Published online Jun 16, 2024. doi: 10.12998/wjcc.v12.i17.3156
Revised: April 13, 2024
Accepted: May 9, 2024
Published online: June 16, 2024
Processing time: 120 Days and 7.5 Hours
Meningioma in the cerebellopontine angle (CPA) without dural attachment is extremely rare. We report a unique case of meningioma derived from the superior petrosal vein without dural attachment.
A 44-year-old right-handed woman presented with a two-month history of headache and tinnitus. Brain magnetic resonance imaging showed a well-defined contrast-enhancing lesion in the right CPA without a dural tail sign. Tumor resection was performed using a right retro sigmoid approach. A dural atta
The rare occurrence of meningioma without dural attachment makes it difficult to determine dural attachment before surgery. The absence of dural attachment makes it easy to completely resect such tumors. Vessels related to tumors should be removed carefully, considering the possible presence of tumor stem cells in the microvessels.
Core Tip: The rare incidence of meningioma without dural attachment poses challenges in preoperative determination of dural attachment. However, the absence of dural attachment facilitates complete tumor resection. Careful removal of vessels associated with tumor is important to remove tumor stem cells in the micrvessels.
- Citation: Kim YJ, Jung S, Jung TY, Moon KS, Kim IY. Meningioma originating from the superior petrosal vein without dural attachment: A case report. World J Clin Cases 2024; 12(17): 3156-3160
- URL: https://www.wjgnet.com/2307-8960/full/v12/i17/3156.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i17.3156
Meningiomas are slow growing extra-axial lesions that may be focal or extend over areas of the pachymeninges. They arise from arachnoidal (arachnoid cap, meningothelial) cells that are usually present in the leptomeninges and Pacchionian granulation. The contiguity of leptomeninges and granulation to the dura mater presumably accounts for the attachment of the tumor to the dura mater[1]. Interestingly, meningioma without dural attachment (MWODA) occasionally have been reported[2]. However, an infratentorial MWODA in the pontocerebellar cistern seems to be extremely rare. We report a meningioma derived from the superior petrosal vein without dural attachment. To our knowledge, this is the first reported case.
The patient complained of headache and tinnitus.
A 44-year-old right-handed woman without a medical history presented with a two-month history of headache and tinnitus.
There was no significant past illness.
There was no significant past or family history.
A neurologic examination revealed no additional neurologic signs except the above-mentioned symptoms.
There were no significant laboratory findings.
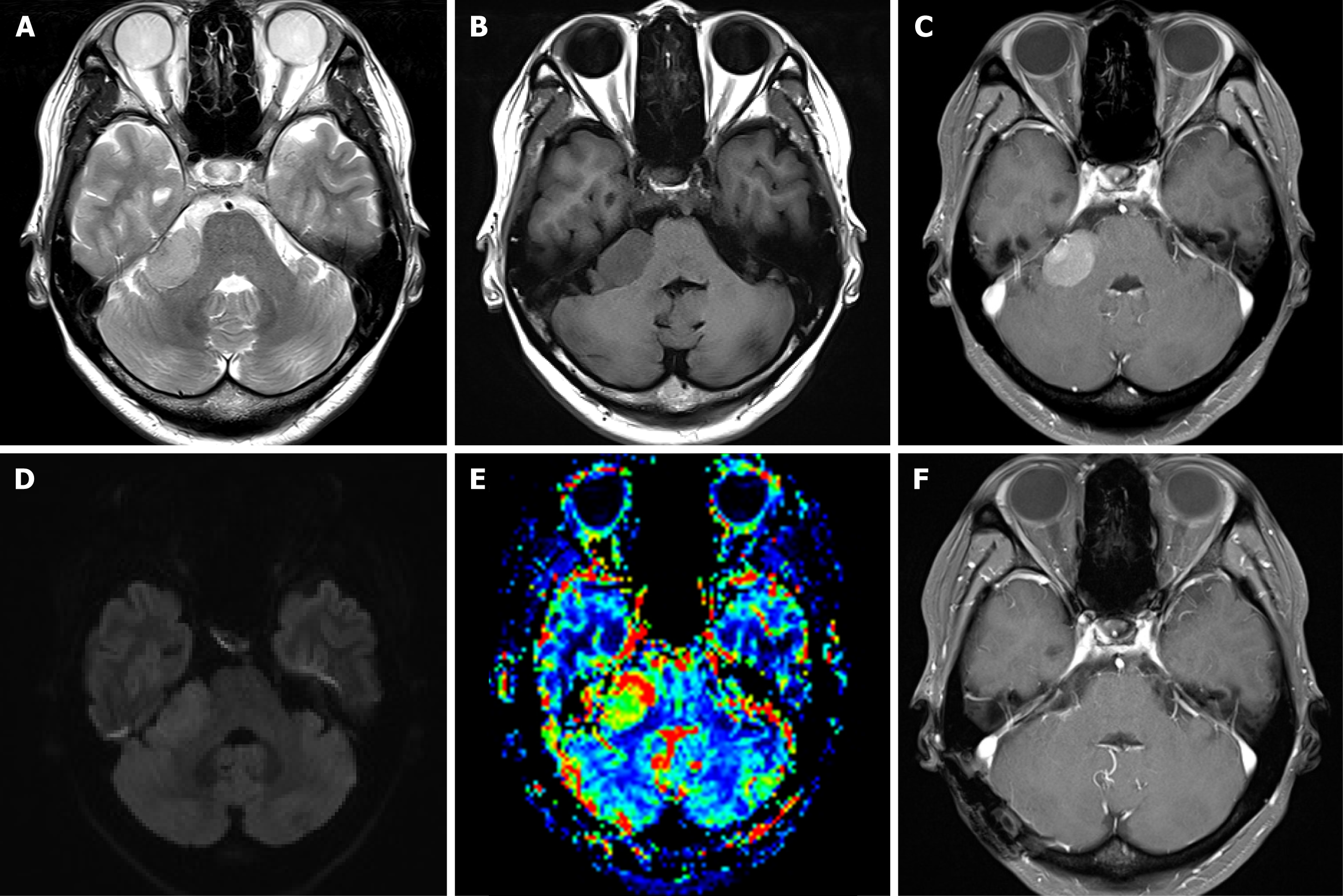
Brain magnetic resonance imaging (MRI) showed a well-defined contrast-enhancing lesion in the right cerebellopontine angle (CPA) without a dural tail sign (Figure 1A-E). MRI revealed a mass (28 mm × 17 mm × 23 mm) in the right CPA without any dural attachment; the mass was primarily isointense on the T2- and hypointense on the T1-weightd image, with avid enhancement. Mass is predominantly isointense/slightly hyperintense on the diffusion-weighted image. Tumoral area demonstrated high relative cerebral blood volume (rCBV).
The patient was diagnosed with CPA meningioma based on imaging and clinical findings.
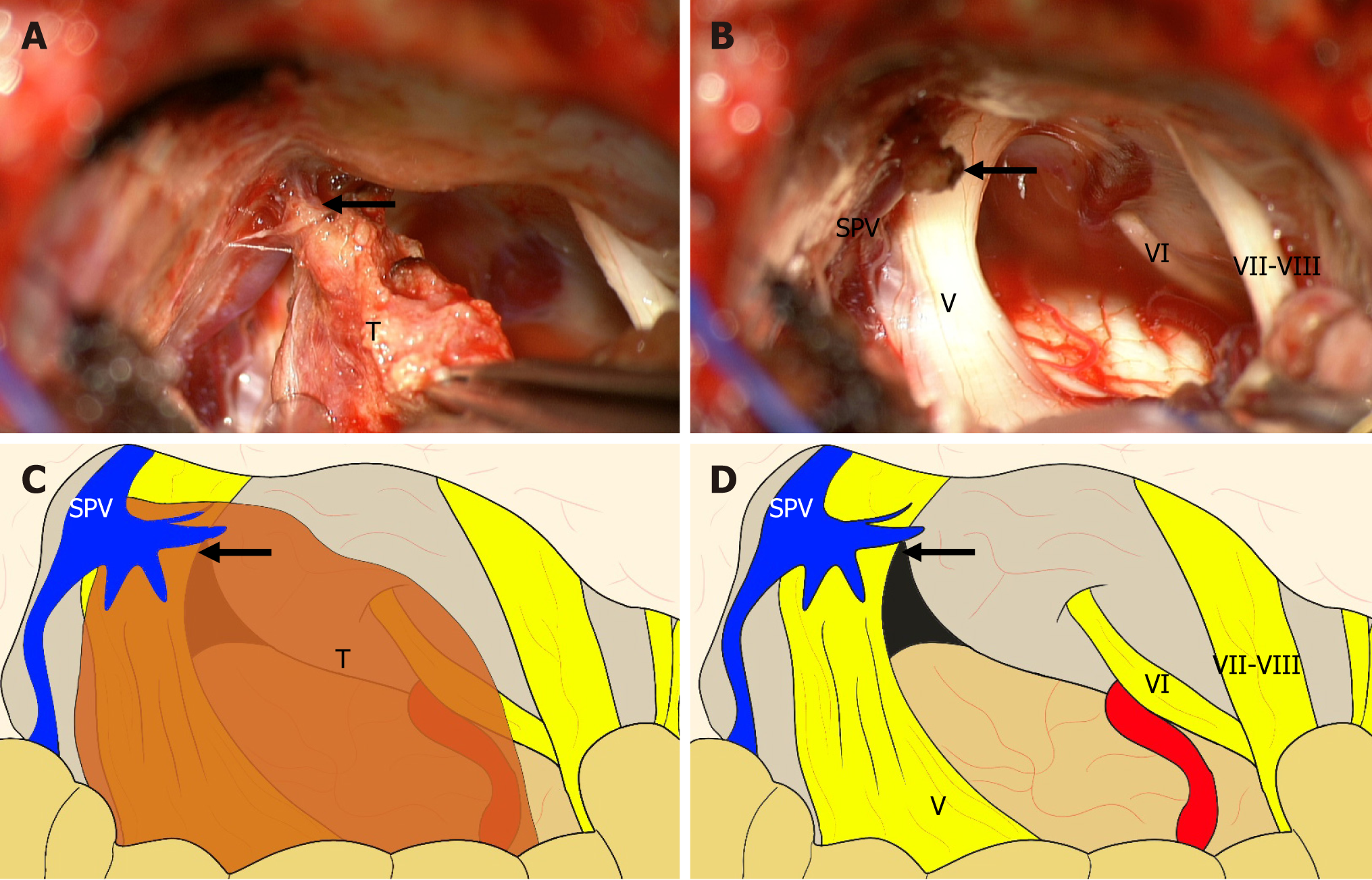
Tumor resection was performed using a right ileocecal approach. After opening the dura mater, a tumor was identified with the posteroinferior displacement of the 7-8th nerve complex. A dural attachment was not seen at the tentorium or posterior surface of the petrous pyramid. The tumor was firmly adherent to the vascular pedicle of the superior petrosal vein (Figure 2). The tumor was dissected from the surrounding structure and completely removed. The site of origin was cauterized and resected with the preservation of the superior petrosal vein. All other neurovascular structures were also preserved. Postoperative imaging showed complete removal of the tumor (Figure 1F).
A histopathologic examination of hematoxylin and eosin-staining of the tumor tissue showed spindly cells with pink cytoplasm in short fascicles, forming syncytial structures and whorls, without mitoses, necrosis, or invasion. Immunohistochemistry was positive for epithelial membrane antigen and vimentin and negative for glial fibrillary acidic protein. The Ki-67 (MIB-1) labeling index was low (1%–2%). The features were consistent with meningothelial meningioma, World Health Organization Grade I. Transient paradoxical cerebrospinal fluid rhinorrhea occurred but subsided after lumbar drainage for three days. The patient’s headache and tinnitus gradually disappeared, and a recurrence was not observed five years after the surgery.
The origin of meningiomas is thought to be arachnoidal (arachnoid cap or meningothelial) cells based on the histological and ultrastructural similarities between meningioma cells and meningioma cells[3,4]. These cells exist in the arachnoid layer and Pacchionian granulation. The contiguity of the arachnoid and granulation to the dura mater presumably explains the typical origin site of meningiomas.
MRI is the state of art in the preoperative diagnosis of meningiomas. CPA MWODA should be discriminated from medulloblastoma, ependymoma, and lymphoma. The radiologic features of meningiomas show low- or iso-intensity signals on T1-weighted MRI, iso- or high-intensity signals on T2-weighted MRI, and homogenous enhancement[5]. Advanced MRI technique can be an additional option to support the diagnosis of brain meningioma. MR perfusion typically demonstrated high rCBV. The typical findings on MR spectroscopy are elevated choline and alanine with diminished N-acetylaspartate[6,7].
The stroma of the choroid plexus, tela choroidea, and the leptomeninges surrounding the ventricular region, pineal region, and Sylvian fissure also have arachnoidal cells, accounting for the development of the MWODA[8,9]. Considering previous studies and operative findings, the arachnoidal cells of the leptomeninges in the Virchow-Robin spaces along the superior petrosal vein might be considered the origin of the meningioma in the presenting case.
Cushing and Eisenhardt first classified MWODA, according to the site of the tumors. Since that time, many case studies have reported MWODA occurring in various sites, making classification less important. Basically, meningiomas can occur anywhere arachnoidal cells are present, including supratentorial (intraventricular, intraparenchymal, pineal region, or Sylvian) and infratentorial (intraventricular, intraparenchymal, cisterna magna, or inferior tela choroidea) locations[9]. Even considering the classifications and reports to date, our case is anatomically quite different from the previous cases and is a unique case of MWODA located in the pontocerebellar cistern.
Before open surgery, it is difficult to know whether a meningioma is attached to the dura or not. Because there are no typical features on brain imaging, the preoperative diagnosis of MWODA is difficult. The dural tail sign is not always present in meningioma in general and is seen in less than 80% of the cases[10]. Considering the demographic difference, it is still difficult to determine the presence of dural attachment before surgery. The average age of the patients with MWODA is about 20 years younger than that of patients with meningioma in general. MWODA tends to occur more in men than in women, differing from meningioma in general, which is more prevalent in women[2]. Except for intraventricular meningiomas, MWODA tends to these features, but this is not always the case. In our case, there was no obvious dural tail sign, and the patient was a 44-year-old woman. However, these features were not sufficient to diagnosis MWODA.
The absence of dural attachment makes it easy to completely resect such tumors. Total surgical removal is the treatment of choice for all meningiomas if they can be performed without significant complications. It is important to both preserve the surrounding neurovascular structures and completely remove the tumor. Meningioma recurrence often occurs at the original site and is usually caused by incomplete removal[11]. Moreover, since tumor stem cells may be present in the microvessels, vessels related to the tumor should be removed carefully while maintaining the patency of the important blood vessels[12]. The meningioma within the pontocerebellar cistern could be completely removed by the retrosigmoid approach with the preservation of the cranial nerves. Unlike cerebellopontine meningiomas, the tumor was not attached to the petrous pyramid and was firmly adhered to the vascular pedicle of the superior petrosal vein, demonstrating that the tumor might be derived from the Virchow-Robin space of the superior petrosal vein. We could cauterize and resect the origin site of the tumor to completely remove the tumor while maintaining the patency of the superior petrosal vein.
Meningioma originating from the superior petrosal vein is extremely rare. It is difficult to know whether the tumor is attached to the dura or other sites such as the petrosal vein before surgery. However, the absence of dural attachment makes it easy to completely resect such tumors. Furthermore, vessels related to the tumor should be removed carefully while maintaining the patency of the important blood vessels, considering the possible presence of tumor stem cells in the microvessels.
| 1. | Chiocca EA, Boviatsis EJ, Westmark RM, Short MP, Richardson EP, Zervas NT. Deep sylvian fissure meningioma without dural attachment in an adult: case report. Neurosurgery. 1994;35:944-6; discussion 946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Zhang J, Chi LY, Meng B, Li F, Zhu SG. Meningioma without dural attachment: case report, classification, and review of the literature. Surg Neurol. 2007;67:535-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Yamashima T. On Arachnoid Villi and Meningiomas: Functional Implication of Ultrastructure, Cell Adhesion Mechanisms, and Extracellular Matrix Composition. Pathol Oncol Res. 1996;2:144-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Yamashima T, Kida S, Yamamoto S. Ultrastructural comparison of arachnoid villi and meningiomas in man. Mod Pathol. 1988;1:224-234. [PubMed] |
| 5. | Matias TB, Cordeiro RA, Duarte JA, de Jarry VM, Appenzeller S, Villarinho L, Reis F. Immune-Mediated Hypertrophic Pachymeningitis and its Mimickers: Magnetic Resonance Imaging Findings. Acad Radiol. 2023;30:2696-2706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 18] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 6. | de Amorim JC, Torricelli AK, Frittoli RB, Lapa AT, Dertkigil SSJ, Reis F, Costallat LT, França Junior MC, Appenzeller S. Mimickers of neuropsychiatric manifestations in systemic lupus erythematosus. Best Pract Res Clin Rheumatol. 2018;32:623-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Ginsberg LE. Radiology of meningiomas. J Neurooncol. 1996;29:229-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Kohta M, Sasayama T, Nakai T, Taniguchi M, Nagashima H, Tanaka K, Mizukawa K, Itoh T, Kohmura E. Cisterna magna meningiomas without dural attachment: Report of two cases. Neurol Neurochir Pol. 2017;51:247-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Brogna C, Lavrador JP, Patel S, Ribas EC, Aizpurua M, Vergani F, Ashkan K, Bhangoo R. Grade II Sylvian fissure meningiomas without dural attachment: case report and review of the literature. CNS Oncol. 2018;7:CNS20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Doddamani RS, Meena RK, Sawarkar D. Ambiguity in the Dural Tail Sign on MRI. Surg Neurol Int. 2018;9:62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Boylan SE, McCunniff AJ. Recurrent meningioma. Cancer. 1988;61:1447-1452. [PubMed] [DOI] [Full Text] |
| 12. | Shivapathasundram G, Wickremesekera AC, Brasch HD, Marsh R, Tan ST, Itinteang T. Expression of Embryonic Stem Cell Markers on the Microvessels of WHO Grade I Meningioma. Front Surg. 2018;5:65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |