Published online Jun 26, 2024. doi: 10.12998/wjcc.v12.i18.3609
Revised: April 28, 2024
Accepted: May 13, 2024
Published online: June 26, 2024
Processing time: 100 Days and 21.7 Hours
Parathyroid carcinoma (PC) is a difficult-to-diagnose rare disease with low inci
This study reported the clinical diagnosis and treatment of a rare patient with PC located in the thyroid gland and provided a case reference for the diagnosis and treatment of PC. A case of a 64-year-old male patient who presented to our hos
The intraoperative frozen section report considered the parathyroid tumor. Surgical tumor resection was promptly performed, and the diagnosis of PC was confirmed.
Core Tip: Parathyroid carcinoma (PC) is a difficult-to-diagnose rare disease with low incidence. Relatively accurate preoperative diagnosis is very important in choosing surgical methods and patient prognosis. This study reported a rare patient with PC located in the thyroid gland. Combined with the results of color thyroid ultrasound and intraoperative frozen section, the primary disease of the patient can be confirmed. Accurate preoperative diagnosis is helpful for timely surgical resection of the tumor and improving the therapeutic effect.
- Citation: Gui SY, Zhang CN, Ling L, Tang RX, Yang J. Parathyroid carcinoma located in the thyroid gland: A case report. World J Clin Cases 2024; 12(18): 3609-3614
- URL: https://www.wjgnet.com/2307-8960/full/v12/i18/3609.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i18.3609
Parathyroid carcinoma (PC) is a rare malignant tumor with a relatively low incidence, accounting for < 1% of primary hyperparathyroidism[1]. PC due to ectopic third and fourth parotid glands during embryonic development is even rare, accounting for about 0.2%[2,3]. This case report presents the clinical diagnosis and treatment of a rare intrathyroidal PC.
A 64-year-old male patient presented to the Cardiology Department of our hospital because of “palpitations” that started 2 d before the presentation.
Six months ago, the patient developed systemic arthralgia and bone pain without obvious inducement, which could be relieved after resting at first and then became worse, accompanied by limb muscle weakness, dry mouth, polyuria and polydipsia, occasional nausea, and no obvious vomiting or abdominal distension. Half a month ago, he presented to the orthopedic outpatient department of our hospital and was administered joint nutrition drugs; however, his symptoms were not significantly relieved.
The patient had a 15-year history of hypertension and had stopped taking irbesartan for nearly 6 months, with normal blood pressure.
The patient had a no family history.
Physical examination results showed a 4 cm × 5 cm mass in the left lobe of the thyroid gland, which was hard and moved with swallowing. Other examination results were normal.
The detection value of cytokeratin 19 fragment was 5.29 ng/mL (normal value < 5.0), and the parathyroid hormone (PTH) value was > 346.90 pmol/L. The blood calcium and 24-h urine calcium values were higher than the normal reference range. Serum creatinine of 241.3 umol/L, uric acid of 573 umol/L, and calcium of 3.76 mmol/L were all higher than the normal range. The outpatient doctor considered “renal insufficiency and multiple myeloma nephropathy pending investigation” and admitted the patient to the nephrology department for calcitonin and furosemide treatment.
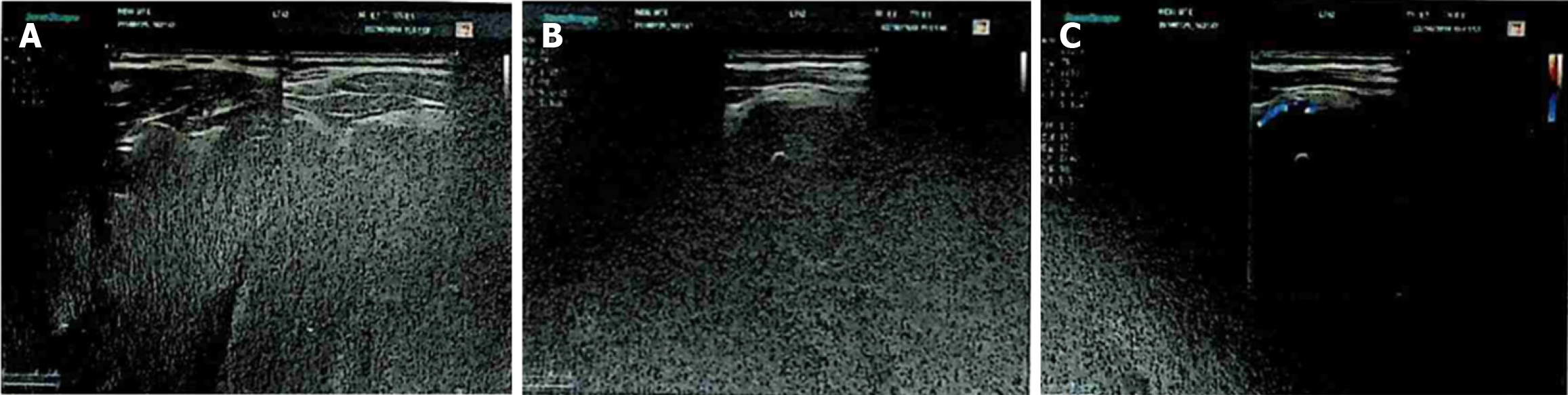
Colored ultrasonography of the patient’s thyroid and cervical lymph nodes showed a cystic solid mass (mostly solid, possibly with calcification) in the left lobe of the thyroid gland (Figure 1), which was considered “primary hyperparathyroidism and hypercalcemic crisis”.
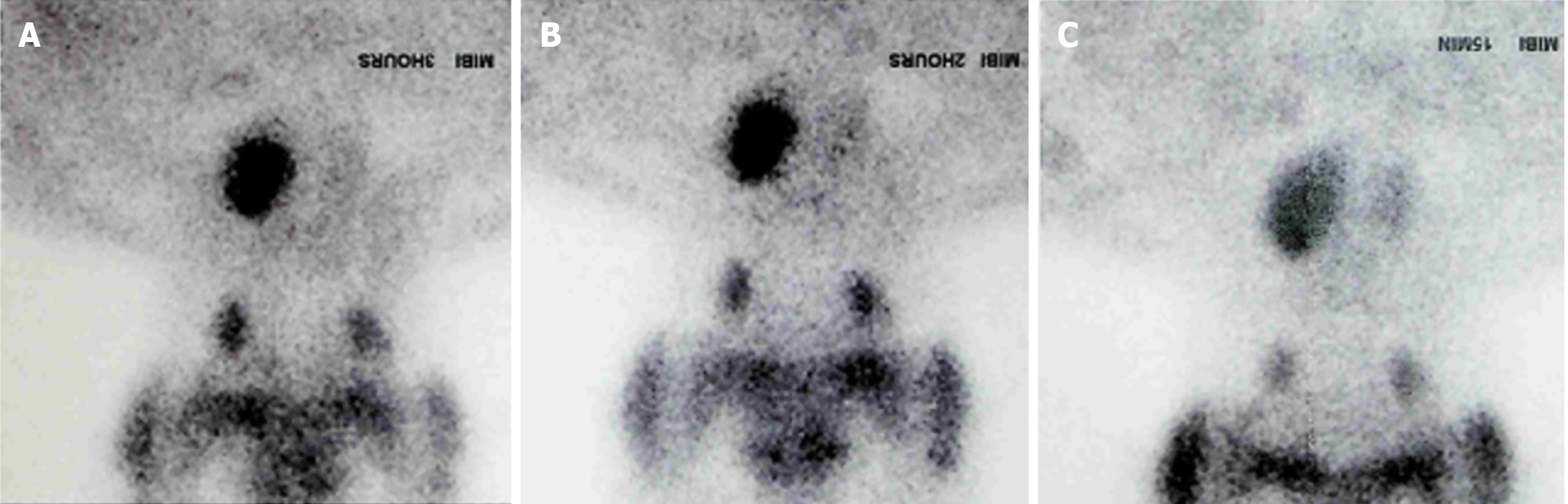
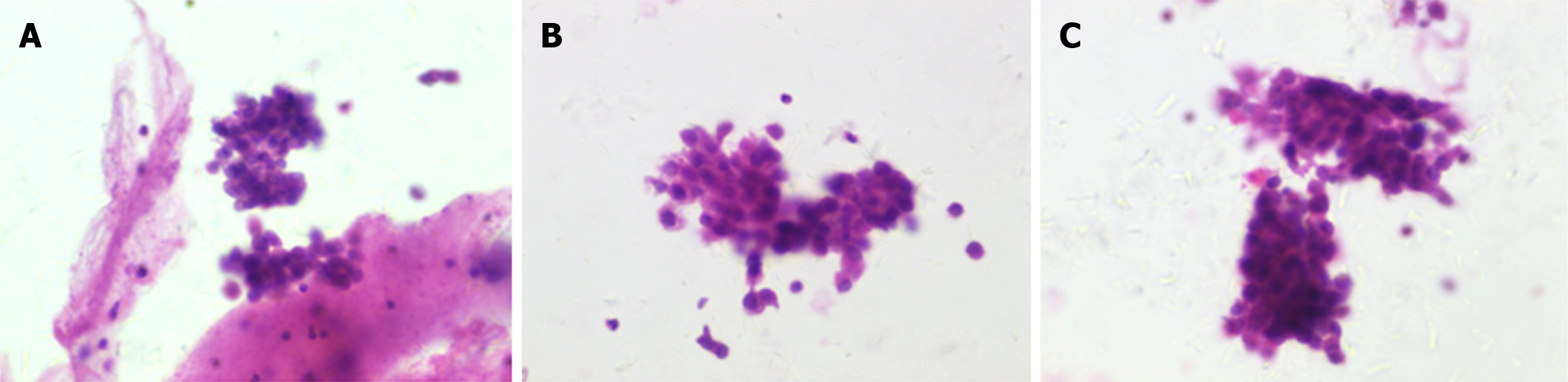
Parathyroid scintigraphy (MIBI) revealed a concentration shadow of radioactivity in the left lobe of the thyroid gland (Figure 2). Fine needle aspiration (FNA) cytological smear of thyroid nodules suggested the possibility of papillary thyroid carcinoma (Figure 3).
The final diagnosis of the presented case is parathyroid adenoma.
The patient was initially diagnosed with hypercalcemic crisis and primary hyperparathyroidism, with the possibility of parathyroid adenoma (PA). Patients were treated with diuretics and calcitonin (calcitonin, 100iu, q6h). After the diagnosis, parathyroid tumor resection under general anesthesia + left thyroid isthmus resection + tissue lymph node resection and biopsy of left central cervical tissue were performed. Intraoperative exploration showed an elevated left lobe of the thyroid gland, and a mass of 3.5 cm × 3 cm in size was palpable behind the bulge, with unclear boundary, complete capsule, and hard quality. No obvious mass was found in the right lobe of the thyroid gland, and no enlarged lymph nodes were found locally and beside the cervical vascular sheath. Considering that the left parathyroid tumor was integrated with the left thyroid lobe, parathyroid tumor resection + left thyroid lobe and isthmus resection was finally performed. Intraoperative frozen section report considered a parathyroid tumor.
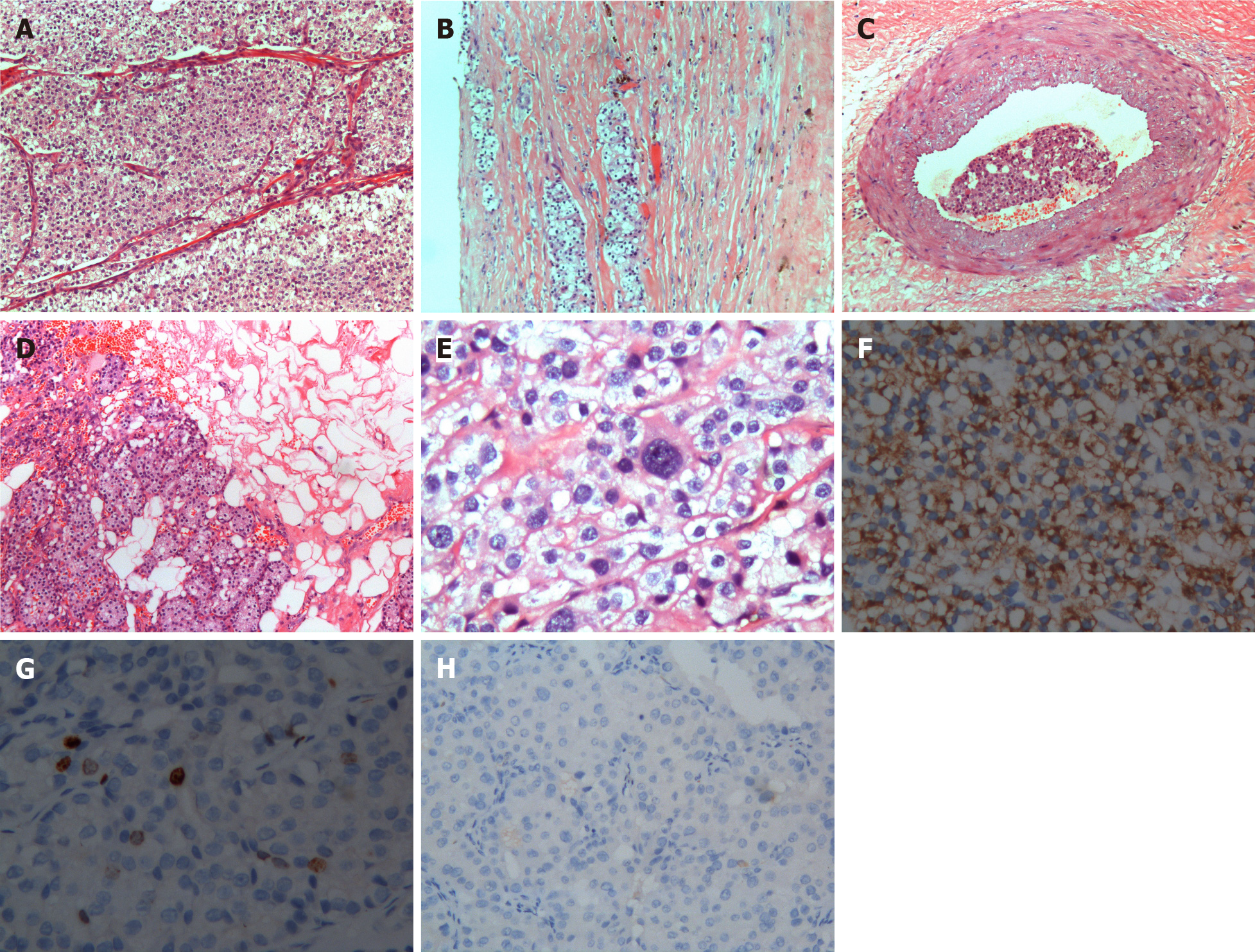
The serum PTH and calcium indexes decreased to normal values post-resection. The results of the postoperative pathological examination showed that the tumor presented multiple nodules of varying sizes, with abundant interstitial blood vessels, and irregular ribbon-like collagen fibers in the tumor, which were intermittently distributed and crisscrossed (Figure 4A). Simultaneously, pathological examination revealed tumor invasion or breakthrough of the capsule (Figure 4B), vascular and fat invasion (Figure 4C and D), and heterocyst (Figure 4E). Immunohistochemistry showed that PTH was diffusely positive (Figure 4F), with approximately 1% of tumor cells positive for Ki-67 (Figure 4G), and calcitonin staining was negative (Figure 4H).
Since Armstrong first reported cases of PC in 1938, about 700 cases of PC have been reported, and only 11 cases of PC located in the thyroid gland have been clearly reported in the literature[4,5]. The clinical symptoms and signs of PC are mainly associated with hypercalcemia caused by primary hyperparathyroidism, recurrent urinary calculus, osteoporosis, pathological fractures, and gastrointestinal and neuropsychiatric symptoms. However, the differentiation between PA and PC is difficult because clinical and laboratory indicators are not specific. Patients with PC usually have higher blood calcium (usually > 14–15 mg/dL) and PTH levels that can exceed the upper normal limit more than 3 to 10 times. On the contrary, PA usually causes only mild to moderate increases in blood calcium and PTH levels[6]. Some studies have found that serum and urine HCG and its highly glycated isomers are abnormally elevated in patients with PC, but not in those with PA; however, more clinical studies are still needed to confirm this[7]. Neck color ultrasonography and MIBI imaging are the first choice for localization diagnosis of parathyroid diseases, which can distinguish and identify normal and ectopic parathyroid tissues, as well as recurrent parathyroid disease, but does not have the specificity to distinguish benign from malignant tumors[8]. CT and magnetic resonance imaging can accurately locate primary tumors and recurrent lesions, which help detect smaller lesions and assess the adhesion and invasion of surrounding tissues and lymph node metastasis.
With the increasing application of FNA in thyroid lesions, B-ultrasound-guided FNA is also of diagnostic value in the clinical suspicion of parathyroid disease. However, because the cytological features of parathyroid and thyroid lesions have many similarities, the parathyroid lesions with FNA in neck masses may be confused with thyroid tumors, especially for parathyroid tissues heterolocated in the thyroid gland, which is more difficult to distinguish. For example, in our case, the cell smear examination indicated papillary thyroid carcinoma after cervical mass FNA. When cytological smear examination alone still cannot distinguish thyroid lesions from parathyroid lesions, the parathyroid hormone indicators can be detected and evaluated with FNA fluid guided by B-ultrasound to help determine the nature of neck lesions, improve the accuracy of B-ultrasound imaging of parathyroid glands, and successfully guide the operation of patients[9-13]. PTH levels were measured in the puncture fluid diluted with saline, and intact plasma PTH levels were measured. The lesion was defined as a parathyroid gland when the PTH concentration in the parathyroid fine-needle biopsy sample was higher than the serum PTH level. The sensitivity and specificity of PTH elution determination by parathyroid fine-needle puncture were 95.5% and 100%[14]. In this case, FNA was performed on the left neck nodule under the B-ultrasound guidance. The cytological smear of FNA suggested the possibility of papillary thyroid cancer. However, the PTH measured when we performed the puncture fluid elution was significantly higher than 3460.90 pmol/L, the PTH measured by contralateral thyroid FNA was 103.40 pmol/L, and the synchronous serum PTH was > 349.6 pmol/L. Therefore, even though the FNA cytological smear at the time suggested the possibility of papillary thyroid cancer, the lesion was still highly suspected to be PC. The patient was advised to undergo surgical treatment as soon as possible, and postoperative pathological results confirmed PC (Figure 4).
PTH elution measurement is a simple and effective method to guide surgeons in the preoperative localization of parathyroid tumors. However, no unified standard and specification has been established. PC is mainly diagnosed by pathologists intra- and postoperatively. Pathologic diagnosis of PC is often difficult. About 80% of PC tumors are well differentiated. Moreover, distinguishing PA from PC based on histomorphological criteria and even from parathyroid gland cells from thyroid cells, was difficult. In this case, the patient was easily misdiagnosed with papillary thyroid cancer. The accuracy of the diagnosis largely depends on the experience of the pathologist. At present, scholars at home and abroad are experiencing difficulties in relying on intraoperative frozen sections to diagnose PC. Immunohistochemistry of tissue sections will be helpful for the diagnosis of PC, and the Ki-67 and cyclin D1 expression will be increased in PC[15]. The decreased P27 expression and increased galectin-3 expression, as well as their association with Ki-67 labeling, help determine the likelihood of malignancy[16]. The CDC73 gene mutation and paraibromin chromosome deletion will also help diagnose PC in the case of ambiguous clinical diagnosis[15,17,18].
The diagnosis of PC is difficult but extremely important. The most effective treatment for PC is surgery, which is not sensitive to chemotherapy or radiation. The prognosis of PC greatly varies, with a recurrence rate of > 50% in 2–3 years postoperatively and 33%–82% in 5 years[19]. In the early operation, standard en bloc resection can be performed with good results, which can provide the best chance of cure and long-term survival for patients[20]. Therefore, the early diagnosis of PC, which can even provide clues of PC preoperatively, will have a significant impact on the choice of surgical methods and the prognosis of patients.
We would like to thank all the authors and relevant staff who have contributed to this study.
| 1. | Kumari N, Mishra D, Pradhan R, Agarwal A, Krishnani N. Utility of fine-needle aspiration cytology in the identification of parathyroid lesions. J Cytol. 2016;33:17-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Harach HR, Vujanić GM. Intrathyroidal parathyroid. Pediatr Pathol. 1993;13:71-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Vila Duckworth L, Winter WE, Vaysberg M, Moran CA, Al-Quran SZ. Intrathyroidal parathyroid carcinoma: report of an unusual case and review of the literature. Case Rep Pathol. 2013;2013:198643. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Tejera Hernández AA, Gutiérrez Giner MI, Vega Benítez V, Fernández San Millan D, Hernández Hernández JR. Intrathyroidal parathyroid carcinoma. A case report and review of literature. Endocrinol Nutr. 2016;63:46-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Balakrishnan M, George SA, Rajab SH, Francis IM, Kapila K. Cytological challenges in the diagnosis of intrathyroidal parathyroid carcinoma: A case report and review of literature. Diagn Cytopathol. 2018;46:47-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Marcocci C, Cetani F. Clinical practice. Primary hyperparathyroidism. N Engl J Med. 2011;365:2389-2397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 210] [Article Influence: 15.0] [Reference Citation Analysis (33)] |
| 7. | Rubin MR, Bilezikian JP, Birken S, Silverberg SJ. Human chorionic gonadotropin measurements in parathyroid carcinoma. Eur J Endocrinol. 2008;159:469-474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Sidhu PS, Talat N, Patel P, Mulholland NJ, Schulte KM. Ultrasound features of malignancy in the preoperative diagnosis of parathyroid cancer: a retrospective analysis of parathyroid tumours larger than 15 mm. Eur Radiol. 2011;21:1865-1873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Barczynski M, Golkowski F, Konturek A, Buziak-Bereza M, Cichon S, Hubalewska-Dydejczyk A, Huszno B, Szybinski Z. Technetium-99m-sestamibi subtraction scintigraphy vs. ultrasonography combined with a rapid parathyroid hormone assay in parathyroid aspirates in preoperative localization of parathyroid adenomas and in directing surgical approach. Clin Endocrinol (Oxf). 2006;65:106-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 65] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Owens CL, Rekhtman N, Sokoll L, Ali SZ. Parathyroid hormone assay in fine-needle aspirate is useful in differentiating inadvertently sampled parathyroid tissue from thyroid lesions. Diagn Cytopathol. 2008;36:227-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 34] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Popowicz B, Klencki M, Sporny S, Jankiewicz-Wika J, Komorowski J, Pisarek H, Słowińska-Klencka D. Usefulness of PTH measurements in FNAB washouts in the identification of pathological parathyroids--analysis of the factors that influence the effectiveness of this method. Endokrynol Pol. 2014;65:25-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Abdelghani R, Noureldine S, Abbas A, Moroz K, Kandil E. The diagnostic value of parathyroid hormone washout after fine-needle aspiration of suspicious cervical lesions in patients with hyperparathyroidism. Laryngoscope. 2013;123:1310-1313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Kuzu F, Arpaci D, Cakmak GK, Emre AU, Elri T, Ilikhan SU, Bahadir B, Bayraktaoglu T. Focused parathyroidectomy without intra-operative parathormone monitoring: The value of PTH assay in preoperative ultrasound guided fine needle aspiration washout. Ann Med Surg (Lond). 2016;6:64-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Ozderya A, Temizkan S, Cetin K, Ozugur S, Gul AE, Aydin K. The results of parathyroid hormone assay in parathyroid aspirates in pre-operative localization of parathyroid adenomas for focused parathyroidectomy in patients with negative or suspicious technetium-99m-sestamibi scans. Endocr Pract. 2017;23:1101-1106. [PubMed] [DOI] [Full Text] |
| 15. | Cetani F, Ambrogini E, Viacava P, Pardi E, Fanelli G, Naccarato AG, Borsari S, Lemmi M, Berti P, Miccoli P, Pinchera A, Marcocci C. Should parafibromin staining replace HRTP2 gene analysis as an additional tool for histologic diagnosis of parathyroid carcinoma? Eur J Endocrinol. 2007;156:547-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 90] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 16. | Wang O, Wang CY, Shi J, Nie M, Xia WB, Li M, Jiang Y, Guan H, Meng XW, Xing XP. Expression of Ki-67, galectin-3, fragile histidine triad, and parafibromin in malignant and benign parathyroid tumors. Chin Med J (Engl). 2012;125:2895-2901. [PubMed] |
| 17. | Guarnieri V, Battista C, Muscarella LA, Bisceglia M, de Martino D, Baorda F, Maiello E, D'Agruma L, Chiodini I, Clemente C, Minisola S, Romagnoli E, Corbetta S, Viti R, Eller-Vainicher C, Spada A, Iacobellis M, Malavolta N, Carella M, Canaff L, Hendy GN, Cole DE, Scillitani A. CDC73 mutations and parafibromin immunohistochemistry in parathyroid tumors: clinical correlations in a single-centre patient cohort. Cell Oncol (Dordr). 2012;35:411-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 60] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 18. | Wang O, Wang C, Nie M, Cui Q, Guan H, Jiang Y, Li M, Xia W, Meng X, Xing X. Novel HRPT2/CDC73 gene mutations and loss of expression of parafibromin in Chinese patients with clinically sporadic parathyroid carcinomas. PLoS One. 2012;7:e45567. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 19. | Cetani F, Pardi E, Marcocci C. Parathyroid Carcinoma. Front Horm Res. 2019;51:63-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 74] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 20. | Fang SH, Lal G. Parathyroid cancer. Endocr Pract. 2011;17 Suppl 1:36-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |