Published online Jun 6, 2024. doi: 10.12998/wjcc.v12.i16.2876
Revised: April 3, 2024
Accepted: April 18, 2024
Published online: June 6, 2024
Processing time: 118 Days and 23.1 Hours
Epithelioid trophoblastic tumor (ETT) is an extremely rare malignant gestational trophoblastic neoplasm commonly presenting with abnormal vaginal bleeding, abdominal pain, and increased human chorionic gonadotropin (hCG). This study reported a case of uterine ETT with the main manifestation being increased hCG.
A 39-year-old female was referred to the Ningbo Maternal and Child Hospital of China in December 2022, complaining of increased hCG levels for 1 month. Magnetic resonance imaging revealed gestational trophoblastic tumor, and hysteroscopic electrotomy and curettage of intrauterine hyperplasia were per
This study reported a case of uterine ETT with the main manifestation being increased hCG, highlighting that ETT should be considered in the presence of abnormal hCG. A total laparoscopic hysterectomy is recommended.
Core Tip: This study presents a rare case of uterine epithelioid trophoblastic tumor (ETT) with elevation of human chorionic gonadotropin (hCG) as the only sign. The patient, initially misdiagnosed with gestational trophoblastic tumor, underwent a successful total laparoscopic hysterectomy, emphasizing the significance of considering ETT in cases with abnormal hCG. The study highlights the diagnostic challenges posed by ETT and advocates for total laparoscopic hysterectomy as a recommended treatment, contributing valuable insights for gynecologists facing similar cases.
- Citation: Huang LN, Deng X, Xu J. Uterine epithelioid trophoblastic tumor with the main manifestation of increased human chorionic gonadotropin: A case report. World J Clin Cases 2024; 12(16): 2876-2880
- URL: https://www.wjgnet.com/2307-8960/full/v12/i16/2876.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i16.2876
An epithelioid trophoblastic tumor (ETT) originates from chorionic-type intermediate trophoblast cells and occurs mainly in women of childbearing age, accounting for 1%-2% of gestational trophoblastic neoplasm (GTN)[1]. The ETT lesions most commonly occur in the corpus uterus, followed by the cervix uteri and lungs, while a few cases occur in other pelvic and abdominal organs such as the vagina, oviduct, intestinal tract, and liver[2]. ETT commonly presents with abnormal vaginal bleeding, abdominal pain, and normal or mildly increased human chorionic gonadotropin (hCG). Due to the rare occurrence of the disease and the lack of specific clinical manifestations, ETT is very difficult to diagnose. This study reported a case of uterine ETT with the main manifestation being increased hCG.
A 39-year-old female was referred to the Ningbo Maternal and Child Hospital of China in December 2022, complaining of increased hCG levels for 1 month.
hCG was 49.21 IU/L at admission. The patient denied any other complaints.
The patient underwent curettage for hydatidiform mole in 2006.
The patient had undergone two full-term cesarean deliveries in 2010 and 2016, respectively. The patient had no relevant family history.
The physical examination was unremarkable and normal.
hCG was 49.21 IU/L at admission.
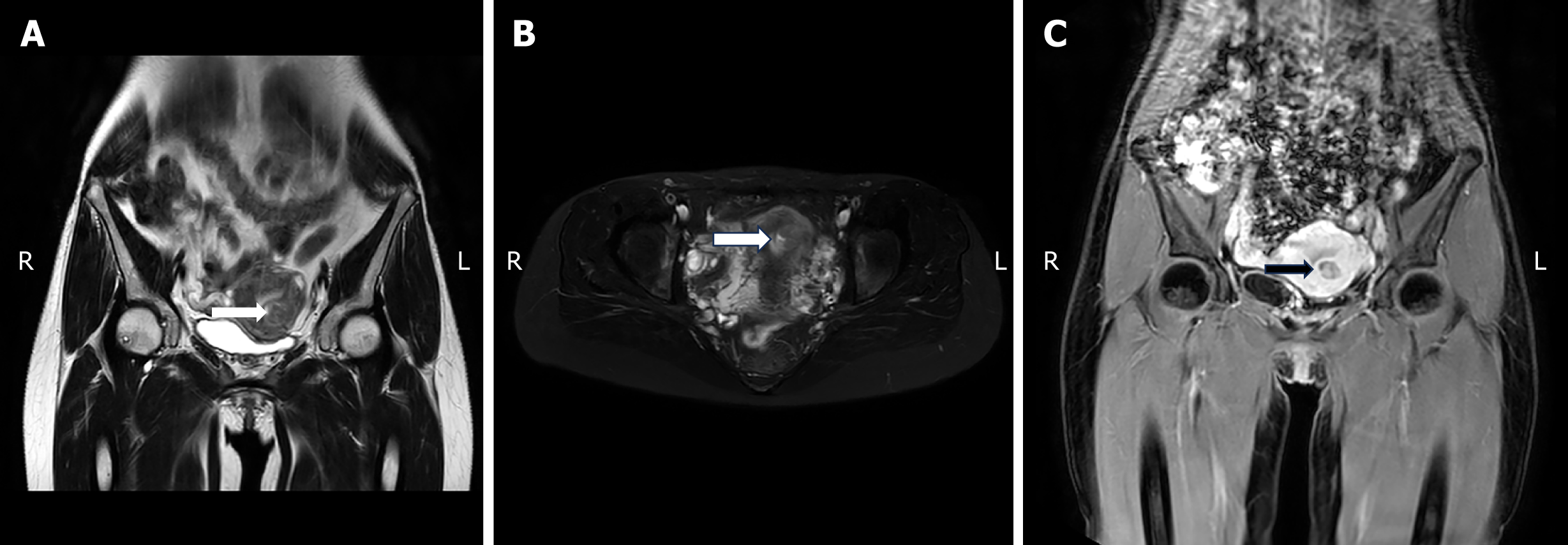
The color Doppler flow imaging of the uterus showed a 21 mm × 7 mm × 20 mm hypoechoic area in the anterior uterine wall with a well-circumscribed margin and a rich blood flow signal (resistance index: 0.46). Magnetic resonance imaging showed roundish long T1 and slightly short T2 signals of 19 mm × 19 mm × 16 mm in the anterior uterine wall (Figure 1), which suggested a GTN.
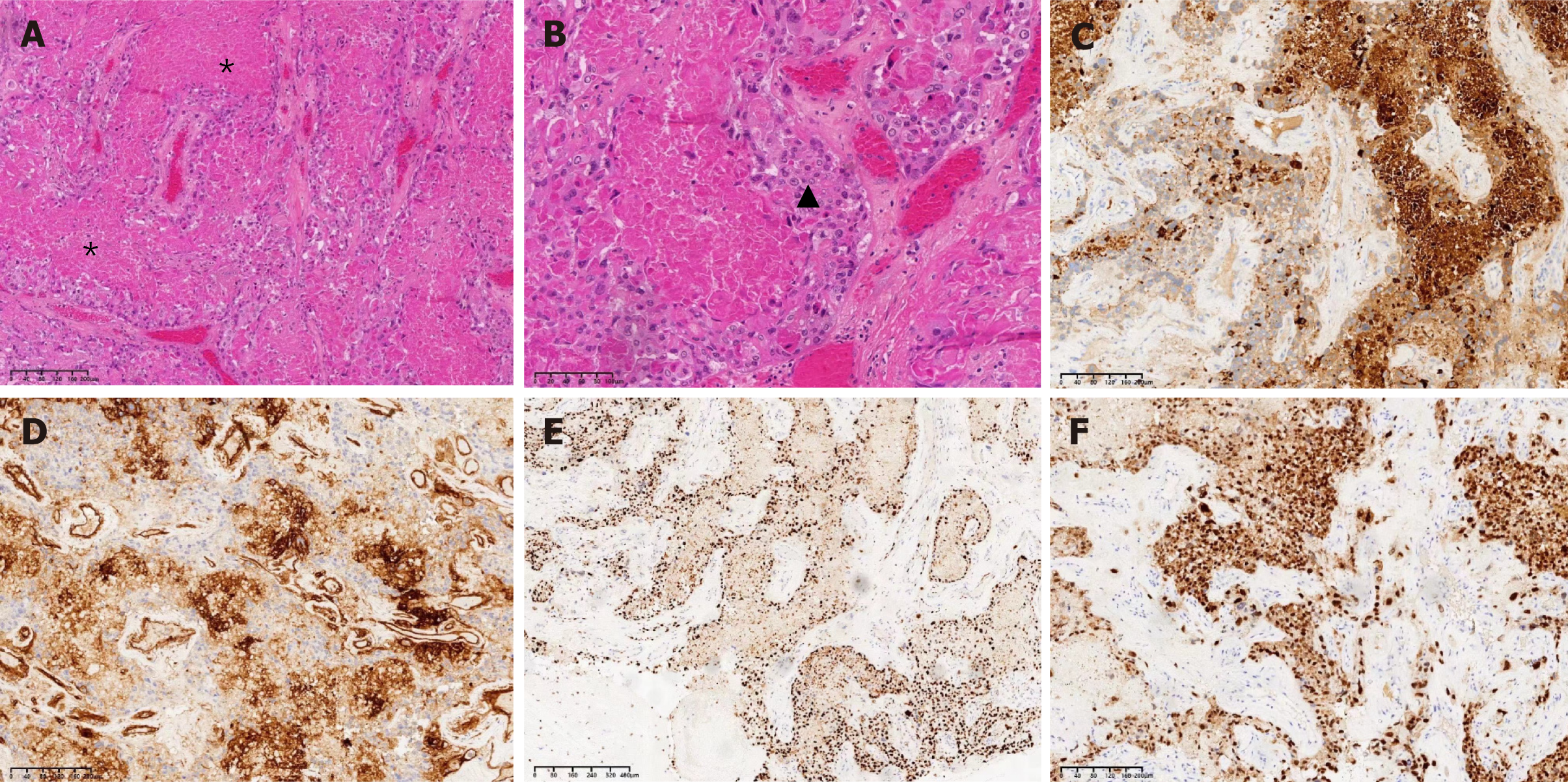
Hysteroscopic electrotomy and curettage of intrauterine hyperplasia were performed. Postoperative pathological examination showed endometrial hyperplastic and intrauterine malignant tumor. Immunohistochemical results showed diffuse positivity for GATA-3, CK (pan), and CD146 and focal positivity for β-hCG, human placental lactogen (hPL), and α-inhibin. Nuclear staining of Ki-67 and P63 was seen (Figure 2). Therefore, the patient was diagnosed with uterine ETT.
Total laparoscopic hysterectomy and bilateral salpingectomy were performed. Postoperative pathology showed tumor residues (infiltrating < 1/2 fibromuscular wall) between the local muscle wall of the uterus, and the maximum diameter of the residual tumor was about 0.6 cm under the microscope.
The hCG levels returned to normal, and the patient did not recur during the postoperative 3-month follow-up.
ETT typically presents with atypical symptoms, such as vaginal bleeding or abdominal pain, but these features were not observed in the present case, posing a challenge to the initial diagnosis. The diagnosis of ETT mainly relies on histopathology and immunohistochemistry. Immunohistochemistry can be used to differentiate ETT from other types of GTN, and the important immunohistochemical markers include p63, α-inhibin, β-hCG, GATA3, hPL, PLAP, and the Ki67 proliferation index[3], consistent with the findings in the case reported here.
Currently, the primary treatment for ETT is hysterectomy, which is recommended for patients with lesions confined to the uterus and no requirement for fertility preservation[4]. In a retrospective review, five women with ETT were cured by hysterectomy[5]. One study reported a case that underwent hysteroscopic resection with uterus preservation and found no recurrence at the 16-month follow-up[6]. For lesions confined to the uterus, complete hysterectomy or extensive resection of lesions can completely alleviate the disease[7]. Considering the strong concealed of ETT, surgery with preservation of reproductive function is generally not recommended[8]. The patient’s hCG decreased to normal after hysteroscopic electrosurgical and curettage of intrauterine hyperplasia, while the pathological results of the specimen showed tumor residue in the endometrial myometrium, indicating that normal hCG after surgery and residual lesion may coexist, and preservation of the uterus should be considered with caution.
The preoperative assessment of the patient indicated that the uterus was of normal size and could be fully extracted vaginally. Therefore, laparoscopic surgery was selected. In cases where the uterus is enlarged and cannot be fully extracted vaginally, open abdominal surgery is still recommended, or protective measures should be taken to remove the specimen (such as placing it in a sealed specimen bag and extracting it through a vaginal incision). The use of a mor
ETT should be considered in the presence of abnormal hCG levels. A total laparoscopic hysterectomy is recommended.
This study reported a case of ETT, the main manifestation of which was increased hCG, providing valuable experience in the diagnosis and treatment of ETT for clinical gynecologists.
| 1. | Horowitz NS, Goldstein DP, Berkowitz RS. Placental site trophoblastic tumors and epithelioid trophoblastic tumors: Biology, natural history, and treatment modalities. Gynecol Oncol. 2017;144:208-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 86] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 2. | Jordan S, Randall LM, Karamurzin Y, Ward P, Lin F, Brewster W, Monk BJ. Differentiating squamous cell carcinoma of the cervix and epithelioid trophoblastic tumor. Int J Gynecol Cancer. 2011;21:918-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Sung WJ, Shin HC, Kim MK, Kim MJ. Epithelioid trophoblastic tumor: clinicopathologic and immunohistochemical analysis of three cases. Korean J Pathol. 2013;47:67-73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Davis MR, Howitt BE, Quade BJ, Crum CP, Horowitz NS, Goldstein DP, Berkowitz RS. Epithelioid trophoblastic tumor: A single institution case series at the New England Trophoblastic Disease Center. Gynecol Oncol. 2015;137:456-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Sobecki-Rausch J, Winder A, Maniar KP, Hoekstra AV, Berry E, Novak K, Lurain JR. Surgery and Platinum/Etoposide-Based Chemotherapy for the Treatment of Epithelioid Trophoblastic Tumor. Int J Gynecol Cancer. 2018;28:1117-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Li J, Shi Y, Wan X, Qian H, Zhou C, Chen X. Epithelioid trophoblastic tumor: a clinicopathological and immunohistochemical study of seven cases. Med Oncol. 2011;28:294-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Yang J, Zong L, Wang J, Wan X, Feng F, Xiang Y. Epithelioid Trophoblastic Tumors: Treatments, Outcomes, and Potential Therapeutic Targets. J Cancer. 2019;10:11-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Jiang F, Xiang Y. [Deeper understanding of epithelioid trophoblastic tumor]. Xiehe Yixue Zazhi. 2018;9:31-35. |
| 9. | Concin N, Matias-Guiu X, Vergote I, Cibula D, Mirza MR, Marnitz S, Ledermann J, Bosse T, Chargari C, Fagotti A, Fotopoulou C, Gonzalez Martin A, Lax S, Lorusso D, Marth C, Morice P, Nout RA, O'Donnell D, Querleu D, Raspollini MR, Sehouli J, Sturdza A, Taylor A, Westermann A, Wimberger P, Colombo N, Planchamp F, Creutzberg CL. ESGO/ESTRO/ESP guidelines for the management of patients with endometrial carcinoma. Int J Gynecol Cancer. 2021;31:12-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1245] [Cited by in RCA: 1113] [Article Influence: 278.3] [Reference Citation Analysis (0)] |
| 10. | Oaknin A, Bosse TJ, Creutzberg CL, Giornelli G, Harter P, Joly F, Lorusso D, Marth C, Makker V, Mirza MR, Ledermann JA, Colombo N; ESMO Guidelines Committee. Endometrial cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol. 2022;33:860-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 312] [Article Influence: 104.0] [Reference Citation Analysis (0)] |
| 11. | Janda M, Gebski V, Davies LC, Forder P, Brand A, Hogg R, Jobling TW, Land R, Manolitsas T, Nascimento M, Neesham D, Nicklin JL, Oehler MK, Otton G, Perrin L, Salfinger S, Hammond I, Leung Y, Sykes P, Ngan H, Garrett A, Laney M, Ng TY, Tam K, Chan K, Wrede CD, Pather S, Simcock B, Farrell R, Robertson G, Walker G, Armfield NR, Graves N, McCartney AJ, Obermair A. Effect of Total Laparoscopic Hysterectomy vs Total Abdominal Hysterectomy on Disease-Free Survival Among Women With Stage I Endometrial Cancer: A Randomized Clinical Trial. JAMA. 2017;317:1224-1233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 257] [Article Influence: 32.1] [Reference Citation Analysis (0)] |