Published online Jun 26, 2024. doi: 10.12998/wjcc.v12.i18.3314
Revised: April 11, 2024
Accepted: May 10, 2024
Published online: June 26, 2024
Processing time: 106 Days and 22.3 Hours
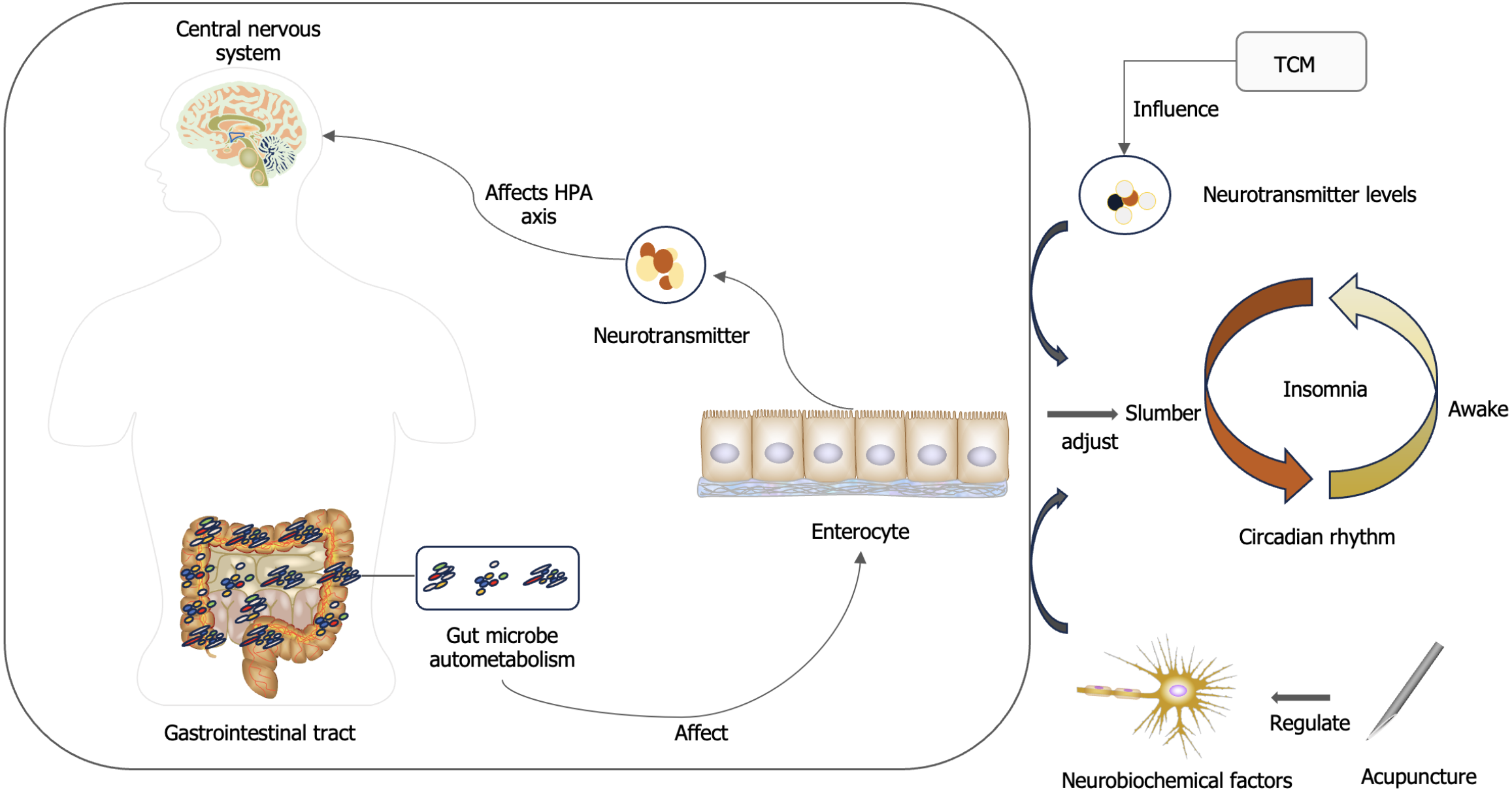
Insomnia, as one of the emotional diseases, has been increasing in recent years, which has a great impact on people's life and work. Therefore, researchers are eager to find a more perfect treatment. The microbiome-gut-brain axis is a new theory that has gradually become popular abroad in recent years and has a profound impact in the field of insomnia. In recent years, traditional Chinese medicine (TCM) has played an increasingly important role in the treatment of insomnia, especially acupuncture and Chinese herbal medicine. It is the main method of TCM in the treatment of insomnia. This paper mainly reviews the combination degree of "microorganism-gut-brain axis" theory with TCM and acupuncture under the system of TCM. To explore the mechanism of TCM and acupuncture in the treatment of insomnia under the guidance of "microorganism-gut-brain axis" theory, in order to provide a new idea for the diagnosis and treatment of insomnia.
