Published online Jun 16, 2024. doi: 10.12998/wjcc.v12.i17.3086
Revised: April 11, 2024
Accepted: April 23, 2024
Published online: June 16, 2024
Processing time: 105 Days and 5 Hours
Patients with Parkinson’s disease (PD) often experience depression, and some may require magnetic resonance imaging (MRI) for diagnosis, which can lead to MRI failure due to claustrophobia.
To explore the value of psychological interventions in successfully completing functional MRI scans of the brain for PD-related depression.
Ninety-six patients with PD were randomly divided into two groups. The control group (47 patients) received general care, and the experimental group (49 pa
Before scanning, no statistically significant difference was observed between the two groups in terms of heart rate, systolic blood pressure, and UPDRS, HAMD, GDS-15, and MRI-AQ scores. After scanning, systolic blood pressure, MRI-AQ score, and scan time in the experimental group were significantly lower than those in the control group, whereas the scan completion rate and image quality score were significantly higher than those in the control group.
Psychological nursing interventions are helpful in alleviating PD-related depression and assessing MR depression scores and may be helpful in the successful completion of functional MRI scans of the patient's brain.
Core Tip: This study investigates the prevalence of depression among Parkinson’s disease (PD) patients, highlighting its significant impact on psychological well-being. Functional magnetic resonance imaging (MRI) plays a crucial role in PD diagnosis, yet patients often experience anxiety during scans due to unfamiliarity and discomfort. Psychological nursing interventions can alleviate anxiety, enhancing patients' ability to undergo MRI scans successfully. The study reveals correlations between anxiety levels, PD severity, and MRI-related depression scores. Psychological nursing significantly reduces blood pressure spikes post-scan and improves completion rates and image quality. Despite limitations like small sample sizes, multi-center studies are proposed for future validation of findings.
- Citation: Zhang XX, Zhang XH, Dong YC. Effects of psychological nursing in Parkinson's related depression patients undergoing functional magnetic resonance imaging: A randomized controlled trial. World J Clin Cases 2024; 12(17): 3086-3093
- URL: https://www.wjgnet.com/2307-8960/full/v12/i17/3086.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i17.3086
Parkinson's disease (PD) is a common chronic degenerative disease of the nervous system in the elderly and is characterized by motor dysfunctions, such as static tremor, motor retardation, muscle rigidity, and postural gait abnormalities[1,2]. Research shows that PD not only manifests as a movement disorder but is also accompanied by anxiety, depression, insomnia, cognitive dysfunction, and other non-movement symptoms[3]. Among these, depression and cognitive im
Currently, the main clinical diagnosis of PD depends on clinical symptoms and physical examination, and the com
For patients to successfully complete MR scanning, effective psychological intervention measures during examinations should be implemented. An important part of psychological nursing interventions is the establishment of harmonious interpersonal relationships between nursing staff and patients. Nurses should engage in proactive communication with patients before the examination, explain basic knowledge of MR scanning and related precautions, and dispel patients' fears and concerns, thereby helping patients relax physically and mentally and alleviating adverse emotions. Nurses should also cooperate with inspectors to ensure a successful completion of the functional MRI examination. This study aimed to explore the value of implementing psychological interventions to help patients with PD-related depression in completing MRI scans and to provide guidance for patients with PD to successfully navigate the MRI scanning process.
A total of 96 patients with PD admitted to our hospital between March 2017 and July 2021 were divided into two groups using a random-number generator. The control group consisted of 47 patients (female/male = 21/26) aged 54-73 years, while the experimental group consisted of 49 patients (female/male = 20/29) aged 58-71 years. This study was conducted after review and approval by the hospital’s medical ethics committee.
The inclusion criteria were as follows: (1) Compliance with the diagnostic criteria for PD-related depression and use of the Unified Parkinson's Disease Assessment Scale (UPDRS), Hamilton Depression Scale (HAMD), and 15 items of the Geriatric Depression Scale (GDS-15) to make a diagnosis; (2) undergoing magnetic resonance examination for the first time; and (3) voluntarily participation in the study and cooperation in completing various questionnaires. Exclusion cri
All patients were treated using the same GE Signa EXCIE1.5T superconducting MR machine with an 8-channel head coil. The magnet's dimensions were 172 cm in length, 244 cm in longitudinal movement range, with a 60 cm aperture. The room was illuminated with warm-colored lighting to ensure ventilation, maintaining a temperature range of 20–25℃. The MRI machine was equipped with light lamps, head coils with mirrors, air-conduction earphones, and alarm balloons. Transverse-axis ESWAN and DTI images were obtained for each patient. The normal scanning duration was 14 min 22 s (3D FSPGR: 3 min 12 s; DTI: 4 min 57 s; ESWAN: 5 min 49 s; positioning image and uniform field correction: 24 s)[11,12]. The control group received routine nursing care, whereas the observation group received psychological care based on routine nursing care.
Routine care: The scanning room was equipped with adjustable lighting, ventilation fans, mirrors, alarm balloons, and air-conduction earphones, and the operating room was equipped with a music player, scanning rack, and speaker. MRI was performed using a GE 1.5T superconducting magnetic resonance imaging instrument. The control group received only routine care which involved informing patients about the need to remove gold and silver accessories and metal ob
Psychological care: His involved actively contacting the patients before the examination, avoiding the use of professional terminology when communicating with the patient, maintaining an easygoing communication with the patient, familiarizing the patient with the scanning area, detailing the MRI process, encouraging deep breathing and short rests before the examination, encouraging the patients to eat and drink a small amount of water, addressing questions from the patient and their families, and alleviating fear, anxiety and other psychological concerns to establish a closer relationship between nurses and patients[13]. Understanding the experience of patients suffering from claustrophobia will help them identify the causes of their condition and understand that it is possible to overcome claustrophobia. With the help of text, pictures, videos, and other methods, patients can acquire pathological knowledge related to claustrophobia and be in
Vital signs: Heart rate and systolic blood pressure of both patient groups were recorded before and after the MRI exa
UPDRS, HAMD, GDS, and MRI Anxiety Questionnaire scores were recorded before and after the scan in both patient groups[16].
The number of patients in both groups that underwent MRI examinations, the scan success rate, and the time required for the patients to complete the scans were recorded. Image quality was assessed using a Likert Scale 5-level scoring me
Statistical analysis was performed using SPSS 22 software. Measurement data were expressed as mean ± SD. Indepen
The results of age comparison between the two groups showed no significant difference (control group: 65.06 ± 5.02 vs experimental group: 63.78 ± 4.24, t = 1.347, P = 0.181). Gender composition ratio also showed no statistical difference (χ2 = 0.146, P = 0.702).
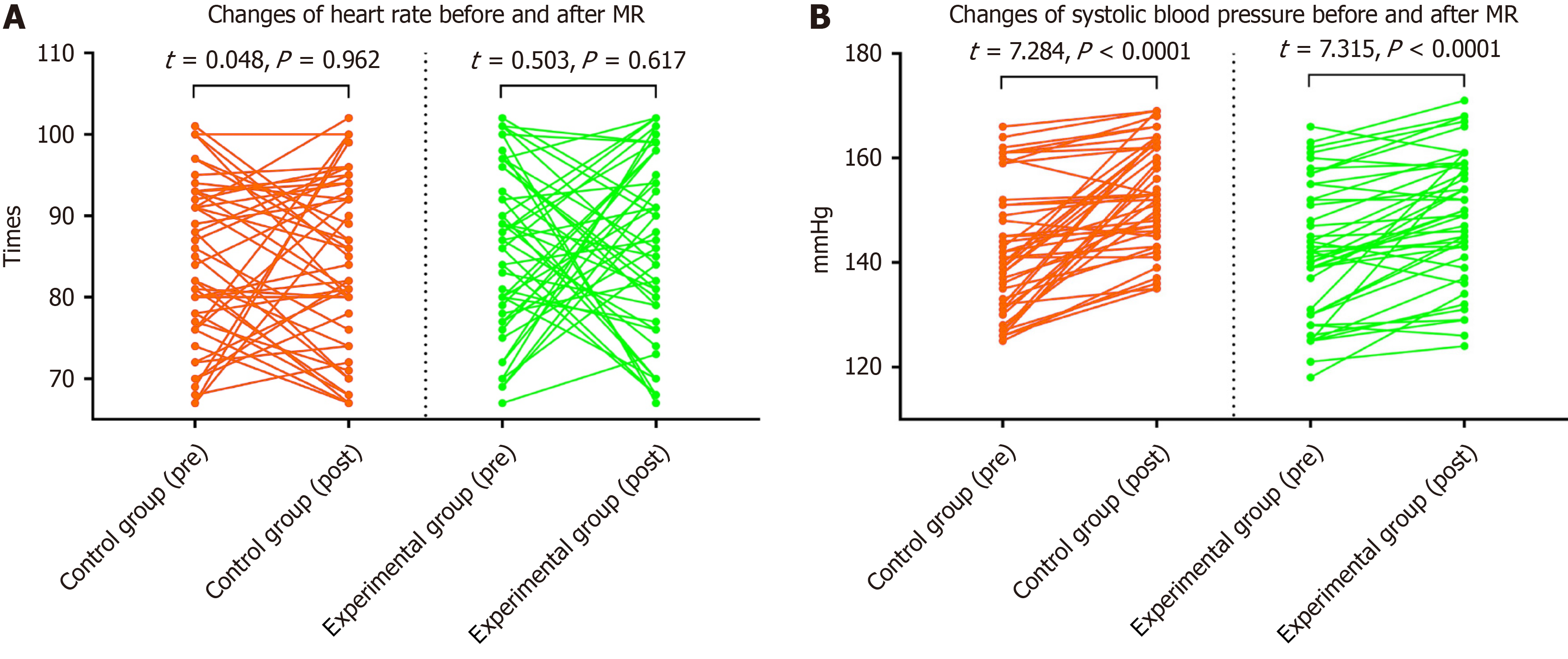
There was no statistically significant difference in heart rate and systolic blood pressure between the two groups before scanning (control group: 84.24 ± 9.88 vs experimental group: 85.37 ± 10.17, t = 0.542, P = 0.589), (control group: 141.89 ± 11.98 vs experimental group: 142.31 ± 13.02, t = 0.160, P = 0.874). After scanning, there was no statistically significant difference in heart rate between the two groups (control group: 84.33 ± 10.46 vs experimental group: 86.53 ± 10.90, t = 0.994, P = 0.323); however, the systolic blood pressure in the control group was significantly higher than that in the ex
The intragroup comparison showed no statistical difference in heart rate before and after scanning between the experimental and control groups. However, both groups exhibited significantly higher systolic blood pressure after scanning than before scanning, with significant differences, as shown in Figure 1. The incidence of a 20 mmHg increase in systolic blood pressure in the control group was 34.04% (16/47), significantly higher than the 4.08% (2/49) incidence of a 20 mmHg increase in systolic blood pressure in the experimental group, with a statistically significant difference (χ2 = 14.135, P < 0.001).
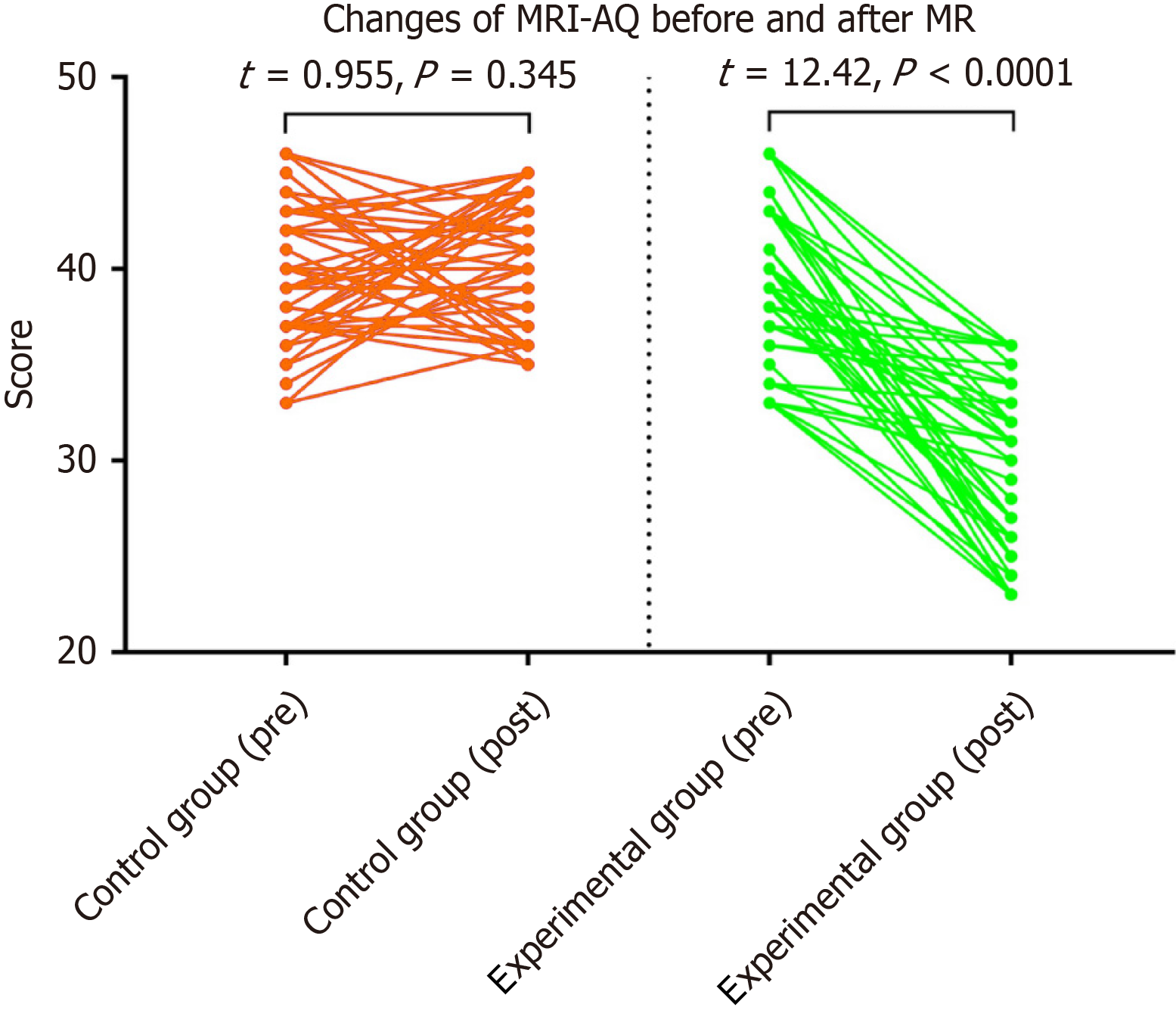
The results showed that there was no statistical difference in the UPDRS, HAMD, GDS - 15, and MRI-anxiety ques
| Scores | Control | Experiment | t | P value |
| UPDRS III | 32.340 ± 3.252 | 32.265 ± 3.696 | 0.106 | 0.916 |
| HAMD | 15.915 ± 5.111 | 14.878 ± 4.952 | 1.01 | 0.315 |
| GDS-15 | 8.809 ± 1.393 | 9.102 ± 1.342 | -1.051 | 0.296 |
| MRI-AQ (pre) | 39.596 ± 3.616 | 39.245 ± 4.121 | 0.443 | 0.659 |
| MRI-AQ (post) | 40.340 ± 3.447 | 29.449 ± 4.505 | 13.263 | < 0.001 |
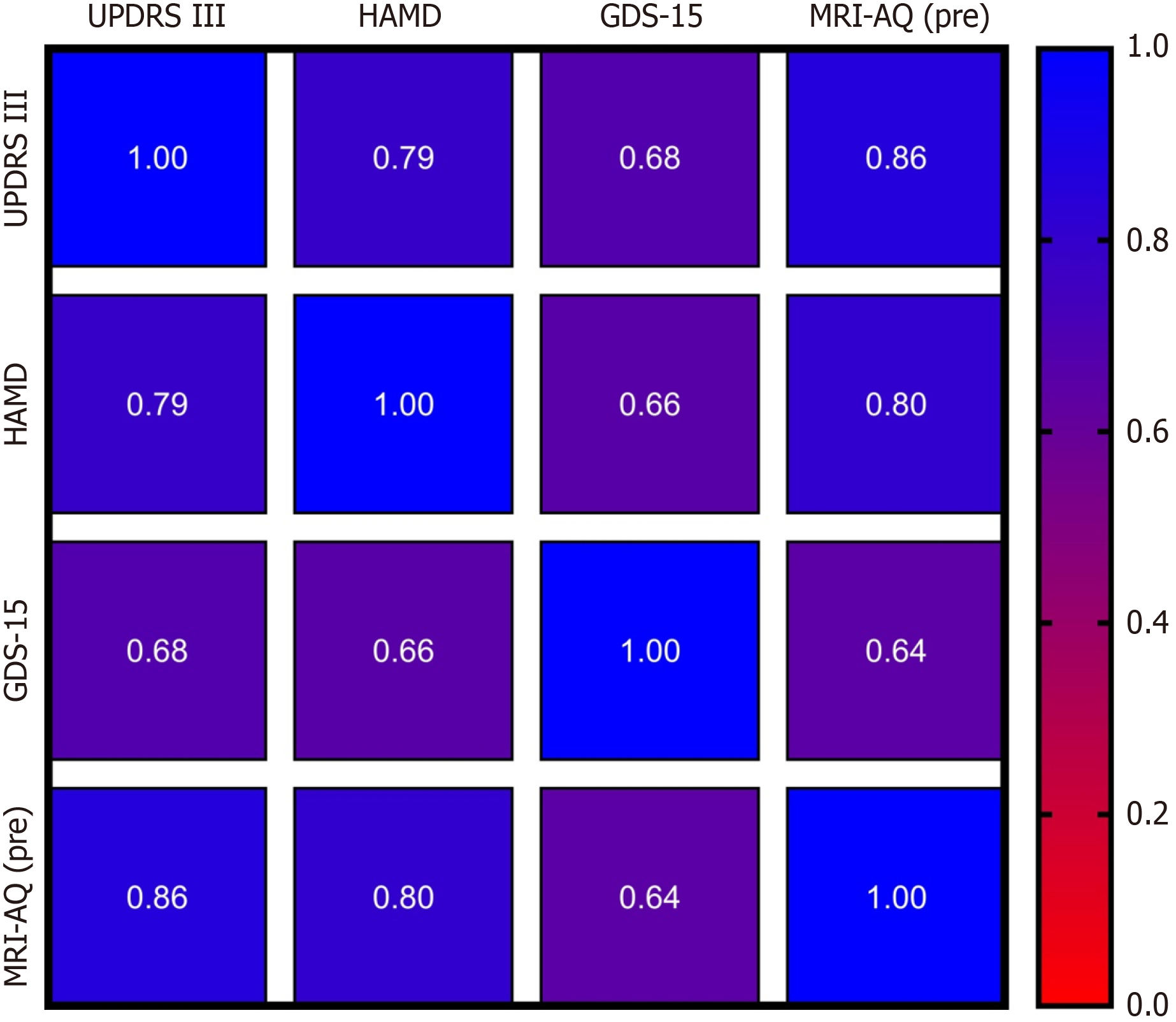
The MRI-AQ (pre) was positively correlated with the UPDRS and HAMD scores, with correlation coefficients of 0.86 and 0.80, respectively. The correlation with the GDS-15 was poor (r = 0.64), as shown in Figure 3.
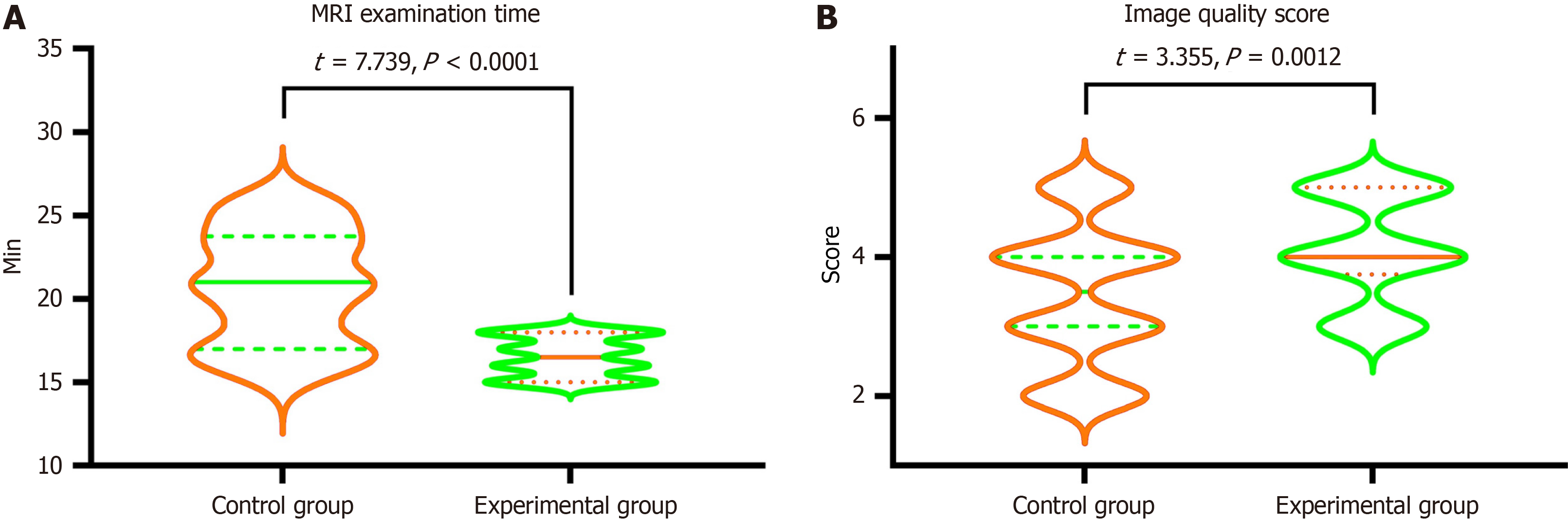
The completion rate of magnetic resonance scanning in the control group was 76.60% (36/47), whereas, in the experimental group, it was significantly higher at 93.88% (46/49), indicating a statistically significant difference (χ2 = 5.752, P = 0.016). The MRI scanning duration of the control group was significantly higher than that of the experimental group, while the image quality score of the control group was significantly lower than that of the experimental group, with sta
Among the clinical symptoms of patients with PD, depression is more common and has a serious impact on psychological status and quality of life. Functional MRI is a particularly important method for diagnosing and evaluating the severity of PD. Currently, there are many studies on functional MR for PD-related depression[17-20]. However, patients with PD may feel uncomfortable and anxious due to unfamiliar equipment, sounds, and examinations. In addition, functional MR scans often take longer[21,22], and during the examination process, patients may feel "buried alive" or "abandoned.” This results in involuntary motion, motion artifacts, decreased image quality, prolonged image post-processing time, and an inability to provide effective coordination.
Regarding the factors that cause anxiety during MR scanning, it is considered that the first factor is related to the patient's PD condition, leading to PD-related depression. The higher the anxiety score of patients with PD, the more likely they were to experience anxiety during MR scanning. Our research results also show that MRI-AQ (pre) is positively correlated with both UPDRS and HAMD. It was also confirmed that the more severe the PD and the higher the HAMD score, the higher the MR-related depression score. However, the slightly poor correlation between MRI-AQ (pre) and GDS-15 may be related to lower GDS-15 discrimination, resulting in a poor correlation between GDS-15 and MRI-AQ (pre), UPDRS, and HAMD. In addition, during the MR scanning process, examination equipment and environment are important factors that cause anxiety in patients with PD. The MRI examination equipment and the examination envi
To alleviate patient anxiety, it is crucial to first address PD-related depression. Psychological care can significantly improve the anxiety levels of patients undergoing MR scanning. The psychological nursing intervention in our study involved improving cognitive and situational stimuli and family support, establishing harmonious interpersonal re
This study found that there was no statistically significant difference between the heart rate before and after exami
In addition, through the application of psychological nursing adjustment, the patients’ MRI-AQ score was significantly lower after the examination than before the examination. It was also confirmed that psychological nursing could help alleviate the anxiety state of patients with PD during magnetic resonance examination, alleviate the pressure on patients during MR scanning, and help patients smoothly complete the magnetic resonance examination. Our results also showed that the completion rate of MR scanning was significantly higher in the experimental group than in the control group. Another result also confirmed that after psychological care, the MR scanning time was significantly shortened, and the MR image quality score increased. On the other hand, it confirmed that psychological care contributed to the smooth completion of functional MRI examinations.
Our study had certain limitations. First, this was a single-center, small-sample size study, potentially limiting the generalizability of the findings. Additionally, the data primarily relied on patient-reported questionnaire responses, which could introduce certain cognitive biases and consequently affect the scoring data. However, in the future, we plan to carry out multi-center and large-sample studies to obtain more robust data.
In summary, the use of the MRI-AQ to score PD-related depression on MR scans was effective. Psychological care can help patients with PD-related depression successfully complete MR scans, shorten examination time, and improve MRI scores.
| 1. | Li A, Li C. Detecting Parkinson's Disease through Gait Measures Using Machine Learning. Diagnostics (Basel). 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 2. | Yang XX, Yang R, Zhang F. Role of Nrf2 in Parkinson's Disease: Toward New Perspectives. Front Pharmacol. 2022;13:919233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 3. | Seppi K, Ray Chaudhuri K, Coelho M, Fox SH, Katzenschlager R, Perez Lloret S, Weintraub D, Sampaio C; the collaborators of the Parkinson's Disease Update on Non-Motor Symptoms Study Group on behalf of the Movement Disorders Society Evidence-Based Medicine Committee. Update on treatments for nonmotor symptoms of Parkinson's disease-an evidence-based medicine review. Mov Disord. 2019;34:180-198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 652] [Cited by in RCA: 633] [Article Influence: 105.5] [Reference Citation Analysis (0)] |
| 4. | Baik K, Kim SM, Jung JH, Lee YH, Chung SJ, Yoo HS, Ye BS, Lee PH, Sohn YH, Kang SW, Kang SY. Donepezil for mild cognitive impairment in Parkinson's disease. Sci Rep. 2021;11:4734. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Wang Y, Bai LP, Liu W, Zhu XD, Zhang XY. Altered BDNF levels are associated with cognitive impairment in Parkinson's disease patients with depression. Parkinsonism Relat Disord. 2022;103:122-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 6. | Radhakrishnan DM, Goyal V. Parkinson's disease: A review. Neurol India. 2018;66:S26-S35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 100] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 7. | Bartl M, Dakna M, Schade S, Wicke T, Lang E, Ebentheuer J, Weber S, Trenkwalder C, Mollenhauer B. Longitudinal Change and Progression Indicators Using the Movement Disorder Society-Unified Parkinson's Disease Rating Scale in Two Independent Cohorts with Early Parkinson's Disease. J Parkinsons Dis. 2022;12:437-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 8. | Watanabe H, Dijkstra JM, Nagatsu T. Parkinson's Disease: Cells Succumbing to Lifelong Dopamine-Related Oxidative Stress and Other Bioenergetic Challenges. Int J Mol Sci. 2024;25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 9. | Tolosa E, Garrido A, Scholz SW, Poewe W. Challenges in the diagnosis of Parkinson's disease. Lancet Neurol. 2021;20:385-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 833] [Article Influence: 208.3] [Reference Citation Analysis (0)] |
| 10. | Al-Shemmari AF, Herbland A, Akudjedu TN, Lawal O. Radiographer's confidence in managing patients with claustrophobia during magnetic resonance imaging. Radiography (Lond). 2022;28:148-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 11. | Ling X, Tang W, Liu G, Huang L, Li B, Li X, Liu S, Xu J. Assessment of brain maturation in the preterm infants using diffusion tensor imaging (DTI) and enhanced T2 star weighted angiography (ESWAN). Eur J Radiol. 2013;82:e476-e483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Wang C, Fan G, Xu K, Wang S. Quantitative assessment of iron deposition in the midbrain using 3D-enhanced T2 star weighted angiography (ESWAN): a preliminary cross-sectional study of 20 Parkinson's disease patients. Magn Reson Imaging. 2013;31:1068-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Chadderdon AL, Carns DR, Pudalov LR, McKernan LC, Honce JM. Underlying Mechanisms of Psychological Interventions in Magnetic Resonance Imaging and Image-Guided Radiology Procedures. Top Magn Reson Imaging. 2020;29:157-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Zaidi SAR, Masood K, Khanzada U, Adil SO, Hussain M. Strategies to cope claustrophobia during magnetic resonance imaging examination. Int J Res Med Sci. 2019;7:1166. [DOI] [Full Text] |
| 15. | Rizzo S, Ferrera N, Pravatà E, Guggenberger R, Stern S, Del Grande F. Is hypnosis a valid alternative to spontaneous breathing general anesthesia for claustrophobic patients undergoing MR exams? A preliminary retrospective study. Insights Imaging. 2021;12:83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Ahlander BM, Årestedt K, Engvall J, Maret E, Ericsson E. Development and validation of a questionnaire evaluating patient anxiety during Magnetic Resonance Imaging: the Magnetic Resonance Imaging-Anxiety Questionnaire (MRI-AQ). J Adv Nurs. 2016;72:1368-1380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 17. | Huang S, Dong Y, Zhao J. The mean kurtosis (MK) is more sensitive diagnostic biomarker than fractional anisotropy (FA) for Parkinson's disease: A diagnostic performance study and meta-analysis. Medicine (Baltimore). 2022;101:e31312. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 18. | Li Z, Liu W, Xiao C, Wang X, Zhang X, Yu M, Hu X, Qian L. Abnormal white matter microstructures in Parkinson's disease and comorbid depression: A whole-brain diffusion tensor imaging study. Neurosci Lett. 2020;735:135238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Liu Z, Su D, Ma L, Chen H, Fang J, Ma H, Zhou J, Feng T. The altered multiscale dynamics of spontaneous brain activity in depression with Parkinson's disease. Neurol Sci. 2022;43:4211-4219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 20. | Wang M, Liao H, Shen Q, Cai S, Zhang H, Xiang Y, Liu S, Wang T, Zi Y, Mao Z, Tan C. Changed Resting-State Brain Signal in Parkinson's Patients With Mild Depression. Front Neurol. 2020;11:28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Buchwitz TM, Ruppert-Junck MC, Greuel A, Maier F, Thieken F, Jakobs V, Eggers C. Exploring impaired self-awareness of motor symptoms in Parkinson's disease: Resting-state fMRI correlates and the connection to mindfulness. PLoS One. 2023;18:e0279722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Dong Y, Liu D, Zhao Y, Yuan Y, Wang W, Wu S, Liang X, Wang Z, Liu L. Assessment of Neuroprotective Effects of Low-Intensity Transcranial Ultrasound Stimulation in a Parkinson's Disease Rat Model by Fractional Anisotropy and Relaxation Time T2(∗) Value. Front Neurosci. 2021;15:590354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Tazegul G, Etcioglu E, Yildiz F, Yildiz R, Tuney D. Can MRI related patient anxiety be prevented? Magn Reson Imaging. 2015;33:180-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 24. | van Minde D, Klaming L, Weda H. Pinpointing moments of high anxiety during an MRI examination. Int J Behav Med. 2014;21:487-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 25. | Thu H, Stutzman SE, Supnet C, Olson DM. Factors Associated With Increased Anxiety in the MRI Waiting Room. J Radiol Nurs. 2015;34:170-174. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Ifeagwazi CM, Egberi HE, Chukwuorji JC. Emotional reactivity and blood pressure elevations: anxiety as a mediator. Psychol Health Med. 2018;23:585-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |