Published online Jun 16, 2024. doi: 10.12998/wjcc.v12.i17.3206
Revised: April 4, 2024
Accepted: April 18, 2024
Published online: June 16, 2024
Processing time: 108 Days and 15.2 Hours
Function-preserving pancreatectomy can improve the long-term quality of life of patients with benign or low-grade malignant tumors, such as intraductal papillary mucinous neoplasms (IPMNs) and mucinous cystic neoplasms. However, there is limited literature on laparoscopic spleen-preserving total pancreatectomy (L-SpTP) due to technical difficulties.
Patient 1 was a 51-year-old male diagnosed with IPMN based on preoperative imaging, showing solid nodules in the pancreatic head and diffuse dilation of the main pancreatic duct with atrophy of the distal pancreas. We performed L-SpTP with preservation of the splenic vessels, and the postoperative pathology report revealed IPMN with invasive carcinoma. Patient 2 was a 60-year-old male with multiple cystic lesions in the pancreatic head and body. L-SpTP was performed, and intraoperatively, the splenic vein was injured and required ligation. Postope
We believe that L-SpTP is a safe and feasible treatment for low-grade malignant pancreatic tumors, but more case studies are needed to evaluate its safety, effi
Core Tip: Spleen-preserving total pancreatectomy (SpTP) can provide patients with a higher long-term quality of life for benign or low-grade malignant pancreatic tumors. However, there is limited literature on laparoscopic SpTP due to technical difficulties. This article reports two cases of laparoscopi SpTP (LSpTP). The postoperative pathology reports showed intraductal papillary mucinous neoplasms and mucinous cystic neoplasm, respectively. Both patients had no major compli
- Citation: Sun MQ, Kang XM, He XD, Han XL. Laparoscopic spleen-preserving total pancreatectomy for the treatment of low-grade malignant pancreatic tumors: Two case reports and review of literature. World J Clin Cases 2024; 12(17): 3206-3213
- URL: https://www.wjgnet.com/2307-8960/full/v12/i17/3206.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i17.3206
Function-preserving pancreatectomy, such as preserving the pylorus, spleen, and duodenum, contributes to better quality of life in the long term for patients with benign or low-grade malignant pancreatic tumors, such as intraductal papillary mucinous neoplasm (IPMN) and mucinous cystic neoplasm (MCN)[1,2]. Spleen-preserving total pancreatectomy (SpTP) has been reported as a treatment for low-grade malignant pancreatic tumors and even pancreatic cancer[3,4]. Addi
Case 1: A 51-year-old male patient with a history of abnormal liver function for more than 4 months and the discovery of a pancreatic mass for 5 d was admitted to the Peking Union Medical Collage Hospital (PUMCH) in March 2022.
Case 2: A 60-year-old male patient with a history of upper abdominal discomfort for 1 month and the discovery of a pancreatic mass for 10 d was admitted to PUMCH in November 2023.
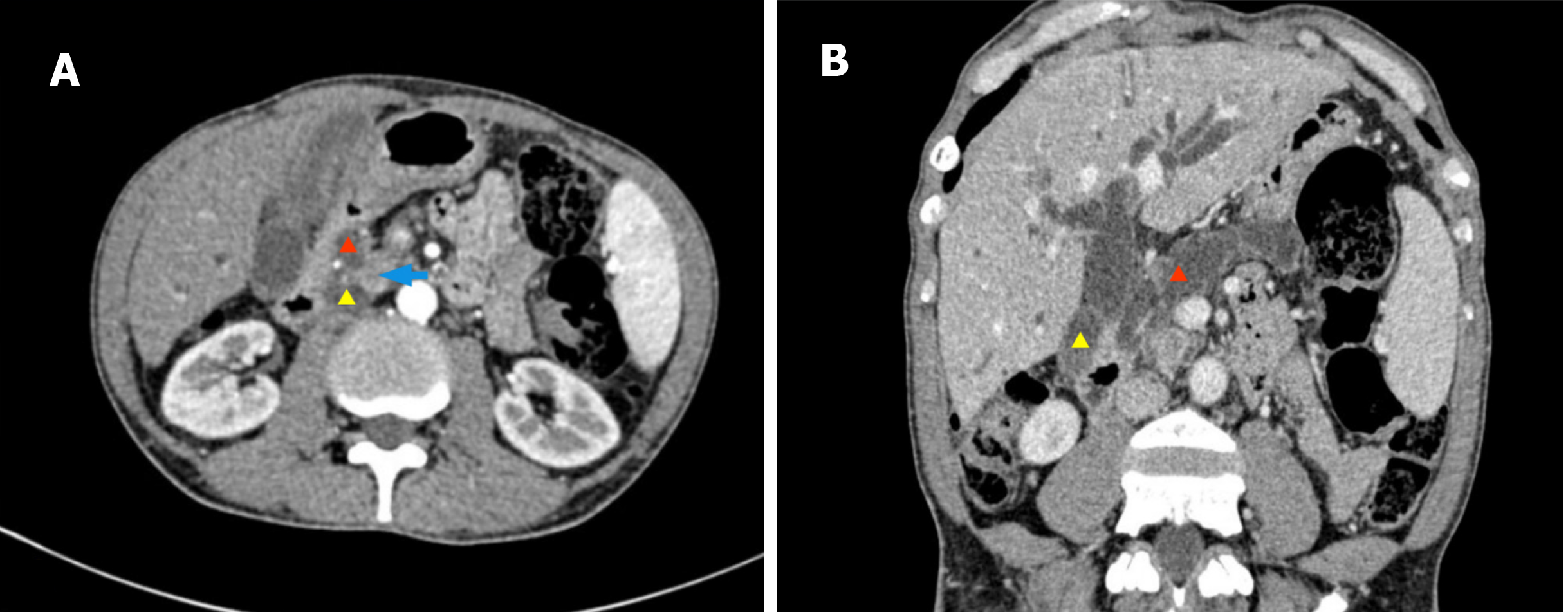
Case 1: Four months before admission, the patient had abnormal liver function test results, including alanine transaminase levels of 265.24 U/L, aspartate transaminase levels of 74.50 U/L, gamma-glutamyl transpeptidase levels of 575.30 U/L, and a total bilirubin (Tbil) level of 14.40 µmol/L. There were no symptoms of jaundice. More than 1 month before admission, the patient experienced dark urine and an increased frequency of bowel movements, approximately 4-5 times per day, with loose stools. The patient also gradually lost weight, with a decrease of approximately 10 kg over a period of 3 months. 5 d before admission, the patient visited our outpatient department and underwent an enhanced abdominal computed tomography (CT) scan, which revealed a nodular lesion in the pancreatic head measuring approximately 2.1 cm 1.8 cm. The boundary between the common bile duct and the pancreatic lesion was unclear, and there was obvious dilation of the intrahepatic and extrahepatic bile ducts, with a width of approximately 1.7 cm at the widest point. There was local interruption of the pancreatic duct and significant dilation in the distal region of the pancreatic duct, with a width of approximately 2.5 cm at the widest point. The pancreatic parenchyma appeared atrophic (Figure 1). Liver func
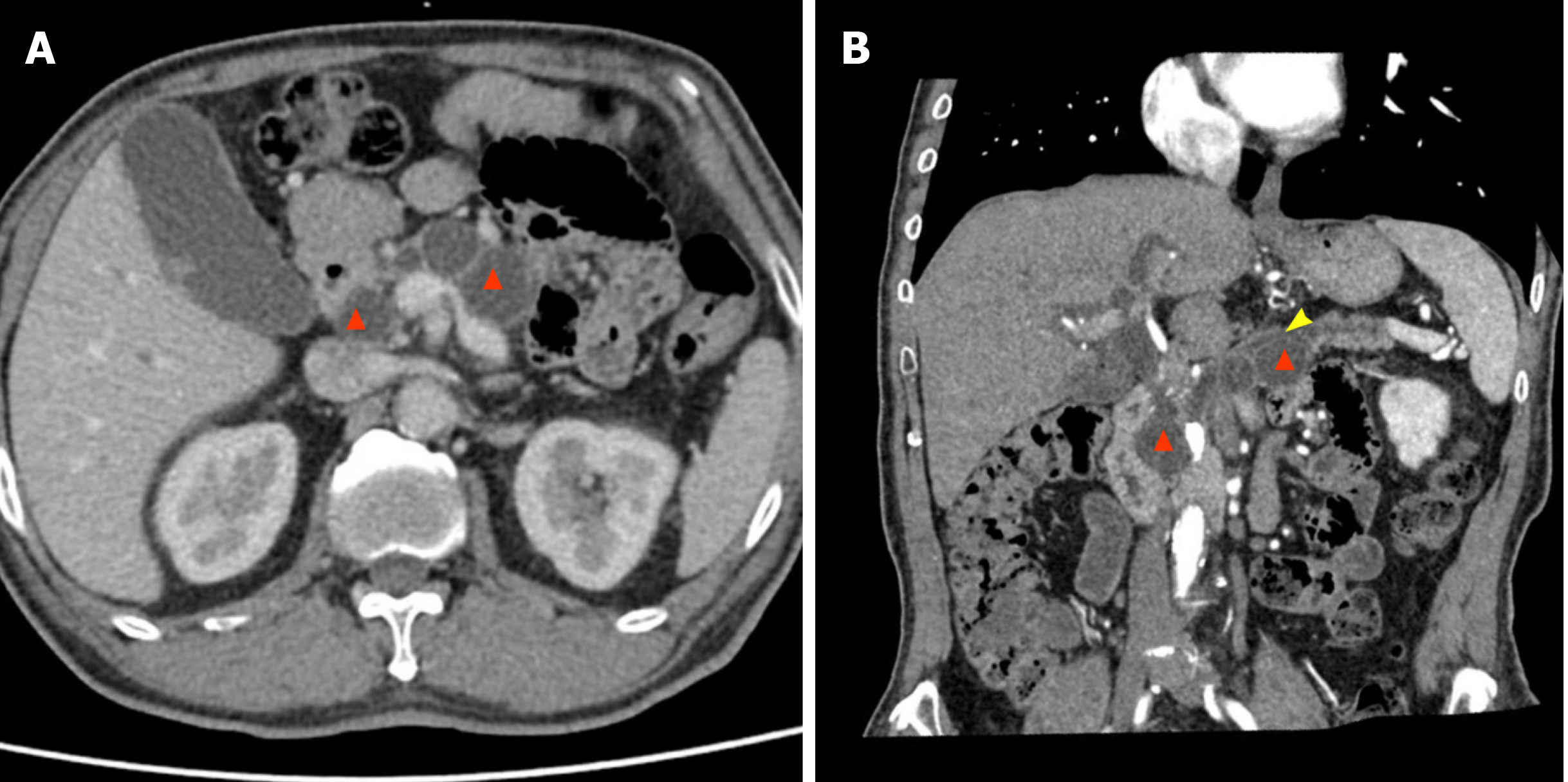
Case 2: One month before admission, the patient experienced upper abdominal discomfort without any apparent cause. 10 d before admission, the patient developed jaundice of the skin and sclera, darkening of urine color, and lightening of stool color. Liver function tests revealed elevated bilirubin levels, with a TBil of 34.5 µmol/L. Magnetic resonance cholangiopancreatography revealed multiple cystic lesions in the pancreas, suggesting the possibility of IPMN and necessitating surgical treatment. The patient then visited our outpatient department, where tumor marker testing revealed a CA19-9 level of 76.1 U/mL. An abdominal enhanced CT scan revealed multiple cystic low-density lesions in the pancreatic head and body, with no significant contrast enhancement. The largest lesion had a diameter of approximately 27 mm × 24 mm. There was slight narrowing of the proximal end of the splenic vein. The pancreatic parenchyma appeared atrophic, and the main pancreatic duct showed diffuse and uneven dilation, with a width of approximately 11 mm at the widest point (Figure 2). The patient was admitted for surgical treatment.
Case 1: The patient had a history of high fasting blood glucose levels for more than 4 years, with a fasting blood glucose of 7.5 mmol/L but no confirmed diagnosis of diabetes.
Case 2: The patient had been diagnosed with hypertension for several years and type 2 diabetes for 17 years, with poor blood sugar control despite insulin therapy.
Case 1: He had a 30-year history of alcohol consumption, with a daily intake of 250 mL. The relevant family history included pancreatic tumors in his mother, but the specific details were unknown. There was no other significant medical history.
Case 2: The patient had a long history of heavy smoking and social drinking. His father passed away due to pancreatic cancer. There was no other significant medical history.
Case 1: Nothing special.
Case 2: Nothing special.
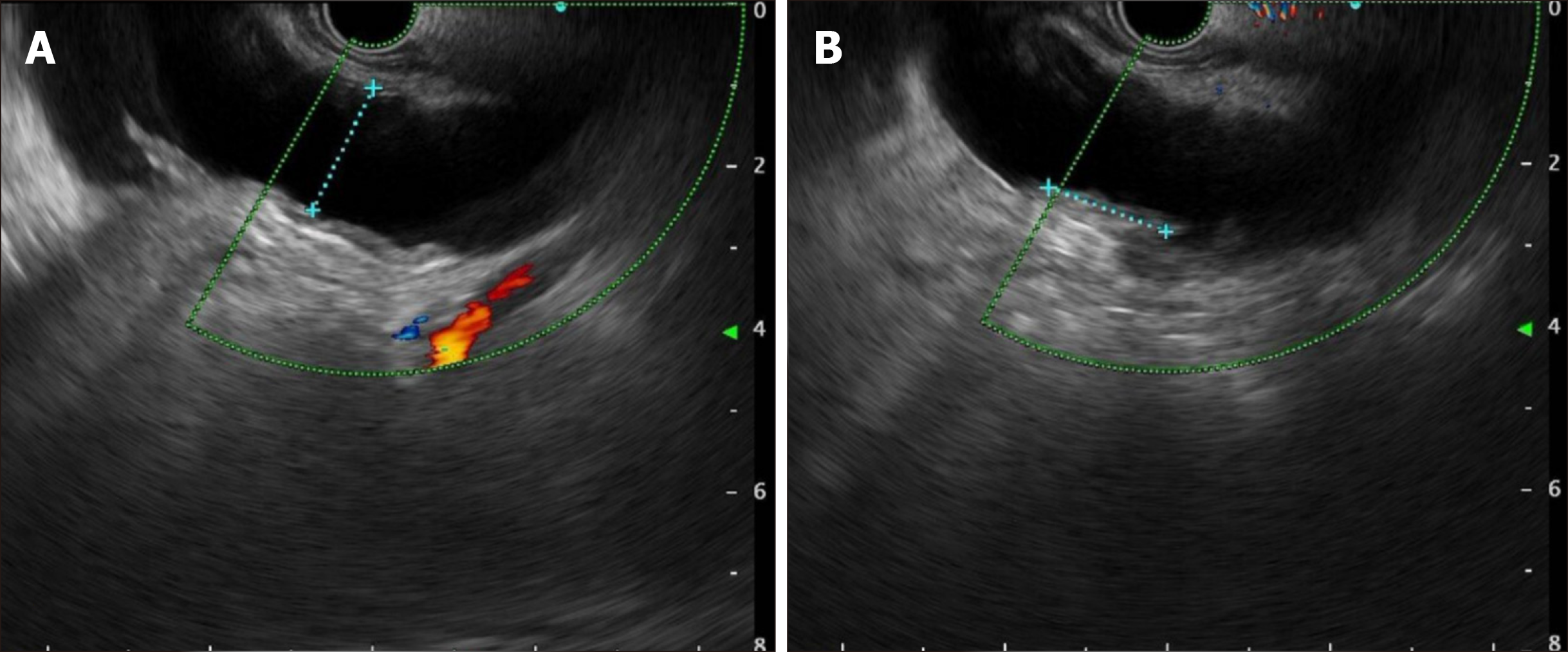
Case 1: The patient was admitted for surgical treatment. After admission, he underwent endoscopic ultrasound exa
Case 2: The imaging and laboratory tests prior to admission have been described earlier. After admission, there were no other important imaging examination results.
Postoperative pathology revealed an IPMN with high-grade dysplasia and evidence of infiltration (moderately differentiated adenocarcinoma). No lymph node metastases were observed (0/16).
Postoperative pathology revealed a MCN of the pancreas with low-grade dysplasia. The surrounding pancreatic tissue showed features of chronic pancreatitis, with low-grade epithelial neoplasia (PanIN1) in the ducts. No lymph node metastases were observed (0/25).
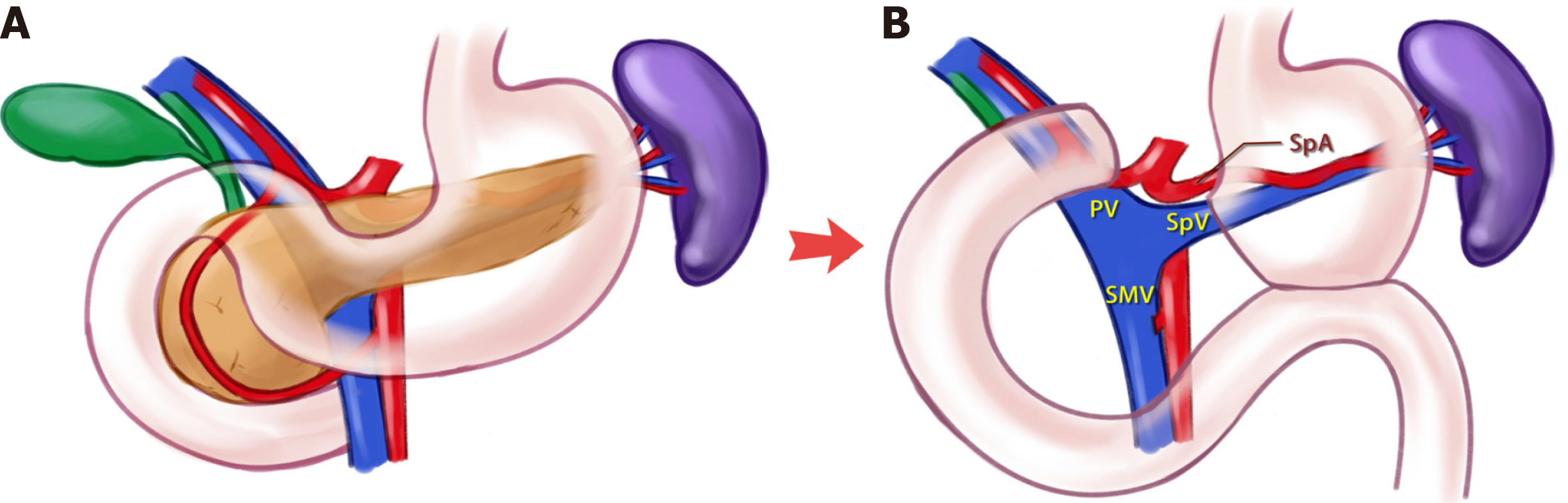
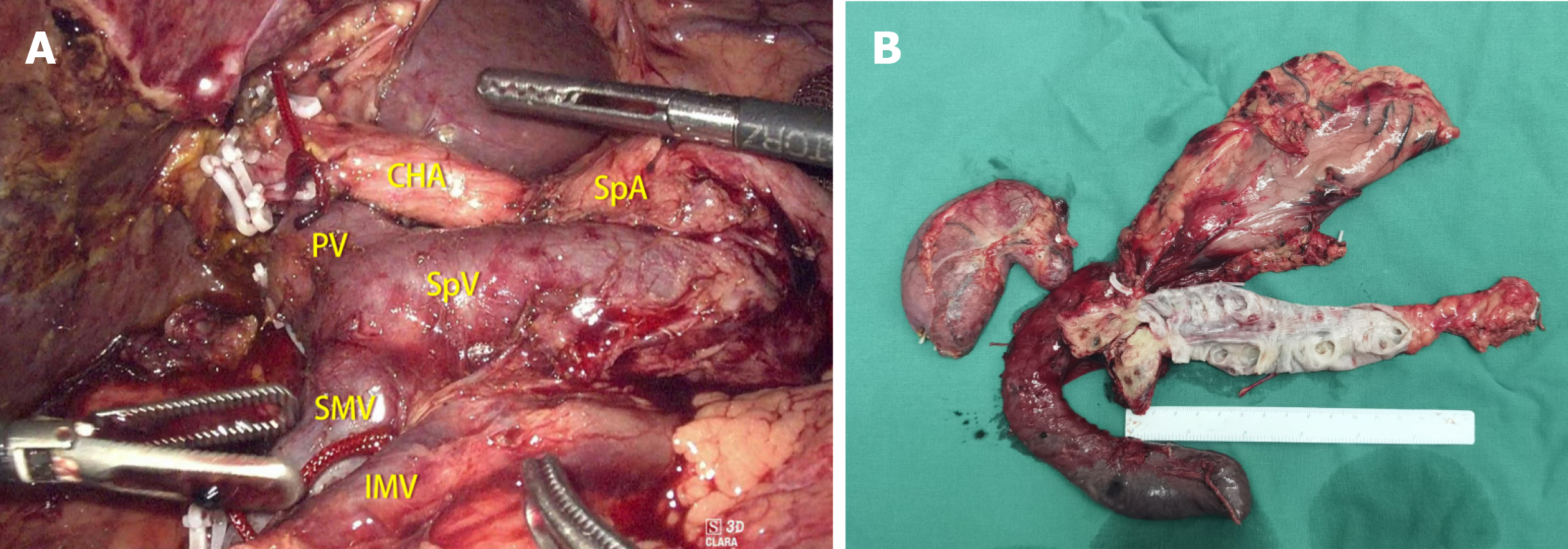
Surgical treatment was performed using a laparoscopic approach. Due to the patient's extensive dilation of the main pancreatic duct and atrophy of the distal pancreatic parenchyma, a decision was made to perform a total pancreatectomy to ensure complete resection. The conventional procedure involved removal of the gallbladder; dissection of the distal stomach, proximal duodenum, and distal common bile duct; and a Kocher incision to mobilize the posterior aspect of the pancreatic head and the duodenum. The posterior artery-first approach was used to dissect the superior mesenteric artery branches, including the inferior pancreaticoduodenal artery. During the dissection of the distal pancreas, adhesions were observed between the pancreas and the splenic vessels, but separation was still feasible. An ultrasonic scalpel was used to carefully dissect the pancreatic body and tail from the splenic vessels, preserving the integrity of the vessels. Finally, the distal pancreas was flipped to the right side, and the portal vein-superior mesenteric vein (PV-SMV) was pulled to the left side before separating the PV-SMV branches from the uncinate process of the pancreas. After complete resection and removal of the specimen, cholangiojejunostomy and gastrojejunostomy were performed sequentially. Drainage tubes were placed at the cholangiojejunostomy and gastrojejunostomy sites and brought out through the abdominal wall. The total operative time was 250 min, with an intraoperative blood loss of 100 mL. The surgical diagram is shown in Figure 4, the intraoperative view is shown in Figure 5A, and the resected specimen is shown in Figure 5B.
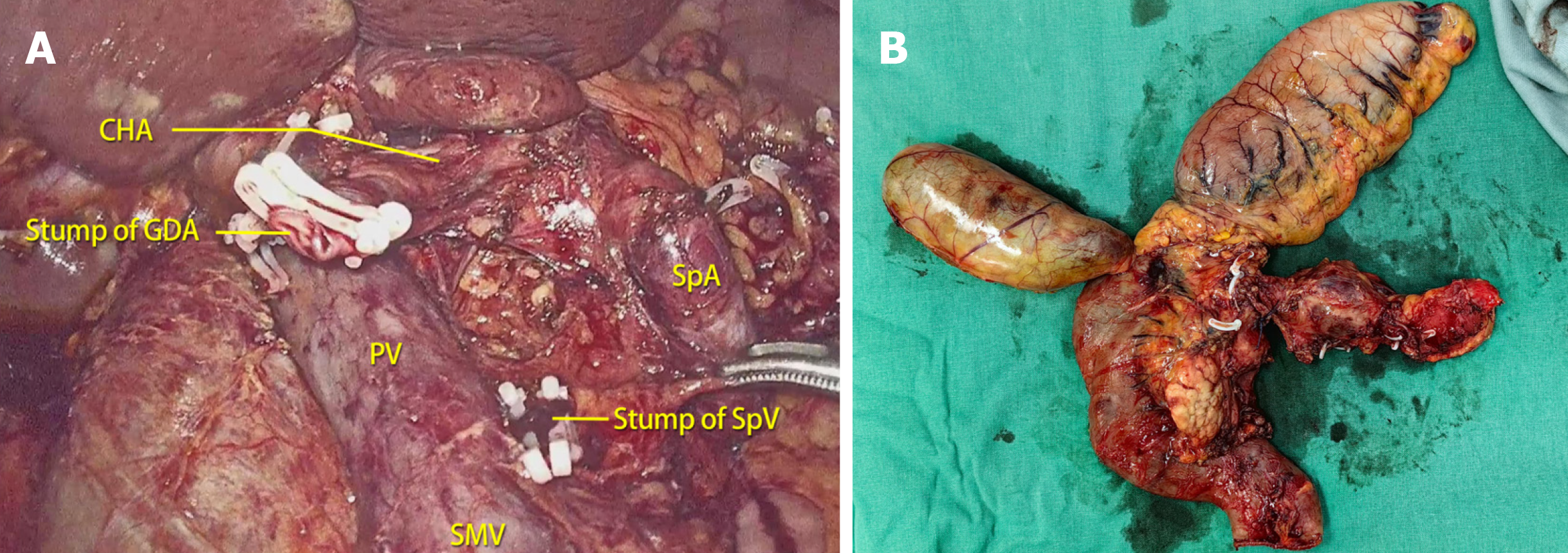
A complete laparoscopic SpTP was performed. The main surgical procedures were similar to those in patient 1. However, in this patient, there was significant adhesion between the splenic vein and the cystic lesion in the pancreatic body, leading to venous injury and hemorrhage during the separation process. The splenic vein was ligated, while the splenic artery was preserved. The total operative time was 200 min, with an intraoperative blood loss of 150 mL. The intraoperative view is shown in Figure 6A, and the image of the resected specimen is shown in Figure 6B. The patient achieved a smooth postoperative recovery, and the cholangiojejunostomy drainage tube was removed on the third day after surgery, followed by removal of the gastrojejunostomy drainage tube on the fifth day. The patient was discharged on the seventh day after surgery.
Following surgery, the patient received chemotherapy with gemcitabine and S-1. At a follow-up visit 20 months after surgery, there was no evidence of tumor recurrence, and the patient tolerated insulin therapy and pancreatic enzyme supplementation well.
At the 3-month follow-up after surgery, the patient presented good short-term recovery.
In the surgical treatment of benign or low-grade malignant tumors of the pancreas, such as IPMN and MCN, surgeons need to consider the curative effect of tumor resection, the preservation of organ function, and the long-term quality of life for patients due to the good prognosis and long survival period associated with these tumors. Multiple low-grade malignant tumor lesions in the head, neck, and body of the pancreas, as well as IPMN with full-length dilation of the main pancreatic duct, are indications for total pancreatectomy. Traditional total pancreatectomy often includes splenec
In recent years, with the popularization of the abovementioned concept and the continuous development of minimally invasive techniques such as laparoscopy and robotic assistance, LSpTP has gradually been reported in the literature. However, due to the technical challenges associated with this procedure, case reports are still the main source of evi
| Year | Ref. | Gender | Age (yr) | Pathology | Surgical procedure | Spleen-preserving technique | Operating time (min) | Intraoperative blood loss (mL) | Morbidity |
| 2011 | Kim et al[11] | Female | 72 | IPMN | LPpSpTP | Warshaw | 450 | 800 | Marginal ulcer |
| 2012 | Choi et al[14] | Female | 74 | IPMN | LPpSpTP | Warshaw | 450 | 800 | Marginal ulcer |
| 2012 | Choi et al[14] | Male | 69 | IPMN | LPpSpTP | Warshaw | 410 | 160 | |
| 2012 | Choi et al[14] | Female | 77 | IPMN | LPpSpTP | Warshaw | 410 | 490 | |
| 2017 | Chapman et al[12] | Male | 66 | IPMN | LSpTP | Kimura | 270 | 150 | |
| 2017 | Wang et al[13] | Female | 68 | IPMN | LPpSpTP | Kimura | 450 | 300 | DGE |
| 2017 | Wang et al[13] | Male | 74 | IPMN | LPpSpTP | Kimura | 480 | 400 | DGE, melena |
| 2019 | Wu et al[15] | Female | 68 | IPMN | LDpSpTP | Kimura | 270 | 250 | |
| 2022 | Bartos et al[16] | NM | 40 | IPMN | LSpTP | Kimura | NM | NM | |
| 2024 | Case 1 | Male | 51 | IPMN | LSpTP | Kimura | 250 | 100 | - |
| 2024 | Case 2 | Male | 60 | MCN | LSpTP | Kimura with SpV resection | 200 | 150 | - |
In this study, we present two cases of LSpTP. Compared to previous reports in the literature, both of these cases involved shorter surgical times, less blood loss, and no serious perioperative complications. In Case 1, postoperative pathology revealed invasive carcinoma, but there was no tumor recurrence at a follow-up of 20 months. In Case 2, the splenic vein was severed during surgery while preserving the splenic artery, which poses a risk of regional portal hy
In conclusion, LSpTP is a feasible surgical option for patients with benign or low-grade malignant tumors of the pancreas requiring total pancreatectomy. It can also be selectively performed with caution in some patients with malignant pancreatic tumors.
| 1. | Kato H, Asano Y, Ito M, Arakawa S, Horiguchi A. Recent trends in organ-preserving pancreatectomy: Its problems and clinical advantages compared with other standard pancreatectomies. Ann Gastroenterol Surg. 2024;8:8-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (1)] |
| 2. | Asano Y, Kato H, Arakawa S, Ito M, Nagakawa T, Nakao A, Ohta T, Yamaue H, Yamamoto M, Satoi S, Kodera Y, Takeyama Y, Ohtsuka M, Endo I, Takada T, Horiguchi A. Clinical outcomes of organ-preserving pancreatectomy for benign or low-grade malignant pancreatic tumors: A multicenter nationwide survey in Japan. J Hepatobiliary Pancreat Sci. 2022;29:898-910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 3. | Beltzer C, Jovine E, Hesch KV, Stifini D, Mastrangelo L, Huth M, Königsrainer A, Nadalin S. Feasibility and outcome of spleen and vessel preserving total pancreatectomy (SVPTP) in pancreatic malignancies - a retrospective cohort study. Langenbecks Arch Surg. 2022;407:3457-3465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (1)] |
| 4. | Yang F, Jin C, Warshaw AL, You L, Mao Y, Fu D. Total pancreatectomy for pancreatic malignancy with preservation of the spleen. J Surg Oncol. 2019;119:784-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 5. | Theilacker C, Ludewig K, Serr A, Schimpf J, Held J, Bögelein M, Bahr V, Rusch S, Pohl A, Kogelmann K, Frieseke S, Bogdanski R, Brunkhorst FM, Kern WV. Overwhelming Postsplenectomy Infection: A Prospective Multicenter Cohort Study. Clin Infect Dis. 2016;62:871-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 75] [Article Influence: 7.5] [Reference Citation Analysis (1)] |
| 6. | Sun LM, Chen HJ, Jeng LB, Li TC, Wu SC, Kao CH. Splenectomy and increased subsequent cancer risk: a nationwide population-based cohort study. Am J Surg. 2015;210:243-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (1)] |
| 7. | Ji S, Xu X, Yu X. Laparoscopic spleen-preserving total pancreatectomy for intraductal papillary mucinous neoplasm (with ). J Visc Surg. 2020;157:441-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (1)] |
| 8. | Lee W, Hwang DW, Han HS, Han IW, Heo JS, Unno M, Ishida M, Tajima H, Nishizawa N, Nakata K, Seyama Y, Isikawa Y, Hwang HK, Jang JY, Hong T, Park JS, Kim HJ, Jeong CY, Matsumoto I, Yamaue H, Kawai M, Ohtsuka M, Mizuno S, Asakuma M, Soejima Y, Hirashita T, Sho M, Takeda Y, Park JI, Kim YH, Yamamoto M, Endo I, Nakamura M, Yoon YS. Comparison of infectious complications after spleen preservation versus splenectomy during laparoscopic distal pancreatectomy for benign or low-grade malignant pancreatic tumors: A multicenter, propensity score-matched analysis. J Hepatobiliary Pancreat Sci. 2023;30:252-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 9. | Hajibandeh S, Ghassemi N, Hajibandeh S, Romman S, Ghassemi A, Laing RW, Bhatt A, Athwal TS, Durkin D. Meta-analysis of laparoscopic spleen-preserving distal pancreatectomy versus laparoscopic distal pancreatectomy with splenectomy: An insight into confounding by indication. Surgeon. 2024;22:e13-e25. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 10. | Coluzzi M, Naziruddin B, Kumano K, Saracino G, Testa G, Beecherl E, Onaca N. Spleen-preserving total pancreatectomy and islet autotransplantation with complete preservation of the splenic arterial and venous supply does not impact islet yield and function. Am J Surg. 2022;224:1295-1300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (1)] |
| 11. | Kim DH, Kang CM, Lee WJ. Laparoscopic-assisted spleen-preserving and pylorus-preserving total pancreatectomy for main duct type intraductal papillary mucinous tumors of the pancreas: a case report. Surg Laparosc Endosc Percutan Tech. 2011;21:e179-e182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 12. | Chapman BC, Paniccia A, Ryan C, Schulick RD, Edil BH. Laparoscopic Spleen-Preserving Total Pancreatectomy for a Main-Duct Intraductal Papillary Mucinous Neoplasm. Ann Surg Oncol. 2017;24:560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 13. | Wang X, Li Y, Cai Y, Liu X, Peng B. Laparoscopic total pancreatectomy: Case report and literature review. Medicine (Baltimore). 2017;96:e5869. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (1)] |
| 14. | Choi SH, Hwang HK, Kang CM, Yoon CI, Lee WJ. Pylorus- and spleen-preserving total pancreatoduodenectomy with resection of both whole splenic vessels: feasibility and laparoscopic application to intraductal papillary mucin-producing tumors of the pancreas. Surg Endosc. 2012;26:2072-2077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 15. | Wu J, Hu Q, Jin L, Yao W, Zhang C, Hu Z, Zhang Y. Laparoscopic duodenum and spleen-preserving total pancreatectomy: A novel surgical technique for pancreatic intraductal papillary mucinous neoplasms. Biosci Trends. 2019;13:456-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 16. | Bartoş A, Pleşa-Furda P, Stoian R, Ciobanu L, Iancu D, Iancu C, Breazu C. Spleen Preserving, Splenic Vessels Spearing, Pure Laparoscopic Total Duodenopancreatectomy for Intraductal Papillary Mucinous Pancreatic Neoplasia (IPMN): Case Report and Technique. Chirurgia (Bucur). 2022;117:472-479. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Boggi U, Palladino S, Massimetti G, Vistoli F, Caniglia F, De Lio N, Perrone V, Barbarello L, Belluomini M, Signori S, Amorese G, Mosca F. Laparoscopic robot-assisted versus open total pancreatectomy: a case-matched study. Surg Endosc. 2015;29:1425-1432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (1)] |