Core Tip: In recent years, traditional Chinese medicine (TCM) has played an increasingly important role in the treatment of insomnia, especially acupuncture and Chinese herbal medicine. It is the main method of TCM in the treatment of insomnia. This paper mainly reviews the combination degree of "microorganism-gut-brain axis" theory with TCM and acupuncture under the system of TCM. To explore the mechanism of TCM and acupuncture in the treatment of insomnia under the guidance of "microorganism-gut-brain axis" theory, in order to provide a new idea for the diagnosis and treatment of insomnia.
- Citation: Pan LM, Hong ZB, Guan RQ. Research progress on insomnia treated by traditional Chinese medicine and acupuncture based on microbial-gut-brain axis theory. World J Clin Cases 2024; 12(18): 3314-3320
- URL: https://www.wjgnet.com/2307-8960/full/v12/i18/3314.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i18.3314
Insomnia is a disease characterized by difficulty in falling asleep, difficulty in maintaining sleep and awakening in the morning and non-restorative sleep, accompanied by mental disorders such as fatigue, depression and anxiety[1]. As a primary and secondary disease, the incidence of insomnia remains high[2]. In recent years, about 15% of the population in China has been diagnosed with insomnia, and 45% of the population has experienced different degrees of insomnia symptoms[3] . It can be seen that insomnia has caused great harm to individuals, families and society. Since V Euler and Gaddum[4] discovered substance P in the brain and gut of horses[4]. The theory of microorganism and gut-brain axis is gradually established and widely accepted in development[5]. Studies have found that this theory is closely related to various mental diseases, especially insomnia. However, this theory is only widely recognized abroad, and is not generally accepted at home. Traditional Chinese medicine (TCM) treatment of insomnia has a long history, mainly based on TCM and acupuncture, but the treatment ideas are diverse. And there is no unified theoretical guidance. In this context, the combination of the two has a realistic basis. Therefore, related research began to gradually emerge. we hope that through this review, we can deeply understand the degree of integration of TCM treatment of insomnia and microbial-gut-brain axis theory. Confirming the scientific and feasibility of microbial-gut-brain axis theory in guiding TCM treatment of insomnia, and point out the future development direction.
TCM can improve the sleep quality of insomnia patients and insomnia animal models. The mechanism is related to the regulation of intestinal flora and the improvement of intestinal flora disorder[6]. Many studies have shown that TCM treatment can significantly change the intestinal microbiota, promote the growth of beneficial bacteria and the excessive growth of harmful bacteria, and help maintain a healthy intestinal environment by balancing the number of probiotics and pathogenic bacteria[7]. At the same time, the role of TCM and intestinal flora is mutual: One is that the active components of TCM regulate the composition and metabolism of intestinal flora. The other is that the intestinal flora decomposes and metabolizes the active components of TCM. These interactions can produce a series of metabolites that affect the physiological and pathological functions of the body[8]. Next, the relationship between microorganism-gut-brain axis and insomnia and the mechanism of action of TCM in the treatment of insomnia through microorganism-gut-brain axis will be discussed in detail.
The gut-brain axis is a bidirectional regulatory pathway in which the motor and sensory parts of the gastrointestinal tract send information to the central nervous system. The central nervous system makes corresponding feedback to the intestinal tract[9]. Intestinal flora can connect with the gut-brain axis through its own metabolites and secreted neurotransmitters to form the microbial-gut-brain axis. This axis involves nervous, endocrine, immune and other aspects, and jointly regulates various physiological activities of the human body. The increasing importance of the microbial-gut-brain axis in the basic areas of biology and physiology of psychiatry, neurodevelopment, and neurodegenerative diseases has been confirmed[10]. Similarly, this axis is also linked to hypertension. for example, hypertension can lead to changes in intestinal ecology, and pathological changes in the intestine and its microbiome can act on the brain through immune and neural pathways, thus exacerbating hypertension[11], and form a vicious circle. Insomnia is also closely related to the above diseases. Including cardiovascular disease, obesity, diabetes, mental illness, hypertension and so on[12]. Insomnia is a concomitant symptom of these diseases. There is a certain degree of coincidence between the two, which proves that the microbial-gut-brain axis may be associated with insomnia.
Based on the theory of microbial-gut-brain axis, many physicians have tried to prove that it is also inextricably linked with insomnia. Some doctors have found that the decrease of γ-aminobutyric acid (GABA) level is the characteristic marker of objective sleep disorders, and involves the changes of intestinal microorganisms and short-chain fatty acids[13]. At the same time, studies have shown that GABA can regulate the sleep-wake cycle, and the activation of GABA receptors is conducive to sleep[14], while lactic acid bacteria and bifidobacteria are the main intestinal bacteria producing GABA[15], from which it can be seen that changes in intestinal flora are associated with insomnia; Studies have found that insomnia is related to the overactivity of the hypothalamic pituitary adrenal (HPA) axis[16], while gut microbes can modulate HPA function by modulating cytokine or bacterial antigen activity[17]. It can be seen that intestinal microorganisms can regulate each other through the HPA axis and the central system, thus affecting sleep. In addition, the most intuitive factor affecting insomnia is no more than circadian rhythm disorder, and intestinal microbiota can affect the human biological clock, resulting in circadian rhythm disorder, further affecting endocrine metabolism, which can cause insomnia[18]. Therefore, the microbial-gut-brain axis can directly and indirectly affect sleep, and insomnia can also lead to changes in the structure and diversity of intestinal flora through this axis.
Jing Yue encyclopedia said "Gai Chu's sleep is based on Yin, and the spirit is its master. When the spirit is peaceful, he will sleep; when the spirit is restless, he will not sleep". And "Miraculous Pivot Evil Guest": "The heart is the master of the five Zang organs and six houses, and the place where the spirit is given up". Another "Medical Reading Secretary": "The heart is the foundation of life, the place of the spirit also, the spirit is insufficient, the spirit will disappear". From this, we can see that one of the causes of insomnia is mental restlessness, and the main cause of mental restlessness is mental deficiency, which can be further inferred to be the dysfunction of the viscera leading to mental deficiency. In a word, insomnia is closely related to the viscera of the human body.
"Miraculous Pivot Ying Health Meeting": "The day is not fine, the night is not dry", because "Qi and blood decline, the muscles are withered, the airway is astringent, the Qi of the five viscera compete with each other, the Ying Qi is weak, and the defensive Qi is internal attack". Insomnia at night is due to deficiency of Qi and blood, deficiency of nutrient Qi, and internal attack of defensive Qi. It shows that Qi and blood are insufficient, the body loses nourishment, Ying and Wei resist each other, and the spirit is uneasy. According to TCM theory, the spleen and stomach are the acquired foundation and the source of Qi and blood, and the deficiency of Qi and blood is caused by pathological changes of the spleen and stomach to a certain extent[19].
There is a saying in the Canon of Internal Medicine that if the stomach is not in harmony, the patient will be restless. In addition, it is said in Miraculous Pivot: Moving and Stomach Qi is injected into the lung. Go up to the empty orifices, follow the eye system, and enter the brain. The imbalance of Yin and Yang in the whole gastrointestinal system and the disharmony of Qi will lead to stomach Qi rushing up to the brain without sleep[20]. Thus it can be seen that the spleen and stomach are very important, and the treatment of insomnia from the spleen and stomach is also the proper meaning. "Miraculous Pivot: Meridians" says: "The meridians of the stomach and foot Yangming originate from the nose and cross the middle Along the hairline, only the forehead skull "has another" foot Yangming difference Lower Collateral Throat Pass". "Large Intestine Hand-Yangming Vein Hold the nose and mouth". "The small intestine and the pulse of the sun Oblique collaterals in zygoma. This shows that the stomach, large intestine, and small intestine are all directly related to the brain, and Zhang and Rong[21] even proposed the hypothesis that the brain controls the meridians and collaterals, which integrates the meridians and collaterals with the brain and nervous system. So that insomnia extends from the brain and nervous system to the meridians. The meridians and the Zang-fu organs are interior-exteriorly related, so the dysfunction of these Zang-fu organs can also affect the brain. Therefore, it is reasonable to believe that brain diseases may be the result of the influence of abdominal organs, anyway.
There are many methods of treating insomnia in TCM, and there are numerous schools. For example, Xu and Wang[22] treats insomnia from the spirit, mainly by calming the nerves, regulating the body and spirit, and treating insomnia from internal and external aspects, with remarkable curative effect[22]. Song et al[23] treats insomnia by giving consideration to both the symptoms and root causes, treating the mind but not the mind, focusing on the congenital and acquired foundation, taking into account both Qi and blood, and treating insomnia from the perspective of Qi, blood, Yin and Yang. The treatment of insomnia from the spleen and stomach is also a mainstream idea. For example, professor Hui and Han[24] divides insomnia into early, middle and late stages (according to the onset time), with excess syndrome, deficiency syndrome and deficiency syndrome as the main diseases, focusing on the treatment from the spleen and stomach, which makes the treatment ideas and methods unique. On the basis of these theories, the mechanism of microbial-gut-brain axis theory in the treatment of insomnia by TCM and related aspects is discussed as follows.
Studies have found that the most commonly used TCMs for the treatment of insomnia are: Semen Ziziphi Spinosae, Radix Glycyrrhizae, Radix Polygalae, Caulis Polygoni Multiflori, Poria, Semen Platycladi, Poria, and Bulbus Lilii[25]. In addition, there are many combinations of TCMs that can also effectively treat insomnia[26]. Such as Ginseng Semen Ziziphi Spinosae, Semen Ziziphi Spinosae, and Radix Angelicae Sinensis. From the perspective of microorganism-gut-brain axis, it was found that saponins in Semen Ziziphi Spinosae could not only regulate insomnia by acting on GABA, but also improve the intestinal flora of patients[27]. In addition, the action mechanism of saponins to achieve tranquilization and hypnosis is similar to that of melatonin[28]; Polygala tenuifolia Willd can enhance the level of 5-hydroxy tryptamine (5-HT) and GABA in aged insomnia rats, and enhance the sleep behavior of insomnia rats[29]. It is not difficult to find that TCM can treat insomnia by regulating the microorganism-gut-brain axis.
TCM prescriptions for the treatment of insomnia include Suanzaoren Decoction, Guipi Decoction, Banxia Xiexin Decoction, Jiaotai pill, Huanglian Ejiao Decoction, Ganmai Dazao Decoction, Chaihu plus Longgu Oyster Decoction, etc. These prescriptions are also closely related to the microbial-intestine-brain axis theory. Based on the theory of microbial-gut-brain axis, various physicians have deeply studied the mechanism of action on the basis of TCM treatment of insomnia, and achieved remarkable results. For example, Ren Xiaoyu found that Suanzaoren Decoction could improve the intestinal flora disorder caused by stress in sleep deprived rats, reduce the number of harmful bacteria, increase the number of beneficial bacteria and improve the intestinal flora structure[30]; Du et al[31] confirmed that the effect of Suanzaoren Decoction on improving insomnia was indirectly achieved by regulating the structure of flora[32]; Suanzaoren Decoction can also regulate the level of neurotransmitters and stabilize the HPA axis to reduce the occurrence of insomnia. Guipi Decoction can relieve insomnia related symptoms by regulating HPA axis, controlling the content of neurotransmitters [norepinephrine (NE), dopamine (DA), 5-HT, etc.], and regulating some inflammatory factors[32]. At the same time, it can increase immunity and reduce the occurrence of diseases. Banxia Xiexin Decoction can regulate intestinal flora and protect digestive tract mucosa[32] is a good prescription for insomnia caused by "stomach disharmony", which shows that Banxia Xiexin Decoction can reversely regulate intestinal microorganisms through the microorganism-intestine-brain axis in the process of treating insomnia. Coptis chinensis in Jiaotai pill has the function of lowering blood sugar and improving the composition and structure of intestinal flora. Jiaotai pill can also repair intestinal injury, and the protection of other organs and tissues is also part of the reason for its role. That compatibility of the Coptis and the cinnamon in the formula can promote the main hypnotic component (Coptis alkaloid) of the Coptis to penetrate through the blood-brain Barry by inhibiting the expression of P-gp of the blood-brain barry, thereby achieving the hypnotic effect; the Jiaotai pill can also regulate the hypothalamus and the monoaminergic system to treat insomnia. It can be seen that Jiaotai pill also treats insomnia by targeting a certain part of the intestinal microorganism-gut-brain axis. It has been proved that the mechanism of Huanglian Ejiao Decoction on insomnia may be related to its inhibition of the decrease of 5-HT content and the increase of γ-GABA level[33]. Similarly, it was found that Ganmai Dazao Decoction could increase the content of NE and 5-HT, improve sleep and relieve depression to a certain extent[34], Chaihu plus Longgu Muli Decoction mainly treats insomnia by regulating the levels of hypothalamic-pituitary-adrenal axis (ACTH, CORT, etc.). And brain monoamine neurotransmitters (NE, DA, 5-HT, etc.)[35].These components are precisely the products of the microbial-gut-brain axis. It can be seen that these compounds are regulating the microbial-gut-brain axis to achieve the purpose of treating insomnia. The mechanism of acupuncture and moxibustion in the treatment of insomnia related to the microbial-gut-brain axis.
It is not difficult to find that the mechanism of action of acupuncture and moxibustion is basically the same as that of TCM from the theory of microorganism-intestine-brain axis (Figure 1). Acupuncture treatment pays attention to the selection of acupoints based on syndrome differentiation, and acupuncture therapy on the basis of syndrome differentiation can achieve good results and improve gastrointestinal function[36]; The application of electroacupuncture and pestle acupuncture in the treatment of insomnia is novel and significant[37]; Acupuncture combined with abdominal circular massage can improve the function of hypothalamus and parahippocampal gyrus, thus achieving the effect of improving insomnia symptoms[38]. In addition, it was found that acupuncture could inhibit the activity of HPA axis, thus improving insomnia symptoms[39]. However, it is not limited to the regulation of HPA axis. For example, Liu et al[40] concluded that the mechanism of action of acupuncture and moxibustion in the treatment of insomnia is mainly to regulate the nervous system, neurotransmitters, inflammatory factors, biological clock genes, and sleep factors, so as to achieve the purpose of regulating sleep disorders. Wang et al[41] also found that acupuncture and moxibustion may treat depression comorbid insomnia by regulating HPA axis, regulating related neurobiochemical factors (various neurotransmitters, nutritional factors, etc.), and inhibiting inflammatory factors, and has a significant effect on improving the sleep quality of patients[42]. Rong et al[42] summarized the principles of acupuncture under the guidance of the microorganism-intestine-brain axis theory: First, insomnia is related to the brain, so the acupoints on the head and neck (such as Baihui, Yintang, Shangxing, Shenting, ToulinQi, Fengchi, etc.) Are often selected; Second, the heart governs the spirit, so the heart meridian of Hand-Shaoyin and the acupoints with the word "spirit" (such as Shenmen, Sishencong, etc.) Are often used. Thirdly, insomnia is closely related to the heart, liver, kidney, etc. Stimulating the Back-shu points (the Qi of the viscera is perfused into the Back-shu points) can directly stimulate the microorganism-intestine-brain axis, which can promote sleep. It can be intuitively found that there are many overlaps between these acupuncture sites and the anatomical sites of the microbial-gut-brain axis. From the perspective of regulating the spleen and stomach to treat insomnia, the main points are Zhongwan, Guanyuan Tianshu, Qihai and so on[43]. These acupuncture therapies can improve insomnia by regulating the secretion of neurotransmitters and some hormones, and can also down-regulate the HPA axis to inhibit sympathetic nerve and improve endocrine[44], thereby improving insomnia symptoms, which are part of the same regulatory mechanism as the microbial-gut-brain axis. To sum up, the mechanism of acupuncture and moxibustion in the treatment of insomnia is mainly achieved by regulating some functions of the microbe-gut-brain axis.
From this review, it is not difficult to find that TCM has a clear way to treat insomnia under the guidance of the theory of microbial-gut-brain axis. But there are still many defects and shortcomings at this stage, such as the combination of the theory and the theory of TCM is not thorough enough, and doctors often verify the correlation between the two from the side, lacking more direct evidence-based. In addition, there is a complementary relationship between TCM and the theory of microbial-intestine-brain axis. Before TCM, the feasibility studies on the treatment of insomnia based on the theory of microbial-intestine-brain axis were basically verified by modern medicine, and there has been no major breakthrough in the treatment of drugs. TCM has a large number of therapeutic drugs, but lacks experimental data to verify their scientific and feasibility. Therefore, the combination of the two is imperative. With the increasing attention of many physicians to experimental data, it is believed that every step of the development of TCM in the future will be supported by solid experimental data, and on this basis, it will also feed back experimental research to make it more convenient. The combination of TCM and microorganism-gut-brain axis also has its own limitations. For example, TCM is mainly based on oral treatment, which must have an impact on intestinal flora. It is somewhat weak to support the theory of microorganism-gut-brain axis. However, it should be noted that this theory is only one of many research methods and cannot represent all. It is hoped that readers can realize and expand the relevant directions so as to find the best way to treat insomnia more quickly.
To sum up, the microbe-gut-brain axis theory, as a new theory, has achieved preliminary results in combination with TCM, including but not limited to the field of insomnia. Although there are few research results at this stage, its prospects are extremely broad, which still requires the continuous efforts of the majority of physicians. It is believed that with the gradual application of new technologies and theories (such as microbiomics, metagenomics, the research in this area will continue to deepen and gradually improve, and the results will be more fruitful, so that there will be more new treatment methods and drugs in clinical practice, and the possibility of curing various diseases will also increase infinitely.
Thank you very much to Mr. Li-Min Pan for his guidance and innovative ideas. Thank you for the article edited and written by Mr. Zhi-Bo Hong.
| 1. | Dopheide JA. Insomnia overview: epidemiology, pathophysiology, diagnosis and monitoring, and nonpharmacologic therapy. Am J Manag Care. 2020;26:S76-S84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 86] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 2. | Chao R, Wu C, An H, Li B, Wu J. Effectiveness comparisons of Chinese patent medicine on insomnia: A protocol for systematic review and Bayesian network meta-analysis. Medicine (Baltimore). 2021;100:e24446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Lou G, Yu Z, Chen L, Zhou Y, Zhang L. Trends in Prescriptions for Insomnia in a Province in China Between 2015 and 2019. Front Psychiatry. 2022;13:915823. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | V Euler US, Gaddum JH. An unidentified depressor substance in certain tissue extracts. J Physiol. 1931;72:74-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1213] [Cited by in RCA: 1118] [Article Influence: 62.1] [Reference Citation Analysis (0)] |
| 5. | Chakrabarti A, Geurts L, Hoyles L, Iozzo P, Kraneveld AD, La Fata G, Miani M, Patterson E, Pot B, Shortt C, Vauzour D. The microbiota-gut-brain axis: pathways to better brain health. Perspectives on what we know, what we need to investigate and how to put knowledge into practice. Cell Mol Life Sci. 2022;79:80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 104] [Article Influence: 34.7] [Reference Citation Analysis (0)] |
| 6. | Feng W, Yang Z, Liu Y, Chen R, Song Z, Pan G, Zhang Y, Guo Z, Ding X, Chen L, Wang Y. Gut microbiota: A new target of traditional Chinese medicine for insomnia. Biomed Pharmacother. 2023;160:114344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 34] [Reference Citation Analysis (0)] |
| 7. | Yang Z, Liu Y, Wang L, Lin S, Dai X, Yan H, Ge Z, Ren Q, Wang H, Zhu F, Wang S. Traditional Chinese medicine against COVID-19: Role of the gut microbiota. Biomed Pharmacother. 2022;149:112787. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 34] [Article Influence: 11.3] [Reference Citation Analysis (1)] |
| 8. | Li J, Li D, Chen Y, Chen W, Xu J, Gao L. Gut Microbiota and Aging: Traditional Chinese Medicine and Modern Medicine. Clin Interv Aging. 2023;18:963-986. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 9. | Hattori N, Yamashiro Y. The Gut-Brain Axis. Ann Nutr Metab. 2021;77 Suppl 2:1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 10. | Cryan JF, O'Riordan KJ, Cowan CSM, Sandhu KV, Bastiaanssen TFS, Boehme M, Codagnone MG, Cussotto S, Fulling C, Golubeva AV, Guzzetta KE, Jaggar M, Long-Smith CM, Lyte JM, Martin JA, Molinero-Perez A, Moloney G, Morelli E, Morillas E, O'Connor R, Cruz-Pereira JS, Peterson VL, Rea K, Ritz NL, Sherwin E, Spichak S, Teichman EM, van de Wouw M, Ventura-Silva AP, Wallace-Fitzsimons SE, Hyland N, Clarke G, Dinan TG. The Microbiota-Gut-Brain Axis. Physiol Rev. 2019;99:1877-2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1156] [Cited by in RCA: 2786] [Article Influence: 464.3] [Reference Citation Analysis (2)] |
| 11. | Wang X, Chen Z, Geng B, Cai J. The Bidirectional Signal Communication of Microbiota-Gut-Brain Axis in Hypertension. Int J Hypertens. 2021;2021:8174789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 12. | Han M, Yuan S, Zhang J. The interplay between sleep and gut microbiota. Brain Res Bull. 2022;180:131-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 67] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 13. | Yu L, Han X, Cen S, Duan H, Feng S, Xue Y, Tian F, Zhao J, Zhang H, Zhai Q, Chen W. Beneficial effect of GABA-rich fermented milk on insomnia involving regulation of gut microbiota. Microbiol Res. 2020;233:126409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 107] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 14. | Dong YJ, Jiang NH, Zhan LH, Teng X, Fang X, Lin MQ, Xie ZY, Luo R, Li LZ, Li B, Zhang BB, Lv GY, Chen SH. Soporific effect of modified Suanzaoren Decoction on mice models of insomnia by regulating Orexin-A and HPA axis homeostasis. Biomed Pharmacother. 2021;143:112141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 15. | Wang Z, Wang Z, Lu T, Chen W, Yan W, Yuan K, Shi L, Liu X, Zhou X, Shi J, Vitiello MV, Han Y, Lu L. The microbiota-gut-brain axis in sleep disorders. Sleep Med Rev. 2022;65:101691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 138] [Reference Citation Analysis (0)] |
| 16. | Dressle RJ, Feige B, Spiegelhalder K, Schmucker C, Benz F, Mey NC, Riemann D. HPA axis activity in patients with chronic insomnia: A systematic review and meta-analysis of case-control studies. Sleep Med Rev. 2022;62:101588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 62] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 17. | Mikulska J, Juszczyk G, Gawrońska-Grzywacz M, Herbet M. HPA Axis in the Pathomechanism of Depression and Schizophrenia: New Therapeutic Strategies Based on Its Participation. Brain Sci. 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 139] [Cited by in RCA: 190] [Article Influence: 47.5] [Reference Citation Analysis (0)] |
| 18. | Frazier K, Chang EB. Intersection of the Gut Microbiome and Circadian Rhythms in Metabolism. Trends Endocrinol Metab. 2020;31:25-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 107] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 19. | Gao LJ, Liu L, Li LL, Zhou YL, Lv RL, Zhou YN, Hunag SH. [Discussion on the theory of spleen and stomach as the acquired root based on the microorganism-intestine-brain axis]. Shizhen Guoyi Guoyao. 2019;30:1449-1450. |
| 20. | Liu JC, Peng YS, Zhang WC. [Theoretical discussion and application progress of "stomach disharmony leads to restlessness"]. Zhonghua Zhongyiyao Zazhi. 2021;36:6635-6638. |
| 21. | Zhang SJ, Rong PJ. [The Paradigm Shift from Structural Meridians to Functional Meridians-On the Hypothesis of "Brain Controlling Meridians"]. Zhenci Yanjiu. 2022;47:1113-1117. |
| 22. | Xu B, Wang P. [Research and analysis on the origin and development of Anxindan]. Zhonhua Zhongyiyao Zazhi. 2022;37:4330-4333. |
| 23. | Song MY, Zhang JP, Wang XJ, Zhong AQ. [Ruan Shiyi's Three Methods of Treating Insomnia]. Chuantong Zhongyiyao Zazhi. 2018;59:1095-1098. |
| 24. | Hui BB, Han ZC. [Professor Han Zucheng's Experience in Treating Insomnia from Spleen and Stomach]. Hebei Zhongyi. 2021;43:1945-1947 + 1951. |
| 25. | Chiao YW, Livneh H, Guo HR, Chen WJ, Lu MC, Lin MC, Yeh CC, Tsai TY. Use of Chinese Herbal Medicines Is Related to a Reduction in Depression Risk Among Patients With Insomnia: A Matched Cohort Study. Front Neurol. 2020;11:583485. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 26. | Shen Y, Xie LJ, Li H, Lv SG. [Analysis of Lv Shaoguang's Treatment of Chronic Insomnia in Perimenopausal Period]. Zhonhua Zhongyiyao Zazhi. 2020;35:4467-4470. |
| 27. | Shen CY, Wan L, Zhu JJ, Jiang JG. Targets and underlying mechanisms related to the sedative and hypnotic activities of saponin extracts from semen Ziziphus jujube. Food Funct. 2020;11:3895-3903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 28. | Zhang L, Yong YY, Deng L, Wang J, Law BY, Hu ML, Wu JM, Yu L, Wong VK, Yu CL, Qin DL, Zhou XG, Wu AG. Therapeutic potential of Polygala saponins in neurological diseases. Phytomedicine. 2023;108:154483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 29. | Ren XJ, Wang GY, Zhang XP, Wang QQ, Peng ZP. Sedative and Hypnotic Effects and Transcriptome Analysis of Polygala tenuifolia in Aged Insomnia Rats. Chin J Integr Med. 2020;26:434-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 30. | Ren XY, Li TL. [Effects of Suanzaoren Decoction on liver function and specific intestinal bacteria in mice with chronic sleep deprivation]. Yaowu Pinggu Yanjiu. 2020;43:226-231. |
| 31. | Du H, Liu JX, Yan Y, Du CH. [Integrated Metabonomics and Intestinal Flora Analysis of the Mechanism of Suanzaoren Decoction in Improving Insomnia in Rats]. Zhongguo Zhongyao Zazhi. 2022;47:6741-6752. |
| 32. | Kang LJ, Xu EP, Ding NN. [Research progress of Guipi Decoction in treating insomnia]. Zhongguo Zhongyiyao Zazhi. 2022;40:64-69. |
| 33. | Ma K, Wang X, Feng S, Xia X, Zhang H, Rahaman A, Dong Z, Lu Y, Li X, Zhou X, Zhao H, Wang Y, Wang S, Baloch Z. From the perspective of Traditional Chinese Medicine: Treatment of mental disorders in COVID-19 survivors. Biomed Pharmacother. 2020;132:110810. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 34. | Chen HS, Gu LJ, Yang YX, Guo JY. GABA and 5-HT Systems Are Involved in the Anxiolytic Effect of Gan-Mai-Da-Zao Decoction. Front Neurosci. 2018;12:1043. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 35. | Xu Y, Xu L, Zheng Y. Application of Chaihu-Guizhi-Longgu-Muli decoction combined with Liuwei Dihuang Pills in the treatment of menopausal insomnia and its effect on sleep quality. Pak J Pharm Sci. 2021;34:2027-2033. [PubMed] |
| 36. | Huangfu YR, Peng W, Guo BJ, Shen ZF, Li L, Liu SW, Zheng H, Hu YP. Effects of acupuncture in treating insomnia due to spleen-stomach disharmony syndrome and its influence on intestinal microbiome: Study protocol for a randomized controlled trial. J Integr Med. 2019;17:161-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 37. | Zhang XY, Tang Q, Tang HL, Wang C. [Study on the difference of therapeutic effect between pestle acupuncture and electroacupuncture on primary insomnia]. Shizhen Guoyi Guoyao. 2020;31:2166-2168. |
| 38. | Zhang Y, Cong D, Liu P, Zhi X, Shi C, Zhao J, Zhang H. Study on the mechanism of regulating the hypothalamic cortical hormone releasing hormone/corticotropin releasing hormone type I receptor pathway by vibro-annular abdominal massage under the brain-intestine interaction in the treatment of insomnia. Medicine (Baltimore). 2021;100:e25854. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 39. | Liu C, Zheng S, Wu W, Wang X, Qin S, Zhao Y, Xi H, Wan Q. Effects of acupuncture on the hypothalamus-pituitary-adrenal axis in chronic insomnia patients: a study protocol for a randomized controlled trial. Trials. 2019;20:810. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 40. | Liu SR, Yu XX, Liu LS, Ni HR. [Discussion on the mechanism of acupuncture and moxibustion in treating insomnia]. Liaoning Zhongyiyao Daxue Xuebao. 2022;24:194-200. |
| 41. | Wang T, Su SY, Zhang X, Lin XY, Wang QX, Su T, Xie CY, Huang L. [Study on the mechanism of acupuncture and moxibustion in the treatment of comorbid depression and insomnia]. Hainan Yixueyuan Xuebao. 2023;29:1182-1186. |
| 42. | Rong HH, Nie S, Liang T, Chen WY. [Research progress of acupuncture and moxibustion treatment of insomnia]. Xiandai Yixue Yu Jiankang Yanjiu. 2020;4:174-176. |
| 43. | Zheng YK, Liu Y, Wu GQ, Wang Y, Li XN, Wang S, Wang XQ. [A proven case of insomnia after ischemic stroke treated with acupuncture at Ashi points along meridians combined with abdominal moxibustion]. Guangming Zhoongyi. 2023;38:149-151. |
| 44. | Lin JG, Kotha P, Chen YH. Understandings of acupuncture application and mechanisms. Am J Transl Res. 2022;14:1469-1481. [PubMed] |