Published online Jun 16, 2024. doi: 10.12998/wjcc.v12.i17.3138
Revised: March 25, 2024
Accepted: April 16, 2024
Published online: June 16, 2024
Processing time: 144 Days and 3 Hours
Salivary gland tumors are relatively rare. Most minor salivary gland tumors are malignant with benign tumors accounting for 18% of the tumors. Pleomorphic adenoma (PA) is the most common salivary gland tumor. Lip PA is uncommon with 9.8% occurring in the upper lip. We are adding on the knowledge of the rare upper lip PA (benign mixed tumor).
We report an upper lip PA (benign mixed tumor) in a 28-year-old man. His com
Blunt dissection is indicated to preserve the cosmesis and function of the upper lip.
Core Tip: Salivary gland tumors are relatively rare. Pleomorphic adenoma (PA) (benign mixed tumor) is the most common benign tumor of the salivary glands. It comprises about 3%-10% of all head and neck tumors and 50% of the major and minor salivary gland neoplasms. Among minor salivary gland tumors, the palate is the most common site of predilection (42.8%-68.8%), followed by the upper lip (15%-20%). PA of the upper lip is relatively rare. Our case report is on the clinical presentation, histopathology, and management of PA (benign mixed tumor) of the upper lip.
- Citation: Chidzonga MM, Mahomva L, Zambuko B, Muungani W. Pleomorphic adenoma (mixed tumor) of the upper lip: A case report. World J Clin Cases 2024; 12(17): 3138-3143
- URL: https://www.wjgnet.com/2307-8960/full/v12/i17/3138.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i17.3138
Pleomorphic adenoma (PA), or mixed tumor, is the most common benign tumor of the salivary glands. In the head and neck area, it comprises about 3%-10% of all head and neck tumors and 50% of the major and minor salivary gland neo
We are reporting a 28-year-old man who presented with a PA of the upper lip that had been growing slowly for the past year.
A 28-year-old male patient presented at our Oral and Maxillofacial Surgery Clinic with a chief complaint of a painless swelling on the left side of the upper lip.
The swelling had been growing slowly for the past 3 years.
There was no history of trauma.
The patient’s medical, dental, and family history was non-contributory.
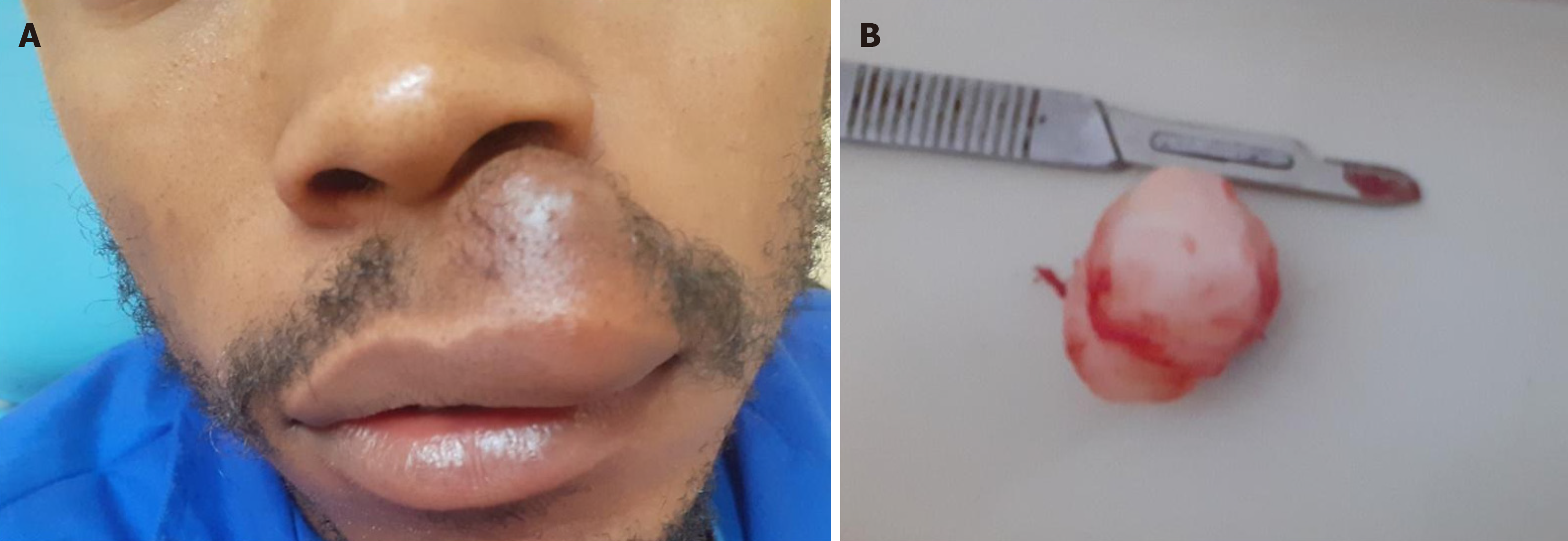
The tumor appeared to be superficial to the orbicularis oris muscle as the patient had a full mouth opening with no asymmetry or limitation. Extra oral examination showed a painless, well-circumscribed tumor, slightly mobile, sessile, nodular, and rubbery (in consistency) tumor measuring 5.0 cm × 2.0 cm (Figure 1A). The overlying skin was of normal color.
The skin over the tumor was not fixed. There was no ulceration, and palpation did not elicit pain, fluctuation, or bleed
Histopathology examination confirmed the lesion as a PA (benign mixed tumor).
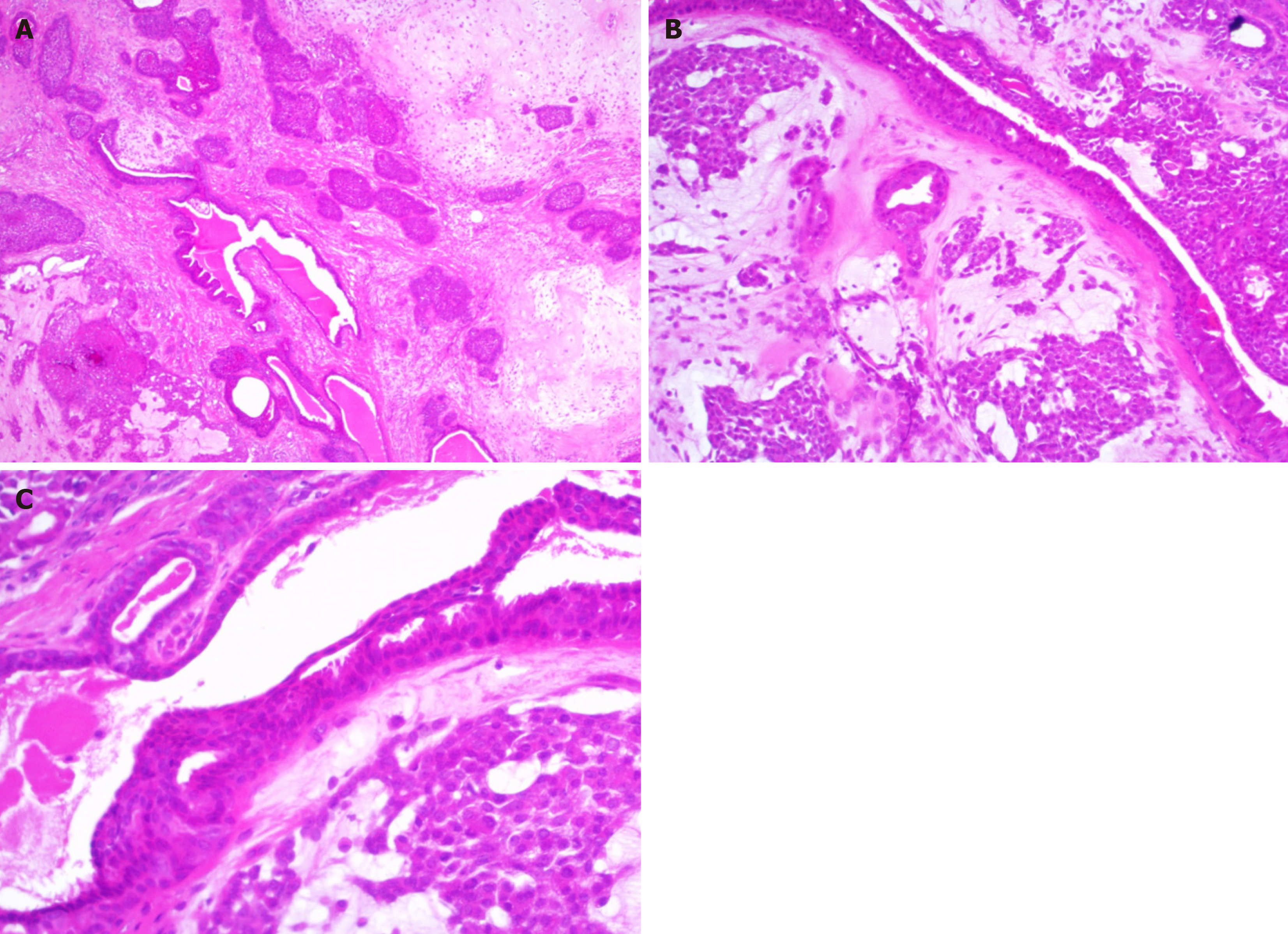
The tumor was excised under local anesthesia using 2% lignocaine with 1:100000 adrenaline hydrochloride. Lignocaine was injected around the tumor and a 4.0-cm-long incision was made over the middle of the vermilion border. Blunt dissection was used to excise the tumor. The excised tumor was nodular, whitish, and encapsulated (Figure 1B). The incision site was closed using Vicryl 4/0. The patient tolerated the procedure well. The surgical specimen was sent to a histopathology laboratory for examination. Macroscopically, the firm whitish tissue measured 3.5 cm × 2.5 cm × 2.0 cm, weighing 7.5 g. Microscopic examination (Figure 2) showed a well-circumscribed and partly encapsulated lesion that is biphasic. Large lobules of myxo-chondroid stroma and intervening cellular nodules of basaloid cells that are rather co
The 3-mo post-surgery review showed that satisfactory healing had been achieved and the patient was pleased by the appearance of his lip.
The average size of lip PAs was 1.5 ± 0.7 cm (range, 0.7-2.2 cm). PA (benign mixed tumor) is the most common benign tumor of the major salivary glands with a predilection for the parotid glands. Minor salivary gland tumors, benign and malignant, constitute 18% of salivary gland tumors[7,8]. However, tumors in the minor salivary glands are uncommon, with PA accounting for nearly 40% of them, and common in the palate[7]. PA has a female preponderance in the third and fourth decades with an average of 33.2 years. In our case, the upper lip PA developed in a 28-year-old man. This is in keeping with the occurrence of upper lip PA in young patients. PA of the lip with external cutaneous skin involvement but with no mucosal involvement is extremely rare[8,9]. This is similar to our case which had no oral involvement. The upper lip has a propensity for benign tumors as opposed to the lower lip where malignant tumors are more common. PA on the lip is more common in the upper lip than in the lower lip with a ratio of 6:1[7,10]. However, this tends to vary with centers where the report comes from[8,11,12]. Umemori et al[12] found that 11.8% of the PAs occurred on the lips, of which 9.8% were distributed on the upper lip and 2.0% on the lower lip. For preoperative diagnostic assistance, ultra
There are few reports on upper lip PA in the literature. Our case report adds to the knowledge of the clinical presentation, diagnosis, and management of upper lip PA.
Gratitude to Mr. Sibve for the photography.
| 1. | Sharma NK, Singh AK, Pandey A, Verma V. Pleomorphic adenoma involving soft tissue overlying the anterior border of ramus of the mandible: A rare ectopic presentation. J Oral Biol Craniofac Res. 2016;6:S62-S64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Singh AK, Kumar N, Sharma P, Singh S. Pleomorphic adenoma involving minor salivary glands of upper lip: A rare phenomenon. J Cancer Res Ther. 2015;11:1025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Vegari S, Naderpour M, Hemmati A, Baybordi H. Pleomorphic adenoma of the cervical heterotopic salivary gland: a case report. Case Rep Otolaryngol. 2012;2012:470652. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Abdelhamid AS, Elzayat S, Essa AA, Elsherief H, Amer M. Pleomorphic adenoma of the cheek: a case presentation. Egypt J Otolaryngol. 2022;38:165. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Singh G, Prinja S, Aarushi. Pleomorphic adenoma of head and neck region: our institutional review. Int J Otorhinolaryngol Head Neck Surg. 2019;5:1522-1526. [DOI] [Full Text] |
| 6. | Almeslet AS. Pleomorphic Adenoma: A Systematic Review. Int J Clin Pediatr Dent. 2020;13:284-287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 47] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 7. | Taiwo AO, Akinshipo A, Braimah RO, Ibikunle AA. Pleomorphic Adenoma of the Upper Lip: A Case Report. Saudi J Med Med Sci. 2018;6:32-35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Gelidan AG, Arab K. Rare upper lip pleomorphic adenoma presents as cutaneous skin lesion: Case report. Int J Surg Case Rep. 2021;85:106142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Suka N, Magoshi S, Ogasawara Y. Pleomorphic adenoma of in the upper lip: a case report and literature review. J Meikai Dent Med. 2021;50:59-65. |
| 10. | Ali I, Gupta AK, Singh S. Pleomorphic adenoma of the upper lip. Natl J Maxillofac Surg. 2011;2:219-221. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Kazikdas KC, Yalcinozan ET, Dirik MA. Pleomorphic adenoma of the upper lip. Natl J Maxillofac Surg. 2020;11:110-112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Umemori K, Ono K, Kanemoto H, Obata K, Kawai H, Nakamura T, Nakano K, Ibaragi S, Nagatsuka H, Sasaki A. Lip pleomorphic adenomas: case series and literature review. Gland Surg. 2022;11:1730-1740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (1)] |