation of cold in patients than simple glucosamine sulfate treatment. The research found that the combination of modified San Bi Tang and GSC had significant therapeutic effects on cold dampness type KO. In terms of pain, joint function, and TCM symptoms, the improvement degree of the experimental group patients was better than that of CG. In addition, the clinical efficacy and overall effectiveness rate of TCM syndrome efficacy in the experimental group were higher than those in CG. These results indicated that the combination of TCM and western medicine had significant advantages in treating cold dampness type KO. The research results are consistent with existing literature on the combined treatment of TCM and western medicine for KO[21]. For example, a randomized controlled trial on the combined treatment of TCM and western medicine for KO found that the combined treatment group was superior to the simple western medicine treatment group in terms of pain, joint function, and quality of life[22]. Another study found that the combination of TCM and western medicine significantly improved pain and joint stiffness symptoms in patients with arthritis and improved their quality of life[23]. These research results indicated that the combination of TCM and western medicine had significant therapeutic effects on KO. However, there are certain differences between the research and the aforementioned literature in terms of treatment methods, research subjects, and efficacy evaluation. The study used modified San Bi Tang combined with GSC for treatment, while other studies used different integrated TCM and western medicine treatment. This study confirmed the therapeutic advantages of combining TCM and western medicine in treating cold dampness type KO, providing new ideas for clinical treatment. With the aggravation of the aging society, the incidence rate of KO is gradually rising, which has brought a heavy burden to patients and society. Integrated TCM and western medicine treatment, as a safe and effective treatment method, is expected to alleviate the pain of patients and improve their quality of life. Future research can expand the sample size and conduct multi-center and large sample randomized controlled trials to confirm the universality of the results of this study.
The study concludes that the combination of modified San Bi Tang and GSC has a better effect in improving pain, joint function, and exacerbation of cold in patients with cold dampness type KO compared to simple glucosamine sulfate treatment. The results showed that both treatment regimens decreased VAS and WOMAC scores and improved 30CST scores, indicating the improvement in pain, joint function, and knee joint performance. The clinical efficacy and TCM symptoms were significantly better in the combined treatment group, with a higher overall effectiveness rate of TCM syndrome efficacy. The study provides evidence for the therapeutic advantages of combining TCM and western medicine in treating cold dampness type KO, offering new insights for clinical practice and further research.
| 1. | Deane KD, Holers VM. Rheumatoid Arthritis Pathogenesis, Prediction, and Prevention: An Emerging Paradigm Shift. Arthritis Rheumatol. 2021;73:181-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 157] [Article Influence: 39.3] [Reference Citation Analysis (0)] |
| 2. | Ytterberg SR, Bhatt DL, Mikuls TR, Koch GG, Fleischmann R, Rivas JL, Germino R, Menon S, Sun Y, Wang C, Shapiro AB, Kanik KS, Connell CA; ORAL Surveillance Investigators. Cardiovascular and Cancer Risk with Tofacitinib in Rheumatoid Arthritis. N Engl J Med. 2022;386:316-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 958] [Article Influence: 319.3] [Reference Citation Analysis (0)] |
| 3. | Allen KD, Thoma LM, Golightly YM. Epidemiology of osteoarthritis. Osteoarthritis Cartilage. 2022;30:184-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 422] [Article Influence: 140.7] [Reference Citation Analysis (0)] |
| 4. | Sharma L. Osteoarthritis of the Knee. N Engl J Med. 2021;384:51-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 574] [Article Influence: 143.5] [Reference Citation Analysis (0)] |
| 5. | Hunter DJ, March L, Chew M. Osteoarthritis in 2020 and beyond: a Lancet Commission. Lancet. 2020;396:1711-1712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 489] [Article Influence: 97.8] [Reference Citation Analysis (0)] |
| 6. | Katz JN, Arant KR, Loeser RF. Diagnosis and Treatment of Hip and Knee Osteoarthritis: A Review. JAMA. 2021;325:568-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 634] [Cited by in RCA: 1202] [Article Influence: 300.5] [Reference Citation Analysis (0)] |
| 7. | Arden NK, Perry TA, Bannuru RR, Bruyère O, Cooper C, Haugen IK, Hochberg MC, McAlindon TE, Mobasheri A, Reginster JY. Non-surgical management of knee osteoarthritis: comparison of ESCEO and OARSI 2019 guidelines. Nat Rev Rheumatol. 2021;17:59-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 298] [Article Influence: 59.6] [Reference Citation Analysis (0)] |
| 8. | Aubourg G, Rice SJ, Bruce-Wootton P, Loughlin J. Genetics of osteoarthritis. Osteoarthritis Cartilage. 2022;30:636-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 82] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 9. | Quicke JG, Conaghan PG, Corp N, Peat G. Osteoarthritis year in review 2021: epidemiology & therapy. Osteoarthritis Cartilage. 2022;30:196-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 218] [Article Influence: 72.7] [Reference Citation Analysis (0)] |
| 10. | Whittaker JL, Runhaar J, Bierma-Zeinstra S, Roos EM. A lifespan approach to osteoarthritis prevention. Osteoarthritis Cartilage. 2021;29:1638-1653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 11. | Jiang Y. Osteoarthritis year in review 2021: biology. Osteoarthritis Cartilage. 2022;30:207-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 134] [Article Influence: 44.7] [Reference Citation Analysis (0)] |
| 12. | Whittaker JL, Truong LK, Dhiman K, Beck C. Osteoarthritis year in review 2020: rehabilitation and outcomes. Osteoarthritis Cartilage. 2021;29:190-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 51] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 13. | Sanchez-Lopez E, Coras R, Torres A, Lane NE, Guma M. Synovial inflammation in osteoarthritis progression. Nat Rev Rheumatol. 2022;18:258-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 363] [Cited by in RCA: 486] [Article Influence: 162.0] [Reference Citation Analysis (0)] |
| 14. | Zhang H, Cai D, Bai X. Macrophages regulate the progression of osteoarthritis. Osteoarthritis Cartilage. 2020;28:555-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 327] [Article Influence: 65.4] [Reference Citation Analysis (0)] |
| 15. | Saleki M, Ahadi T, Razi M, Raeisi GR, Forough B, Ali MK. Comparison of the effects of acupuncture and isometric exercises on symptom of knee osteoarthritis. Int J Prev Med. 2013;4:S73-S77. [PubMed] |
| 16. | Veronese N, Ecarnot F, Cheleschi S, Fioravanti A, Maggi S. Possible synergic action of non-steroidal anti-inflammatory drugs and glucosamine sulfate for the treatment of knee osteoarthritis: a scoping review. BMC Musculoskelet Disord. 2022;23:1084. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 17. | Torshin IY, Lila AM, Gromova OA. Hepatoprotective effects of chondroitin sulfate and glucosamine sulfate. Farmakoèkonomika. 2022;14:537-547. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Golshayan NS, Karbasi S, Masaeli E, Bahremandi-toloue E, Nasr-esfahani MH, Rafienia M. Evaluation of the effects of glucosamine sulfate on poly (3- hydroxybutyrate) -chitosan/carbon nanotubes electrospun scaffold for cartilage tissue engineering applications. Polymer-Plastics Technology and Materials. 2022;61:1244-1264. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Torshin IY, Gromova ОA, Lila AM. Prospects for the use of chondroitin sulfate and glucosamine sulfate in the treatment of patients with obesity-associated osteoarthritis (metabolic syndrome). Farmakoèkonomika. 2022;15:390-401. [DOI] [Full Text] |
| 20. | Richard MJ, Driban JB, McAlindon TE. Pharmaceutical treatment of osteoarthritis. Osteoarthritis Cartilage. 2023;31:458-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 108] [Article Influence: 54.0] [Reference Citation Analysis (0)] |
| 21. | Holden MA, Nicolson PJA, Thomas MJ, Corp N, Hinman RS, Bennell KL. Osteoarthritis year in review 2022: rehabilitation. Osteoarthritis Cartilage. 2023;31:177-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 22. | El-ghany SA, Elmogy M, El-aziz AAA. A fully automatic fine tuned deep learning model for knee osteoarthritis detection and progression analysis. Egyptian Informatics Journal. 2023;24:229-240. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 23. | Lawford BJ, Bennell KL, Hall M, Egerton T, Filbay S, McManus F, Lamb KE, Hinman RS. Removing Pathoanatomical Content From Information Pamphlets About Knee Osteoarthritis Did Not Affect Beliefs About Imaging or Surgery, but Led to Lower Perceptions That Exercise Is Damaging and Better Osteoarthritis Knowledge: An Online Randomised Controlled Trial. J Orthop Sports Phys Ther. 2023;53:1-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |