Published online Jun 6, 2024. doi: 10.12998/wjcc.v12.i16.2789
Revised: April 23, 2024
Accepted: April 28, 2024
Published online: June 6, 2024
Processing time: 79 Days and 23.9 Hours
Vitamin deficiencies are linked to various eye diseases, and the influence of vitamin D on cataract formation has been noted in prior research. However, detailed investigations into the causal relationship between 25-(OH)D status and cataract development remain scarce.
To explore a possible causal link between cataracts and vitamin D.
In this study, we explored the causal link between 25-(OH)D levels and cataract development using Mendelian randomization. Our analytical approach included inverse-variance weighting (IVW), MR-Egger, weighted median, simple mode, and weighted mode methods. The primary analyses utilized IVW with random effects, supplemented by sensitivity and heterogeneity tests using both IVW and MR-Egger. MR-Egger was also applied for pleiotropy testing. Additionally, a leave-one-out analysis helped identify potentially impactful single-nucleotide polymorphisms.
The analysis revealed a positive association between 25-(OH)D levels and the risk of developing cataracts (OR = 1.11, 95%CI: 1.00-1.22; P = 0.032). The heterogeneity test revealed that our IVW analysis exhibited minimal heterogeneity (P > 0.05), and the pleiotropy test findings confirmed the absence of pleiotropy within our IVW analysis (P > 0.05). Furthermore, a search of the human genotype-phenotype association database failed to identify any potentially relevant risk-factor single nucleotide polymorphisms.
There is a potential causal link between 25-(OH)D levels and the development of cataracts, suggesting that greater 25-(OH)D levels may be a contributing risk factor for cataract formation. Further experimental research is required to confirm these findings.
Core Tip: Previous studies have documented the role of vitamin D in cataract development, yet investigations into the causal relationship between 25-(OH)D status and cataract onset are still lacking. Using Mendelian randomization, our study established a significant association between elevated 25-(OH)D levels and increased cataract risk. Additionally, a search of the human genotype-phenotype association database revealed no potentially relevant risk-factor single nucleotide polymorphisms. These findings need to be verified by further experiments.
- Citation: Wang CH, Xin ZK. Causal association between 25-hydroxyvitamin D status and cataract development: A two-sample Mendelian randomization study. World J Clin Cases 2024; 12(16): 2789-2795
- URL: https://www.wjgnet.com/2307-8960/full/v12/i16/2789.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i16.2789
The term “cataract” is usually used to refer to the disease characterized by opacity resulting from the degeneration of proteins in the lens, which occurs as a result of disorders in the metabolism of the lens. Cataracts, characterized by clouding of the lens, are the leading cause of blindness globally, accounting for 51% of all cases[1]. In 2010, approximately 10.8 million individuals were blind from cataracts, a figure projected to surge to 40 million by 2025 due to population growth, aging, and extended life expectancies[2,3]. Its etiology is complex and diverse, and conditions such as aging, genetics, local nutritional disorders, immune and metabolic abnormalities, trauma, poisoning, and radiation can lead to metabolic disorders of the lens[4-7]. In this situation, light is blocked by the cloudy lens and cannot be projected on the retina, resulting in blurred vision. It is more common in individuals older than 40 years of age, and its incidence increases with age.
25-Hydroxyvitamin D is the main form of vitamin D stored in the human body and is also the standard for measuring vitamin D status in the human body. Vitamin D is a fat-soluble vitamin that is consumed primarily through food and sunlight and then converted into the biologically active 1,25-dihydroxyvitamin D in the liver and kidneys. Vitamin D plays an important role in calcium absorption and bone health, and a lack of vitamin D can lead to rickets, osteoporosis, weakened immunity and other problems[8,9]. In addition, a few studies have shown that higher vitamin D levels are related to a greater risk of colon cancer and prostate cancer[10,11]. Vitamin D supplementation needs to be determined based on the amount of 25-hydroxyvitamin D in the blood and individual circumstances.
Vitamin deficiencies can lead to a range of eye disorders, and the use of vitamin supplements to prevent certain eye diseases has become a topic of great interest among ophthalmologists in recent years. Vitamin D deficiency may lead to issues such as orbital constriction, bulging eyes, and refractive errors. The role of nutrients in the cause of cataracts has been described in previous studies. However, studies on the causal association between 25-(OH)D status and cataract development are lacking. Therefore, in this paper, we investigated the causal relationship between 25-(OH)D status and cataract development by using magnetic resonance (MR).
Based on the genome-wide association study (GWAS) summary data of 25-(OH)D status and cataract development, this study screened eligible IVs for MR analysis to explore the causal relationship between 25-(OH)D status and cataract development. This study strictly followed the three assumptions of MR analysis: (1) the IVs selected were related to exposure; (2) the IVs were not related to any confounding factors; and (3) the IVs can affect outcomes only through exposure. All datasets used in this study are publicly available.
GWAS data for 25-(OH)D status and cataract development were obtained from the IEU OpenGWAS project (mrcieu.ac.uk) website. The website was accessed on 10 February 2024. These data included 16668957 single-nucleotide polymorphisms (SNPs) associated with 25 hydroxyvitamin D levels (ieu-b-4812) and 8885805 SNPs associated with cataracts (bbj-a-94), with a sample size of 451099 participants. The present study was a reanalysis of previously collected and published publicly available data and therefore did not require additional ethical approval.
Sensitivity analyses were performed using several methods. First, the Cochran Q test was performed to assess the heterogeneity between the individual SNP estimates, and a statistically significant Q statistic was considered to indicate that the analyses were significantly heterogeneous. Second, the Mendelian randomization–pleiotropy residual sum and outlier (MR PRESSO) test was used to validate the results in the IVW model by correcting for the effects of outliers; if outliers were identified, they were removed, and the analysis was repeated. Third, the horizontal pleiotropy of SNPs was tested using the MR Egger intercept test, and if the intercept term in the MR Egger intercept test analysis was statistically significant, it was considered to indicate that the MR analysis had significant horizontal pleiotropy. Fourth, “leave-one-out” sensitivity analyses were performed by removing a single SNP at a time to assess whether the variant drove the association between the exposure and outcome variables. Fifth, funnel plots and forest plots were constructed to visualize the results of the sensitivity analyses. In the MR analyses, P < 0.05 was considered to indicate a statistically significant potential causal relationship. All the statistical analyses were performed using the “TwoSampleMR” package in R software version 4.3.0.
In this study, 102 SNPs strongly associated with 25-(OH)D (P < 5 × 10-8) without chain disequilibrium (r2 < 0.001, kb = 10000) were screened out. Eighty-five SNPs were left after excluding SNPs that were directly associated with the outcome metrics (see Supplementary Table 1). A search of the human genotype-phenotype association database revealed the absence of potentially relevant risk-factor SNPs.
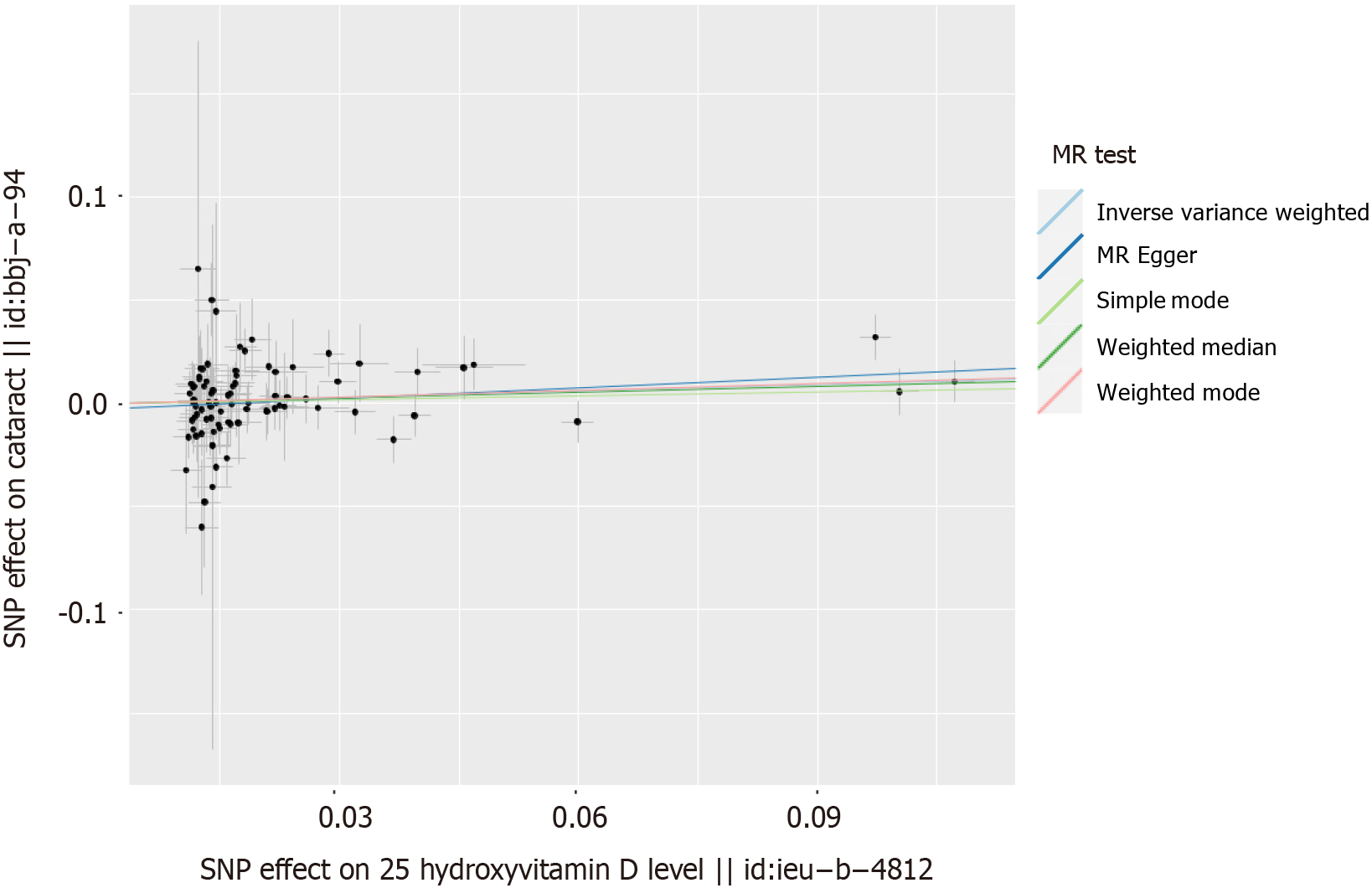
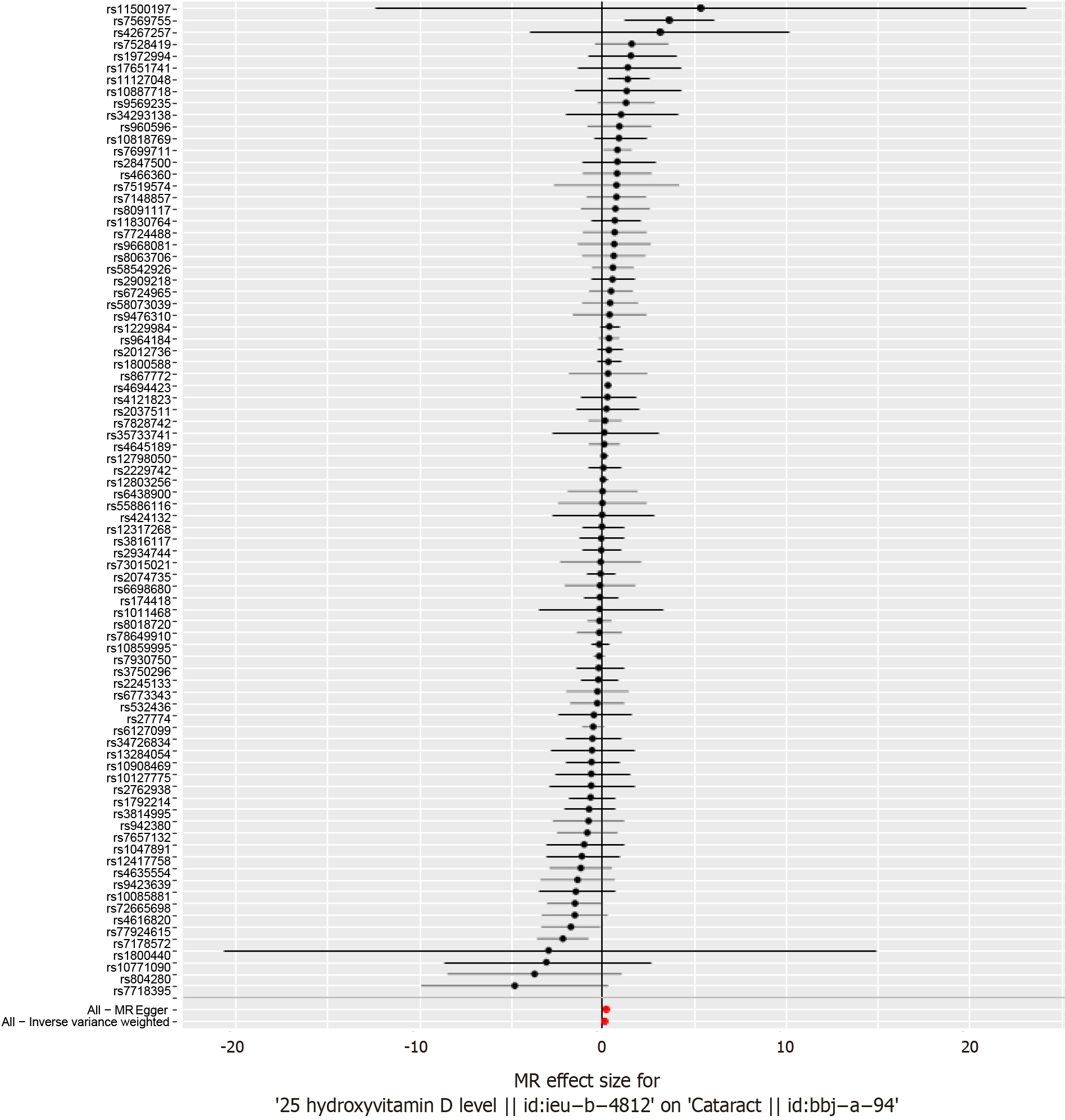
The results from the IVW MR analysis indicate a causal association between 25-(OH)D status and cataract development (IVW: OR = 1.11, 95%CI: 1.00–1.22, P = 0.032; Table 1). Both the scatter plot (Figure 1) and the forest plot (Figure 2) demonstrate that higher levels of 25-(OH)D are associated with an increased risk of cataracts.
| Method | Beta | SE | OR (95%CI) | P value |
| MR Egger | 0.18 | 0.07 | 1.20 (1.03-1.37) | < 0.05 |
| Weighted median | 0.09 | 0.07 | 1.10 (0.95-1.27) | 0.20 |
| IVW | 0.10 | 0.05 | 1.11 (1.01-1.22) | < 0.05 |
| Simple mode | 0.06 | 0.15 | 1.06 (0.80-1.41) | 0.68 |
| Weighted mode | 0.11 | 0.05 | 1.11 (1.00-1.23) | < 0.05 |
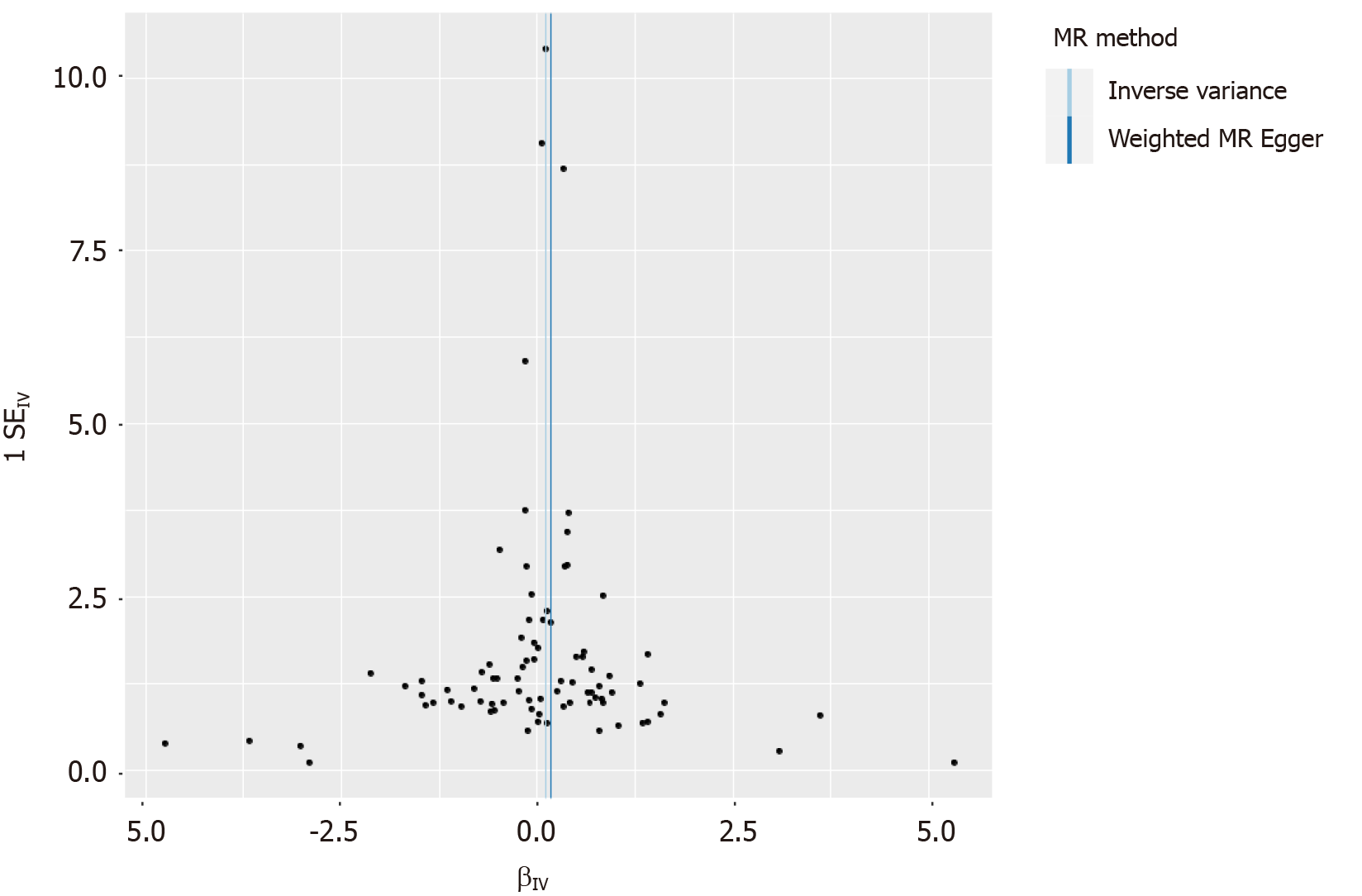
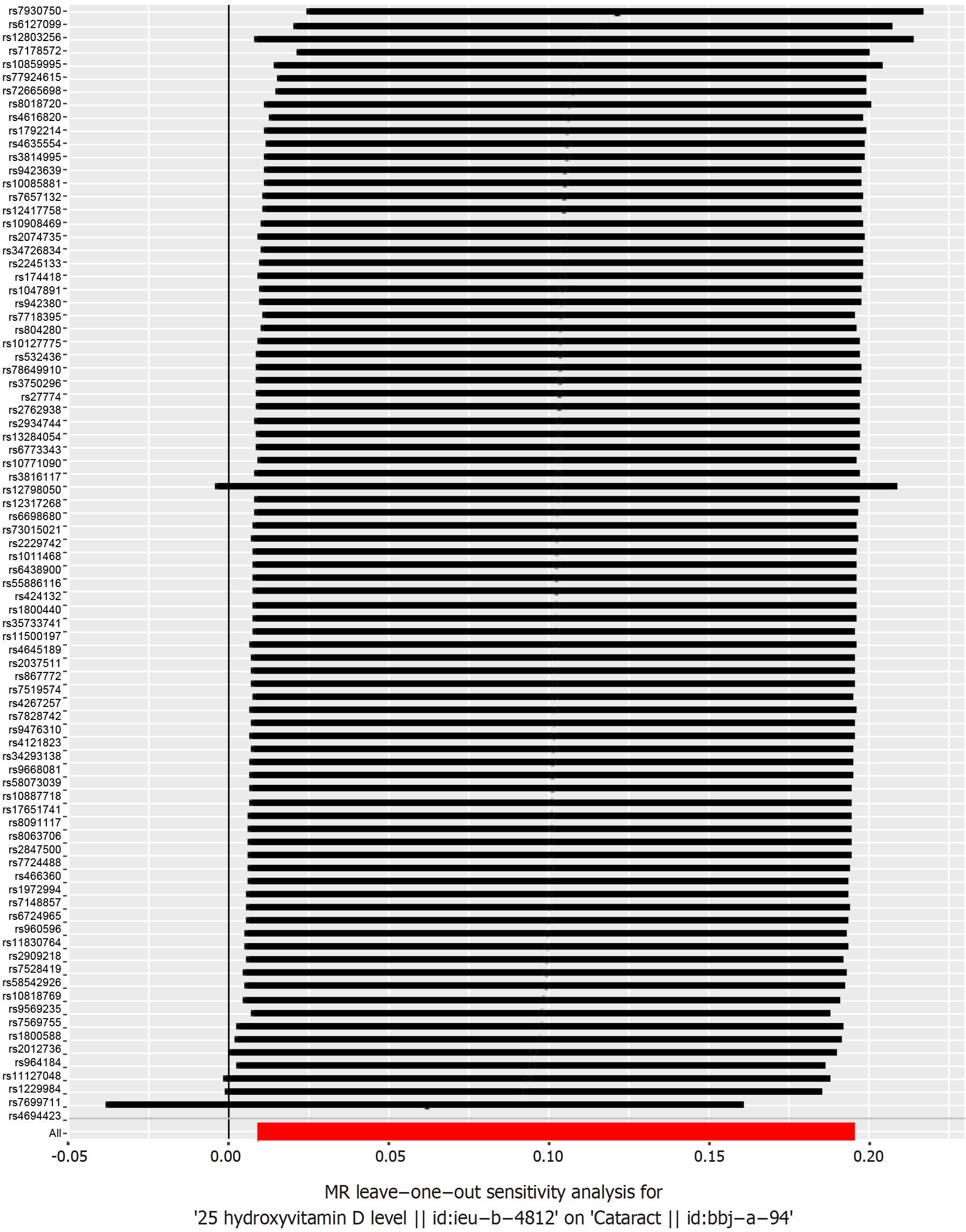
Heterogeneity was tested using the IVW method (Cochran Q test, P = 0.202), and the results suggested that there was no heterogeneity. A funnel plot was drawn to show the heterogeneity results, as shown in Figure 3. MR-PRESSO was used to screen for SNPs that could lead to heterogeneity, and the results did not reveal any SNPs that would lead to heterogeneity in the results. The results of the MR-PRESSO global test suggested that there was no pleiotropy (P = 0.182). The “leave-one-out” method uses the IVW method by default, and as shown in Figure 4, no single SNP was shown to have a large impact on the overall results after its removal, indicating that the results are robust.
Cataracts are the most common cause of blindness in the world; their impact on patients is obvious, and they have a substantial negative impact on the living standards of patients[1]. At present, surgery is the only treatment that is effective. Its etiology and pathogenesis are very complex and unclear, and more detailed and definite research is needed. The role of prevention in cataracts cannot be ignored. Among the preventative factors, targeting the cause is essential. At present, the causes of cataracts can be summarized as follows: (1) Age is one of the main causes of cataracts. With age, the body's metabolic capacity gradually weakens, resulting in a decrease in the transparency of the lens. This type of cataract is called senile cataract and is the most common type; (2) Long-term exposure to ultraviolet light is also an important factor in cataract formation. When people work in the sun and perform outdoor activities, their lenses are exposed to ultraviolet light for a long time. UV light can damage the lens of the eye, causing it to gradually lose its transparency; (3) Certain diseases and genetic factors are also associated with the development of cataracts. For example, chronic diseases such as diabetes and high blood pressure can increase the risk of cataracts. In addition, the influence of dietary factors cannot be ignored. Foods that are rich in antioxidants, such as vitamins A, C and E, can prevent lens protein and membrane damage. Over 16 years of follow-up, Lu et al[12] reported that women with the highest intake of long-chain omega-3 fats were less likely to undergo cataract extraction. Women who eat fatty fish at least once a week have a significantly lower risk of undergoing cataract removal surgery. Eating fish will appropriately reduce the incidence of cataracts. However, increased total dietary fat intake increases the risk of cataract extraction. An increased body mass index is considered a risk factor for posterior subcapsular opacity cataracts and nuclear and cortical cataracts. Alcohol intake is also a risk factor for cataracts.
Regardless of the specific nutrient, on the one hand, we should ensure sufficient intake in the daily diet to maintain the metabolic needs of the body; on the other hand, we also need to avoid excessive intake of nutrients, as that would increase the burden on the body. In the human body, when the 25-hydroxyvitamin D content is too high, clinical symptoms, including nausea, vomiting, and limb weakness, as well as mental symptoms, can occur. In severe cases, frequent urination, dry mouth, etc., can occur; to treat the above issues, individuals should consume adequate nutrition and maintain the balance of water and electrolytes while closely monitoring changes in vital signs. After a period of discontinuation, when the basic symptoms disappear, supplementation can be resumed. 25-Hydroxyvitamin D is a fat-soluble vitamin, and if too much of it is taken orally, it can accumulate in the liver and cause further toxic symptoms.
The present analysis revealed a positive association between 25-(OH)D levels and the risk of developing cataracts, with an OR of 1.11 and a 95%CI ranging from 1.00 to 1.22 (P = 0.032). This suggests a potential causal relationship between 25-(OH)D levels and cataract development, indicating that 25-(OH)D levels could be a contributing risk factor for the onset of cataracts. The findings of this study are similar to those of Liu et al[13], who also reported that increased vitamin D levels were associated with a greater risk of cataracts (OR = 1.14, 95%CI: 1.03–1.28) according to IVW. This study's conclusion is also supported by the findings of Ye et al[14]. According to conventional theories, the protective effects of vitamin D are primarily mediated through immune system modulation, including the activation of cytotoxic T cells and the enhancement of the antimicrobial peptide cationic antimicrobial peptides or the plasma membrane-bound glycoprotein CD14. However, a potential explanation for the increased cataract risk associated with high levels of vitamin D could be that elevated vitamin D concentrations lead to enhanced absorption of dietary calcium, which is known to be a risk factor for cataracts[15].
To explore the specific physiological mechanism by which vitamin D increases the risk of cataracts, relevant validation experiments are needed. According to some studies, the main source of vitamin D in the body relies on sunlight exposure, and ultraviolet light is an important risk factor for cataracts[16]. Therefore, vitamins can promote cataracts. People who lack vitamin D and calcium, especially elderly people, need increased sunlight exposure to obtain more calcium and vitamin D, but that increased exposure increases the risk of cataracts. Therefore, the link between vitamin D and cataracts remains controversial. Some studies have found a negative association between vitamin D and cataracts, while others have found no association between vitamin D and cataracts[17-20]. In the elderly population, a considerable proportion of the population with osteoporosis and other diseases supplements calcium, vitamin D and other nutrients. It should be noted that in this process, the appropriate amount of nutrient intake is beneficial to health. To avoid excessive consumption, individuals should consume the recommended dose.
This study is subject to several limitations. Firstly, as the GWAS data were derived solely from individuals of European descent, the results do not reflect a truly randomized population sample and may not be generalizable to other ethnic groups. Secondly, despite conducting various sensitivity analyses to validate the MR study hypotheses, fully excluding the influence of horizontal pleiotropy in the instrumental variables remains challenging. Lastly, the current GWAS sample size is inadequate, necessitating further in-depth studies with more comprehensive GWAS data in the future.
Using Mendelian randomization, we analyzed the causal association between 25-(OH)D levels and cataracts, and the results showed that there is a possible causal association between 25-(OH)D status and cataract development, and that the 25-(OH)D level is a possible risk factor for cataracts. These findings need to be verified by further experiments.
| 1. | Who Health Organization. Blindness and vision impairment. Aug 10, 2023. [cited 25 February 2024]. Available from: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment. |
| 2. | Khairallah M, Kahloun R, Bourne R, Limburg H, Flaxman SR, Jonas JB, Keeffe J, Leasher J, Naidoo K, Pesudovs K, Price H, White RA, Wong TY, Resnikoff S, Taylor HR; Vision Loss Expert Group of the Global Burden of Disease Study. Number of People Blind or Visually Impaired by Cataract Worldwide and in World Regions, 1990 to 2010. Invest Ophthalmol Vis Sci. 2015;56:6762-6769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 230] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 3. | Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96:614-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2555] [Cited by in RCA: 2148] [Article Influence: 165.2] [Reference Citation Analysis (0)] |
| 4. | Harding JJ, van Heyningen R. Epidemiology and risk factors for cataract. Eye (Lond). 1987;1 ( Pt 5):537-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | West SK, Valmadrid CT. Epidemiology of risk factors for age-related cataract. Surv Ophthalmol. 1995;39:323-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 210] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 6. | Age-Related Eye Disease Study Research Group. Risk factors associated with age-related nuclear and cortical cataract : a case-control study in the Age-Related Eye Disease Study, AREDS Report No. 5. Ophthalmology. 2001;108:1400-1408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 106] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Holekamp NM, Shui YB, Beebe DC. Vitrectomy surgery increases oxygen exposure to the lens: a possible mechanism for nuclear cataract formation. Am J Ophthalmol. 2005;139:302-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 278] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 8. | Bouillon R, Marcocci C, Carmeliet G, Bikle D, White JH, Dawson-Hughes B, Lips P, Munns CF, Lazaretti-Castro M, Giustina A, Bilezikian J. Skeletal and Extraskeletal Actions of Vitamin D: Current Evidence and Outstanding Questions. Endocr Rev. 2019;40:1109-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 514] [Cited by in RCA: 667] [Article Influence: 111.2] [Reference Citation Analysis (0)] |
| 9. | Theodoratou E, Tzoulaki I, Zgaga L, Ioannidis JP. Vitamin D and multiple health outcomes: umbrella review of systematic reviews and meta-analyses of observational studies and randomised trials. BMJ. 2014;348:g2035. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 690] [Cited by in RCA: 671] [Article Influence: 61.0] [Reference Citation Analysis (0)] |
| 10. | Weinstein SJ, Yu K, Horst RL, Ashby J, Virtamo J, Albanes D. Serum 25-hydroxyvitamin D and risks of colon and rectal cancer in Finnish men. Am J Epidemiol. 2011;173:499-508. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Xu Y, Shao X, Yao Y, Xu L, Chang L, Jiang Z, Lin Z. Positive association between circulating 25-hydroxyvitamin D levels and prostate cancer risk: new findings from an updated meta-analysis. J Cancer Res Clin Oncol. 2014;140:1465-1477. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 77] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 12. | Lu M, Cho E, Taylor A, Hankinson SE, Willett WC, Jacques PF. Prospective study of dietary fat and risk of cataract extraction among US women. Am J Epidemiol. 2005;161:948-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Liu H, Shen X, Yu T, Wang Y, Cai S, Jiang X, Cai X. A putative causality of vitamin D in common diseases: A mendelian randomization study. Front Nutr. 2022;9:938356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Ye Y, Yang H, Wang Y, Zhao H. A comprehensive genetic and epidemiological association analysis of vitamin D with common diseases/traits in the UK Biobank. Genet Epidemiol. 2021;45:24-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 15. | Ghahramani M, Yousefi R, Khoshaman K, Alavianmehr MM. The impact of calcium ion on structure and aggregation propensity of peroxynitrite-modified lens crystallins: new insights into the pathogenesis of cataract disorders. Colloids Surf B Biointerfaces. 2015;125:170-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Vinson JA. Oxidative stress in cataracts. Pathophysiology. 2006;13:151-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 172] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 17. | Park S, Choi NK. Serum 25-hydroxyvitamin D and Age-Related Cataract. Ophthalmic Epidemiol. 2017;24:281-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Rao P, Millen AE, Meyers KJ, Liu Z, Voland R, Sondel S, Tinker L, Wallace RB, Blodi BA, Binkley N, Sarto G, Robinson J, LeBlanc E, Mares JA. The Relationship Between Serum 25-Hydroxyvitamin D Levels and Nuclear Cataract in the Carotenoid Age-Related Eye Study (CAREDS), an Ancillary Study of the Women's Health Initiative. Invest Ophthalmol Vis Sci. 2015;56:4221-4230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Jee D, Kim EC. Association between serum 25-hydroxyvitamin D levels and age-related cataracts. J Cataract Refract Surg. 2015;41:1705-1715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Rahman ST, Waterhouse M, Romero BD, Baxter C, English D, Mackey DA, Ebeling PR, Armstrong BK, McLeod DSA, Hartel G, O'Connell RL, van der Pols JC, Venn AJ, Webb PM, Whiteman DC, Neale RE. Vitamin D Supplementation and the Incidence of Cataract Surgery in Older Australian Adults. Ophthalmology. 2023;130:313-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |