Published online Jun 16, 2024. doi: 10.12998/wjcc.v12.i17.3243
Revised: April 28, 2024
Accepted: May 17, 2024
Published online: June 16, 2024
Processing time: 96 Days and 7.7 Hours
This case series investigated the clinical manifestations, diagnoses, and treatment of cerebral abscesses caused by Streptococcus anginosus. We retrospectively analyzed the clinical characteristics and outcomes of three cases of cerebral ab
Case 1 presented with a history of left otitis media and exhibited high fever, confusion, and vomiting as primary symptoms. Postoperative pus culture indi
Preoperative enhanced head MRI plays a critical role in distinguishing brain tumors from abscesses. Selecting the correct early diagnostic methods for brain abscesses and providing timely intervention are very important. This case series was in accordance with the CARE guidelines.
Core Tip: Brain abscess patients are often at risk and the condition can be fatal. Several complications might arise after cure; therefore, early diagnosis and timely treatment intervention are particularly important in order to improve the prognosis of brain abscess patients. However, the early diagnosis of brain abscesses is always difficult. We reviewed and analyzed specific treatment processes and early diagnosis of three cases of brain abscesses caused by Streptococcus anginosus.
- Citation: Tan SD, Li MH. Brain abscess caused by Streptococcus anginosus group: Three case reports. World J Clin Cases 2024; 12(17): 3243-3252
- URL: https://www.wjgnet.com/2307-8960/full/v12/i17/3243.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i17.3243
A brain abscess is the focal accumulation of infectious pus in the brain parenchyma, which can result as a complication of another infection or can arise from trauma or surgery. The most common genera causing community-acquired brain abscesses are Viridans streptococci and Staphylococcus spp. Viridans streptococci belong to the Streptococcus pharyngis group, also known as Streptococcus milleri (Unk. millieri) and Streptococcus retardans (Str. mi-tis), Streptococcus haematobium (Str. sanguis), and Streptococcus salivarius (salivarius) and Streptococcus mutans (Str. mutans). The Streptococcus pharyngeus group consisted of three species: Streptococcus intermedius, Streptococcus pharyngeus, and Streptococcus constellatus. Viridans Streptococci contain proteolytic enzymes that predispose them to cause tissue necrosis which leads to abscesses. This case study reports analysis of data from three patients admitted to Shaoxing People’s Hospital with Streptococcus pharyngis group brain abscesses. In this case report, clinical data were obtained from three patients with Streptococcus pharyngis infections were retrospectively analyzed, with focus on the importance of plasma microbial cell-free DNA (mcfDNA), next-generation sequencing, initial antimicrobial drug selection, and early surgical intervention for regression.
Case 1: A 43-year-old male with a history of left otitis media presented with chief complaints of high fever, confusion, and vomiting for one day”.
Case 2: A 63-year-old female patient was admitted to the hospital with a chief complaint of "dizziness since 2 d".
Case 3: A 58-year-old male patient was admitted to the hospital with "discovery of a mass in the left temporal lobe for 1 wk.
Case 1: The patient was unconscious around 8:00 AM on September 5, 2021, with vomiting, which consisted of gastric content, accompanied by fever, however, without limb convulsions, frothing at the mouth, chills, cough, sputum, limb movement impairment, facial drooping, salivation, incontinence, or signs of trauma. The patient was brought to the emergency department of our hospital, where head computed tomography (CT) indicated a “low-density lesion in the left temporal lobe”, suggesting a brain abscess. The patient was treated with measures to reduce intracranial pressure and antibiotics, and was admitted to the hospital with a suspected “brain abscess”.
Case 2: The patient began experiencing dizziness on April 11, 2019, with no apparent cause; there was no rotation of objects, nausea or vomiting, blurred vision, limb convulsions, frothing at the mouth, rolling back of the eyes, or impairment of limb movement. The patient sought treatment at the Seventh People’s Hospital of Shaoxing and underwent head CT tomography, which revealed a “space-occupying lesion in the left frontal lobe”. The patient still had dizziness on April 11, 2019, and was admitted to the hospital with a suspected diagnosis of “frontal lobe mass lesion”.
Case 3: The patient suffered a left ankle joint fracture due to a traffic accident on March 12, 2017. During the surgical procedure at our hospital, a head magnetic resonance imaging (MRI) with contrast enhancement and diffusion-weighted imaging (DWI) revealed a "space-occupying lesion in the left temporal lobe", and a preliminary diagnosis was of a possible metastatic tumor. After the fracture improved, the patient was admitted to the Neurology Department.
Case 1: The patient’s general health was average, with no history of diabetes, hypertension, infectious diseases, drug allergies, surgeries, or trauma; however, he had a history of vaccinations.
Case 2: The patient denied a history of diabetes, hypertension, hepatitis, infectious diseases, drug or food allergies, surgery, or trauma.
Case 3: The patient was in good health, with no history of diabetes or hypertension however, had a confirmed history of hepatitis. having had hepatitis over 20 years ago, with an unspecified treatment. The patient had a history of surgery, having undergone treatment for a "left femoral fracture" at another hospital 8 years ago, details of which were unavailable.
Case 1: Born in Keqiao District, Shaoxing City, Zhejiang Province; high school education; unknown occupation; no history of exposure to epidemic water or toxic radiation; confirmed history of smoking for approximately 20 years, averaging 10 cigarettes per day; and confirmed history of alcohol consumption, averaging 1 oz per day. The subjects father died from liver cancer, and his mother died from cerebellar atrophy, his sister was healthy, and there was no family history of diabetes, hypertension, obesity, infectious diseases, tumors, or other hereditary diseases.
Case 2: Born in Yuecheng District, Shaoxing City, Zhejiang Province; occupation unknown; no history of exposure to toxic radiation, smoking, or drinking.
Case 3: Born in Yuecheng District, Shaoxing City, Zhejiang Province, high school education, occupational worker, no history of exposure to toxic substances or radiation, confirmed history of smoking for approximately 20 years, averaging 2-3 cigarettes per day, not quitting smoking, no history of alcohol consumption, parents deceased, one healthy sister, and no family history of genetic diseases.
Case 1: Body temperature was 39.9°C, pulse was 102 beats per minute, respiratory rate was 20 breaths per minute, and blood pressure was 18.52/13.87 kPa. The patient was conscious, however, confused and restless, and uncooperative with the examination, with a Glasgow Coma Scale score of 9. The right pupil diameter was 3 mm with brisk light reflex, and the left pupil diameter was 3 mm with slightly delayed light reflex. Fluid drainage was observed from the left ear, and the external auditory canal was dry. Neck resistance was present, coarse breath sounds were heard in the lungs, with no distinct abnormalities upon cardiac auscultation, the abdomen was soft without tenderness upon palpation, with normal limb movement, and bilateral Babinski sign was negative.
Case 2: Body temperature was 36.6°C, and blood pressure was 15.73/11.20 kPa. The patient was conscious, with good alertness, and was cooperative, with bilateral symmetrical pupils with a diameter of about 4 mm, sensitive to light stimulation. Head and neck examination revealed a soft neck, normal muscle strength in all limbs, and no pathological abnormalities.
Case 3: Body temperature was 36.8°C, and blood pressure was 12.00/8.00 kPa. The patient was conscious and clear-minded, with bilateral pupils about 3 mm in diameter, with light reflex present. No resistance was found in the neck, and no pathological reflex was observed.
Case 1: During admission, blood tests showed a white blood cell count of 22.77 × 109/L, with a neutrophil percentage of 93.3%. Serum C-reactive protein (CRP) levels were 98.42 mg/L. The preliminary diagnosis was of a brain abscess.
Case 2: Routine blood parameters showed a white blood cell count of 6.83 × 1012/L, with 83% neutrophils. Serum CRP levels were 55.28 mg/L.
Case 3: Routine blood tests showed white blood cell counts of 6.20 × 109/L, with a neutrophil percentage of 75.3% and serum CRP levels determined to be 11.77 mg/L.
Case 1: The head CT scan at the time of admission revealed "left otitis media with a patchy hypodense lesion in the left temporal lobe, suggesting a possible abscess".
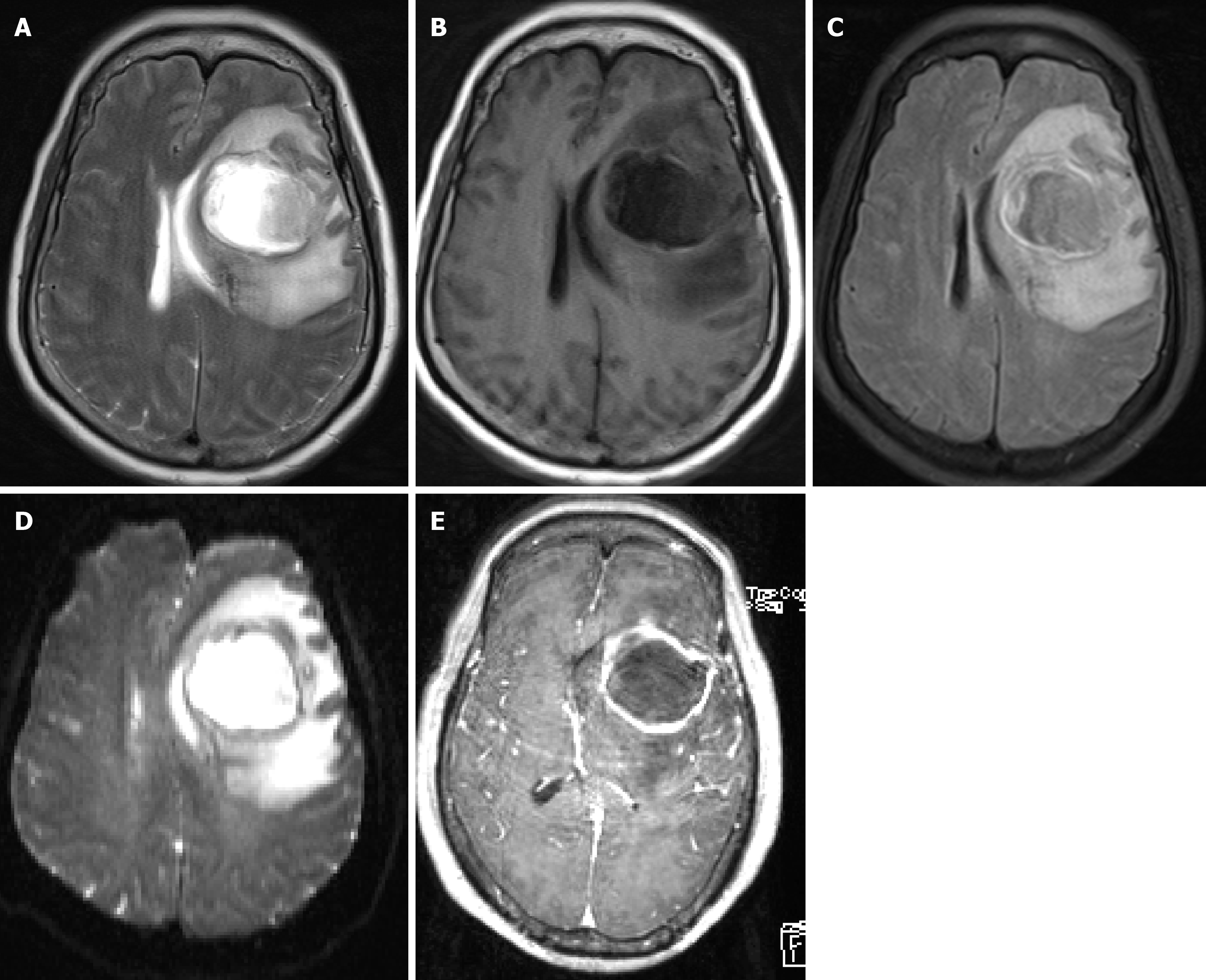
Case 2: Head MRI enhancement and DWI revealed a space-occupying lesion in the left frontal lobe; the preliminary diagnosis was a left frontal mass lesion (Figure 1).
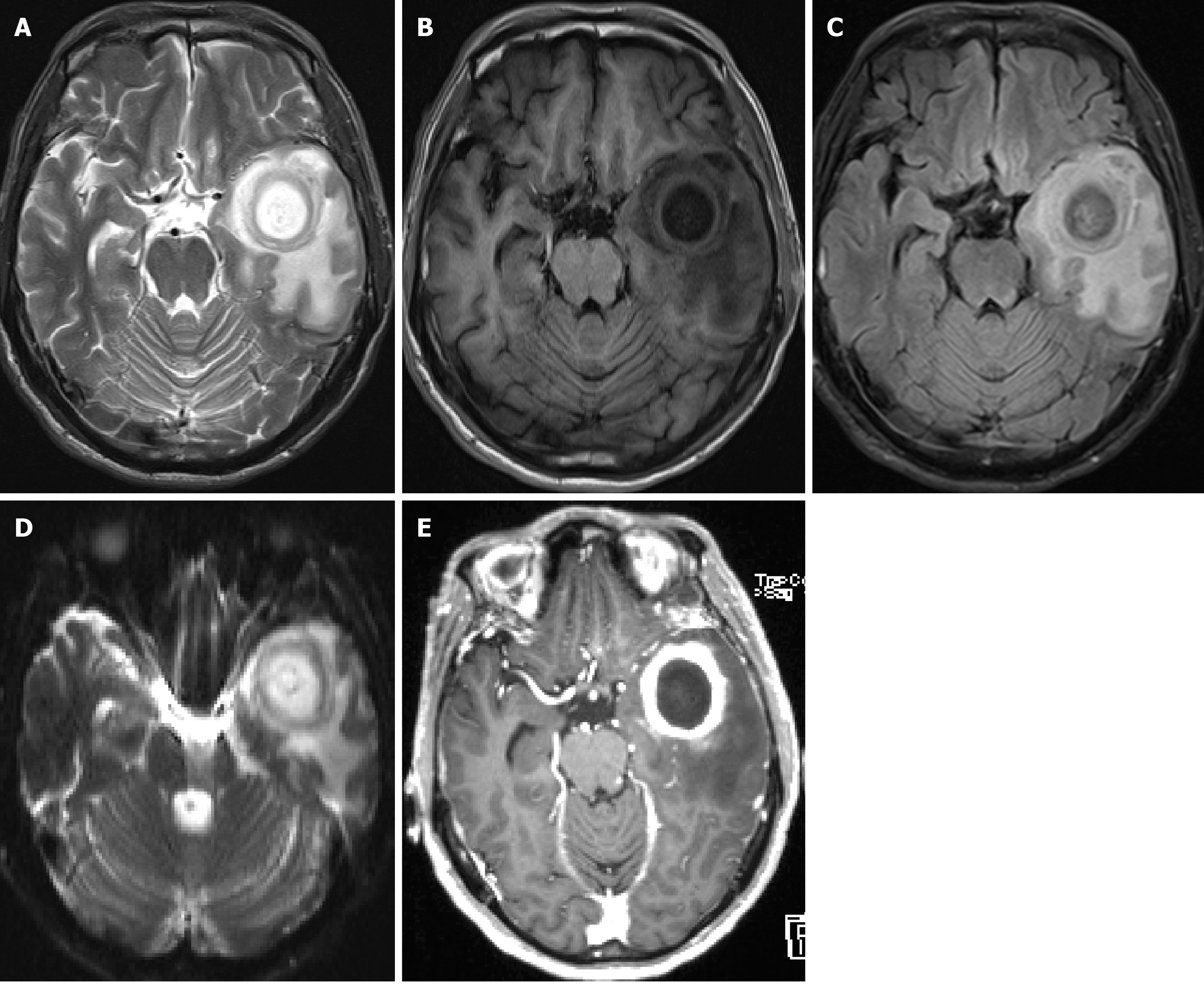
Case 3: Repeated head MRI enhanced scan and DWI showed "extensive abnormal signals in the left temporal lobe, middle fossa floor, infratemporal fossa, pterygopalatine fossa, and surrounding muscles and muscle spaces, considering left temporal lobe brain abscess, however, tumor lesions could not be completely ruled out (Figure 2).
On September 7, 2021, the patient, a post-operative brain abscess case with a history of otitis media, presented a white blood cell count of 25.28 × 109/L. They were being treated with linezolid and meropenem for the infection. An infectious disease consultation was requested, and the recommendation was to continue the current treatment and to monitor blood routine and biochemical indicators promptly. On September 9, 2021, the patient's condition was critical, and the cerebrospinal fluid (CSF) culture results were available. Another infectious disease consultation was conducted, with the following recommendations: The CSF culture revealed Streptococcus constellatus. The current treatment with linezolid in combination with meropenem for intracranial infection was agreed upon. However, since the inflammation indicators were not significantly decreasing, it was suggested to repeat an echocardiogram and evaluate the possibility of other deep abscesses. On September 21, 2021, abnormal liver function was noted, and hepatoprotective treatment was initiated. A consultation with gastroenterology was requested, and the opinion was that if the current use of polyene phosphatidylcholine injections was not effective, they could be switched to compound glycyrrhizin injection and glutathione injections for liver protection.
On April 16, 2019, the patient is scheduled for a total intracranial mass resection under general anesthesia. The chest CT scan shows a significant reduction in volume in the right upper lobe of the lung and multiple enlarged lymph nodes within the mediastinum. A consultation with cardiothoracic surgery was requested, and the opinion was as follows: Considering congenital underdevelopment of the right upper lung, no specific treatment is needed.
On March 30, 20117, the patient's enhanced chest CT scan shows a left upper lung nodule that does not rule out the possibility of malignancy. A consultation with cardiothoracic surgery was requested, and the opinion was as follows: Considering the chest CT and brain MRI findings, lung cancer with brain metastasis should be considered. It is recommended that the patient be transferred to another department for treatment after surgery on the lesion.
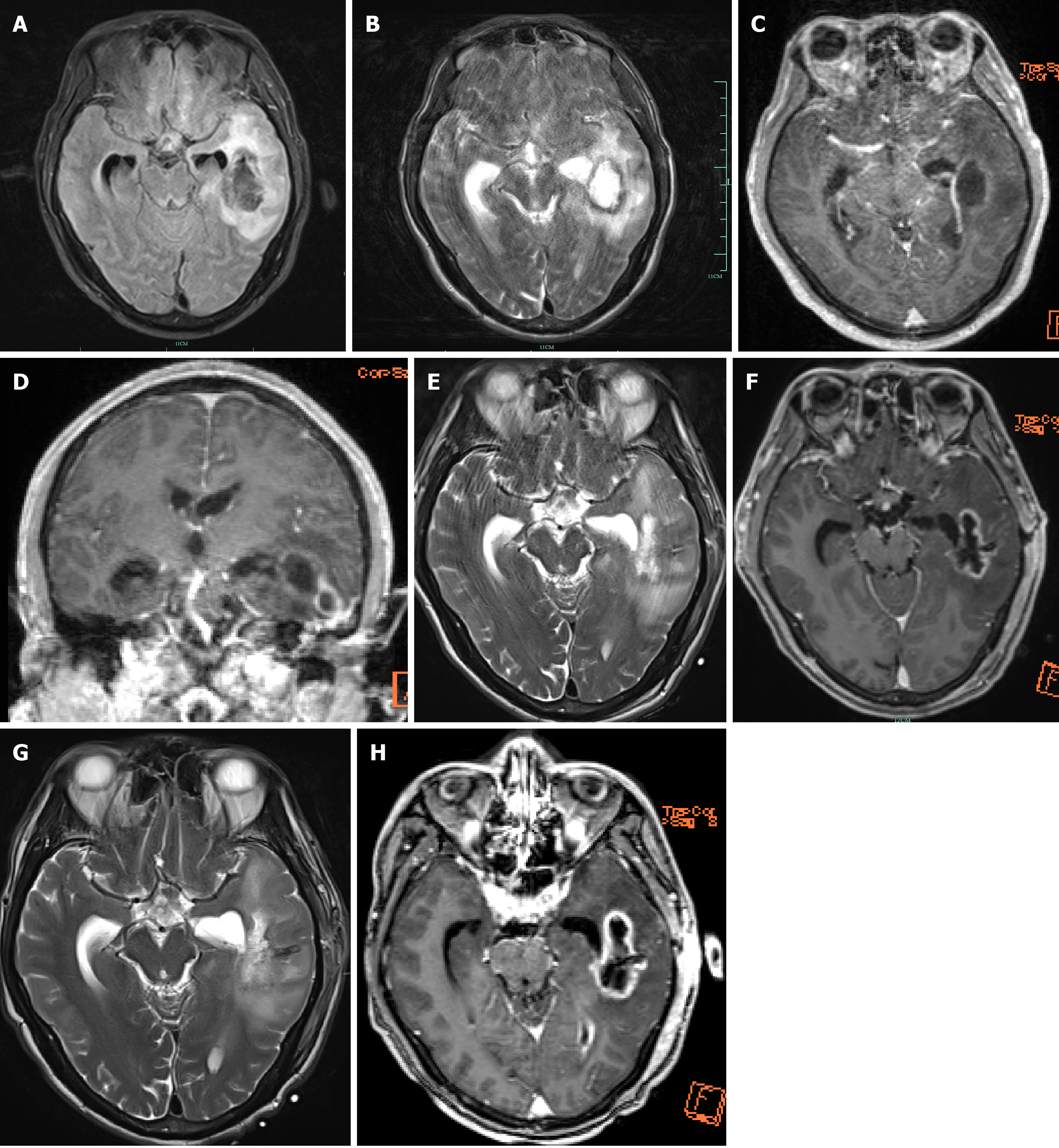
Further diagnostic tests: During the brain abscess puncture and drainage procedure, CRP levels measured were 182.39 mg/L, procalcitonin levels were 5.07 ng/mL, the CSF white blood cell count was 1.95000 × 1011, and the neutrophil percentage was 91.5%. Biochemical analysis of the CSF revealed its protein content to be 812.45 mg/dL. Postoperative brain abscess culture and sensitivity testing revealed Streptococcus constellatus infection, and the pathogen is highly sensitive to erythromycin, clindamycin, ceftriaxone, and vancomycin at the +++ level. Further contrast-enhanced and DWI indicated a left temporal lobe brain abscess accompanied by purulent meningitis and ventricular rupture. Left mastoiditis was considered in this case (Figure 3).
Final diagnosis: A left temporal lobe brain abscess was accompanied by suppurative meningitis and ventricular rupture. Left mastoiditis was considered in this case.
Further diagnostic tests: CRP levels continued to increase.
Final diagnosis: The final diagnosis, based on laboratory tests and craniotomy findings, was a cerebral abscess.
Further diagnostic tests: Postoperative pus culture and drug sensitivity testing revealed Streptococcus pharyngitis ++ infection, with resistance to clindamycin and erythromycin and sensitivity to chloramphenicol, ceftriaxone, levofloxacin, and penicillin G.
Final diagnosis: Based on the findings of imaging and intraoperative observation, the patient was diagnosed with a left temporal lobe brain abscess.
Upon admission, the patient underwent brain decompression treatment and was provided anti-infective therapy using ceftriaxone. Following the final diagnosis, emergency surgery was performed including left brain stereotactic abscess puncture and drainage, ventriculostomy, mastoidectomy, and catheter drainage. Postoperatively, the patient received combined anti-inflammatory treatment consisting of ceftriaxone and vancomycin, as well as hormonal therapy and treatment for reducing intracranial pressure.
Two days after admission, the patient’s consciousness decreased, the bilateral pupils were enlarged by 3 mm, the light reflex was slow, and urinary incontinence was observed. Emergency stereotactic puncture and drainage of the left frontal lobe brain abscess were performed, and the intraoperative evidence verified the presence of a brain abscess in the left frontal lobe area. After surgery, the patient was treated with ceftriaxone 2 g every 12 h to prevent infection measure, and was provided treatment to reduce intracranial pressure and hormonal imbalance. Abscess culture and sensitivity testing revealed that the patient was moderately sensitive to Streptococcus, penicillin G, erythromycin, chloramphenicol, clindamycin, ceftriaxone, levofloxacin, and vancomycin.
During surgery, a pale-yellow lesion, approximately 4 cm × 3 cm in size with clear boundaries, was found located appro
The patient’s condition improved on the 20th day after surgery, and subsequent brain MRI showed a reduction in the lesion size (Figure 3). The family requested discharge. Follow-up revealed that the patient’s condition was stable, with no signs of intracranial infection.
On the 20th day after surgery, the patient recovered consciousness, and she was able to eat. On the 34th postoperative day, the patient returned to the clinic without any abnormal symptoms. Outpatient treatment included amoxicillin, clavulanate potassium tablets, and rifampicin as antimicrobial therapy. Subsequent follow-up revealed no signs of intracranial infection.
The patient's condition was stable 10 d after surgery, with an expected recovery. In the outpatient department, the patient was prescribed amoxicillin-clavulanate potassium and rifampicin tablets for a 6-week course of antibiotic treatment. Follow-up head CT revealed partial absorption of gas and edema in the surgical area.
The advantages of these case studies include: (1) Thoroughly collecting patients’ medical records, data from laboratory tests, and imaging studies; (2) conduct a detailed study of the patient's treatment, including the types, usage, and duration of antibiotics, as well as the surgical process and methods; and (3) follow-up of the patient's prognosis and the patient's condition over a telephonic inquiry after discharge. Disadvantages: (1) The follow-up period was not long enough, mostly because of the patient's unwillingness to continue communication, leading to the abandonment of tracking; and (2) lack of advanced laboratory testing methods, such as plasma mcfDNA and next-generation sequencing.
This case report analyzes and reviews clinical data of three patients with brain abscesses caused by Streptococcus spp., highlighting the importance of early diagnosis for the prognosis of brain abscesses. It also combines treatment methods and prognostic conditions to prepare practitioners and guide clinical practice. In the future, for similar patients, more advanced methods such as plasma mcfDNA and next-generation sequencing can be used to improve early detection rates, thereby achieving better patient prognoses.
By analyzing clinical data of three patients with brain abscesses who sought early medical attention, were diagnosed early, and received timely treatment, and by tracking their prognoses, this case report proposes the hypothesis that early diagnosis and treatment of brain abscess patients will improve their prognoses.
Streptococcus pharyngis is a subgroup of Viridans streptococci, which are gram-positive, peroxidase-negative, and partly Anaerobic cocci. Although these bacteria often colonize the oropharynx and the gastrointestinal tract without harming the host, they are conditionally pathogenic and often cause invasive diseases. Immunodeficiency and congenital heart disease are often considered as risk factors for these infections. Infection with Streptococcus pharyngis is an important cause of central nervous system abscesses in adults and children. These abscesses include brain abscesses, epidural abscesses, and subdural effusions, and can cause meningitis or cavernous sinus thrombosis[1,2].
The main cause of community-acquired brain abscesses is the spread of suppurative lesions or blood-borne infections, with a high probability of Streptococcus oxalis or Staphylococcus infection, and a higher possibility of concurrent anaerobic infections, especially mixed infections with other oral anaerobes (e.g., Clostridium spp.). Microbiological diagnosis requires 16S rRNA gene sequencing, macrogene sequencing, or molecular diagnostic techniques, in addition to traditional culture and pus Gram staining, to enhance the detection rate of pathogenic bacteria. The penicillin-mediated and penicillin resistance rates of the Streptococcus pharyngis group are less than 2%[2]. Ceftriaxone-resistant strains are rare, and resistance to the drug is not routinely tested[3]. One hundred and twenty isolates of Streptococcus pharyngis were tested in vitro, with minimal inhibit concentrations (MICs) of 0.5 mg/L for vancomycin[4] and 2 μg/mL for linezolid MIC90[5], thus indicating that the bacteria are sensitive to both the antibiotics. However, this drug should not be used clinically to treat this group of bacteria because of its susceptibility to daptomycin resistance. The rate of erythromycin resistance in 141 blood strains of streptococci tested in German laboratories was 5.7% (8 strains)[5] and macrolide antimicrobial resistance was avoided wherever possible. Streptococcus pharyngis group bacteria are sensitive to fluoroquinolones, however, are prone to resistance. Most strains in the Streptococcus pharyngis group are resistant to aminoglycosides[6], thus the aforementioned four drugs are not prescribed for treating patients infected with these bacteria. Ceftriaxone in combination with tinidazole or ampicillin-sulbactam is the considered to be the appropriate empirical dose. Vancomycin or linezolid may also be used in addition to anti-anaerobic bacteria if beta-lactams cannot be used due to allergy or resistance.
The three patients mentioned in this case report were considered to have had otogenic, insidious, and hematogenic onsets, respectively, with varying clinical presentations before the diagnosis of brain abscess was confirmed, with the third patient having no significant neurological symptoms. In all three cases, there was no history of long-term glucocorticoid or immunosuppressant use, and it was difficult to differentiate brain tumors and abscesses upon performing imaging for the first time, suggesting that insidious onset and difficulties in early differentiation are crucial reasons for clinicians to misdiagnose brain abscesses as brain tumors or cerebral infarcts. Advanced laboratory techniques such as plasma mcfDNA and metagenomic next-generation sequencing (mNGS) can be used for diagnosis. This method involves replicating the nucleic acid molecules of the pathogen several million or even tens of millions times and extracting them to construct a library that can then be amplified using PCR and mixed in equal amounts for sequencing[7]. This allows the identification and typing of various pathogens, especially in complex infectious diseases in which pathogens are rare, emerging, or atypical. This method is highly sensitive, specific, efficient in terms of time required for diagnosis, and non-invasive. It is well-suited for the early diagnosis of brain abscesses.
Plasma mcfDNA mNGS is used to diagnose common and complex infections by capturing and identifying highly fragmented mcfDNA in circulation. Specific practical methods include dry and wet lab tests[8]. The extraction process is divided into magnetic bead and extraction column methods[9], followed by library construction, PCR amplification, and sequencing to obtain results. This study focuses on the use of plasma mcfDNA mNGS with respect to blood infections as one of the main routes of infection for brain abscesses is the bloodstream. In 2016, Grumaz et al[10] reported a complete mNGS diagnostic workflow that could identify the pathogen causing sepsis in plasma samples within 30 h of sampling, which is extremely rapid. Further studies have shown that, compared to traditional culture methods, mcfDNA mNGS significantly increases the pathogen detection rate in sepsis specimens (by approximately 20% to 30%)[11-14]. In 2019, Blauwkamp introduced the first commercial quantitative plasma mNGS test (the Karius test) to detect pathogens in plasma samples from 350 patients with suspected sepsis. The test revealed that mNGS had a sensitivity of 92.9% and specificity of 62.7% for diagnosing sepsis. However, for patients who had received antimicrobial treatment within 2 wk, mNGS significantly outperformed blood culture in terms of pathogen detection rates (47.9% vs 19.6%)[15]. Although this study did not include all immunocompromised individuals, it made a significant contribution to the clinical detection of bloodstream infections.
There is no uniform opinion on the course of anti-infective therapy for bacterial brain abscesses, which varies with conservative alone or anti-infective treatment combined with surgery; the British Society for Antimicrobial Chemotherapy recommends that antimicrobial therapy should be provided up to 4–6 wk for completely surgically resected brain abscesses and up to 6–8 wk for punctures, and for aspiration it should be provided up to 6–8 wk[16], and empirical antimicrobial therapy should be initiated as soon as a clinical diagnosis of bacterial brain abscess is made. Xu et al[17] reported a preventive course of antibiotics for 5 wk to a patient with a brain abscess caused by Streptococcus constellatus infection, whereas Şenol et al[18] reported an antibiotic course of 12 wk to a patient with a brain abscess caused by Streptococcus constellatus. In this report, all three patients were treated within this timeframe, and all were cured within 6 wk.
Plasma mcfDNA mNGS can provide crucial laboratory testing support for treating patients with brain abscesses that are difficult to differentiate from brain tumors in the early stages. It can also guide early empirical treatment and targeted use of antibiotics, thereby effectively improving patient outcomes. Although this technology currently faces many challenges and shortcomings in the clinical scenario and requires further development, its popularity is limited and the cost of testing is high, making it unsuitable for many patients with poor economic conditions, advent of this technology shows that results from a single technology cannot be reliable. It has changed the diagnostic model of past infectious diseases, enabling accurate, efficient, and faster diagnosis. It is a testing technology that will truly benefit patients in the future. In the treatment of brain abscesses, targeted selection of antibiotics based on bacterial sensitivity test results and understanding specificity of brain abscesses also requires considering the drug crossing the blood-brain barrier and penetration of the abscess wall when selecting antibiotics. Brain abscesses require an early multidisciplinary assessment and treatment.
I sincerely thank my graduate supervisor and the corresponding author of this paper, Professor Ming-Hui Li, as well as the staff in the imaging department for providing the imaging data.
| 1. | Whiley RA, Beighton D, Winstanley TG, Fraser HY, Hardie JM. Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus (the Streptococcus milleri group): association with different body sites and clinical infections. J Clin Microbiol. 1992;30:243-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 284] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 2. | Jiang S, Li M, Fu T, Shan F, Jiang L, Shao Z. Clinical Characteristics of Infections Caused by Streptococcus Anginosus Group. Sci Rep. 2020;10:9032. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 80] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 3. | Chagneau CV, Alcouffe O, Grare M, Oswald E, Massip C. Screening for β-lactam resistance by penicillin G in the Streptococcus anginosus group challenged by rare strains with altered PBPs. J Antimicrob Chemother. 2022;77:1847-1850. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Chen KH, Huang YT, Liao CH, Sheng WH, Hsueh PR. In Vitro Activities of Tedizolid and Linezolid against Gram-Positive Cocci Associated with Acute Bacterial Skin and Skin Structure Infections and Pneumonia. Antimicrob Agents Chemother. 2015;59:6262-6265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Asmah N, Eberspächer B, Regnath T, Arvand M. Prevalence of erythromycin and clindamycin resistance among clinical isolates of the Streptococcus anginosus group in Germany. J Med Microbiol. 2009;58:222-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Southwick FS. Pathogenesis, clinical manifestations, and diagnosis of brain abscess. uptodate. [cited 28 April 2024]. Available from: https://www.uptodate.com/contents/pathogenesis-clinical-manifestations-and-diagnosis-of-brain-abscess?topicRef=6872&source=related_link. |
| 7. | Chiu CY, Miller SA. Clinical metagenomics. Nat Rev Genet. 2019;20:341-355. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 761] [Cited by in RCA: 909] [Article Influence: 151.5] [Reference Citation Analysis (0)] |
| 8. | Wang LL, Wu WJ. Research Progress of Plasma Microbial Cell-Free DNA Metagenomic Next-Generation Sequencing in Infectious Diseases. Linchuang Jianyan Zazhi. 2021;39:516-520. [DOI] [Full Text] |
| 9. | Sorber L, Zwaenepoel K, Deschoolmeester V, Roeyen G, Lardon F, Rolfo C, Pauwels P. A Comparison of Cell-Free DNA Isolation Kits: Isolation and Quantification of Cell-Free DNA in Plasma. J Mol Diagn. 2017;19:162-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 158] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 10. | Grumaz S, Stevens P, Grumaz C, Decker SO, Weigand MA, Hofer S, Brenner T, von Haeseler A, Sohn K. Next-generation sequencing diagnostics of bacteremia in septic patients. Genome Med. 2016;8:73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 177] [Cited by in RCA: 250] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 11. | Rossoff J, Chaudhury S, Soneji M, Patel SJ, Kwon S, Armstrong A, Muller WJ. Noninvasive Diagnosis of Infection Using Plasma Next-Generation Sequencing: A Single-Center Experience. Open Forum Infect Dis. 2019;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 93] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 12. | Lee RA, Al Dhaheri F, Pollock NR, Sharma TS. Assessment of the Clinical Utility of Plasma Metagenomic Next-Generation Sequencing in a Pediatric Hospital Population. J Clin Microbiol. 2020;58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 65] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 13. | Miao Q, Ma Y, Wang Q, Pan J, Zhang Y, Jin W, Yao Y, Su Y, Huang Y, Wang M, Li B, Li H, Zhou C, Li C, Ye M, Xu X, Li Y, Hu B. Microbiological Diagnostic Performance of Metagenomic Next-generation Sequencing When Applied to Clinical Practice. Clin Infect Dis. 2018;67:S231-S240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 596] [Article Influence: 99.3] [Reference Citation Analysis (0)] |
| 14. | Wang L, Guo W, Shen H, Guo J, Wen D, Yu Y, Wu W. Plasma Microbial Cell-Free DNA Sequencing Technology for the Diagnosis of Sepsis in the ICU. Front Mol Biosci. 2021;8:659390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 15. | Goggin KP, Gonzalez-Pena V, Inaba Y, Allison KJ, Hong DK, Ahmed AA, Hollemon D, Natarajan S, Mahmud O, Kuenzinger W, Youssef S, Brenner A, Maron G, Choi J, Rubnitz JE, Sun Y, Tang L, Wolf J, Gawad C. Evaluation of Plasma Microbial Cell-Free DNA Sequencing to Predict Bloodstream Infection in Pediatric Patients With Relapsed or Refractory Cancer. JAMA Oncol. 2020;6:552-556. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 90] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 16. | Qian YY, Jin JL, Zhang WH. Progress on medical treatment of bacterial brain abscess. Weishegnwu Yu Ganran. 2018;13:49-55. [DOI] [Full Text] |
| 17. | Xu LB, Huang LF, Zhao M. A case ofbrain abscess caused by Streptococcus constellatus. Wenzhouyikedaxue Xuebao. 2016;46:620-621. [DOI] [Full Text] |
| 18. | Şenol Ö, Süslü HT, Tatarlı N, Tiryaki M, Güçlü B. Thalamic abscess caused by a rare pathogen: streptococcus constellatus. Pan Afr Med J. 2016;24:256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |